Microtia Ear Reconstruction with Patient-Specific 3D Models—A Segmentation Protocol
Abstract
1. Introduction
2. Materials and Methods
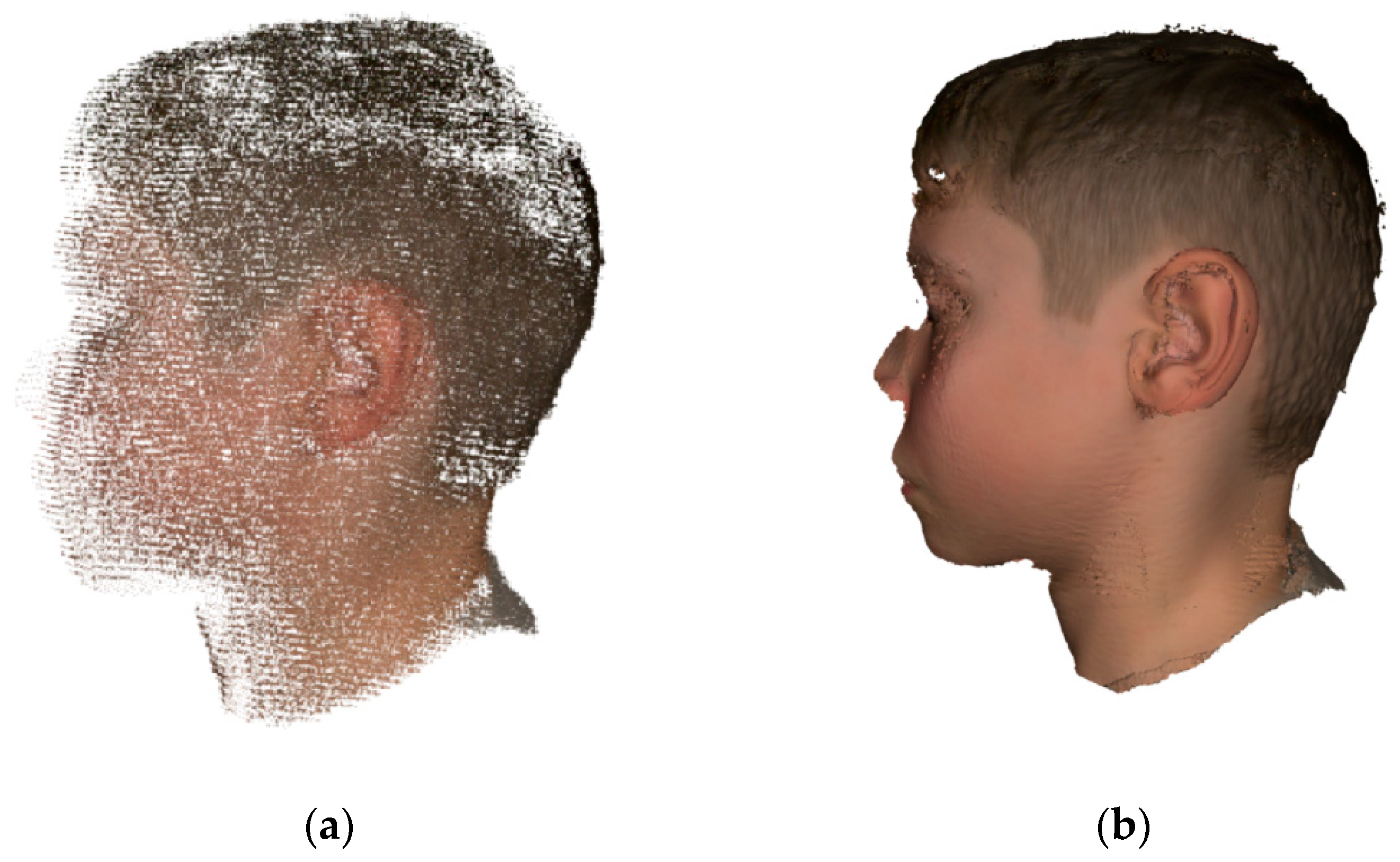
2.1. Surface Scanning of Auricles
2.2. Digital Models Preparation
2.3. 3D Printing of the Models
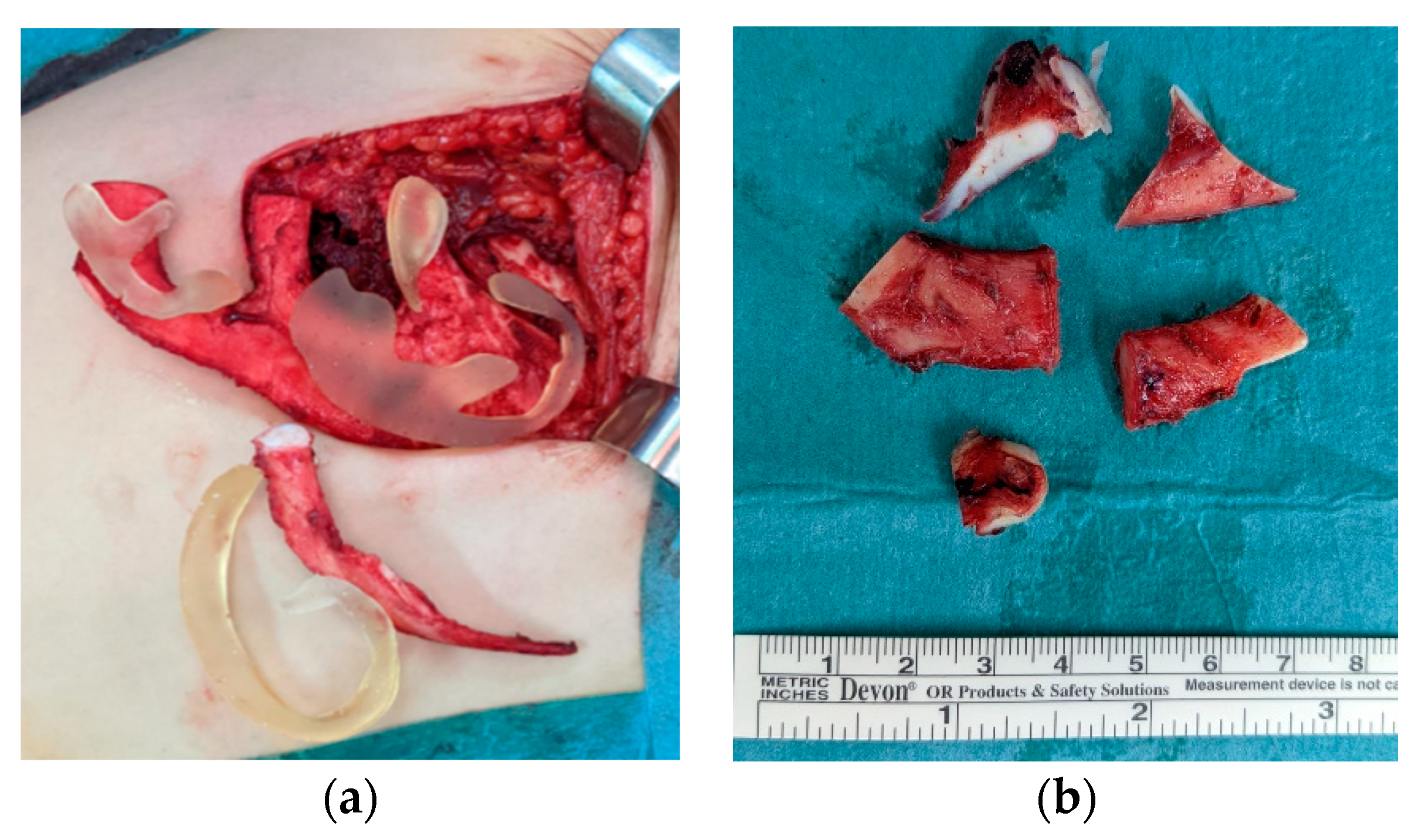
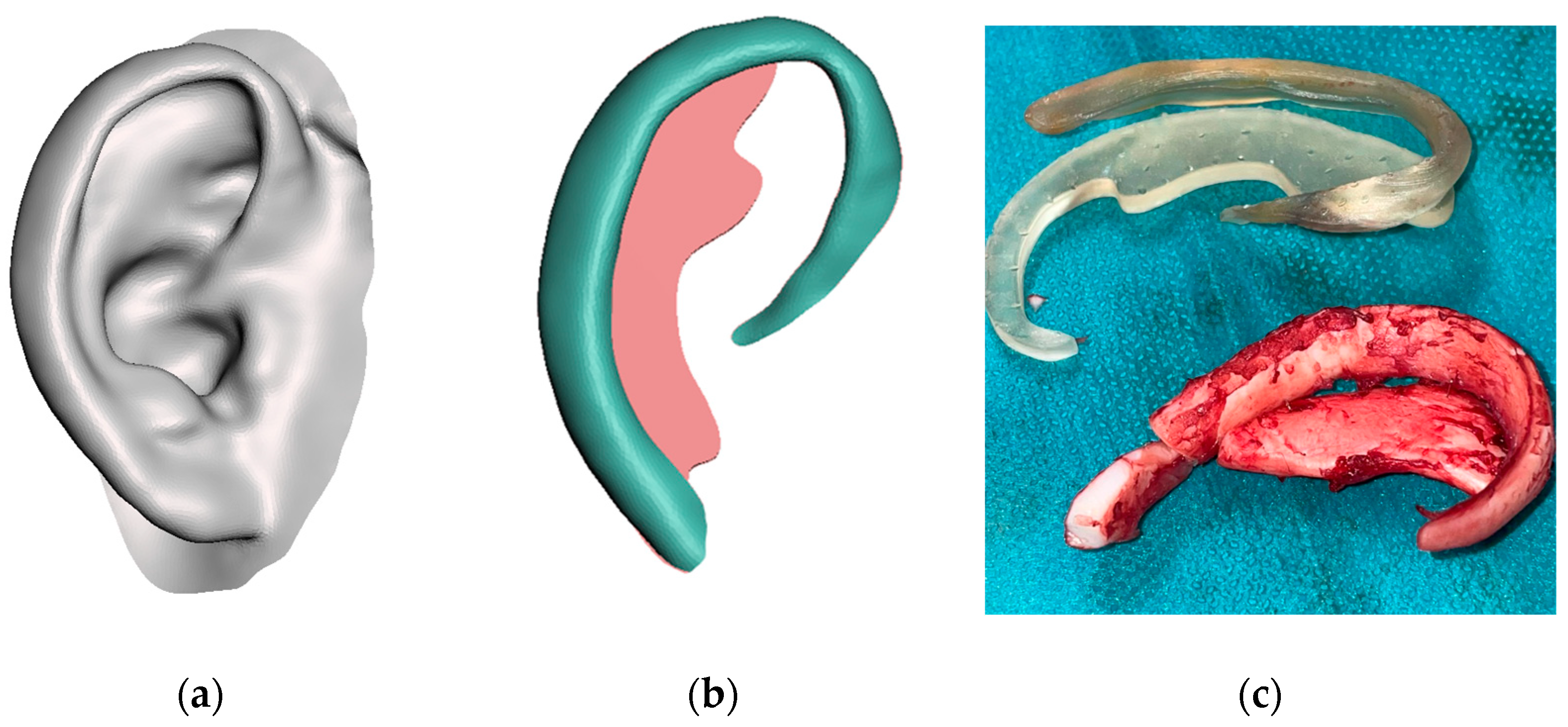
2.4. Framework Fabrication
3. Results
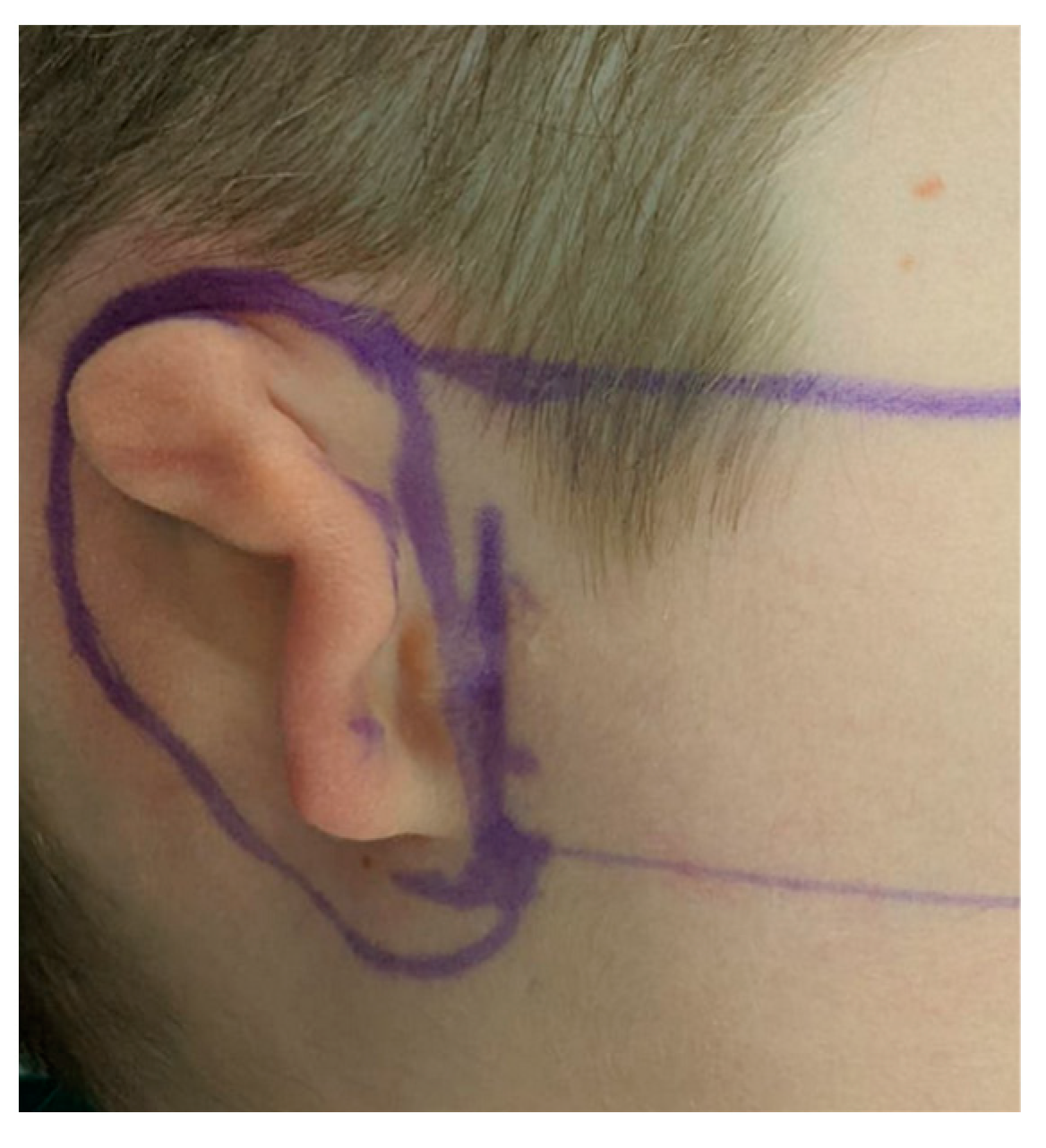
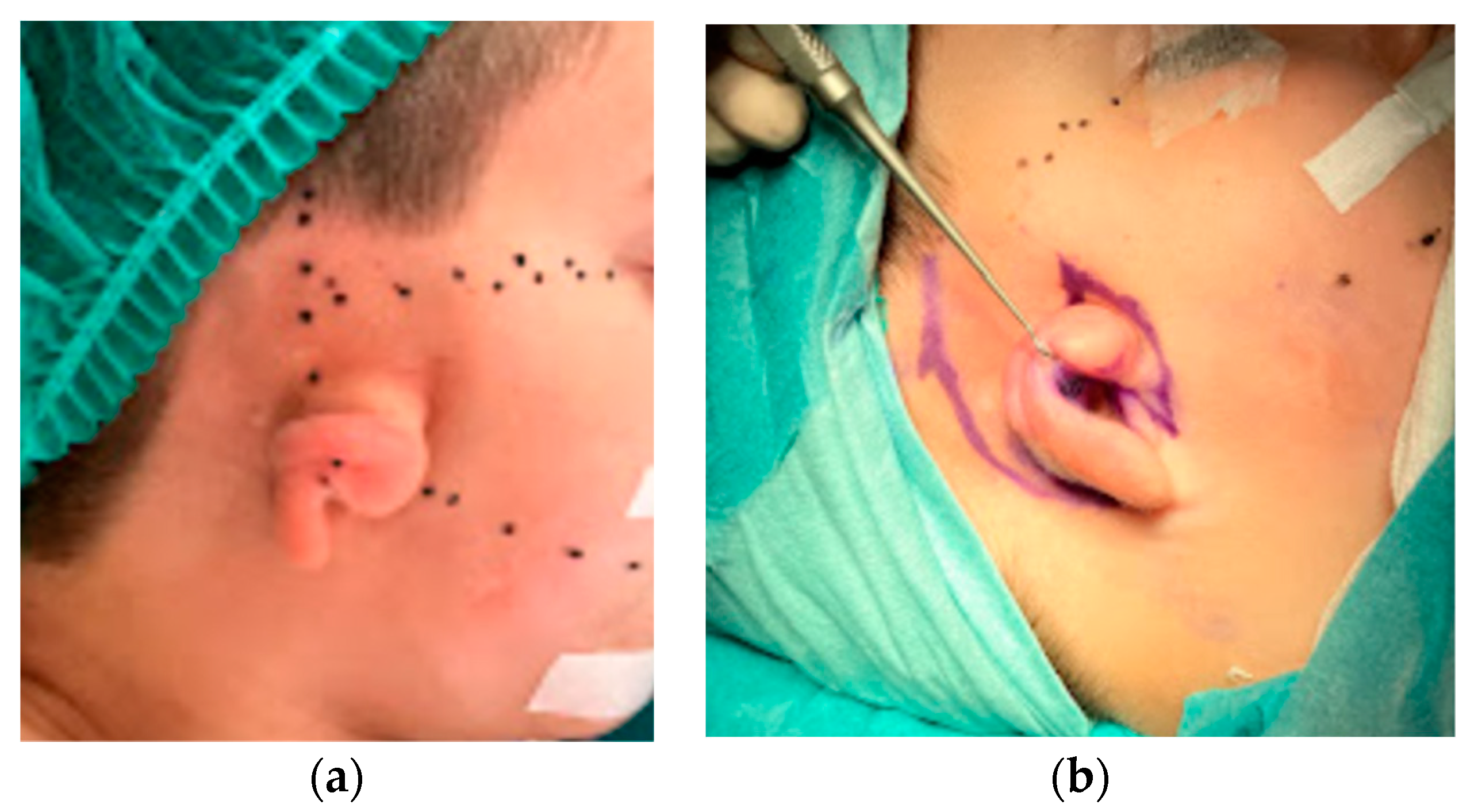
3.1. Case Report: Case 1
3.2. Case Reports: Case 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luquetti, D.V.; Leoncini, E.; Mastroiacovo, P. Microtia-anotia: A global review of prevalence rates. Birth Defects Res. A Clin. Mol. Teratol. 2011, 91, 813–822. [Google Scholar] [CrossRef] [PubMed]
- Zeng, W.; Lin, F.; Shi, T.; Zhang, R.; Nian, Y.; Ruan, J.; Zhou, T. Fused deposition modelling of an auricle framework for microtia reconstruction based on CT images. Rapid Prototyp. J. 2008, 14, 280–284. [Google Scholar] [CrossRef]
- Nagata, S. Total auricular reconstruction with a three-dimensional costal cartilage framework. Ann. Chirgugerie Plast. Esthetique. 1995, 40, 371–399. [Google Scholar]
- Tanzer, R.C. Total reconstruction of the external ear. Ann. Plast. Surg. 1983, 10, 76–85. [Google Scholar] [CrossRef]
- Nagata, S. Modification of the stages in total reconstruction of the auricle: Part III. Grafting the three-dimensional costal cartilage framework for small concha-type microtia. Plast. Reconstr. Surg. 1994, 93, 243–268. [Google Scholar] [CrossRef]
- Firmin, F. State-of-the-art autogenous ear reconstruction in cases of microtia. Adv. Otorhinolaryngol. 2010, 68, 25–52. [Google Scholar] [CrossRef]
- Yotsuyanagi, T.; Yamashita, K.; Yamauchi, M.; Nakagawa, T.; Sugai, A.; Kato, S.; Gonda, A.; Suzuki, A.; Onuma, M. Establishment of a Standardized Technique for Concha-type Microtia-How to Incorporate the Cartilage Frame into the Remnant Ear. Plast. Reconstr. Surg. Glob. Open 2019, 7, e2337. [Google Scholar] [CrossRef]
- Fan, X.; Niu, X.; Wang, Y.; Chen, Y.; Fan, Y.; Wang, J.; Chen, X. Comparison of three-dimensional and two-dimensional templates on auricle reconstruction in patients with unilateral microtia. Am. J. Transl. Res. 2019, 11, 3771–3778. [Google Scholar] [PubMed]
- Flores, R.L.; Liss, H.; Raffaelli, S.; Humayun, A.; Khouri, K.S.; Coelho, P.G.; Witek, L. The technique for 3D printing patient-specific models for auricular reconstruction. J. Craniomaxillofac. Surg. 2017, 45, 937–943. [Google Scholar] [CrossRef]
- Duan, W.; Liu, Y. Correction of Tanzer Type IIB Constricted Ears via Z-shaped Double V-Y Advancement Flaps. Ann. Plast. Surg. 2019, 82, 284–288. [Google Scholar] [CrossRef]
- Kelley, T.F.; Moulton-Barrett, R.; Dugan, F.M.; Crumley, R.L. The use of 3-dimensional models in auricular reconstruction. Arch. Otolaryngol.-Head Neck Surg. 1998, 124, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Liacouras, P.; Garnes, J.; Roman, N.; Petrich, A.; Grant, G.T. Designing and manufacturing an auricular prosthesis using computed tomography, 3-dimensional photographic imaging, and additive manufacturing: A clinical report. J. Prosthet. Dent. 2011, 105, 78–82. [Google Scholar] [CrossRef]
- Liu, Y.; Lu, G.; Zhang, D. An Effective 3D Ear Acquisition System. PLoS ONE 2015, 10, e0129439. [Google Scholar] [CrossRef][Green Version]
- Zhou, J.; Pan, B.; Yang, Q.; Zhao, Y.; Leren, H.; Lin, L.; Sun, H.; Song, Y.; Yu, X.; Sun, Z.; et al. Three-dimensional autologous cartilage framework fabrication assisted by new additive manufactured ear-shaped templates for microtia reconstruction. Plast. Reconstr. Aesthet. Surg. 2016, 69, 1436–1444. [Google Scholar] [CrossRef] [PubMed]
- Buchberger, B.; Scholl, K.; Krabbe, L.; Spiller, L.; Lux, B. Radiation exposure by medical X-ray applications. Ger Med. Sci. 2022, 20, Doc06. [Google Scholar] [CrossRef]
- Ross, M.T.; Cruz, R.; Brooks-Richards, T.; Hafner, L.M.; Powell, S.K.; Woodruff, M.A. Smartphones for frugal three-dimensional scanning of the external ear with application to microtia⋆. J. Plast. Reconstr. Aesthet. Surg. 2018, 71, 1362–1380. [Google Scholar] [CrossRef]
- You, P.; Liu, Y.-C.C.; Silva, R.C. Fabrication of 3D Models for Microtia Reconstruction Using Smartphone-Based Technology. Ann. Otol. Rhinol. Laryngol. 2021, 131, 373–378. [Google Scholar] [CrossRef]
- Othman, S.A.; Saffai, L.; Hassan, W.N.W. Validity and reproducibility of the 3D VECTRA photogrammetric surface imaging system for the maxillofacial anthropometric measurement on cleft patients. Clin. Oral Investig. 2019, 24, 2853–2866. [Google Scholar] [CrossRef]
- Ronde, E.M.; Esposito, M.; Lin, Y.; van Etten-Jamaludin, F.S.; Bulstrode, N.W.; Breugem, C.C. Long-term aesthetics, patient-reported outcomes, and auricular sensitivity after microtia reconstruction: A systematic review. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 3213–3234. [Google Scholar] [CrossRef]
- Cao, Y.; Vacanti, J.P.; Paige, K.T.; Upton, J.; Vacanti, C.A. Transplantation of chondrocytes utilizing a polymer-cell construct to produce tissue-engineered cartilage in the shape of a human ear. Plast. Reconstr. Surg. 1997, 100, 297–304. [Google Scholar] [CrossRef]
- Jia, L.; Hua, Y.; Zeng, J.; Liu, W.; Wang, D.; Zhou, G.; Liu, X.; Jiang, H. Bioprinting and regeneration of auricular cartilage using a bioactive bioink based on microporous photocrosslinkable acellular cartilage matrix. Bioact. Mater. 2022, 16, 66–81. [Google Scholar] [CrossRef] [PubMed]
- Zhou, G.; Jiang, H.; Yin, Z.; Liu, Y.; Zhang, Q.; Zhang, C.; Pan, B.; Zhou, J.; Zhou, X.; Sun, H.; et al. In Vitro Regeneration of Patient-specific Ear-shaped Cartilage and Its First Clinical Application for Auricular Reconstruction. EBioMedicine 2018, 28, 287–302. [Google Scholar] [CrossRef] [PubMed]
- Mussi, E.; Servi, M.; Facchini, F.; Volpe, Y.; Furferi, R. A rapid prototyping approach for custom training of autologous ear reconstruction. Int. J. Interact. Des. Manuf. 2021, 15, 577–585. [Google Scholar] [CrossRef]
- Mussi, E.; Servi, M.; Facchini, F.; Furferi, R.; Governi, L.; Volpe, Y. A novel ear elements segmentation algorithm on depth map images. Comput. Biol. Med. 2021, 129, 104157. [Google Scholar] [CrossRef] [PubMed]
- Facchini, F.; Morabito, A.; Buonamici, F.; Mussi, E.; Servi, M.; Volpe, Y. Autologous Ear Reconstruction: Towards a Semiautomatic CAD-Based Procedure for 3D Printable Surgical Guides. In CAD’20 Proceedings-Presentations; CAD Solutions LLC: El Paso, TX, USA, 2020. [Google Scholar] [CrossRef]
- Nilsson, J.; Hindocha, N. Time matters-differences between computer-assisted surgery and conventional planning in cranio-maxillofacial surgery: A systematic review and meta-analysis. J. Cranio-Maxillofac. Surg. 2019, 48, 132–140. [Google Scholar] [CrossRef]
- Cheng, H. Prolonged operative duration is associated with complications: A systematic review and meta-analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef]





Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez-Arias, J.P.; Gutiérrez Venturini, A.; Pampín Martínez, M.M.; Gómez García, E.; Muñoz Caro, J.M.; San Basilio, M.; Martín Pérez, M.; Cebrián Carretero, J.L. Microtia Ear Reconstruction with Patient-Specific 3D Models—A Segmentation Protocol. J. Clin. Med. 2022, 11, 3591. https://doi.org/10.3390/jcm11133591
Rodríguez-Arias JP, Gutiérrez Venturini A, Pampín Martínez MM, Gómez García E, Muñoz Caro JM, San Basilio M, Martín Pérez M, Cebrián Carretero JL. Microtia Ear Reconstruction with Patient-Specific 3D Models—A Segmentation Protocol. Journal of Clinical Medicine. 2022; 11(13):3591. https://doi.org/10.3390/jcm11133591
Chicago/Turabian StyleRodríguez-Arias, Juan Pablo, Alessandro Gutiérrez Venturini, Marta María Pampín Martínez, Elena Gómez García, Jesús Manuel Muñoz Caro, Maria San Basilio, Mercedes Martín Pérez, and José Luis Cebrián Carretero. 2022. "Microtia Ear Reconstruction with Patient-Specific 3D Models—A Segmentation Protocol" Journal of Clinical Medicine 11, no. 13: 3591. https://doi.org/10.3390/jcm11133591
APA StyleRodríguez-Arias, J. P., Gutiérrez Venturini, A., Pampín Martínez, M. M., Gómez García, E., Muñoz Caro, J. M., San Basilio, M., Martín Pérez, M., & Cebrián Carretero, J. L. (2022). Microtia Ear Reconstruction with Patient-Specific 3D Models—A Segmentation Protocol. Journal of Clinical Medicine, 11(13), 3591. https://doi.org/10.3390/jcm11133591





