Maternal Race and Stillbirth: Cohort Study and Systematic Review with Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Fetal Medicine Foundation Study
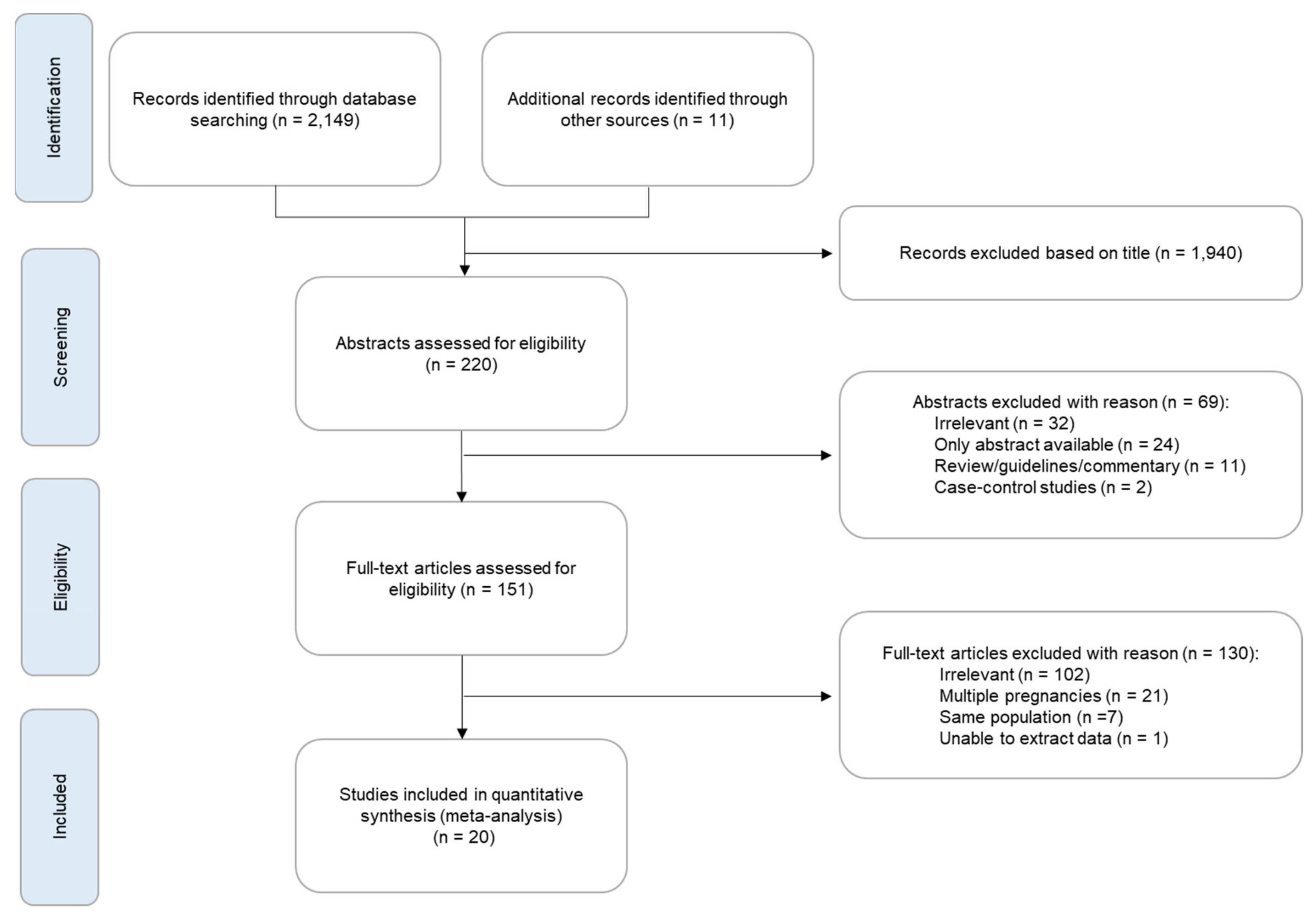
2.2. Systematic Review and Meta-Analysis
3. Results
3.1. Fetal Medicine Foundation Study
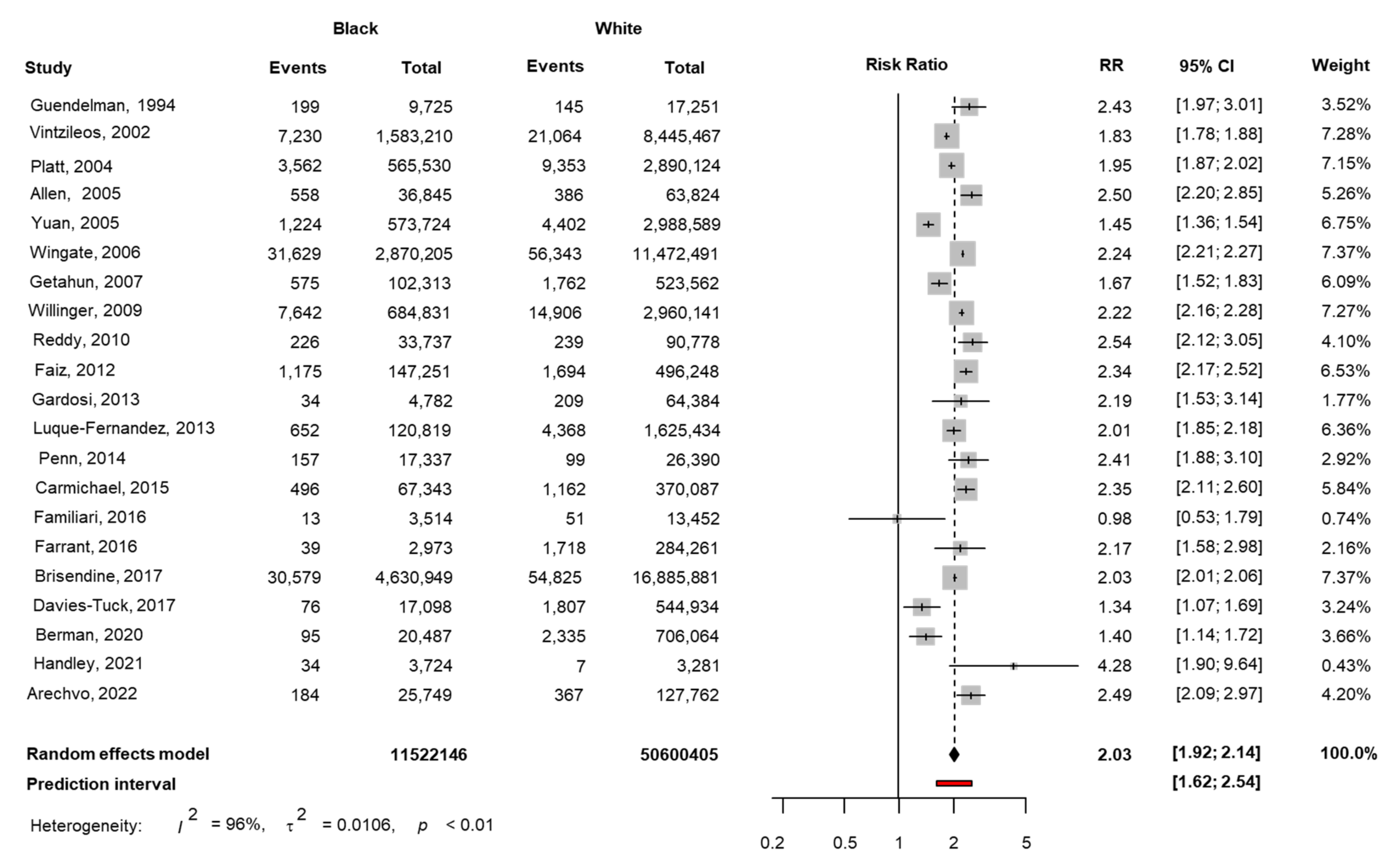
3.2. Systematic Review and Meta-Analysis
4. Discussion
4.1. Main Findings
4.2. Interpretation of Results and Implications for Clinical Practice
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hug, L.; You, D.; Blencowe, H.; Mishra, A.; Wang, Z.; Fix, M.J.; Wakefield, J.; Moran, A.C.; Gaigbe-Togbe, V.; Suzuki, E.; et al. UN Inter-agency Group for Child Mortality Estimation and its Core Stillbirth Estimation Group. Global, regional, and national estimates and trends in stillbirths from 2000 to 2019: A systematic assessment. Lancet 2021, 398, 772–785. [Google Scholar] [CrossRef]
- Guendelman, S.; Chavez, G.; Christianson, R. Fetal deaths in Mexican-American, black, and white non-Hispanic women seeking government-funded prenatal care. J. Commun. Health 1994, 19, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Vintzileos, A.M.; Ananth, C.V.; Smulian, J.C.; Scorza, W.E.; Knuppel, R.A. Prenatal care and black-white fetal death disparity in the United States: Heterogeneity by high-risk conditions. Obstet. Gynecol. 2002, 99, 483–489. [Google Scholar] [CrossRef] [PubMed]
- Platt, R.W.; Joseph, K.S.; Ananth, C.V.; Grondines, J.; Abrahamowicz, M.; Kramer, M.S. A proportional hazards model with time-dependent covariates and time-varying effects for analysis of fetal and infant death. Am. J. Epidemiol. 2004, 160, 199–206. [Google Scholar] [CrossRef]
- Allen, C.L.; Hulsey, T.M.; Hulsey, T.C. The influence of race on fetal outcome. Am. J. Perinatol. 2005, 22, 245–248. [Google Scholar] [CrossRef]
- Yuan, H.; Platt, R.W.; Morin, L.; Joseph, K.S.; Kramer, M.S. Fetal deaths in the United States, 1997 vs. 1991. Am. J. Obstet. Gynecol. 2005, 193, 489–495. [Google Scholar] [CrossRef] [Green Version]
- Wingate, M.S.; Alexander, G.R. Racial and ethnic differences in perinatal mortality: The role of fetal death. Ann. Epidemiol. 2006, 16, 485–491. [Google Scholar] [CrossRef]
- Getahun, D.; Ananth, C.V.; Kinzler, W.L. Risk factors for antepartum and intrapartum stillbirth: A population-based study. Am. J. Obstet. Gynecol. 2007, 196, 499–507. [Google Scholar]
- Willinger, M.; Ko, C.W.; Reddy, U.M. Racial disparities in stillbirth risk across gestation in the United States. Am. J. Obstet. Gynecol. 2009, 201, 469. [Google Scholar] [CrossRef] [Green Version]
- Reddy, U.M.; Laughon, S.K.; Sun, L.; Troendle, J.; Willinger, M.; Zhang, J. Prepregnancy risk factors for antepartum stillbirth in the United States. Obstet. Gynecol. 2010, 116, 1119–1126. [Google Scholar] [CrossRef] [Green Version]
- Faiz, A.S.; Demissie, K.; Rich, D.Q.; Kruse, L.; Rhoads, G.G. Trends and risk factors of stillbirth in New Jersey 1997–2005. J. Matern. Fetal. Neonatal. Med. 2012, 25, 699–705. [Google Scholar] [CrossRef]
- Gardosi, J.; Madurasinghe, V.; Williams, M.; Malik, A.; Francis, A. Maternal and fetal risk factors for stillbirth: Population based study. BMJ 2013, 346, f108. [Google Scholar] [CrossRef] [Green Version]
- Luque-Fernandez, M.A.; Franco, M.; Gelaye, B.; Schomaker, M.; Garitano, I.G.; D’Este, C.; Williams, M.A. Unemployment and stillbirth risk among foreign-born and Spanish pregnant women in Spain, 2007–2010: A multilevel analysis study. Eur. J. Epidemiol. 2013, 28, 991–999. [Google Scholar] [CrossRef]
- Penn, N.; Oteng-Ntim, E.; Oakley, L.L.; Doyle, P. Ethnic variation in stillbirth risk and the role of maternal obesity: Analysis of routine data from a London maternity unit. BMC Pregnancy Childbirth 2014, 14, 404. [Google Scholar] [CrossRef] [Green Version]
- Carmichael, S.L.; Blumenfeld, Y.J.; Mayo, J.; Wei, E.; Gould, J.B.; Stevenson, D.K.; Shaw, G.M. March of Dimes Prematurity Research Center at Stanford University School of Medicine. Prepregnancy Obesity and Risks of Stillbirth. PLoS ONE 2015, 10, e0138549. [Google Scholar]
- Farrant, B.M.; Shepherd, C.C. Maternal ethnicity, stillbirth and neonatal death risk in Western Australia 1998–2010. Aust. N. Z. J. Obstet. Gynaecol. 2016, 56, 532–536. [Google Scholar] [CrossRef]
- Brisendine, A.E.; Rice, W.S.; Goldfarb, S.S.; Wingate, M.S. The weathering hypothesis and stillbirth: Racial disparities across the life span. Ethn. Health 2020, 25, 354–366. [Google Scholar] [CrossRef]
- Davies-Tuck, M.L.; Davey, M.A.; Wallace, E.M. Maternal region of birth and stillbirth in Victoria, Australia 2000–2011: A retrospective cohort study of Victorian perinatal data. PLoS ONE 2017, 12, e0178727. [Google Scholar] [CrossRef]
- Berman, Y.; Ibiebele, I.; Patterson, J.A.; Randall, D.; Ford, J.B.; Nippita, T.; Morris, J.M.; Davies-Tuck, M.L.; Torvaldsen, S. Rates of stillbirth by maternal region of birth and gestational age in New South Wales, Australia 2004–2015. Aust. N. Z. J. Obstet. Gynaecol. 2020, 60, 425–432. [Google Scholar] [CrossRef]
- Handley, S.C.; Mullin, A.M.; Elovitz, M.A.; Gerson, K.D.; Montoya-Williams, D.; Lorch, S.A.; Burris, H.H. Changes in Preterm Birth Phenotypes and Stillbirth at 2 Philadelphia Hospitals during the SARS-CoV-2 Pandemic, March-June 2020. JAMA 2021, 325, 87–89. [Google Scholar] [CrossRef]
- Yerlikaya, G.; Akolekar, R.; McPherson, K.; Syngelaki, A.; Nicolaides, K.H. Prediction of stillbirth from maternal demographic and pregnancy characteristics. Ultrasound Obstet. Gynecol. 2016, 48, 607–612. [Google Scholar] [CrossRef]
- Robinson, H.P.; Fleming, J.E. A critical evaluation of sonar crown rump length measurements. Br. J. Obstet. Gynaecol. 1975, 82, 702–710. [Google Scholar] [CrossRef]
- Nicolaides, K.H. Screening for fetal aneuploidies at 11 to 13 weeks. Prenat. Diagn. 2011, 31, 7–15. [Google Scholar] [CrossRef]
- Syngelaki, A.; Hammami, A.; Bower, S.; Zidere, V.; Akolekar, R.; Nicolaides, K.H. Diagnosis of fetal non-chromosomal abnormalities on routine ultrasound examination at 11–13 weeks’ gestation. Ultrasound Obstet. Gynecol. 2019, 54, 468–476. [Google Scholar] [CrossRef] [Green Version]
- Nicolaides, K.H.; Wright, D.; Syngelaki, A.; Wright, A.; Akolekar, R. Fetal Medicine Foundation fetal and neonatal population weight charts. Ultrasound Obstet. Gynecol. 2018, 52, 44–51. [Google Scholar] [CrossRef] [Green Version]
- Births and Deaths Registration Act 1953, Amended by the Stillbirth Definition Act 1992. Available online: https://www.legislation.gov.uk (accessed on 1 April 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 1 April 2022).
- Viechtbauer, W. Conducting Meta-Analyses in R with the metafor Package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef] [Green Version]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022); Cochrane: London, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 1 April 2022).
- Spineli, L.M.; Pandis, N. Prediction interval in random-effects meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 586–588. [Google Scholar] [CrossRef]
- Sterne, J.A.; Egger, M.; Smith, G.D. Systematic reviews in health care: Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001, 323, 101–105. [Google Scholar] [CrossRef]
- Harbord, R.M.; Egger, M.; Sterne, J.A. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat. Med. 2006, 25, 3443–3457. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Cote, P.; Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Balduzzi, S.; Rücker, G.; Schwarzer, G. How to perform a meta-analysis with R: A practical tutorial. Evid. Based Ment. Health 2019, 22, 153–160. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression, 3rd ed.; Sage: Thousand Oaks, CA, USA, 2019; Available online: https://socialsciences.mcmaster.ca/jfox/Books/Companion/ (accessed on 1 April 2022).
- Familiari, A.; Scala, C.; Morlando, M.; Bhide, A.; Khalil, A.; Thilaganathan, B. Mid-pregnancy fetal growth, uteroplacental Doppler indices and maternal demographic characteristics: Role in prediction of stillbirth. Acta Obstet. Gynecol. Scand. 2016, 95, 1313–1318. [Google Scholar] [CrossRef] [PubMed]
- Ashoor, G.; Syngelaki, A.; Papastefanou, I.; Nicolaides, K.H.; Akolekar, R. Development and validation of model for prediction of placental dysfunction-related stillbirth from maternal factors, fetal weight and uterine artery Doppler at mid-gestation. Ultrasound Obstet. Gynecol. 2022, 59, 61–68. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | White (N = 127,762) | Black (N = 25,749) | South Asian (N = 7834) | East Asian (N = 3218) | Mixed (N = 4403) |
|---|---|---|---|---|---|
| Stillbirth | 367 (0.287) | 184 (0.715) * | 25 (0.319) | 11 (0.342) | 14 (0.318) |
| Age (years) | 30.8 (5.78) | 30.7 (5.96) * | 31.5 (4.99) * | 32.4 (5.23) * | 30.0 (6.07) * |
| Height (cm) | 165 (6.51) | 165 (6.42) * | 159 (6.19) * | 160 (5.96) * | 164 (6.84) * |
| Weight (kg) | 70.1 (15.4) | 75.8 (16.8) * | 63.3 (12.6) * | 58.7 (10.2) * | 69.5 (15.9) * |
| Conception | |||||
| Natural | 122,760 (96.1) | 25,314 (98.3) * | 7477 (95.4) * | 3079 (95.7) | 4287 (97.4) * |
| In vitro fertilisation | 3642 (2.85) | 265 (1.03) * | 273 (3.48) * | 110 (3.42) | 93 (2.11) * |
| Ovulation drugs | 1360 (1.06) | 170 (0.660) * | 84 (1.07) | 29 (0.901) | 23 (0.522) * |
| Smoking | 13,855 (10.8) | 1020 (3.96) * | 90 (1.15) * | 44 (1.37) * | 432 (9.81) * |
| Chronic hypertension | 1182 (0.925) | 891 (3.46) * | 101 (1.29) * | 20 (0.622) | 44 (0.999) |
| Diabetes mellitus Type 1 | 622 (0.487) | 62 (0.241) * | 21 (0.268) * | 5 (0.155) * | 15 (0.341) |
| Diabetes mellitus Type 2 | 541 (0.423) | 519 (2.02) * | 200 (2.55) * | 37 (1.15) * | 33 (0.749) * |
| SLE/APS | 262 (0.205) | 78 (0.303) * | 27 (0.345) * | 4 (0.124) | 8 (0.182) |
| Nulliparous | 61,899 (48.4) | 9653 (37.5) * | 3634 (46.4) * | 1622 (50.4) * | 2106 (47.8) |
| Previous miscarriage <16 weeks | 10,346 (8.10) | 1731 (6.72) * | 549 (7.01) * | 261 (8.11) | 380 (8.63) |
| Previous miscarriage 16–23 weeks | 266 (0.208) | 241 (0.936) * | 25 (0.319) | 7 (0.218) | 20 (0.454) * |
| Parous | 65,863 (51.6) | 16,096 (62.5) * | 4200 (53.6) * | 1596 (49.6) * | 2297 (52.2) |
| Previous PE | 3829 (3.00) | 1208 (4.69) * | 229 (2.92) | 46 (1.43) * | 113 (2.57) |
| Previous SGA | 7530 (5.89) | 2830 (11.0) * | 1032 (13.2) * | 291 (9.04) * | 390 (8.86) * |
| Previous stillbirth | 862 (0.675) | 446 (1.73) * | 65 (0.830) | 21 (0.653) | 39 (0.886) |
| Previous miscarriage <16 weeks | 17,767 (13.9) | 4003 (15.5) * | 990 (12.6) * | 358 (11.1) * | 633 (14.4) |
| Previous miscarriage 16–23 weeks | 694 (0.543) | 437 (1.70) * | 52 (0.664) | 11 (0.342) | 38 (0.863) * |
| Predictors | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Maternal age (years) | 0.78 | 0.71–0.87 | <0.001 | 0.85 | 0.77–0.94 | 0.001 |
| Maternal age (years)2 | 1.00 | 1.00–1.01 | <0.001 | 1.00 | 1.00–1.00 | 0.001 |
| Body mass index (kg/m2) | 1.05 | 1.04–1.07 | <0.001 | 1.04 | 1.03–1.05 | <0.001 |
| Race | ||||||
| White (reference) | ||||||
| Black | 2.50 | 2.09–2.98 | <0.001 | 2.36 | 1.96–2.84 | <0.001 |
| East Asian | 1.19 | 0.61–2.06 | 0.569 | 1.46 | 0.75–2.55 | 0.216 |
| South Asian | 1.11 | 0.72–1.63 | 0.610 | 1.26 | 0.82–1.86 | 0.262 |
| Mixed | 1.11 | 0.62–1.82 | 0.709 | 1.12 | 0.62–1.84 | 0.681 |
| Conception by in vitro fertilization | 1.17 | 0.73–1.87 | 0.512 | 1.14 | 0.67–1.82 | 0.598 |
| Conception by ovulation drugs | 1.89 | 1.04–3.43 | 0.038 | 1.96 | 1.01–3.40 | 0.028 |
| Smoking | 1.69 | 1.33–2.11 | <0.001 | 1.92 | 1.50–2.43 | <0.001 |
| Diabetes Type 1 | 4.02 | 2.00–7.14 | <0.001 | 3.90 | 1.93–6.95 | <0.001 |
| Diabetes Type 2 | 2.84 | 1.55–4.72 | <0.001 | 1.47 | 0.79–2.50 | 0.187 |
| Chronic hypertension | 3.67 | 2.45–5.27 | <0.001 | 2.04 | 1.34–3.01 | 0.001 |
| Previous obstetric history | ||||||
| Nulliparous (reference) | ||||||
| Nulliparous-previous miscarriage <16 weeks | 0.95 | 0.69–1.28 | 0.742 | 0.87 | 0.63–1.17 | 0.369 |
| Nulliparous-previous miscarriage 16–23 weeks | 2.36 | 0.84–5.16 | 0.058 | 1.36 | 0.48–3.00 | 0.505 |
| Parous-no previous miscarriage/stillbirth | 0.80 | 0.67–0.97 | 0.023 | 0.70 | 0.57–0.85 | <0.001 |
| Parous-previous miscarriage <16 weeks | 0.87 | 0.67–1.12 | 0.292 | 0.71 | 0.54–0.92 | 0.012 |
| Parous-previous miscarriage 16–23 weeks | 0.85 | 0.26–2.00 | 0.750 | 0.49 | 0.15–1.18 | 0.166 |
| Parous-previous stillbirth | 4.08 | 2.55–6.17 | <0.001 | 2.55 | 1.58–3.92 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arechvo, A.; Nikolaidi, D.A.; Gil, M.M.; Rolle, V.; Syngelaki, A.; Akolekar, R.; Nicolaides, K.H. Maternal Race and Stillbirth: Cohort Study and Systematic Review with Meta-Analysis. J. Clin. Med. 2022, 11, 3452. https://doi.org/10.3390/jcm11123452
Arechvo A, Nikolaidi DA, Gil MM, Rolle V, Syngelaki A, Akolekar R, Nicolaides KH. Maternal Race and Stillbirth: Cohort Study and Systematic Review with Meta-Analysis. Journal of Clinical Medicine. 2022; 11(12):3452. https://doi.org/10.3390/jcm11123452
Chicago/Turabian StyleArechvo, Anastasija, Despoina A. Nikolaidi, María M. Gil, Valeria Rolle, Argyro Syngelaki, Ranjit Akolekar, and Kypros H. Nicolaides. 2022. "Maternal Race and Stillbirth: Cohort Study and Systematic Review with Meta-Analysis" Journal of Clinical Medicine 11, no. 12: 3452. https://doi.org/10.3390/jcm11123452
APA StyleArechvo, A., Nikolaidi, D. A., Gil, M. M., Rolle, V., Syngelaki, A., Akolekar, R., & Nicolaides, K. H. (2022). Maternal Race and Stillbirth: Cohort Study and Systematic Review with Meta-Analysis. Journal of Clinical Medicine, 11(12), 3452. https://doi.org/10.3390/jcm11123452







