Chronic Obstructive Pulmonary Disease in Elderly Patients with Acute and Advanced Heart Failure: Palliative Care Needs—Analysis of the EPICTER Study
Abstract
1. Introduction
2. Material and Methods
2.1. Study Population
2.2. Study Variables
2.3. Statistical Analysis
2.4. Ethical Aspects
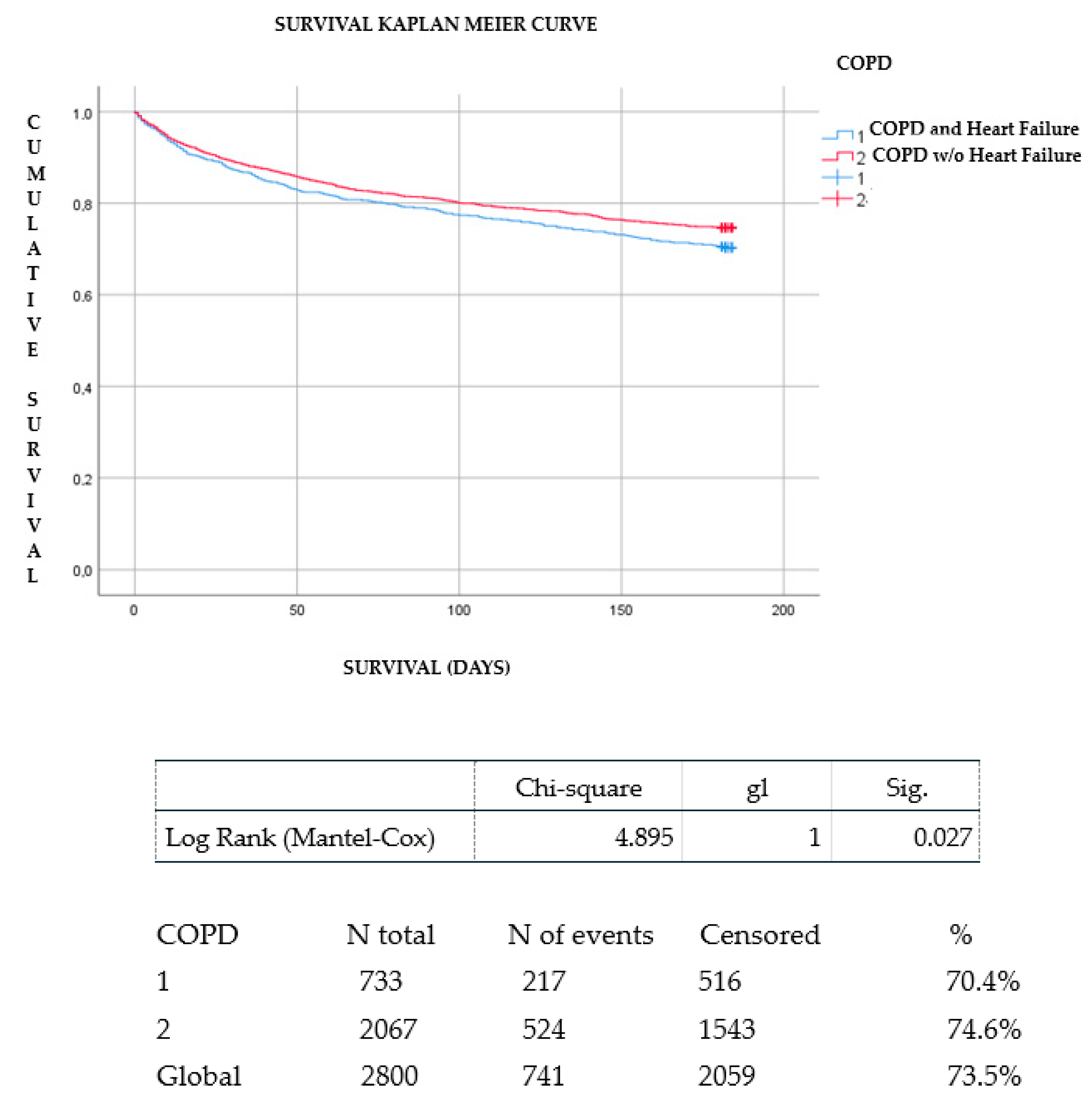
2.5. Results
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Roversi, S.; Fabbri, L.M.; Sin, D.D.; Hawkins, N.M.; Agustí, A. Chronic Obstructive Pulmonary Disease and Cardiac Diseases. An Urgent Need for Integrated Care. Am. J. Respir. Crit. Care Med. 2016, 194, 1319–1336. [Google Scholar] [CrossRef] [PubMed]
- Mullerova, H.; Agusti, A.; Erqou, S.; Mapel, D.W. Cardiovascular comorbidity in COPD: Systematic literature review. Chest 2013, 144, 1163–1178. [Google Scholar] [CrossRef] [PubMed]
- Hesse, K.; Bourke, S.; Steer, J. Heart failure in patients with COPD exacerbations: Looking below the tip of the iceberg. Respir. Med. 2022, 196, 106800. [Google Scholar] [CrossRef]
- Simou, A.; Xanthopoulos, A.; Giamouzis, G.; Papagiannis, D.; Dimos, A.; Economou, D.; Skoularigis, J.; Triposkiadis, F. Coexisting morbidity burden in elderly hospitalized patients with and without heart failure. Hell. J. Cardiol. 2022, 65, 53–55. [Google Scholar] [CrossRef]
- Tinè, M.; Bazzan, E.; Semenzato, U.; Biondini, D.; Cocconcelli, E.; Balestro, E.; Casara, A.; Baraldo, S.; Turato, G.; Cosio, M.G.; et al. Heart failure is highly prevalent and difficult to diagnose in severe exacerbations of COPD presenting to the emergency department. J. Clin. Med. 2020, 9, 2644. [Google Scholar] [CrossRef]
- Loosen, S.H.; Roderburg, C.; Curth, O.; Gaensbacher, J.; Joerdens, M.; Luedde, T.; Konrad, M.; Kostev, K.; Luedde, M. The spectrum of comorbidities at the initial diagnosis of heart failure a case control study. Sci. Rep. 2022, 12, 2670. [Google Scholar] [CrossRef]
- Rushton, C.A.; Satchithananda, D.K.; Jones, P.W.; Kadam, U.T. Noncardiovascular comorbidity, severity and prognosis in non-selected heart failure populations: A systematic review and meta-analysis. Int. J. Cardiol. 2015, 196, 98–106. [Google Scholar] [CrossRef]
- Yoshihisa, A.; Takiguchi, M.; Shimizu, T.; Nakamura, Y.; Yamauchi, H.; Iwaya, S.; Owada, T.; Miyata, M.; Abe, S.; Sato, T.; et al. Cardiovascular function and prognosis of patients with heart failure coexistent with chronic obstructive pulmonary disease. J. Cardiol. 2014, 64, 256–264. [Google Scholar] [CrossRef]
- Fisher, K.A.; Stefan, M.S.; Darling, C.; Lessard, D.; Goldberg, R.J. Impact of COPD on the mortality and treatment of patients hospitalized with acute decompensated heart failure: The Worcester Heart Failure Study. Chest 2015, 147, 637–645. [Google Scholar] [CrossRef][Green Version]
- Creagh-Brown, B. Benefits of b blockers in chronic obstructive pulmonary disease and heart failure. BMJ 2014, 348, g3316. [Google Scholar] [CrossRef]
- Kwon, B.-J.; Kim, D.-B.; Jang, S.-W.; Yoo, K.-D.; Moon, K.-W.; Shim, B.J.; Ahn, S.-H.; Cho, E.-J.; Rho, T.-H.; Kim, J.-H. Prognosis of heart failure patients with reduced and preserved ejection fraction and coexistent chronic obstructive pulmonary disease. Eur. J. Heart Fail. 2010, 12, 1339–1344. [Google Scholar] [CrossRef]
- Mentz, R.J.; Fiuzat, M.; Wojdyla, D.M.; Chiswell, K.; Gheorghiade, M.; Fonarow, G.C.; O’Connor, C.M. Clinical characteristics and outcomes of hospitalized heart failure patients with systolic dysfunction and chronic obstructive pulmonary disease: Findings from OPTIMIZE-HF. Eur. J. Heart Fail. 2012, 14, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Martınez-Selles, M.; Garcıa Robles, J.A.; Prieto, L.; Dominguez Munos, M.; Frades, E.; Dıaz-Castro, O.; Almendral, J. Systolic dysfunction is a predictor of long term mortality in men but not in women with heart failure. Eur. Heart J. 2003, 24, 2046–2053. [Google Scholar] [CrossRef] [PubMed]
- Méndez-Bailón, M.; Lorenzo-Villalba, N.; Romero-Correa, M.; Guisado-Espartero, E.; González-Soler, J.; Rugeles-Niño, J.; Sebastián-Leza, A.; Ceresuela-Eito, L.; Romaní-Costa, V.; Quesada-Simón, A.; et al. Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study. J. Clin. Med. 2022, 11, 571. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.B.; Warraich, H.J.; Butler, J.; Vaduganathan, M. Surprise, surprise: Improving the referral pathway to palliative care interventions in advanced heart failure. Eur. J. Heart Fail. 2019, 21, 235–237. [Google Scholar] [CrossRef]
- Díez-Manglano, J.; Sánchez Muñoz, L.Á.; García Fenoll, R.; Freire, E.; Isasi de Isasmendi Pérez, S.; Carneiro, A.H.; Torres Bonafonte, O. Spanish and Portuguese Societies of Internal Medicine consensus guideline about best practice in end-of-life care. Rev. Clin. Esp. 2020, 221, 33–44. [Google Scholar] [CrossRef]
- Florea, V.G.; Henein, M.Y.; Rauchhaus, M.; Koloczek, V.; Sharma, R.; Doehner, W.; Poole-Wilson, P.A.; Coats, A.J.; Anker, S.D. The cardiac component of cardiac cachexia. Am. Heart J. 2002, 144, 45–50. [Google Scholar] [CrossRef]
- Argilés, J.M.; Busquets, S.; López-Soriano, F.J.; Figueras, M. Fisiopatología de la caquexia neoplásica Pathophysiology of neoplasic cachexia. Nutr. Hosp. 2006, 21, 4–9. [Google Scholar]
- Roesthuis, L.; van der Hoeven, H.; Sinderby, C.; Frenzel, T.; Ottenheijm, C.; Brochard, L.; Doorduin, J.; Heunks, L. Effects of levosimendan on respiratory muscle function in patients weaning from mechanical ventilation. Intensive Care Med. 2019, 45, 1372–1381. [Google Scholar] [CrossRef]
- Farmakis, D.; Alvarez, J.; Gal, T.B.; Brito, D.; Fedele, F.; Fonseca, C.; Gordon, A.C.; Gotsman, I.; Grossini, E.; Guarracino, F.; et al. Levosimendan beyond inotropy and acute heart failure: Evidence of pleiotropic effects on the heart and other organs: An expert panel position paper. Int. J. Cardiol. 2016, 222, 303–312. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Metra, M.; Lund, L.H.; Milicic, D.; Costanzo, M.R.; Filippatos, G.; Gustafsson, F.; Tsui, S.; Barge-Caballero, E.; De Jonge, N.; et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018, 20, 1505–1535. [Google Scholar] [CrossRef] [PubMed]
- Cereda, A.; Toselli, M.; Palmisano, A.; Leone, R.; Vignale, D.; Nicoletti, V.; Campo, G.; Monello, A.; Ippolito, D.; Giannini, F.; et al. Is pleural effusion in COVID-19 interstitial pneumonia related to in-hospital mortality? Ital. J. Med. 2021, 15, 56–58. [Google Scholar] [CrossRef]
- Ruocco, G.; Pastorini, G.; Feola, M. Echocardiography and impedance cardiography as determinants of successful slow levosimendan infusion in advanced older heart failure patients. J. Geriatr. Cardiol. 2021, 18, 1058–1062. [Google Scholar] [PubMed]
| Variable | HF with COPD (n = 812) | HF without COPD (n = 2288) | p |
|---|---|---|---|
| Age (years) mean ± SD | 77.5 ± 10.1 | 79.4 ± 11.1 | 0.001 |
| Sex (male), N (%) | 575 (70.8%) | 955 (41.7%) | 0.001 |
| NYHA III-IV, N (%) | 233/802 (29.1%) | 486/2241 (21.7%) | 0.001 |
| LVEF, mean ± SD | 50.08 ± 16.5 | 51.26 ± 15.9 | 0.65 |
| NTpro-BNP pg/mL, mean | 7910.4 | 8550.2 | 0.4 |
| Comorbidities | |||
| Charlson comorbidity index mean ± SD | 4.49 ± 1.76 | 3.24 ± 1.8 | 0.0001 |
| Hypertension N (%) | 694/809 (85.8%) | 1936/2283 (84.8%) | 0.528 |
| Diabetes N (%) | 397/810 (49%) | 1010/2279 (44.3%) | 0.022 |
| Ischemic heart disease N (%) | 271/804 (33.7%) | 713/2257 (31.6%) | 0.271 |
| Atrial fibrillation N (%) | 470/809 (58.1%) | 1286/2281 (56.4%) | 0.409 |
| Valve disease N (%) | 176/377 (37.8%) | 1012/2194 (46.1%) | 0.001 |
| Chronic kidney disease N (%) | 410/807 (50.8%) | 1041/2270 (45.9%) | 0.017 |
| Cerebrovascular disease N (%) | 164/797 (20.6%) | 498/2269 (21.9%) | 0.453 |
| Anemia N (%) | 382/806 (47.4%) | 1118/2274 (48.7%) | 0.390 |
| Variable | HF with COPD n = 528 | HF without COPD n = 1480 | p-Value |
|---|---|---|---|
| Dyspnea N (%) | 455/528 (86.2%) | 1114/1480 (75.3%) | 0.0001 |
| >10% Weight loss N (%) | 48/356 (13.5%) | 121/900 (11.9%) | 0.236 |
| Functional impairment N (%) | 146/379 (38.5%) | 390/715 (35.3%) | 0.265 |
| Anxiety N (%) | 187/528 (35.4%) | 462/1480 (31.2%) | 0.043 |
| Nausea N (%) | 52/528 (9.8%) | 176/1480 (11.9%) | 0.231 |
| Chest pain N (%) | 99/528 (18.8%) | 281/1478 (19%) | 0.948 |
| Generalized pain N (%) | 157/528 (29.7%) | 394/1477 (26.7%) | 0.098 |
| Delirium N (%) | 83/528 (15.7%) | 217/1480 (14.7%) | 0.570 |
| Insomnia N (%) | 197/528 (37.3%) | 507/1478 (35%) | 0.222 |
| Variable | HF with COPD (n = 812) | HF without COPD (n = 2288) | p |
|---|---|---|---|
| Non-invasive mechanical ventilation n (%) | 62 (7.6%) | 105 (4.6%) | 0.004 |
| High Flow oxygen n (%) | 74/529 (14%) | 229/2014 (11.4%) | 0.018 |
| Nitroglicerine iv | 69/805(86%) | 237/2281(20.4%) | 0.222 |
| Hypertonic saline + furosemide n (%) | 15/536 (2.8%) | 34/1495 (2.3%) | 0.297 |
| Furosemide perfusion n (%) | 138/812 (17%) | 364/2288 (15.9%) | 0.770 |
| Use of amines n (%) | 50/812 (6.2%) | 110/2288 (4.8%) | 0.326 |
| Levosimendan n (%) | 11/812 (1.4%) | 23/2288 (1%) | |
| Dialysis n (%) | 6/536 (1.1%) | 17/1493 (1.1%) | 1.000 |
| Oral morphine n (%) | 151/536 (28.2%) | 379/1497 (25.3%) | 0.109 |
| Subcutaneous morphine n (%) | 74/472 (15.7%) | 223/1304 (17.1%) | 0.263 |
| Benzodiazepines n (%) | 185/535 (34.6%) | 496/1496 (33.2%) | 0.292 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Méndez-Bailón, M.; Lorenzo-Villalba, N.; Romero-Correa, M.; Josa-Laorden, C.; Inglada-Galiana, L.; Menor-Campos, E.; Gómez-Aguirre, N.; Clemente-Sarasa, C.; Salas-Campos, R.; García-Redecillas, C.; et al. Chronic Obstructive Pulmonary Disease in Elderly Patients with Acute and Advanced Heart Failure: Palliative Care Needs—Analysis of the EPICTER Study. J. Clin. Med. 2022, 11, 3709. https://doi.org/10.3390/jcm11133709
Méndez-Bailón M, Lorenzo-Villalba N, Romero-Correa M, Josa-Laorden C, Inglada-Galiana L, Menor-Campos E, Gómez-Aguirre N, Clemente-Sarasa C, Salas-Campos R, García-Redecillas C, et al. Chronic Obstructive Pulmonary Disease in Elderly Patients with Acute and Advanced Heart Failure: Palliative Care Needs—Analysis of the EPICTER Study. Journal of Clinical Medicine. 2022; 11(13):3709. https://doi.org/10.3390/jcm11133709
Chicago/Turabian StyleMéndez-Bailón, Manuel, Noel Lorenzo-Villalba, Miriam Romero-Correa, Claudia Josa-Laorden, Luis Inglada-Galiana, Eva Menor-Campos, Noelia Gómez-Aguirre, Carolina Clemente-Sarasa, Rosario Salas-Campos, Carmen García-Redecillas, and et al. 2022. "Chronic Obstructive Pulmonary Disease in Elderly Patients with Acute and Advanced Heart Failure: Palliative Care Needs—Analysis of the EPICTER Study" Journal of Clinical Medicine 11, no. 13: 3709. https://doi.org/10.3390/jcm11133709
APA StyleMéndez-Bailón, M., Lorenzo-Villalba, N., Romero-Correa, M., Josa-Laorden, C., Inglada-Galiana, L., Menor-Campos, E., Gómez-Aguirre, N., Clemente-Sarasa, C., Salas-Campos, R., García-Redecillas, C., Asenjo-Martínez, M., Trullàs, J. C., Cortés-Rodríguez, B., de la Guerra-Acebal, C., Serrado Iglesias, A., Aparicio-Santos, R., Formiga, F., Andrès, E., Aramburu-Bodas, O., ... on behalf of EPICTER Study Group. (2022). Chronic Obstructive Pulmonary Disease in Elderly Patients with Acute and Advanced Heart Failure: Palliative Care Needs—Analysis of the EPICTER Study. Journal of Clinical Medicine, 11(13), 3709. https://doi.org/10.3390/jcm11133709







