Conventional Laparoscopy versus Robotic-Assisted Aortic Lymph-Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
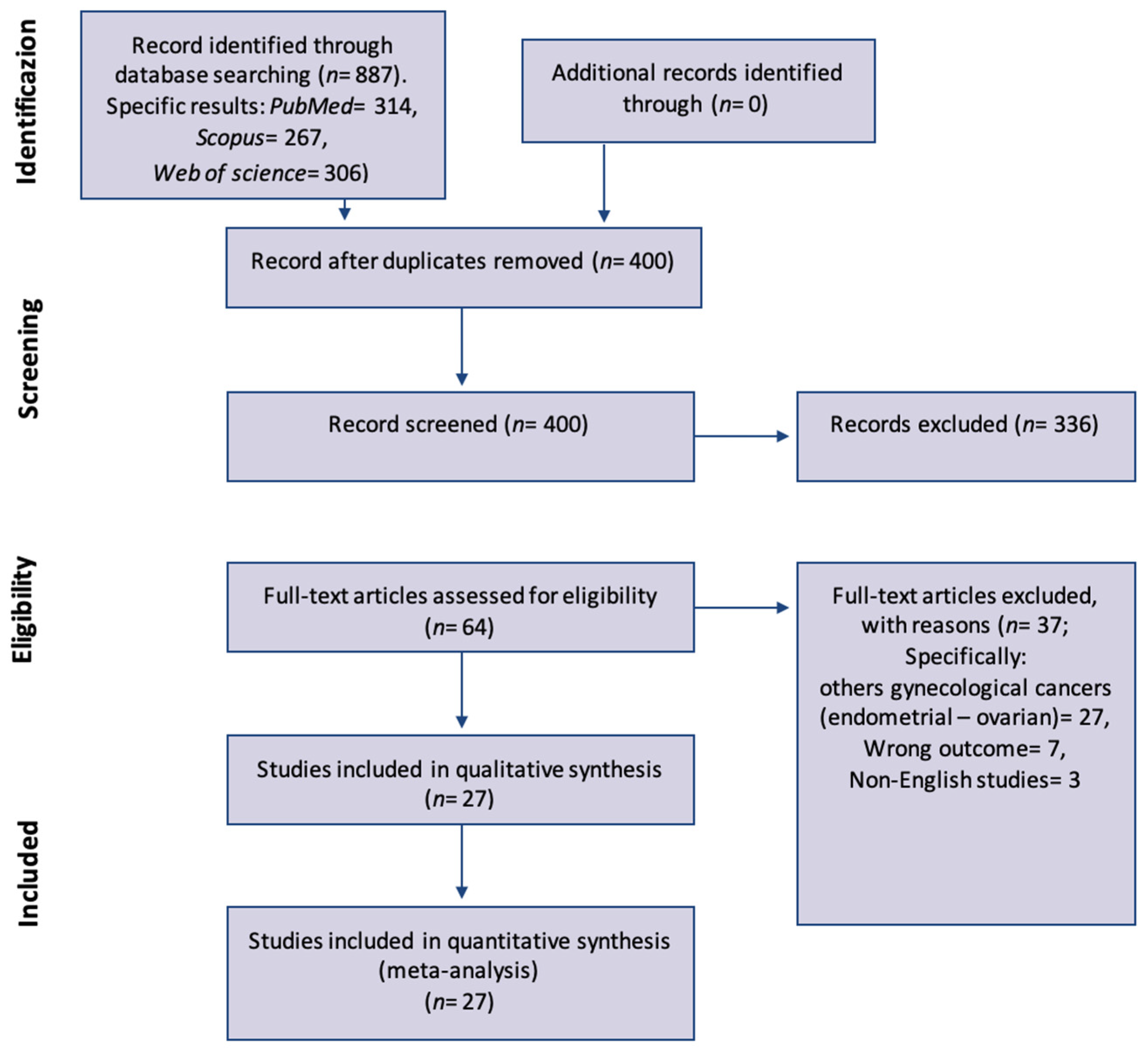
2. Materials and Methods
Statistical Analysis
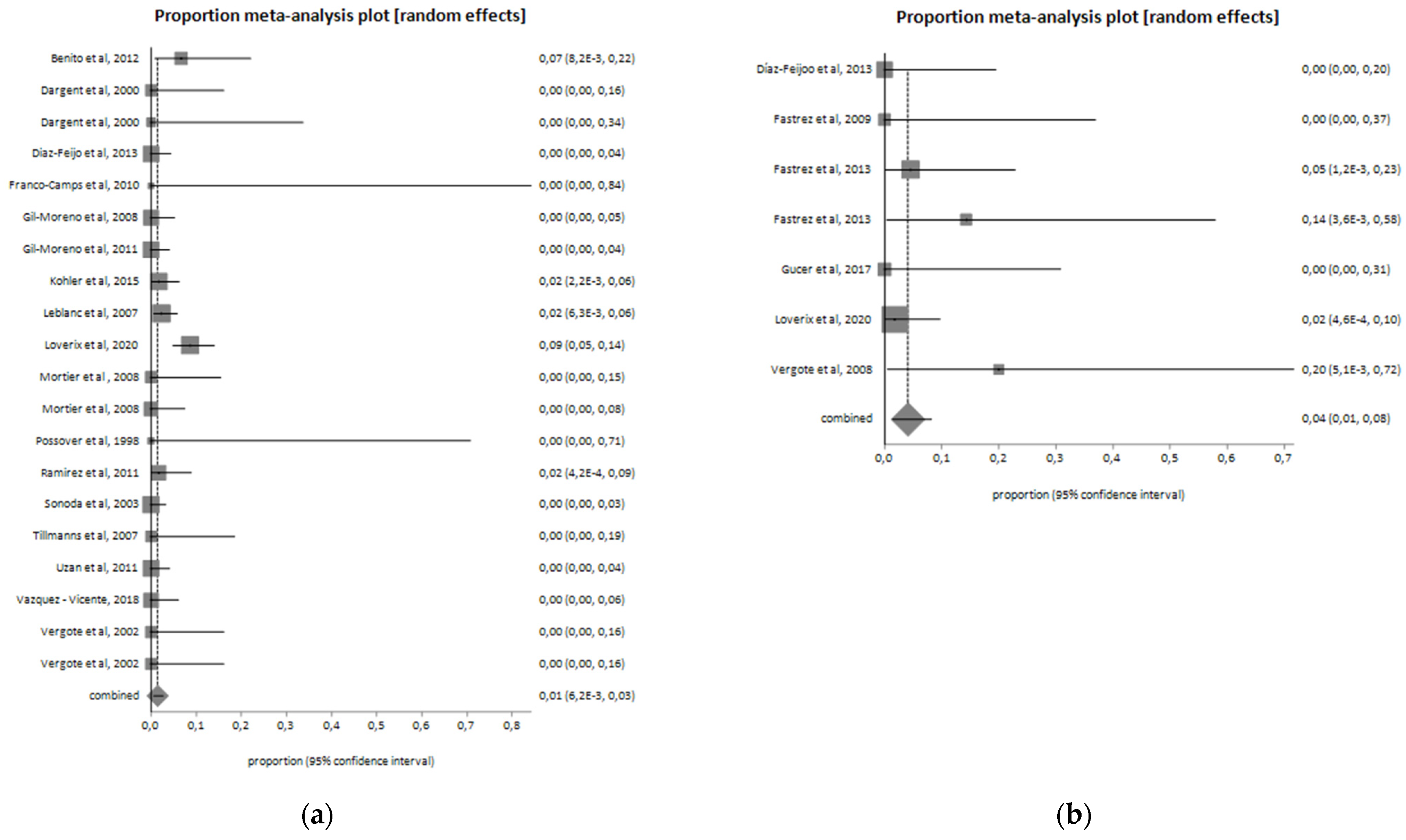
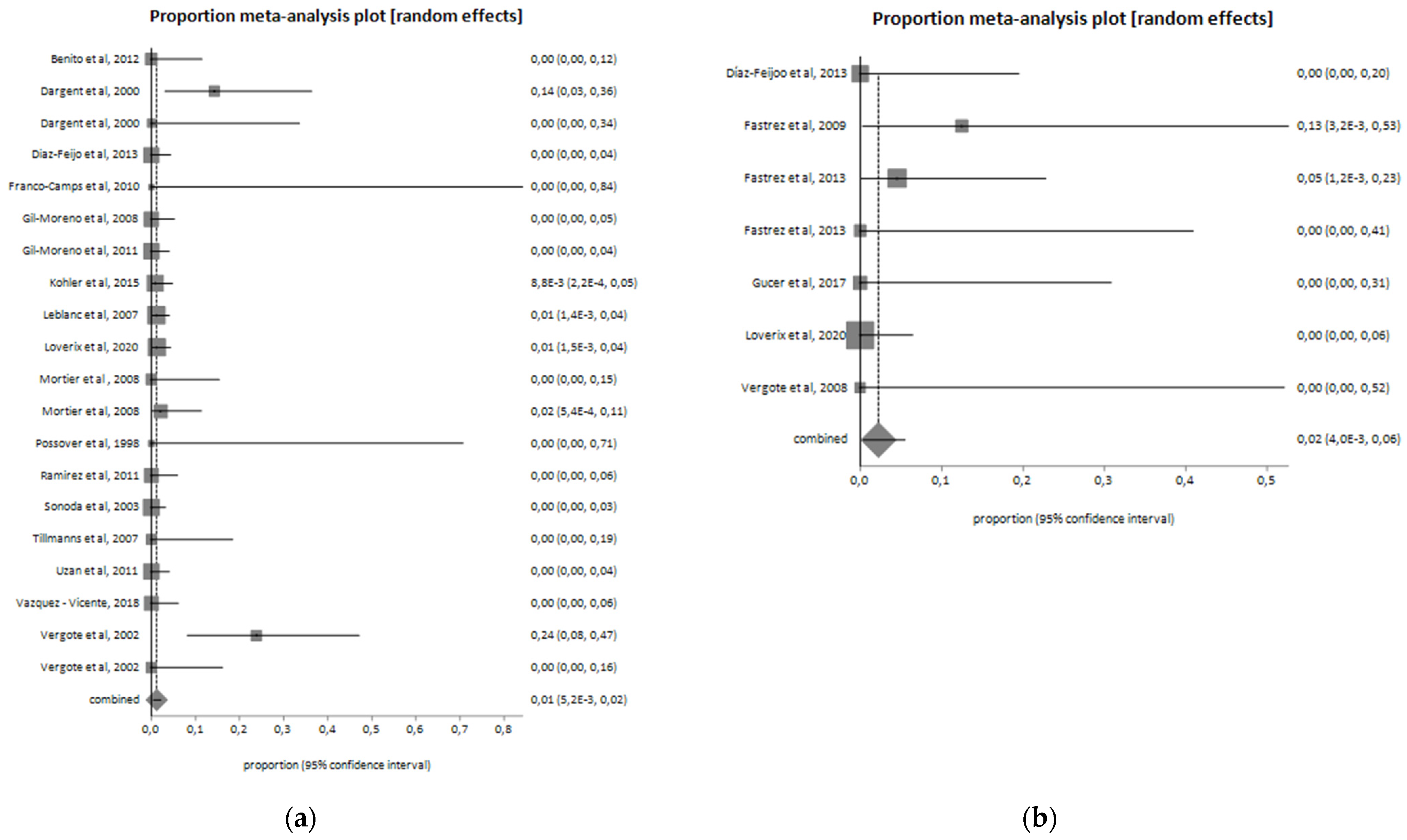
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Authors, Years | Type of Study | Cases | Stage | OT (Minutes) | EBL (mL) | Conversions | HT (Days) | Number of Lymph Nodes Excised | Intra-Operative Complications (n and Type) | Post-Operative Complications (n and Type) | BMI (Median) | Age (Median) | Technique |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Díaz-Feijoo et al., 2013 [27] | Retrospective study | 17 | IB2-IVA | 150 | 20 | 0 | 2 | 17 | 0 | 3 (not specified) | 23 | 49 | Robotic Retroperitoneal |
| Fastrez et al., 2009 [28] | Retrospective study | 8 | IB2-IVA | 137.5 | / | 1 | 4.5 | 14 | 0 | 0 | 24.3 | 58 | Robotic Transperitoneal |
| Fastrez et al., 2013 [29] | Retrospective study | 22 | IB2-IVA | 165 | / | 1 | 6 | 19.5 | 1 aortic injury | 4: 1 chylous ascites; 2 symptomatic lymphocele; 1 epiploic hernia through umbilical port | 27 | 55 | Robotic Transperitoneal |
| Fastrez et al., 2013 [29] | Retrospective study | 7 | IB2-IVA | 100 | / | 0 | 2.5 | 9.5 | 1 partial section of the right ureter | 0 | 24 | 50.5 | Robotic Retroperitoneal |
| Gucer et al., 2017 [30] | Prospective observational preliminary study | 10 | IIB-IVA | 141 | 12.5 | 0 | 4 | 25 | 0 | 2: 1 symptomatic lymphocyst; 1 local infection on assistant port site | 28.5 | 46 | Robotic Transperitoneal |
| Loverix et al., 2020 [10] | Retrospective study | 55 | IB1-IVA | 74.5 | 25 | 0 | 1.8 | 1 bleeding | 4: 3 urinary tract infection; 1 salpingitis | 24.7 | 49 | Robotic Transperitoneal and Retroperitoneal | |
| Vergote et al., 2008 [31] | Retrospective study | 5 | IIB-IIIB | 83.8 | 50 | 0 | 2.2 | 9.2 | 1 right ureter damage | 0 | 23.8 | 49.6 | Robotic Retroperitoneal |
| Benito et al., 2012 [13] | Retrospective study | 30 | IB2-IVA | 118.7 | 75 | 0 | 1.9 | 14.2 | 2: 1 lumbar artery injury; 1 bowel injury | 0 | 26.3 | 47.6 | Laparoscopic Retroperitoneal |
| Dargent et al., 2000 [14] | Retrospective study | 21 | IB1-IVA | 119 | / | 3 | / | 15 | 0 | 1 lymphocele | 23 | 50 | Laparoscopic Retroperitoneal |
| Dargent et al., 2000 [14] | Retrospective study | 9 | IB1-IVA | 160 | / | 0 | / | 19 | 0 | 1 phlebitis | 23 | 50 | Laparoscopic Transperitoneal |
| Diaz-Feijoo et al., 2013 [27] | Retrospective study | 83 | IB2-IVA | 150 | 20 | 0 | 2 | 17 | 0 | 3: 2 lymphocysts; 1 chylous ascites | 26.4 | 51 | Laparoscopic Retroperitoneal |
| Franco-Camps et al., 2010 [15] | Retrospective study | 2 | IIIB-IVA | 140 | 95 | 0 | 2 | 6 | 0 | 0 | 29 | 71 | Laparoscopic Retroperitoneal |
| Gil-Moreno et al., 2008 [17] | Retrospective study | 69 | 140 | 100 | 0 | 2 | 15.2 | 0 | 4: 2 retroperitoneal hematoma; 2 lymphocyst | 27 | 51 | Laparoscopic Retroperitoneal | |
| Gil-Moreno et al., 2011 [16] | Retrospective study | 87 | IB2-IVA | 150 | 0 | 2 | 0 | 6: 2 retroperitoneal hematoma; 3 lymphocysts;1 urinary tract infection | 26.5 | Laparoscopic Retroperitoneal | |||
| Köhler et al., 2015 [18] | Trial | 113 | IIB-IVA | / | / | 1 | / | 17 | 2 vascular injuries | 9: 1 thrombosis; 1 ileus; 4 symptomatic lymphoceles; 1 nerve irritation; and 2 others (not specified) | 26.2 | 47.2 | Laparoscopic Transperitoneal |
| Leblanc et al., 2007 [3] | Retrospective study | 173 | IB2-IVA | 155 | 100 | 2 | 1.4 | 20.8 | 4: 1 obturator nerve injury; 2 ureteric injuries; 1 vascular injury (vena cava) | 22: 17 symptomatic lymphocysts; 3 transient ascites; 1 retroperitoneal hematoma; 1 bowel obstruction resulting from herniating bowel through an umbilical port site | 27.1 | 45 | Laparoscopic Retroperitoneal |
| Loverix et al., 2020 [10] | Retrospective study | 162 | IIB-IVA | 75 | 62.5 | 2 | 2 | 14: 2 ureteral trauma;11 bleeding; 1 other | 25: 2 wound problem with conservative management; 1 retroperitoneal hematoma with conservative management; 1 severe pain; 4 urinary tract infection;8 blood transfusion; 1 vasovagal syncope; 1 severe vaginal blood; 1 iron supplements for anemia; 1 DVT with lung embolism treated with LMWH; 1 placement of ureteral stent for ureteral trauma; 1 retroperitoneal abscess with evacuation under anesthesia; 1 re-laparotomy for bleeding of the internal epigastric artery; 1 laparoscopic repair of ureteral trauma; 1 hospitalization in intensive care unit for hyponatremia | 24.4 | 48 | Laparoscopic Transperitoneal and Retroperitoneal | |
| Mortier et al., 2008 [19] | Retrospective study | 22 | IB2-IIIB | 68 | 90 | 0 | 2 | 5 | 0 | 0 | 24 | 48 | Laparoscopic Transperitoneal |
| Mortier et al., 2008 [19] | Retrospective study | 47 | IB2-IIIB | 62 | 90 | 1 | 2 | 8 | 0 | 3: 2 lymphocoeles; 1 retroperitoneal hematoma | 24 | 48 | Laparoscopic Retroperitoneal |
| Possover et al., 1998 [20] | Retrospective study | 3 | IIIB | 218 | 200 | 0 | 4 | 10 | 0 | 0 | / | 46.3 | Laparoscopic Retroperitoneal |
| Ramirez et al., 2011 [21] | Retrospective study | 60 | IB2-IVA | 140 | 22.5 | 0 | 1 | 11 | 1 bleeding from an ascending lumbar vein at the level of the left renal vein | 7 lymphocyst | 26,7 | 48 | Laparoscopic Retroperitoneal |
| Sonoda et al., 2003 [22] | Retrospective study | 111 | IB2-IVA | 157 | 100 | 0 | 2 | 19 | 0 | 14: 11 symptomatic lymphoceles; 2 retroperitoneal hematomas; 1 trocar-site hernia | 24 | 46 | Laparoscopic Retroperitoneal |
| Tillmanns et al., 2007 [23] | Retrospective study | 18 | IIB-IVA | 108 | 25 | 0 | 10 | 0 | 1 lymphocyst | 29 | 49 | Laparoscopic Retroperitoneal | |
| Uzan et al., 2011 [24] | Retrospective study | 89 | IB2-IVA | 185 | / | 0 | 3 | 13 | 0 | 3 lymphocysts | 23 | 45 | Laparoscopic Retroperitoneal |
| Vázquez-Vicente, 2018 [25] | Retrospective study | 59 | IB2-IVA | 180 | / | 0 | 1.7 | 16.4 | 0 | 4: 3 lymphoceles; 1 intrabdominal abscess | 24.6 | 52.3 | Laparoscopic Transperitoneal and Retroperitoneal |
| Vergote et al., 2002 [26] | Retrospective study | 21 | IB2-IIIB | 55 | 78 | 5 | 1 | 6 | 0 | 1 retroperitoneal hematoma | / | 51 | Laparoscopic Retroperitoneal |
| Vergote et al., 2002 [26] | Retrospective study | 21 | IB2-IIIB | 70 | 78 | 0 | 1 | 6 | 0 | 0 | / | 51 | Laparoscopic Transperitoneal |
Appendix B
| Author, Year | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Díaz-Feijoo et al., 2013 [27] |
|
|
| Fastrez et al., 2009 [28] |
| / |
| Fastrez et al., 2013 [29] |
| / |
| Gucer et al., 2017 [30] |
|
|
| Loverix et al., 2020 [10] |
|
|
| Vergote et al., 2008 [31] |
| / |
| Benito et al., 2012 [13] |
| / |
| Dargent et al., 2000 [14] |
| / |
| Franco-Camps et al., 2010 [15] |
| / |
| Gil-Moreno et al., 2008 [17] |
| / |
| Gil-Moreno et al., 2011 [16] |
|
|
| Köhler et al., 2015 [18] |
| / |
| Leblanc et al., 2007 [3] |
| / |
| Mortier et al., 2008 [19] |
|
|
| Possover et al., 1998 [20] |
| / |
| Ramirez et al., 2011 [21] |
|
|
| Sonoda et al., 2003 [22] |
|
|
| Tillmanns et al., 2007 [23] |
|
|
| Uzan et al., 2011 [24] |
|
|
| Vázquez-Vicente, 2018 [25] |
| / |
| Vergote et al., 2002 [26] |
|
|
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Liu, B.; Gao, S.; Li, S. A Comprehensive Comparison of CT, MRI, Positron Emission Tomography or Positron Emission Tomography/CT, and Diffusion Weighted Imaging-MRI for Detecting the Lymph Nodes Metastases in Patients with Cervical Cancer: A Meta-Analysis Based on 67 Studies. Gynecol. Obstet. Investig. 2017, 82, 209–222. [Google Scholar] [CrossRef]
- Leblanc, E.; Narducci, F.; Frumovitz, M.; Lesoin, A.; Castelain, B.; Baranzelli, M.C.; Taieb, S.; Fournier, C.; Querleu, D. Therapeutic Value of Pretherapeutic Extraperitoneal Laparoscopic Staging of Locally Advanced Cervical Carcinoma. Gynecol. Oncol. 2007, 105, 304–311. [Google Scholar] [CrossRef]
- Chantalat, E.; Vidal, F.; Leguevaque, P.; Lepage, B.; Mathevet, P.; Deslandres, M.; Motton, S. Cervical Cancer with Paraaortic Involvement: Do Patients Truly Benefit from Tailored Chemoradiation Therapy? A Retrospective Study on 8 French Centers. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 193, 118–122. [Google Scholar] [CrossRef]
- Rogers, L.; Siu, S.S.N.; Luesley, D.; Bryant, A.; Dickinson, H.O. Radiotherapy and Chemoradiation after Surgery for Early Cervical Cancer. Cochrane Database Syst. Rev. 2012, 5, CD007583. [Google Scholar] [CrossRef]
- Choi, H.J.; Ju, W.; Myung, S.K.; Kim, Y. Diagnostic Performance of Computer Tomography, Magnetic Resonance Imaging, and Positron Emission Tomography or Positron Emission Tomography/Computer Tomography for Detection of Metastatic Lymph Nodes in Patients with Cervical Cancer: Meta-Analysis. Cancer Sci. 2010, 101, 1471–1479. [Google Scholar] [CrossRef]
- Choi, H.J.; Roh, J.W.; Seo, S.-S.; Lee, S.; Kim, J.-Y.; Kim, S.-K.; Kang, K.W.; Lee, J.S.; Jeong, J.Y.; Park, S.-Y. Comparison of the Accuracy of Magnetic Resonance Imaging and Positron Emission Tomography/Computed Tomography in the Presurgical Detection of Lymph Node Metastases in Patients with Uterine Cervical Carcinoma: A Prospective Study. Cancer 2006, 106, 914–922. [Google Scholar] [CrossRef]
- Frumovitz, M.; Querleu, D.; Gil-Moreno, A.; Morice, P.; Jhingran, A.; Munsell, M.F.; Macapinlac, H.A.; Leblanc, E.; Martinez, A.; Ramirez, P.T. Lymphadenectomy in Locally Advanced Cervical Cancer Study (LiLACS): Phase III Clinical Trial Comparing Surgical with Radiologic Staging in Patients with Stages IB2-IVA Cervical Cancer. J. Minim. Invasive Gynecol. 2014, 21, 3–8. [Google Scholar] [CrossRef]
- Capozzi, V.A.; Sozzi, G.; Monfardini, L.; Di Donna, M.C.; Giallombardo, V.; Lo Balbo, G.; Butera, D.; Berretta, R.; Chiantera, V. Transperitoneal versus Extraperitoneal Laparoscopic Aortic Lymph Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis. Eur. J. Surg. Oncol. 2021, 47, 2256–2264. [Google Scholar] [CrossRef]
- Loverix, L.; Salihi, R.R.; Van Nieuwenhuysen, E.; Concin, N.; Han, S.; van Gorp, T.; Vergote, I. Para-Aortic Lymph Node Surgical Staging in Locally-Advanced Cervical Cancer: Comparison between Robotic versus Conventional Laparoscopy. Int. J. Gynecol. Cancer 2020, 30, 466–472. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Basch, E.; Becker, C.; Rogak, L.J.; Schrag, D.; Reeve, B.B.; Spears, P.; Smith, M.L.; Gounder, M.M.; Mahoney, M.R.; Schwartz, G.K.; et al. Composite Grading Algorithm for the National Cancer Institute’s Patient-Reported Outcomes Version of the Common Terminology Criteria for Adverse Events (PRO-CTCAE). Clin. Trials 2021, 18, 104–114. [Google Scholar] [CrossRef]
- Benito, V.; Lubrano, A.; Arencibia, O.; Andújar, M.; Pinar, B.; Medina, N.; Falcón, J.M.; Falcón, O. Laparoscopic Extraperitoneal Para-Aortic Lymphadenectomy in the Staging of Locally Advanced Cervical Cancer: Is It a Feasible Procedure at a Peripheral Center? Int. J. Gynecol. Cancer 2012, 22, 332–336. [Google Scholar] [CrossRef]
- Dargent, D.; Ansquer, Y.; Mathevet, P. Technical Development and Results of Left Extraperitoneal Laparoscopic Paraaortic Lymphadenectomy for Cervical Cancer. Gynecol. Oncol. 2000, 77, 87–92. [Google Scholar] [CrossRef]
- Franco-Camps, S.; Cabrera, S.; Pérez-Benavente, A.; Díaz-Feijoo, B.; Bradbury, M.; Xercavins, J.; Gil-Moreno, A. Extraperitoneal Laparoscopic Approach for Diagnosis and Treatment of Aortic Lymph Node Recurrence in Gynecologic Malignancy. J. Minim. Invasive Gynecol. 2010, 17, 570–575. [Google Scholar] [CrossRef]
- Gil-Moreno, A.; Franco-Camps, S.; Cabrera, S.; Pérez-Benavente, A.; Martínez-Gómez, X.; Garcia, A.; Xercavins, J. Pretherapeutic Extraperitoneal Laparoscopic Staging of Bulky or Locally Advanced Cervical Cancer. Ann. Surg. Oncol. 2011, 18, 482–489. [Google Scholar] [CrossRef]
- Gil-Moreno, A.; Díaz-Feijoo, B.; Pérez-Benavente, A.; del Campo, J.M.; Xercavins, J.; Martínez-Palones, J.M. Impact of Extraperitoneal Lymphadenectomy on Treatment and Survival in Patients with Locally Advanced Cervical Cancer. Gynecol. Oncol. 2008, 110, S33–S35. [Google Scholar] [CrossRef]
- Köhler, C.; Mustea, A.; Marnitz, S.; Schneider, A.; Chiantera, V.; Ulrich, U.; Scharf, J.-P.; Martus, P.; Vieira, M.A.; Tsunoda, A. Perioperative Morbidity and Rate of Upstaging after Laparoscopic Staging for Patients with Locally Advanced Cervical Cancer: Results of a Prospective Randomized Trial. Am. J. Obstet. Gynecol. 2015, 213, 503.e1–503.e7. [Google Scholar] [CrossRef]
- Mortier, D.G.; Stroobants, S.; Amant, F.; Neven, P.; VAN Limbergen, E.; Vergote, I. Laparoscopic Para-Aortic Lymphadenectomy and Positron Emission Tomography Scan as Staging Procedures in Patients with Cervical Carcinoma Stage IB2-IIIB. Int. J. Gynecol. Cancer 2008, 18, 723–729. [Google Scholar] [CrossRef]
- Possover, M.; Krause, N.; Drahonovsky, J.; Schneider, A. Left-Sided Suprarenal Retrocrural Para-Aortic Lymphadenectomy in Advanced Cervical Cancer by Laparoscopy. Gynecol. Oncol. 1998, 71, 219–222. [Google Scholar] [CrossRef]
- Ramirez, P.T.; Jhingran, A.; Macapinlac, H.A.; Euscher, E.D.; Munsell, M.F.; Coleman, R.L.; Soliman, P.T.; Schmeler, K.M.; Frumovitz, M.; Ramondetta, L.M. Laparoscopic Extraperitoneal Para-Aortic Lymphadenectomy in Locally Advanced Cervical Cancer: A Prospective Correlation of Surgical Findings with Positron Emission Tomography/Computed Tomography Findings. Cancer 2011, 117, 1928–1934. [Google Scholar] [CrossRef] [PubMed]
- Sonoda, Y.; Leblanc, E.; Querleu, D.; Castelain, B.; Papageorgiou, T.H.; Lambaudie, E.; Narducci, F. Prospective Evaluation of Surgical Staging of Advanced Cervical Cancer via a Laparoscopic Extraperitoneal Approach. Gynecol. Oncol. 2003, 91, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Tillmanns, T.; Lowe, M.P. Safety, Feasibility, and Costs of Outpatient Laparoscopic Extraperitoneal Aortic Nodal Dissection for Locally Advanced Cervical Carcinoma. Gynecol. Oncol. 2007, 106, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Uzan, C.; Souadka, A.; Gouy, S.; Debaere, T.; Duclos, J.; Lumbroso, J.; Haie-Meder, C.; Morice, P. Analysis of Morbidity and Clinical Implications of Laparoscopic Para-Aortic Lymphadenectomy in a Continuous Series of 98 Patients with Advanced-Stage Cervical Cancer and Negative PET-CT Imaging in the Para-Aortic Area. Oncologist 2011, 16, 1021–1027. [Google Scholar] [CrossRef]
- Vázquez-Vicente, D.; Fernández Del Bas, B.; García Villayzán, J.; Di Fiore, H.A.; Luna Tirado, J.; Casado Echarren, V.; García-Foncillas, J.; Plaza Arranz, J.; Chiva, L. Laparoscopic Paraaortic Surgical Staging in Locally Advanced Cervical Cancer: A Single-Center Experience. Clin. Transl. Oncol. 2018, 20, 1455–1459. [Google Scholar] [CrossRef] [PubMed]
- Vergote, I.; Amant, F.; Berteloot, P.; Van Gramberen, M. Laparoscopic Lower Para-Aortic Staging Lymphadenectomy in Stage IB2, II, and III Cervical Cancer. Int. J. Gynecol. Cancer 2002, 12, 22–26. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Feijoo, B.; Gil-Ibáñez, B.; Pérez-Benavente, A.; Martínez-Gómez, X.; Colás, E.; Sánchez-Iglesias, J.L.; Cabrera-Díaz, S.; Puig-Puig, O.; Magrina, J.F.; Gil-Moreno, A. Comparison of Robotic-Assisted vs. Conventional Laparoscopy for Extraperitoneal Paraaortic Lymphadenectomy. Gynecol. Oncol. 2014, 132, 98–101. [Google Scholar] [CrossRef]
- Fastrez, M.; Vandromme, J.; George, P.; Rozenberg, S.; Degueldre, M. Robot Assisted Laparoscopic Transperitoneal Para-Aortic Lymphadenectomy in the Management of Advanced Cervical Carcinoma. Eur. J. Obstet. Gynecol. Reprod. Biol. 2009, 147, 226–229. [Google Scholar] [CrossRef]
- Fastrez, M.; Goffin, F.; Vergote, I.; Vandromme, J.; Petit, P.; Leunen, K.; Degueldre, M. Multi-Center Experience of Robot-Assisted Laparoscopic Para-Aortic Lymphadenectomy for Staging of Locally Advanced Cervical Carcinoma. Acta Obstet. Gynecol. Scand. 2013, 92, 895–901. [Google Scholar] [CrossRef]
- Gucer, F.; Misirlioglu, S.; Ceydeli, N.; Taskiran, C. Robot-Assisted Laparoscopic Transperitoneal Infrarenal Lymphadenectomy in Patients with Locally Advanced Cervical Cancer by Single Docking: Do We Need a Backup Procedure? J. Robot. Surg. 2018, 12, 49–58. [Google Scholar] [CrossRef]
- Vergote, I.; Pouseele, B.; Van Gorp, T.; Vanacker, B.; Leunen, K.; Cadron, I.; Neven, P.; Amant, F. Robotic Retroperitoneal Lower Para-Aortic Lymphadenectomy in Cervical Carcinoma: First Report on the Technique Used in 5 Patients. Acta Obstet. Gynecol. Scand. 2008, 87, 783–787. [Google Scholar] [CrossRef] [PubMed]
- Marnitz, S.; Köhler, C.; Roth, C.; Füller, J.; Hinkelbein, W.; Schneider, A. Is There a Benefit of Pretreatment Laparoscopic Transperitoneal Surgical Staging in Patients with Advanced Cervical Cancer? Gynecol. Oncol. 2005, 99, 536–544. [Google Scholar] [CrossRef] [PubMed]
- Di Donna, M.C.; Cicero, C.; Sozzi, G.; Cucinella, G.; Scambia, G.; Chiantera, V. Laparoscopic Aortic Lymphadenectomy in Left-Sided Inferior Vena Cava. Int. J. Gynecol. Cancer 2020, 30, 1462–1463. [Google Scholar] [CrossRef]
- Lim, P.C.; Kang, E.; Park, D.H. Learning Curve and Surgical Outcome for Robotic-Assisted Hysterectomy with Lymphadenectomy: Case-Matched Controlled Comparison with Laparoscopy and Laparotomy for Treatment of Endometrial Cancer. J. Minim. Invasive Gynecol. 2010, 17, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Reyes Claret, A.; Martínez Canto, M.C.; Robles Gourley, A.; Llull Gomila, M.; Martín Jiménez, Á. Transperitoneal Laparoscopic Para-Aortic Lymphadenectomy and Body Mass Index: Is It Really a Limiting Factor for the Procedure? J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 416–422. [Google Scholar] [CrossRef]
- Hong, D.G.; Park, N.Y.; Chong, G.O.; Cho, Y.L.; Park, I.S.; Lee, Y.S.; Lee, D.H. Laparoscopic Transperitoneal Infrarenal Para-Aortic Lymphadenectomy in Patients with FIGO Stage IB1-II B Cervical Carcinoma. JSLS 2012, 16, 229–235. [Google Scholar] [CrossRef][Green Version]
- Yoshida, H.; Yamamoto, M.; Shigeta, H. Learning Curve of Laparoscopic Extraperitoneal Para-Aortic Lymphadenectomy for Endometrial Carcinoma: A Cumulative Sum Analysis. Surg. Oncol. 2020, 35, 254–260. [Google Scholar] [CrossRef]
- Ponce, J.; Barahona, M.; Pla, M.J.; Rovira, J.; Garcia-Tejedor, A.; Gil-Ibanez, B.; Gaspar, H.M.; Sabria, E.; Bartolomé, C.; Marti, L. Robotic Transperitoneal Infrarenal Para-Aortic Lymphadenectomy with Double Docking: Technique, Learning Curve, and Perioperative Outcomes. J. Minim. Invasive Gynecol. 2016, 23, 622–627. [Google Scholar] [CrossRef]
- Bentivegna, E.; Koual, M.; Nguyen-Xuan, H.-T.; Plait, L.; Seidler, S.; Achen, G.; Bats, A.-S.; Azaïs, H. Docking for Robotic Extraperitoneal Para-Aortic Lymphadenectomy with Da Vinci Xi Surgical System. J. Gynecol. Obstet. Hum. Reprod. 2021, 50, 102131. [Google Scholar] [CrossRef]

| Laparoscopic | Robotic | p | |
|---|---|---|---|
| Number of studies | 20 | 7 | |
| Number of cases | 1200 | 124 | |
| Operative time (min) | 129 | 121.7 | 0.8 |
| Total complications (n) | 127 | 17 | 0.29 |
| Intraoperative complications (n) | 23 | 4 | 0.31 |
| Postoperative complications (n) | 104 | 13 | 0.5 |
| Number of lymph nodes excised | 12.7 | 15.7 | 0.38 |
| EBL | 81.1 | 26.9 | 0.02 |
| Hospital stay | 1.9 | 3.3 | 0.02 |
| Age | 49.8 | 51.0 | 0.62 |
| BMI | 25.5 | 25.0 | 0.33 |
| Type of Intraoperative Complication | Laparoscopic (n = 1200) | Robotic (n = 124) | p |
|---|---|---|---|
| Vascular injuries | 18 (1.5%) | 2 (1.6%) | |
| Ureteric injuries | 3 (0.3%) | 2 (1.6%) | |
| Nerve injury | 1 (0.1%) | 0 (0%) | |
| Bowel injury total | 1 (0.1%) | 0 (0%) | |
| Total | 23 (2%) | 4 (3.2%) | 0.31 |
| Type of Postoperative Complication | Laparoscopic (n = 1200) | Robotic (n = 124) | p |
|---|---|---|---|
| Lymphatic complication | 57 (4.7%) | 6 (4.8%) | |
| Vascular complication | 15 (1.2%) | 0 (0%) | |
| Urinary complication | 7 (0.6%) | 3 (2.4%) | |
| Bowel complication | 1 (0.1%) | 0 (0%) | |
| Trocar site hernia | 2 (0.2%) | 1 (0.8%) | |
| Others | 22 (1.8%) | 3 (2.4.%) | |
| Total | 104 (8.6%) | 13 (10.4%) | 0.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Donna, M.C.; Giallombardo, V.; Lo Balbo, G.; Cucinella, G.; Sozzi, G.; Capozzi, V.A.; Abbate, A.; Laganà, A.S.; Garzon, S.; Chiantera, V. Conventional Laparoscopy versus Robotic-Assisted Aortic Lymph-Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 3332. https://doi.org/10.3390/jcm11123332
Di Donna MC, Giallombardo V, Lo Balbo G, Cucinella G, Sozzi G, Capozzi VA, Abbate A, Laganà AS, Garzon S, Chiantera V. Conventional Laparoscopy versus Robotic-Assisted Aortic Lymph-Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2022; 11(12):3332. https://doi.org/10.3390/jcm11123332
Chicago/Turabian StyleDi Donna, Mariano Catello, Vincenzo Giallombardo, Giuseppina Lo Balbo, Giuseppe Cucinella, Giulio Sozzi, Vito Andrea Capozzi, Antonino Abbate, Antonio Simone Laganà, Simone Garzon, and Vito Chiantera. 2022. "Conventional Laparoscopy versus Robotic-Assisted Aortic Lymph-Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 11, no. 12: 3332. https://doi.org/10.3390/jcm11123332
APA StyleDi Donna, M. C., Giallombardo, V., Lo Balbo, G., Cucinella, G., Sozzi, G., Capozzi, V. A., Abbate, A., Laganà, A. S., Garzon, S., & Chiantera, V. (2022). Conventional Laparoscopy versus Robotic-Assisted Aortic Lymph-Nodal Staging for Locally Advanced Cervical Cancer: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 11(12), 3332. https://doi.org/10.3390/jcm11123332








