Differences in Pulmonary and Extra-Pulmonary Traits between Women and Men with Chronic Obstructive Pulmonary Disease
Abstract
:1. Introduction
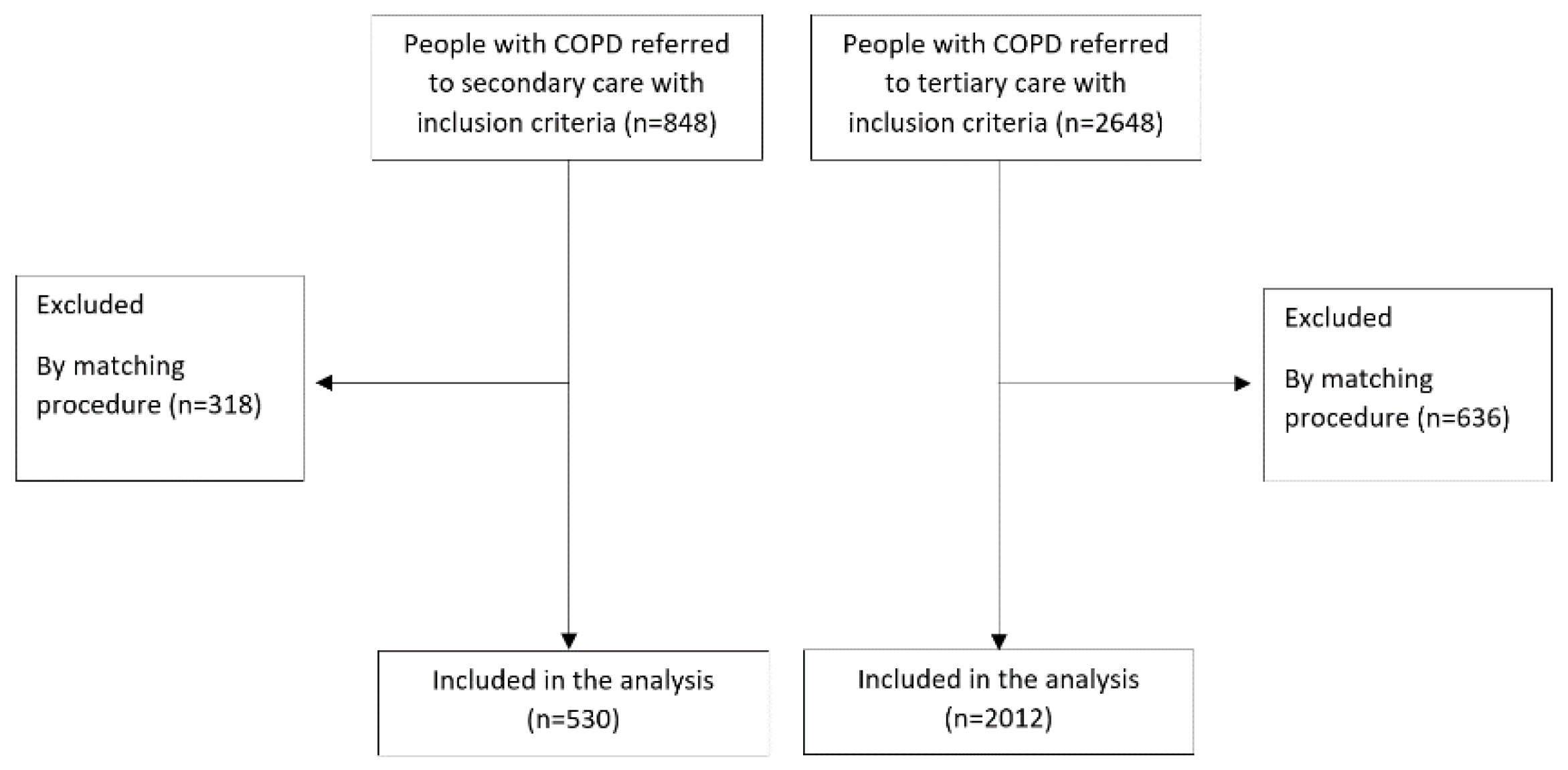
2. Materials and Methods
2.1. Data Collection
2.2. Statistical Analysis
3. Results
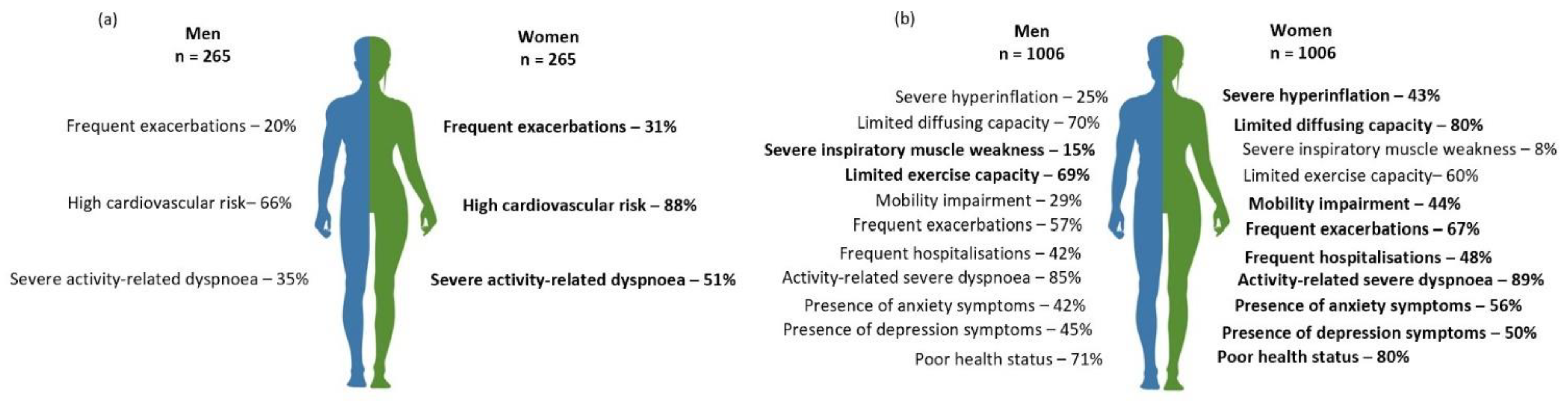
3.1. Pulmonary Traits
3.2. Extra-Pulmonary Traits
3.3. Behavioral Traits
4. Discussion
4.1. Pulmonary Traits
4.2. Extra-Pulmonary Traits
4.3. Behavioral Traits
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ntritsos, G.; Franek, J.; Belbasis, L.; Christou, M.A.; Markozannes, G.; Altman, P.; Fogel, R.; Sayre, T.; Ntzani, E.E.; Evangelou, E. Gender-specific estimates of COPD prevalence: A systematic review and meta-analysis. Int. J. Chron. Obs. Pulm. Dis. 2018, 13, 1507–1514. [Google Scholar] [CrossRef] [Green Version]
- Tsiligianni, I.; Rodríguez, M.R.; Lisspers, K.; LeeTan, T.; Infantino, A. Call to action: Improving primary care for women with COPD. Npj Prim. Care Respir. Med. 2017, 27, 11. [Google Scholar] [CrossRef] [Green Version]
- Aryal, S.; Diaz-Guzman, E.; Mannino, D.M. Influence of sex on chronic obstructive pulmonary disease risk and treatment outcomes. Int. J. Chron. Obs. Pulmon. Dis. 2014, 9, 1145–1154. [Google Scholar] [CrossRef] [Green Version]
- LoMauro, A.; Aliverti, A. Sex and gender in respiratory physiology. Eur. Respir. Rev. 2021, 30, 210038. [Google Scholar] [CrossRef]
- Chapman, K.R.; Tashkin, D.P.; Pye, D.J. Gender bias in the diagnosis of COPD. Chest 2001, 119, 1691–1695. [Google Scholar] [CrossRef]
- Åberg, J.; Hasselgren, M.; Montgomery, S.; Lisspers, K.; Ställberg, B.; Janson, C.; Sundh, J. Sex-related differences in management of Swedish patients with a clinical diagnosis of chronic obstructive pulmonary disease. Int. J. Chronic Obs. Pulm. Dis. 2019, 14, 961–969. [Google Scholar] [CrossRef] [Green Version]
- Trigueros, J.A.; Riesco, J.A.; Alcázar-Navarrete, B.; Campuzano, A.; Pérez, J. Clinical Features Of Women With COPD: Sex Differences In A Cross-Sectional Study In Spain (“The ESPIRAL-ES Study”). Int. J. Chronic Obstr. Pulm. Dis. 2019, 14, 2469–2478. [Google Scholar] [CrossRef] [Green Version]
- De Torres, J.P.; Casanova, C.; Hernández, C.; Abreu, J.; Aguirre-Jaime, A.; Celli, B.R. Gender and COPD in Patients Attending a Pulmonary Clinic. Chest 2005, 128, 2012–2016. [Google Scholar] [CrossRef]
- Di Marco, F.; Verga, M.; Reggente, M.; Maria Casanova, F.; Santus, P.; Blasi, F.; Allegra, L.; Centanni, S. Anxiety and depression in COPD patients: The roles of gender and disease severity. Respir. Med. 2006, 100, 1767–1774. [Google Scholar] [CrossRef] [Green Version]
- Choi, J.Y.; Kim, S.Y.; Lee, J.H.; Park, Y.B.; Kim, Y.H.; Um, S.-J.; Jung, K.S.; Yoo, K.H.; Park, S.J.; Yoon, H.K. Clinical Characteristics of Chronic Obstructive Pulmonary Disease in Female Patients: Findings from a KOCOSS Cohort. Int. J. Chronic Obstr. Pulm. Dis. 2020, 15, 2217–2224. [Google Scholar] [CrossRef]
- McDonald, V.M.; Fingleton, J.; Agusti, A.; Hiles, S.A.; Clark, V.L.; Holland, A.E.; Marks, G.B.; Bardin, P.P.; Beasley, R.; Pavord, I.D.; et al. Treatable traits: A new paradigm for 21st century management of chronic airway diseases: Treatable Traits Down Under International Workshop report. Eur. Respir. J. 2019, 53, 1802058. [Google Scholar] [CrossRef] [PubMed]
- Graham, B.L.; Steenbruggen, I.; Miller, M.R.; Barjaktarevic, I.Z.; Cooper, B.G.; Hall, G.L.; Hallstrand, T.S.; Kaminsky, D.A.; McCarthy, K.; McCormack, M.C.; et al. Standardization of Spirometry 2019 Update. An Official American Thoracic Society and European Respiratory Society Technical Statement. Am. J. Respir. Crit. Care Med. 2019, 200, e70–e88. [Google Scholar] [CrossRef]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; McCormack, M.C.; Carlin, B.W.; Sciurba, F.C.; Pitta, F.; et al. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428. [Google Scholar] [CrossRef]
- Mahler, D.A.; Wells, C.K. Evaluation of clinical methods for rating dyspnea. Chest 1988, 93, 580–586. [Google Scholar] [CrossRef] [Green Version]
- GOLD. Global Strategy for Prevention, Diagnosis and Management of COPD; GOLD: Brussels, Belgium, 2022. [Google Scholar]
- Payne, R.A. Cardiovascular risk. Br. J. Clin. Pharm. 2012, 74, 396–410. [Google Scholar] [CrossRef]
- Engelen, M.P.; Schols, A.M.; Heidendal, G.A.; Wouters, E.F. Dual-energy X-ray absorptiometry in the clinical evaluation of body composition and bone mineral density in patients with chronic obstructive pulmonary disease. Am. J. Clin. Nutr. 1998, 68, 1298–1303. [Google Scholar] [CrossRef] [Green Version]
- Ofenheimer, A.; Breyer-Kohansal, R.; Hartl, S.; Burghuber, O.C.; Krach, F.; Schrott, A.; Wouters, E.F.M.; Franssen, F.M.E.; Breyer, M.K. Reference values of body composition parameters and visceral adipose tissue (VAT) by DXA in adults aged 18-81 years-results from the LEAD cohort. Eur. J. Clin. Nutr. 2020, 74, 1181–1191. [Google Scholar] [CrossRef]
- Laveneziana, P.; Albuquerque, A.; Aliverti, A.; Babb, T.; Barreiro, E.; Dres, M.; Dubé, B.-P.; Fauroux, B.; Gea, J.; Guenette, J.A.; et al. ERS statement on respiratory muscle testing at rest and during exercise. Eur. Respir. J. 2019, 53, 1801214. [Google Scholar] [CrossRef] [Green Version]
- Graham, B.L.; Brusasco, V.; Burgos, F.; Cooper, B.G.; Jensen, R.; Kendrick, A.; MacIntyre, N.R.; Thompson, B.R.; Wanger, J. 2017 ERS/ATS standards for single-breath carbon monoxide uptake in the lung. Eur. Respir. J. 2017, 49, 1600016. [Google Scholar] [CrossRef] [Green Version]
- Wanger, J.; Clausen, J.L.; Coates, A.; Pedersen, O.F.; Brusasco, V.; Burgos, F.; Casaburi, R.; Crapo, R.; Enright, P.; van der Grinten, C.P.M.; et al. Standardisation of the measurement of lung volumes. Eur. Respir. J. 2005, 26, 511. [Google Scholar] [CrossRef]
- Radtke, T.; Crook, S.; Kaltsakas, G.; Louvaris, Z.; Berton, D.; Urquhart, D.S.; Kampouras, A.; Rabinovich, R.A.; Verges, S.; Kontopidis, D.; et al. ERS statement on standardisation of cardiopulmonary exercise testing in chronic lung diseases. Eur. Respir. Rev. 2019, 28, 180101. [Google Scholar] [CrossRef] [Green Version]
- Van’t Hul, A.; Gosselink, R.; Kwakkel, G. Constant-load cycle endurance performance: Test-retest reliability and validity in patients with COPD. J. Cardiopulm. Rehabil. 2003, 23, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Van Remoortel, H.; Raste, Y.; Louvaris, Z.; Giavedoni, S.; Burtin, C.; Langer, D.; Wilson, F.; Rabinovich, R.; Vogiatzis, I.; Hopkinson, N.S.; et al. Validity of six activity monitors in chronic obstructive pulmonary disease: A comparison with indirect calorimetry. PLoS ONE 2012, 7, e39198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Worm-Smeitink, M.; Gielissen, M.; Bloot, L.; van Laarhoven, H.W.M.; van Engelen, B.G.M.; van Riel, P.; Bleijenberg, G.; Nikolaus, S.; Knoop, H. The assessment of fatigue: Psychometric qualities and norms for the Checklist individual strength. J. Psychosom. Res. 2017, 98, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van der Molen, T.; Willemse, B.W.; Schokker, S.; ten Hacken, N.H.; Postma, D.S.; Juniper, E.F. Development, validity and responsiveness of the Clinical COPD Questionnaire. Health Qual Life Outcomes 2003, 1, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, P.W.; Harding, G.; Berry, P.; Wiklund, I.; Chen, W.H.; Kline Leidy, N. Development and first validation of the COPD Assessment Test. Eur. Respir. J. 2009, 34, 648. [Google Scholar] [CrossRef] [Green Version]
- Spruit, M.A.; Augustin, I.M.L.; Vanfleteren, L.E.; Janssen, D.J.A.; Gaffron, S.; Pennings, H.-J.; Smeenk, F.; Pieters, W.; van den Bergh, J.J.A.M.; Michels, A.-J.; et al. Differential response to pulmonary rehabilitation in COPD: Multidimensional profiling. Eur. Respir. J. 2015, 46, 1625. [Google Scholar] [CrossRef]
- Vaes, A.W.; Delbressine, J.M.L.; Mesquita, R.; Goertz, Y.M.J.; Janssen, D.J.A.; Nakken, N.; Franssen, F.M.E.; Vanfleteren, L.E.G.W.; Wouters, E.F.M.; Spruit, M.A. Impact of pulmonary rehabilitation on activities of daily living in patients with chronic obstructive pulmonary disease. J. Appl. Physiol. 2018, 126, 607–615. [Google Scholar] [CrossRef]
- Koolen, E.H.; van Hees, H.W.; van Lummel, R.C.; Dekhuijzen, R.; Djamin, R.S.; Spruit, M.A.; van ‘t Hul, A.J. “Can do” versus “do do”: A Novel Concept to Better Understand Physical Functioning in Patients with Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2019, 8, 340. [Google Scholar] [CrossRef] [Green Version]
- Van’t Hul, A.J.; Koolen, E.H.; Antons, J.C.; de Man, M.; Djamin, R.S.; In’t Veen, J.; Simons, S.O.; van den Heuvel, M.; van den Borst, B.; Spruit, M.A. Treatable traits qualifying for nonpharmacological interventions in COPD patients upon first referral to a pulmonologist: The COPD sTRAITosphere. ERJ Open Res. 2020, 6, 00438-2020. [Google Scholar] [CrossRef] [PubMed]
- Herth, F.J.F.; Slebos, D.J.; Criner, G.J.; Valipour, A.; Sciurba, F.; Shah, P.L. Endoscopic Lung Volume Reduction: An Expert Panel Recommendation—Update 2019. Respiration 2019, 97, 548–557. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, R.; Viegi, G.; Brusasco, V.; Crapo, R.O.; Burgos, F.; Casaburi, R.; Coates, A.; van der Grinten, C.P.M.; Gustafsson, P.; Hankinson, J.; et al. Interpretative strategies for lung function tests. Eur. Respir. J. 2005, 26, 948. [Google Scholar] [CrossRef] [PubMed]
- Charususin, N.; Gosselink, R.; Decramer, M.; McConnell, A.; Saey, D.; Maltais, F.; Derom, E.; Vermeersch, S.; van Helvoort, H.; Heijdra, Y.; et al. Inspiratory muscle training protocol for patients with chronic obstructive pulmonary disease (IMTCO study): A multicentre randomised controlled trial. BMJ Open 2013, 3, e003101. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Black, L.F.; Hyatt, R.E. Maximal respiratory pressures: Normal values and relationship to age and sex. Am. Rev. Respir Dis. 1969, 99, 696–702. [Google Scholar] [CrossRef]
- GOLD. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstruuctive Pulmonary Disease; GOLD: Brussels, Belgium, 2021. [Google Scholar]
- Lee, J.S.; Seo, J.B.; Lee, S.M.; Park, T.S.; Lee, S.W.; Oh, Y.M.; Lee, J.H.; Kim, E.K.; Kim, T.H.; Park, J.H.; et al. Pharmacological treatment response according to the severity of symptoms in patients with chronic obstructive pulmonary disease. J. Thorac. Dis. 2015, 7, 1765–1773. [Google Scholar] [CrossRef]
- Goërtz, Y.M.J.; Looijmans, M.; Prins, J.B.; Janssen, D.J.A.; Thong, M.S.Y.; Peters, J.B.; Burtin, C.; Meertens-Kerris, Y.; Coors, A.; Muris, J.W.M.; et al. Fatigue in patients with chronic obstructive pulmonary disease: Protocol of the Dutch multicentre, longitudinal, observational FAntasTIGUE study. BMJ Open 2018, 8, e021745. [Google Scholar] [CrossRef] [Green Version]
- Bjelland, I.; Dahl, A.A.; Haug, T.T.; Neckelmann, D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002, 52, 69–77. [Google Scholar] [CrossRef]
- Smid, D.E.; Franssen, F.M.E.; Gonik, M.; Miravitlles, M.; Casanova, C.; Cosio, B.G.; de Lucas-Ramos, P.; Marin, J.M.; Martinez, C.; Mir, I.; et al. Redefining Cut-Points for High Symptom Burden of the Global Initiative for Chronic Obstructive Lung Disease Classification in 18,577 Patients With Chronic Obstructive Pulmonary Disease. J. Am. Med. Dir. Assoc. 2017, 18, 1097.e1011–1097.e1024. [Google Scholar] [CrossRef] [Green Version]
- Guo, Y.; Zhang, T.; Wang, Z.; Yu, F.; Xu, Q.; Guo, W.; Wu, C.; He, J. Body mass index and mortality in chronic obstructive pulmonary disease: A dose-response meta-analysis. Medicine 2016, 95, e4225. [Google Scholar] [CrossRef]
- Pouliot, M.C.; Després, J.P.; Lemieux, S.; Moorjani, S.; Bouchard, C.; Tremblay, A.; Nadeau, A.; Lupien, P.J. Waist circumference and abdominal sagittal diameter: Best simple anthropom.metric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am. J. Cardiol. 1994, 73, 460–468. [Google Scholar] [CrossRef]
- Troosters, T.; Gosselink, R.; Decramer, M. Six minute walking distance in healthy elderly subjects. Eur. Respir. J. 1999, 14, 270–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wasserman, K.; Hansen, J.E.; Sue, D.Y.; Whipp, B.J.; Froelicher, V.F. Principles of exercise testing and interpretation. J. Cardiopulm. Rehabil. Prev. 1987, 7, 189. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Craig, C.L.; Aoyagi, Y.; Bell, R.C.; Croteau, K.A.; De Bourdeaudhuij, I.; Ewald, B.; Gardner, A.W.; Hatano, Y.; Lutes, L.D.; et al. How many steps/day are enough? For older adults and special populations. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 80. [Google Scholar] [CrossRef] [Green Version]
- Bennett, D.A. How can I deal with missing data in my study? Aust. N. Z. J. Public Health 2001, 25, 464–469. [Google Scholar] [CrossRef]
- DeMeo, D.L.; Ramagopalan, S.; Kavati, A.; Vegesna, A.; Han, M.K.; Yadao, A.; Wilcox, T.K.; Make, B.J.; Investigators, C.O. Women manifest more severe COPD symptoms across the life course. Int. J. Chronic Obstr. Pulm. Dis. 2018, 13, 3021–3029. [Google Scholar] [CrossRef] [Green Version]
- Donnell, D.E.; Laveneziana, P. Physiology and consequences of lung hyperinflation in COPD. Eur. Respir. Rev. 2006, 15, 61. [Google Scholar] [CrossRef]
- O’Donnell, D.E.; Laveneziana, P. Dyspnea and Activity Limitation in COPD: Mechanical Factors. COPD J. Chronic Obstr. Pulm. Dis. 2007, 4, 225–236. [Google Scholar] [CrossRef]
- Rochester, D.F.; Braun, N.M. Determinants of maximal inspiratory pressure in chronic obstructive pulmonary disease. Am. Rev. Respir. Dis. 1985, 132, 42–47. [Google Scholar] [CrossRef]
- Souto-Miranda, S.; Jácome, C.; Alves, A.; Machado, A.; Paixão, C.; Oliveira, A.; Marques, A. International predictive equations of maximum respiratory mouth pressures: Are they suitable for the Portuguese adult population? Pulmonology 2021, 27, 366–368. [Google Scholar] [CrossRef]
- Effing, T.W.; Vercoulen, J.H.; Bourbeau, J.; Trappenburg, J.; Lenferink, A.; Cafarella, P.; Coultas, D.; Meek, P.; van der Valk, P.; Bischoff, E.W.M.A.; et al. Definition of a COPD self-management intervention: International Expert Group consensus. Eur. Respir. J. 2016, 48, 46. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, S.E.; Barker, R.E.; Nolan, C.M.; Patel, S.; Maddocks, M.; Man, W.D.C. Pulmonary rehabilitation in patients with an acute exacerbation of chronic obstructive pulmonary disease. J. Thorac. Dis. 2018, 10, S139–S1399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef]
- Zysman, M.; Burgel, P.R.; Court-Fortune, I.; Brinchault-Rabin, G.; Nesme-Meyer, P.; Surpas, P.; Deslée, G.; Perez, T.; Le Rouzic, O.; Jebrak, G.; et al. Relationship between gender and survival in a real-life cohort of patients with COPD. Respir. Res. 2019, 20, 191. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Becklake, M.R.; Kauffmann, F. Gender differences in airway behaviour over the human life span. Thorax 1999, 54, 1119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McCarthy, B.; Casey, D.; Devane, D.; Murphy, K.; Murphy, E.; Lacasse, Y. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst. Rev. 2015, 2, Cd003793. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.S.; Waller, J.W.; Cook, R.M.; Cavalera, S.L.; Lim, W.T.; Osadnik, C.R. Effect of Pulmonary Rehabilitation on Symptoms of Anxiety and Depression in COPD: A Systematic Review and Meta-Analysis. Chest 2019, 156, 80–91. [Google Scholar] [CrossRef]
- Williams, M.T.; Johnston, K.N.; Paquet, C. Cognitive Behavioral Therapy for People with Chronic Obstructive Pulmonary Disease: Rapid Review. Int. J. Chronic Obstr. Pulm. Dis. 2020, 15, 903–919. [Google Scholar] [CrossRef] [Green Version]
- Maddocks, M.; Lovell, N.; Booth, S.; Man, W.D.; Higginson, I.J. Palliative care and management of troublesome symptoms for people with chronic obstructive pulmonary disease. Lancet 2017, 390, 988–1002. [Google Scholar] [CrossRef] [Green Version]
- Mechakra-Tahiri, S.D.; Freeman, E.E.; Haddad, S.; Samson, E.; Zunzunegui, M.V. The gender gap in mobility: A global cross-sectional study. BMC Public Health 2012, 12, 598. [Google Scholar] [CrossRef] [Green Version]
- Dal Negro, R.W.; Bonadiman, L.; Turco, P. Prevalence of different comorbidities in COPD patients by gender and GOLD stage. Multidiscip. Respir. Med. 2015, 10, 24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Walli-Attaei, M.; Joseph, P.; Rosengren, A.; Chow, C.K.; Rangarajan, S.; Lear, S.A.; AlHabib, K.F.; Davletov, K.; Dans, A.; Lanas, F.; et al. Variations between women and men in risk factors, treatments, cardiovascular disease incidence, and death in 27 high-income, middle-income, and low-income countries (PURE): A prospective cohort study. Lancet 2020, 396, 97–109. [Google Scholar] [CrossRef]
- Sarwar, M.R.; McDonald, V.M.; Abramson, M.J.; Paul, E.; George, J. Treatable traits in an English cohort: Prevalence and predictors of future decline in lung function and quality of life in COPD. ERJ Open Res. 2021, 7, 00934–02020. [Google Scholar] [CrossRef] [PubMed]
| Trait | Cut-Off | Reference(s) |
|---|---|---|
| Pulmonary traits | ||
| Severe hyperinflation | RV/TLC ≥ 0.58 | [33] |
| Limited diffusing capacity | DLCO < 60% predicted | [34] |
| Severe inspiratory muscle weakness | Pimax < 50% predicted | [35,36] |
| Frequent exacerbations | ≥2 previous year | [37] |
| Frequent hospital admission | ≥1 previous year | [37] |
| Extra-pulmonary traits | ||
| Extra-pulmonary-symptoms | ||
| Severe activity-related dyspnea | mMRC ≥ 2 | [38] |
| Severe fatigue | CIS-F ≥ 36 points | [39] |
| Symptoms of anxiety | HADS ≥ 8 points | [40] |
| Symptoms of depression | HADS ≥ 8 points | [40] |
| Extra-pulmonary–health status | ||
| Poor health status | CAT ≥ 18 points CCQ ≥ 1.9 points | [41] [41] |
| Extra-pulmonary-physical | ||
| Underweight Obese | BMI < 21 kg/m2 BMI > 30 kg/m2 | [42] |
| Low muscle mass | LMI < 10th percentile | [18] |
| High cardiovascular risk | Waist circumference ≥ 80 cm in women and ≥ 94 cm in men | [43] |
| Limited exercise capacity | 6MWD < 70% predicted CPET workmax < 70% predicted | [31] [44] [45] |
| Behavioral traits | ||
| Low physical activity | <5000 steps/day | [46] |
| Current smoking | N.A. | N.A. |
| Patients Referred to Secondary Care | Patients Referred to Tertiary Care | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Sample (n = 530) | Female (n = 265; 50%) | Male (n = 265; 50%) | p-Value | Total Sample (n = 2012) | Female (n = 1006; 50%) | Male (n = 1006; 50%) | p-Value | Between Total Samples p-Value | |
| Age, years | 63.3 ± 8.4 | 63.2 ± 8.4 | 63.3 ± 8.4 | 0.885 | 65.7 ± 7.9 | 65.6 ± 7.9 | 65.9 ± 8.0 | 0.330 | <0.001 * |
| 40–49, n (%) | 21 (4.0) | 11 (4.1) | 10 (3.8) | 0.820 | 49 (2.4) | 21 (2.1) | 28 (2.8) | 0.738 | <0.001 * |
| 50–59, n (%) | 160 (30.2) | 82 (30.9) | 78 (29.4) | 445 (22.1) | 230 (22.9) | 215 (21.4) | |||
| 60–69, n (%) | 215 (40.6) | 103 (38.9) | 112 (42.3) | 894 (44.4) | 451 (44.8) | 443 (44.0) | |||
| 70–79, n (%) | 119 (22.5) | 63 (23.8) | 56 (21.1) | 571 (28.4) | 278 (27.6) | 293 (29.1) | |||
| 80–89, n (%) | 15 (2.8) | 6 (2.3) | 9 (3.4) | 53 (2.6) | 26 (2.6) | 27 (2.7) | |||
| Pulmonary Traits | |||||||||
| FEV1% predicted | 55.2 [43.1–68.3] | 55.0 [43.0–68.3] | 55.7 [43.3–67.7] | 0.999 | 43.6 [32.1–59.5] | 43.6 [32.4–59.8] | 43.5 [31.6–59.2] | 0.733 | <0.001 * |
| GOLD 1, n (%) | 51 (9.6) | 23 (8.7) | 28 (10.5) | 0.649 | 118 (6.0) | 55 (5.6) | 64 (6.4) | 0.415 | <0.001 * |
| GOLD 2, n (%) | 273 (51.5) | 139 (52.5) | 134 (50.5) | 639 (32.2) | 324 (32.8) | 315 (31.6) | |||
| GOLD 3, n (%) | 197 (37.2) | 100 (37.7) | 97 (36.7) | 811 (40.9) | 415 (42.0) | 396 (39.8) | |||
| GOLD 4, n (%) | 9 (1.7) | 3 (1.1) | 6 (2.3) | 416 (21.0) | 195 (19.7) | 221 (22.2) | |||
| FVC, % predicted | 92.1 ± 17.1 | 91.8 ± 16.6 | 92.3 ± 17.6 | 0.755 | 94.7 ± 21.4 | 94.1 ± 21.6 | 95.3 ± 21.2 | 0.200 | 0.003 * |
| FEV1/FVC | 48.6 ± 11.9 | 49.8 ± 12.3 | 47.5 ± 11.4 | 0.024 * | 38.5 ± 12.5 | 39.1 ± 11.8 | 37.9 ± 13.1 | 0.003 * | <0.001 * |
| ITGV, % predicted | N.A. | N.A. | N.A. | N.A. | 148.4 [121.7–175.7] | 152.8 [129.8–180.6] | 142.9 [114.1–170.7] | <0.001 * | N.A. |
| ERV, % predicted | N.A. | N.A. | N.A. | N.A. | 111.7 [84.8–141.1] | 109.7 [84.1–140.0] | 114.6 [86.1–142.2] | 0.122 | N.A. |
| RV, % predicted | N.A. | N.A. | N.A. | N.A. | 158.9 [123.8–197.3] | 166.2 [134.3–202.4] | 151.7 [115.5–190.0] | <0.001 * | N.A. |
| TLC, % predicted | N.A. | N.A. | N.A. | N.A. | 117.6 [104.8–130.0] | 123.1 [110.2–134.3] | 112.7 [100.2–125.1] | <0.001 * | N.A. |
| RV/TLC, % | N.A. | N.A. | N.A. | N.A. | 53.2 ± 11.5 | 56.2 ± 11.1 | 50.3 ± 11.1 | <0.001 * | N.A. |
| RV/TLC ≥ 0.58, n (%) | N.A. | N.A. | N.A. | N.A. | 663 (34.1) | 414 (43.0) | 249 (25.4) | <0.001 * | N.A. |
| DLCO, % predicted | N.A. | N.A. | N.A. | N.A. | 47.8 [37.8–60.3] | 46.0 [37.1–57.2] | 49.7 [38.6–63.4] | <0.001 * | N.A. |
| DLCO < 60% | N.A. | N.A. | N.A. | N.A. | 1383 (74.7) | 712 (79.6) | 671 (70.1) | <0.001 * | N.A. |
| Kco, % predicted | N.A. | N.A. | N.A. | N.A. | 60.2 [48.7–78.1] | 57.1 [47.3–73.7] | 63.7 [50.6–83.0] | <0.001 * | N.A. |
| Pimax, cmH2O | N.A. | N.A. | N.A. | N.A. | 68.6 ± 21.7 | 61.4 ± 19.2 | 75.9 ± 21.6 | <0.001 * | N.A. |
| Pimax, % predicted | N.A. | N.A. | N.A. | N.A. | 78.9 ± 24.4 | 86.9 ± 26.1 | 71.0 ± 19.6 | <0.001 * | N.A. |
| Pimax < 50% predicted | N.A. | N.A. | N.A. | N.A. | 226 (11.4) | 81 (8.2) | 145 (14.6) | <0.001 * | N.A. |
| AECOPD past 12 months, n a | 0.0 [0.0–1.0] | 1.0 [0.0–2.0] | 0.0 [0.0–1.0] | 0.063 | 2.0 [1.0–4.0] | 2.0 [1.0–4.0] | 2.0 [1.0–4.0] | <0.001 * | <0.001 * |
| ≥2 AECOPD, n (%) a | 114 (25.0) | 68 (30.5) | 46 (19.7) | 0.008 * | 1241 (62.1) | 669 (66.8) | 572 (57.4) | <0.001 * | <0.001 * |
| Hospitalisations due to COPD previous 12 months, n a | 0.0 [0.0–0.0] | 0.0 [0.0–0.0] | 0.0 [0.0–0.0] | 0.086 | 0.0 [0.0–1.0] | 0.0 [0.0–1.0] | 0.0 [0.0–1.0] | 0.021 * | <0.001 * |
| ≥1 hospitalisations, n (%) a | 31 (7.3) | 18 (8.8) | 13 (6.0) | 0.267 | 890 (44.5) | 475 (47.5) | 415 (41.6) | 0.008 * | <0.001 * |
| GOLD groups (A-D), n (%) | |||||||||
| GOLD A | 42 (12.6) | 71 (40.3) | 104 (53.1) | 0.031 * | 24 (1.2) | 7 (0.7) | 17 (1.7) | <0.001 * | <0.001 * |
| GOLD B | 110 (32.9) | 49 (27.9) | 51 (26.0) | 301 (15.0) | 130 (12.9) | 171 (17.0) | |||
| GOLD C | 30 (9.0) | 22 (12.5) | 21 (10.7) | 53 (2.6) | 18 (1.8) | 35 (3.5) | |||
| GOLD D | 152 (45.5) | 34 (19.3) | 20 (10.2) | 1631 (81.2) | 850 (84.6) | 781 (77.8) | |||
| LTOT, n (%) | N.A. | N.A. | N.A. | N.A. | 412 (21.0) | 233 (23.8) | 179 (18.3) | <0.001 * | N.A. |
| Patients Referred to Secondary Care | Patients Referred to Tertiary Care | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Sample (n = 530) | Female (n = 265; 50%) | Male (n = 265; 50%) | p-Value | Total Sample (n = 2012) | Female (n = 1006; 50%) | Male (n = 1006; 50%) | p-Value | Between Total Samples p-Value | |
| Extra-Pulmonary Traits-Symptoms | |||||||||
| mMRC, score a | 1.0 [0.0–2.0] | 2.0 [1.0–2.0] | 1.0 [0.0–2.0] | <0.001 * | 2.0 [2.0–3.0] | 2.0 [2.0–3.0] | 2.0 [2.0–3.0] | 0.006 * | <0.001 * |
| mMRC ≥2 points a | 197 (42.7) | 116 (50.9) | 81 (34.8) | <0.001 * | 1737 (87.0) | 889 (89.1) | 848 (85.0) | 0.006 * | <0.001 * |
| CIS-F, score a | 37.0 [27.0–47.0] | 37.0 [28.0–47.0] | 37.0 [26.0–47.0] | 0.604 | N.A. | N.A. | N.A. | N.A. | N.A. |
| CIS-F score < 36 | 182 (47.4) | 86 (46.7) | 96 (48.0) | 0.805 | N.A. | N.A. | N.A. | N.A. | N.A. |
| CIS-F score ≥ 36 | 202 (52.6) | 98 (53.3) | 104 (52.0) | N.A. | N.A. | N.A. | N.A. | N.A. | |
| HADS, anxiety score | N.A. | N.A. | N.A. | N.A. | 7.0 [4.0–11.0] | 8.0 [5.0–11.0] | 7.0 [4.0–10.0] | <0.001 * | N.A. |
| HADS, anxiety score ≥ 8 points | N.A. | N.A. | N.A. | N.A. | 941 (49.2) | 544 (56.3) | 397 (42.0) | <0.001 * | N.A. |
| HADS, depression score | N.A. | N.A. | N.A. | N.A. | 7.0 [4.0–10.0] | 8.0 [4.0–10.0] | 7.0 [4.0–10.0] | 0.002 * | N.A. |
| HADS, depression score ≥ 8 points | N.A. | N.A. | N.A. | N.A. | 909 (47.6) | 486 (50.3) | 423 (44.8) | 0.015 * | N.A. |
| Extra-Pulmonary Traits–Health Status | |||||||||
| CAT, score | N.A. | N.A. | N.A. | N.A. | 22.0 [18.0–26.0] | 23.0 [19.0–27.0] | 21.0 [16.0–25.0] | <0.001 * | N.A. |
| CAT ≥18 points | N.A. | N.A. | N.A. | N.A. | 1448 (75.5) | 773 (79.9) | 675 (71.0) | <0.001 * | N.A. |
| CCQ, score | |||||||||
| CCQ symptoms | 2.5 [1.5–3.3] | 2.3 [1.5–3.3] | 2.5 [1.5–3.3] | 0.232 | N.A. | N.A. | N.A. | N.A. | N.A. |
| CCQ functional state | 1.8 [1.0–3.0] | 1.8 [1.0–3.2] | 1.8 [1.0–3.0] | 0.387 | N.A. | N.A. | N.A. | N.A. | N.A. |
| CCQ mental state | 1.0 [0.0–2.0] | 1.0 [0.0–2.5] | 1.0 [0.0–2.0] | 0.269 | N.A. | N.A. | N.A. | N.A. | N.A. |
| CCQ, total score | 1.8 [1.2–2.9] | 1.9 [1.2–2.9] | 1.8 [1.2–2.9] | 0.515 | N.A. | N.A. | N.A. | N.A. | N.A. |
| CCQ, total score ≥ 1.9 | 237 (49.5) | 123 (51.5) | 114 (47.5) | 0.386 | N.A. | N.A. | N.A. | N.A. | N.A. |
| Extra-Pulmonary Traits–Physical | |||||||||
| BMI, Kg/m2 | 25.2 ± 4.6 | 25.2 ± 4.6 | 25.2 ± 4.5 | 0.901 | 25.4 [21.8–29.4] | 25.1 [21.5–29.3] | 25.6 [22.1–29.6] | 0.078 | 0.049 * |
| BMI < 21, n (%) | 98 (18.5) | 51 (19.2) | 47 (17.7) | 0.811 | 409 (20.3) | 219 (21.8) | 190 (18.9) | 0.275 | <0.001 * |
| BMI > 30, n (%) | 77 (14.5) | 40 (15.1) | 37 (14.0) | 451 (22.4) | 222 (22.1) | 229 (22.8) | |||
| Total body fat, Kg | N.A. | N.A. | N.A. | N.A. | 25.4 [18.2–33.3] | 26.0 [18.7–34.6] | 24.8 [17.7–31.9] | 0.002 * | N.A. |
| Bone mass content, Kg | N.A. | N.A. | N.A. | N.A. | 23.1 [19.3–27.4] | 19.4 [17.4–21.8] | 27.2 [24.5–30.4] | <0.001 * | N.A. |
| Fat-free mass, Kg | N.A. | N.A. | N.A. | N.A. | 45.8 [39.0–53.5] | 39.2 [35.8–43.1] | 53.2 [48.3–58.7] | <0.001 * | N.A. |
| LMI, Kg/m2 | N.A. | N.A. | N.A. | N.A. | 15.4 [13.8–17.3] | 14.2 [13.1–15.5] | 16.8 [15.4–18.5] | <0.001 * | N.A. |
| LMI < 10th percentile, n (%) | N.A. | N.A. | N.A. | N.A. | 524 (26.0) | 255 (25.3) | 269 (26.7) | 0.477 | N.A. |
| Waist circumference, cm a | 96.6 ± 12.9 | 93.0 ± 12.0 | 99.9 ± 12.9 | <0.001 * | N.A. | N.A. | N.A. | N.A. | N.A. |
| Waist circumference, ≥80 cm women, ≥94 cm men | 324 (76.6) | 177 (88.1) | 147 (66.2) | <0.001 * | N.A. | N.A. | N.A. | N.A. | N.A. |
| Use of walking aid, n (%) | N.A. | N.A. | N.A. | N.A. | 723 (36.4) | 437 (44.0) | 286 (28.7) | <0.001 * | N.A. |
| 6MWD, m | 450.0 [372.0–512.0] | 420.0 [355.0–491.0] | 479.0 [400.0–530.0] | <0.001 * | 395.0 [313.5–467.0] | 375.0 [295.0–441.0] | 415.0 [339.5–486.5] | <0.001 * | <0.001 * |
| 6MWD, % predicted | 69.0 [60.0–77.7] | 69.5 [61.4–76.6] | 68.7 [78.6] | 0.811 | 64.0 [51.0–74.0] | 66.0 [53.0–76.0] | 62.0 [50.0–72.0] | <0.001 * | <0.001 * |
| 6MWD < 70% predicted | 284 (53.6) | 142 (53.6) | 142 (53.6) | 1.000 | 1276 (64.4) | 589 (59.6) | 687 (69.1) | <0.001 * | <0.001 * |
| CPET Workmax, Watts | N.A. | N.A. | N.A. | N.A. | 60.0 [43.0–81.0] | 51.0 [38.0–67.0] | 70.0 [51.0–93.5] | <0.001 * | N.A. |
| CPET Workmax, % predicted | N.A. | N.A. | N.A. | N.A. | 45.0 [34.0–58.0] | 50.0 [38.0–64.0] | 41.0 [31.0–52.0] | <0.001 * | N.A. |
| Workmax, <70% predicted | N.A. | N.A. | N.A. | N.A. | 1627 (88.1) | 752 (82.5) | 875 (93.5) | <0.001 * | N.A. |
| CWRT, Workmax, Wattsa | N.A. | N.A. | N.A. | N.A. | 46.0 [33.0–61.0] | 39.0 [29.0–50.0] | 52.0 [29.0–70.0] | <0.001 * | N.A. |
| CWRT time cycled, s a | N.A. | N.A. | N.A. | N.A. | 215.0 [160.0–303.0] | 200.0 [152.0–274.0] | 235.0 [169.0–335.0] | <0.001 * | N.A. |
| 1 RM Leg extension, Kg | N.A. | N.A. | N.A. | N.A. | 27.5 [20.0–37.5] | 22.5 [15.0–30.0] | 35.0 [25.0–45.0] | <0.001 * | N.A. |
| 1 RM Leg press, Kg | N.A. | N.A. | N.A. | N.A. | 70.0 [50.0–100.0] | 50.0 [30.0–70.0] | 90.0 [60.0–120.0] | <0.001 * | N.A. |
| Behavioural Traits | |||||||||
| Smoking status, n (%) | |||||||||
| Former smoker | 90 (17.5) | 50 (19.5) | 40 (15.4) | 0.187 | 1442 (72.0) | 726 (72.5) | 716 (71.4) | 0.346 | <0.001 * |
| Current smoker | 229 (44.5) | 118 (46.1) | 111 (42.9) | 492 (24.6) | 246 (24.6) | 246 (24.5) | |||
| Never smoker | 196 (38.1) | 88 (34.4) | 108 (41.7) | 70 (3.5) | 29 (2.8) | 41 (4.0) | |||
| Pack-years, n | N.A. | N.A. | N.A. | N.A. | 40.0 [30.0–52.0] | 40.0 [28.0–50.0] | 44.0 [30.0–60.0] | <0.001 * | N.A. |
| Steps per day, n | 5008.0 [3043.67–7433.80] | 4795.0 [2842.50–7200.0] | 5118.67 [3138.0–7782.0] | 0.159 | N.A. | N.A. | N.A. | N.A. | N.A. |
| Steps per day < 5000 | 264 (49.8) | 138 (52.1) | 126 (47.5) | 0.297 | N.A. | N.A. | N.A. | N.A. | N.A. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Souto-Miranda, S.; van ‘t Hul, A.J.; Vaes, A.W.; Antons, J.C.; Djamin, R.S.; Janssen, D.J.A.; Franssen, F.M.E.; Marques, A.; Spruit, M.A. Differences in Pulmonary and Extra-Pulmonary Traits between Women and Men with Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2022, 11, 3680. https://doi.org/10.3390/jcm11133680
Souto-Miranda S, van ‘t Hul AJ, Vaes AW, Antons JC, Djamin RS, Janssen DJA, Franssen FME, Marques A, Spruit MA. Differences in Pulmonary and Extra-Pulmonary Traits between Women and Men with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine. 2022; 11(13):3680. https://doi.org/10.3390/jcm11133680
Chicago/Turabian StyleSouto-Miranda, Sara, Alex J. van ‘t Hul, Anouk W. Vaes, Jeanine C. Antons, Remco S. Djamin, Daisy J. A. Janssen, Frits M. E. Franssen, Alda Marques, and Martijn A. Spruit. 2022. "Differences in Pulmonary and Extra-Pulmonary Traits between Women and Men with Chronic Obstructive Pulmonary Disease" Journal of Clinical Medicine 11, no. 13: 3680. https://doi.org/10.3390/jcm11133680
APA StyleSouto-Miranda, S., van ‘t Hul, A. J., Vaes, A. W., Antons, J. C., Djamin, R. S., Janssen, D. J. A., Franssen, F. M. E., Marques, A., & Spruit, M. A. (2022). Differences in Pulmonary and Extra-Pulmonary Traits between Women and Men with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine, 11(13), 3680. https://doi.org/10.3390/jcm11133680






