The Management of Hypertensive Emergencies—Is There a “Magical” Prescription for All?
Abstract
:1. Introduction
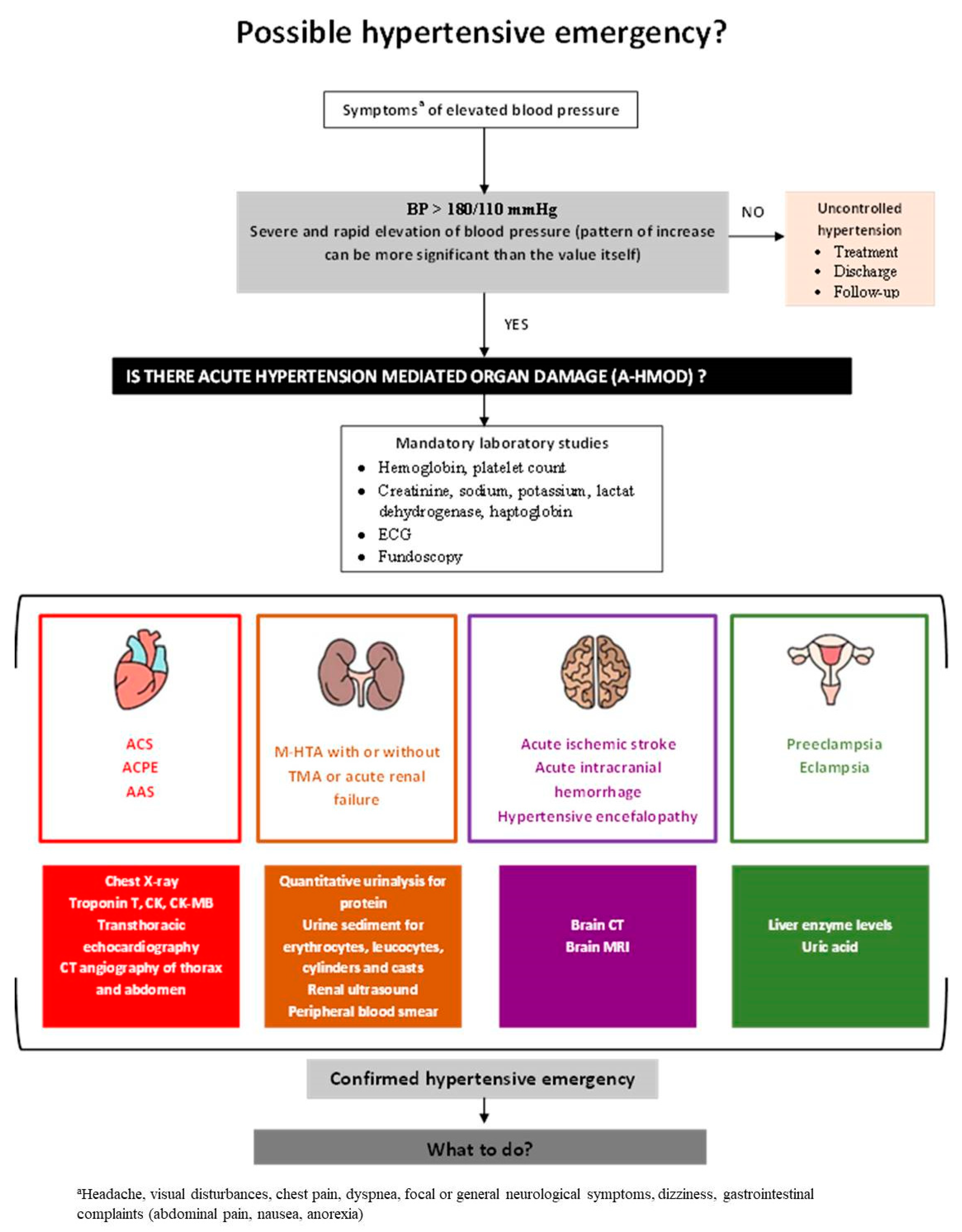
2. Definition and Epidemiology—Setting the Stage
3. Diagnostic Work-Up to Identify Hypertensive Emergencies
4. Management
4.1. General Principles
| Intravenous Antihypertensive Drugs for the Management of Hypertensive Emergencies | ||||
|---|---|---|---|---|
| Drug | Dose | Mechanism of Action | Adverse Effects | Contraindications |
| ESMOLOL | 500 to 1000 μg/kg i.v. bolus in 1 min or 50–250 μg/kg/min continuous i.v. infusion | Cardioselective β1-blocker resulting in decreased cardiac output | Hypotension, Dizziness, Peripheral ischemia, Infusion site reaction, Bradycardia | Sinus bradycardia, Sick sinus syndrome, Second- or third-degree heart block, Heart failure, Cardiogenic shock, Pulmonary hypertension, Asthma, COPD |
| LABETALOL | 0.25–0.5 mg/kg i.v. bolus or 2–4 mg/min i.v. infusion, thereafter 5–20 mg/h | Non-selective α1 and β-adrenergic blocker resulting in decreased cardiac output and direct vasodilation | Symptomatic postural hypotension, Flushing, Acute left ventricular failure, Bronchospasm, Bradycardia | Asthma, Heart failure, Second- or third-degree heart block, Cardiogenic Shock, Severe bradycardia |
| CLEVIDIPINE | 1–2 mg/h i.v. infusion, increase every 2 min with 2 mg/h i.v. bolus or 15–30 mg/min continuous i.v. infusion | Block L-type calcium channels, which leads to coronary and peripheral vasodilation | Systemic hypotension, Reflex tachycardia | Allergies to soybeans, soy products, eggs or egg products, Defective lipid metabolism, Severe aortic stenosis |
| NICARDIPINE | 5 mg/h continuous i.v. infusion, increase dose by 2.5 mg/h every 15 min to a maximum dose of 15 mg/h | Block L-type calcium channels, which leads to coronary and peripheral vasodilation | Dizziness, Flushing, Reflex tahycardia, Nausea, Vomiting, Increased intracranial pressure | Liver failure |
| NITROGLYCERINE | 5–200 μg/min continuous i.v. infusion, increase by 5 μg/min every 5 min | Nitric oxide donor | Headache, Reflex tachycardia, Vomiting, Flushing, Methemoglobinemia, Syncope Venodilator | Known history of increased intracranial pressure, Severe anemia, Right-sided myocardial infarction, Concurrent use with PDE-5 inhibitors |
| NITROPRUSSIDE | 0.25–10 μg/kg/min continuous i.v. infusion, increase by 0.5 μg/kg/min every 5 min to a maximal dose only for 10 min | Nitric oxide donor Direct arterial and venous dilator | Nausea, Vomiting, Muscle twitching, Thiocyanate intoxication, Methemoglobinemia acidosis, Cyanide poisoning | Concurrent use with PDE-5 inhibitors, Septic shock, Vitamin B12 deficiency |
| ENALAPRILAT | 0.625–1.25 mg i.v. bolus every 6 h | Inhibits conversion of angiotensin I to angiotensin II causing vasodilation, reduced aldosterone secretion, inhibiting cardiac and vascular remodeling | Hypotension, Cough, Hyperkaliemia, Cholestatic jaundice | Renal failure in patients with bilateral renal artery stenosis, History of angioedema, Pregnancy and lactation, Acute myocardial infarction |
| CLONIDINE | 150–300 μg i.v. bolus in 5–10 min | Agonist of both imidazoline and α2-adrenergic receptors reducing sympathetic outflow from the vasomotor center in the brain and increasing vagal tone | Sedation, Rebound hypertension | |
| PHENTOLAMINE | 0.5–1 mg/kg i.v. bolus or 50–300 μg/kg/min continuous i.v. infusion | Non-selective α-adrenergic blocker | Tachyarrhythmias, Orthostatic hypotension, Chest pain | |
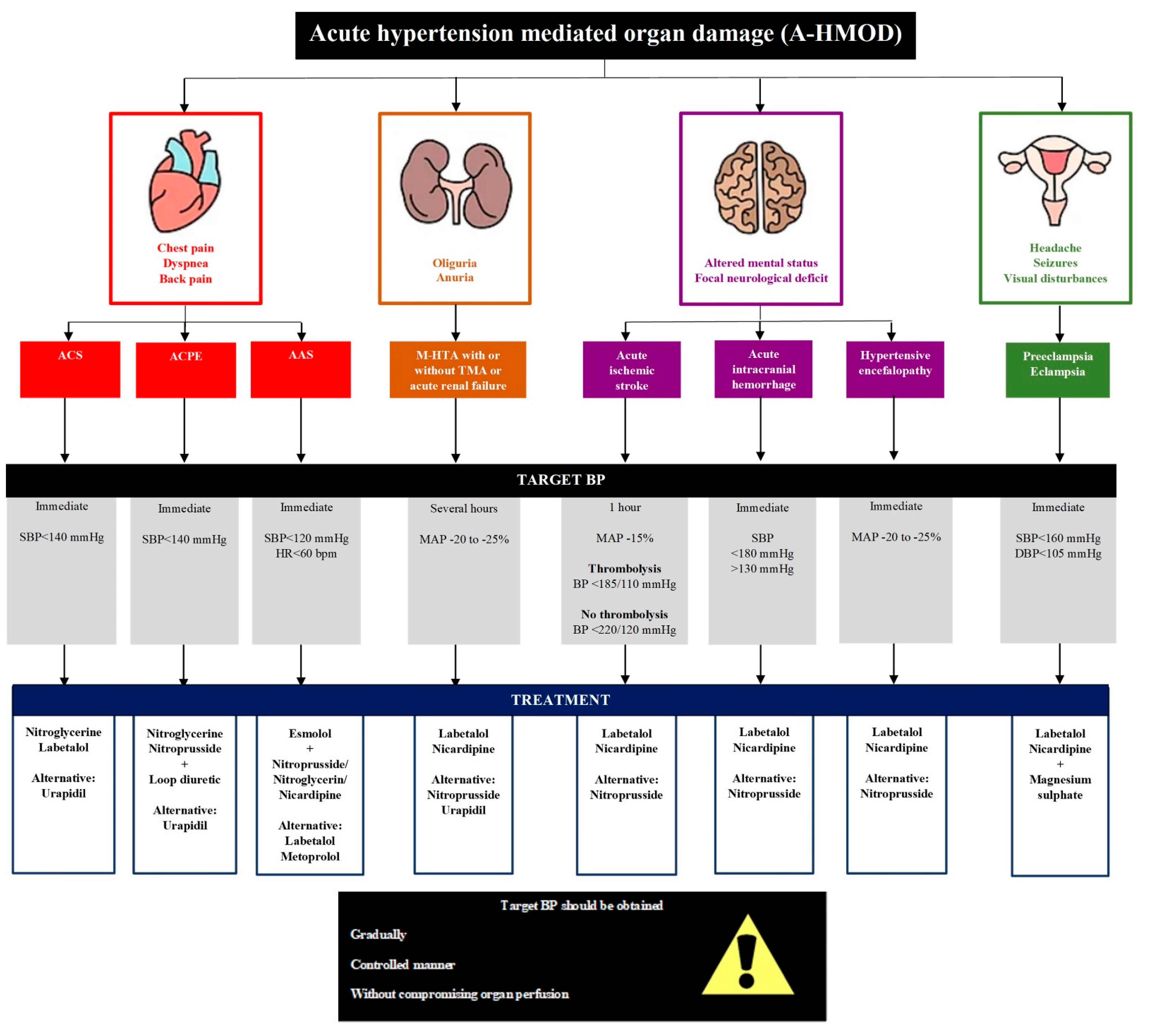
4.2. Hypertensive Encefalopathy
4.3. Acute Ischemic Stroke
4.4. Acute Intracranial Hemorrhage
4.5. Acute Coronary Syndrome
4.6. Acute Cardiogenic Pulmonary Oedema
4.7. Acute Aortic Syndrome
4.8. Thrombotic Microangiopathy and Acute Renal Failure
4.9. Eclampsia and Severe Pre-Eclampsia
4.10. Pheocromocytoma/Paraganglioma (PPGL)
4.11. Acute Perioperative Hypertension and Postoperative Surgical Hypertension
4.12. Hypertension with Retinopathy
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Johnson, W.; Nguyen, M.L.; Patel, R. Hypertension Crisis in the Emergency Department. Cardiol. Clin. 2012, 30, 533–543. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.; McNaughton, C.; Joyce, K.; Binz, S.; Levy, P. Hypertension Management in Emergency Departments. Am. J. Hypertens. 2020, 33, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Adebayo, O.; Rogers, R.L. Hypertensive Emergencies in the Emergency Department. Emerg. Med. Clin. N. Am. 2015, 33, 539–551. [Google Scholar] [CrossRef] [PubMed]
- Whelton, P.K.; Carey, R.M.; Aronow, W.S.; Casey, D.E., Jr.; Collins, K.J.; Dennison Himmelfarb, C.; DePalma, S.M.; Gidding, S.; Jamerson, K.A.; Jones, D.W.; et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American college of cardiology/American Heart Association task. Hypertension 2018, 71, 1269–1324. [Google Scholar] [CrossRef] [PubMed]
- Muiesan, M.L.; Salvetti, M.; Amadoro, V.; Di Somma, S.; Perlini, S.; Semplicini, A.; Borghi, C.; Volpe, M.; Saba, P.S.; Cameli, M.; et al. An update on hypertensive emergencies and urgencies. J. Cardiovasc. Med. 2015, 16, 372–382. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tocci, G.; Presta, V.; Volpe, M. Hypertensive crisis management in the emergency room: Time to change? J. Hypertens. 2020, 38, 33–34. [Google Scholar] [CrossRef]
- Balahura, A.M.; Mihailescu, A.M.; Weias, E.A.; Badila, E.; Bartos, D. Hypertensive Crises At the Emergency Room—Who Are the Patients? A Tertiary Center Experience. J. Hypertens. 2019, 37, e75. [Google Scholar] [CrossRef]
- Tocci, G.; Sciarretta, S.; Volpe, M. Development of heart failure in recent hypertension trials. J. Hypertens. 2008, 26, 1477–1486. [Google Scholar] [CrossRef]
- Keith, N.M. Some different types of essential hypertension: Their course and prognosis. Am. J. Med. Sci. 1974, 268, 336–345. [Google Scholar] [CrossRef]
- van den Born, B.-J.H.; Lip, G.Y.H.; Brguljan-Hitij, J.; Cremer, A.; Segura, J.; Morales, E.; Mahfoud, F.; Amraoui, F.; Persu, A.; Kahan, T.; et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur. Hear. J. Cardiovasc. Pharm. 2019, 5, 37–46. [Google Scholar] [CrossRef] [Green Version]
- Papadopoulos, D.P.; Sanidas, E.A.; Viniou, N.A.; Gennimata, V.; Chantziara, V.; Barbetseas, I.; Makris, T.K. Cardiovascular Hypertensive Emergencies. Curr. Hypertens. Rep. 2015, 17, 5. [Google Scholar] [CrossRef] [PubMed]
- Peacock, F.; Amin, A.; Granger, C.B.; Pollack, C.V.; Levy, P.; Nowak, R.; Kleinschmidt, K.; Varon, J.; Wyman, A.; Gore, J.M. Hypertensive heart failure: Patient characteristics, treatment, and outcomes. Am. J. Emerg. Med. 2011, 29, 855–862. [Google Scholar] [CrossRef] [PubMed]
- Manning, L.; Robinson, T.G.; Anderson, C.S. Control of blood pressure in hypertensive neurological emergencies. Curr. Hypertens. Rep. 2014, 16, 436. [Google Scholar] [CrossRef] [PubMed]
- Perez, M.I.; Musini, V.M. Pharmacological interventions for hypertensive emergencies: A Cochrane systematic review. J. Hum. Hypertens. 2008, 22, 596–607. [Google Scholar] [CrossRef] [PubMed]
- Sharma, K.; Mathews, E.P.; Newton, F. CE: Hypertensive Emergencies: A Review. Am. J. Nurs. 2021, 121, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart disease and stroke statistics—2018 update: A report from the American Heart Association. Circulation 2018, 137, 67–492. [Google Scholar] [CrossRef]
- Shorr, A.F.; Zilberberg, M.D.; Sun, X.; Johannes, R.S.; Gupta, V.; Tabak, Y.P. Severe acute hypertension among inpatients admitted from the emergency department. J. Hosp. Med. 2012, 7, 203–210. [Google Scholar] [CrossRef] [Green Version]
- Zampaglione, B.; Pascale, C.; Marchisio, M.; Cavallo-Perin, P. Hypertensive urgencies and emergencies. Prevalence and clinical presentation. Hypertension 1996, 27, 144–147. [Google Scholar] [CrossRef]
- Hannemann, A.; Friedrich, N.; Lüdemann, J.; Völzke, H.; Rettig, R.; Peters, J.; Reincke, M.; Döring, A.; Nauck, M.; Wallaschofski, H. Reference intervals for aldosterone, renin, and the aldosterone-to-renin ratio in the population-based study of health in pomerania (SHIP-1). Horm. Metab. Res. 2010, 42, 392–399. [Google Scholar] [CrossRef]
- Janke, A.T.; McNaughton, C.D.; Brody, A.M.; Welch, R.D.; Levy, P.D. Trends in the incidence of hypertensive emergencies in us emergency departments from 2006 to 2013. J. Am. Heart Assoc. 2016, 5, e004511. [Google Scholar] [CrossRef]
- Vilela Martin, J.F.; Higashiama, É.; Garcia, E.; Luizon, M.R.; Cipullo, J.P. Hypertensive crisis profile. Prevalence and clinical presentation. Arq. Bras. Cardiol. 2004, 83, 125–136. [Google Scholar]
- Polgreen, L.A.; Suneja, M.; Tang, F.; Carter, B.L.; Polgreen, P.M. Increasing trend in admissions for malignant hypertension and hypertensive encephalopathy in the United States. Hypertension 2015, 65, 1002–1007. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Salvetti, M.; Paini, A.; Colonetti, E.; Tarozzi, L.; Bertacchini, F.; Aggiusti, C.; Stassaldi, D.; Rosei, C.A.; Rosei, E.A.; Muiesan, M.L. Hypertensive emergencies and urgencies: A single-centre experience in Northern Italy 2008–2015. J. Hypertens. 2020, 38, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Kotruchin, P.; Mitsungnern, T.; Ruangsaisong, R.; Imoun, S.; Pongchaiyakul, C. Hypertensive Urgency Treatment and Outcomes in a Northeast Thai Population: The Results from the Hypertension Registry Program. High Blood Press. Cardiovasc. Prev. 2018, 25, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Leiba, A.; Cohen-Arazi, O.; Mendel, L.; Holtzman, E.J.; Grossman, E. Incidence, aetiology and mortality secondary to hypertensive emergencies in a large-scale referral centre in Israel (1991–2010). J. Hum. Hypertens. 2016, 30, 498–502. [Google Scholar] [CrossRef]
- Saguner, A.M.; Dür, S.; Perrig, M.; Schiemann, U.; Stuck, A.E.; Bürgi, U.; Erne, P.; Schoenenberger, A.W. Risk factors promoting hypertensive crises: Evidence from a longitudinal study. Am. J. Hypertens. 2010, 23, 775–780. [Google Scholar] [CrossRef]
- Guiga, H.; Decroux, C.; Michelet, P.; Loundou, A.; Cornand, D.; Silhol, F.; Vaisse, B.; Sarlon-Bartoli, G. Hospital and out-of-hospital mortality in 670 hypertensive emergencies and urgencies. J. Clin. Hypertens. 2017, 19, 1137–1142. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Simek, S.; Garg, N.; Vaduganathan, M.; Kaiksow, F.; Stein, J.H.; Fonarow, G.C.; Pandey, A.; Bhatt, D.L. Thirty-Day Readmissions after Hospitalization for Hypertensive Emergency. Hypertension 2019, 73, 60–67. [Google Scholar] [CrossRef]
- Marik, P.E.; Rivera, R. Hypertensive emergencies: An update. Curr. Opin. Crit. Care 2011, 17, 569–580. [Google Scholar] [CrossRef]
- Miller, J.B.; Suchdev, K.; Jayaprakash, N.; Hrabec, D.; Sood, A.; Sharma, S.; Levy, P.D. New developments in hypertensive encephalopathy. Curr. Hypertens. Rep. 2018, 20, 13. [Google Scholar] [CrossRef]
- Karras, D.J.; Kruus, L.K.; Cienki, J.J.; Wald, M.M.; Chiang, W.K.; Shayne, P.; Ufberg, J.W.; Harrigan, R.A.; Wald, D.A.; Heilpern, K.L. Evaluation and treatment of patients with severely elevated blood pressure in academic emergency departments: A multicenter study. Ann. Emerg. Med. 2006, 47, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; de Simone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. J. Hypertens. 2018, 36, 1953–2041. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vidt, D.G. Emergency room management of hypertensive urgencies and emergencies. J. Clin. Hypertens. 2001, 3, 158–164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Udeh, C.I.; Ting, M.; Arango, M.; Mick, S. Delayed presentation of nitroprusside-induced cyanide toxicity. Ann. Thorac. Surg. 2015, 99, 1432–1434. [Google Scholar] [CrossRef]
- Miller, J.B.; Kinni, H.; Amer, A.; Levy, P.D. Therapies to Reduce Blood Pressure Acutely. Curr. Hypertens. Rep. 2016, 18, 43. [Google Scholar] [CrossRef] [PubMed]
- Ipek, E.; Oktay, A.A.; Krim, S.R. Hypertensive crisis: An update on clinical approach and management. Curr. Opin. Cardiol. 2017, 32, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Behl, T.; Kaur, I.; Sehgal, A.; Singh, S.; Bhatia, S.; Al-Harrasi, A.; Zengin, G.; Babes, E.; Brisc, C.; Stoicescu, M.; et al. Bioinformatics accelerates the major tetrad: A real boost for the pharmaceutical industry. Int. J. Mol. Sci. 2021, 22, 6184. [Google Scholar] [CrossRef] [PubMed]
- Malesker, M.A.; Hilleman, D.E. Intravenous labetalol compared with intravenous nicardipine in the management of hypertension in critically Ill patients. J. Crit. Care 2012, 27, 528.e7–528.e14. [Google Scholar] [CrossRef] [PubMed]
- Liu-DeRyke, X.; Janisse, J.; Coplin, W.M.; Parker, D.; Norris, G.; Rhoney, D.H. A comparison of nicardipine and labetalol for acute hypertension management following stroke. Neurocrit. Care 2008, 9, 167–176. [Google Scholar] [CrossRef] [PubMed]
- Liu-Deryke, X.; Levy, P.D.; Parker, D.; Coplin, W.; Rhoney, D.H. A prospective evaluation of labetalol versus nicardipine for blood pressure management in patients with acute stroke. Neurocrit. Care 2013, 19, 41–47. [Google Scholar] [CrossRef]
- Immink, R.V.; Van Den Born, B.J.H.; Van Montfrans, G.A.; Kim, Y.S.; Hollmann, M.W.; Van Lieshout, J.J. Cerebral hemodynamics during treatment with sodium nitroprusside versus labetalol in malignant hypertension. Hypertension 2008, 52, 236–240. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peacock, W.F.; Varon, J.; Baumann, B.M.; Borczuk, P.; Cannon, C.M.; Chandra, A.; Cline, D.M.; Diercks, D.; Hiestand, B.; Hsu, A.; et al. CLUE: A randomized comparative effectiveness trial of IV nicardipine versus labetalol uwse in the emergency department. Crit. Care 2011, 15, R157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fugate, J.E.; Rabinstein, A.A. Posterior reversible encephalopathy syndrome: Clinical and radiological manifestations, pathophysiology, and outstanding questions. Lancet Neurol. 2015, 14, 914–925. [Google Scholar] [CrossRef]
- Gierthmühlen, J.; Allardt, A.; Sawade, M.; Wasner, G.; Baron, R. Role of sympathetic nervous system in activity-induced cerebral perfusion. J. Neurol. 2010, 257, 1798–1805. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Rossitto, G.; Maifredini, C.; Barchitta, A.; Bettella, A.; Latella, R.; Ruzza, L.; Sabini, B.; Seccia, T.M. Management of hypertensive emergencies: A practical approach. Blood Press. 2021, 30, 208–219. [Google Scholar] [CrossRef]
- Legriel, S.; Schraub, O.; Azoulay, E.; Hantson, P.; Magalhaes, E.; Coquet, I.; Bretonniere, C.; Gilhodes, O.; Anguel, N.; Mégarbane, B.; et al. Determinants of Recovery from Severe Posterior Reversible Encephalopathy Syndrome. PLoS ONE 2012, 7, e44534. [Google Scholar] [CrossRef]
- Bulwa, Z.; Gomez, C.R.; Morales-Vidal, S.; Biller, J. Management of Blood Pressure After Acute Ischemic Stroke. Curr. Neurol. Neurosci. Rep. 2019, 19, 29. [Google Scholar] [CrossRef]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke A. Stroke 2019, 50, 344–418. [Google Scholar] [CrossRef]
- Ahmed, N.; Nasman, P.; Wahlgren, N.G. Effect of Intravenous Nimodipine on Blood Pressure and Outcome After Acute Stroke. Stroke 2000, 31, 1250–1255. [Google Scholar] [CrossRef] [PubMed]
- Kaste, M.; Fogelholm, R.; Erilä, T.; Palomäki, H.; Murros, K.; Rissanen, A.; Sarna, S. A randomized, double-blind, placebo-controlled trial of nimodipine in acute ischemic hemispheric stroke. Stroke 1994, 25, 1348–1353. [Google Scholar] [CrossRef] [Green Version]
- Sandset, E.C.; Anderson, C.S.; Bath, P.M.; Christensen, H.; Fischer, U.; Gąsecki, D.; Lal, A.; Manning, L.S.; Sacco, S.; Steiner, T.; et al. European Stroke Organisation (ESO) guidelines on blood pressure management in acute ischaemic stroke and intracerebral haemorrhage. Eur. Stroke J. 2021, 6, XLVIII–LXXXIX. [Google Scholar] [CrossRef] [PubMed]
- Anadani, M.; Arthur, A.S.; Tsivgoulis, G.; Simpson, K.N.; Alawieh, A.; Orabi, Y.; Goyal, N.; Alexandrov, A.V.; Maier, I.L.; Psychogios, M.; et al. Blood Pressure Goals and Clinical Outcomes after Successful Endovascular Therapy: A Multicenter Study. Ann. Neurol. 2020, 87, 830–839. [Google Scholar] [CrossRef] [PubMed]
- Gross, H.; Grose, N. Emergency Neurological Life Support: Acute Ischemic Stroke. Neurocrit. Care 2017, 27, 102–115. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.S.; Heeley, E.; Huang, Y.; Wang, J.; Stapf, C.; Delcourt, C.; Lindley, R.; Robinson, T.; Lavados, P.; Neal, B.; et al. Rapid Blood-Pressure Lowering in Patients with Acute Intracerebral Hemorrhage. N. Engl. J. Med. 2013, 368, 2355–2365. [Google Scholar] [CrossRef] [PubMed]
- Qureshi, A.; Palesch, Y.Y.; Barsan, W.G.; Hanley, D.F.; Hsu, C.Y.; Martin, R.L.; Moy, C.S.; Silbergleit, R.; Steiner, T.; Suarez, J.I.; et al. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N. Engl. J. Med. 2016, 375, 1033–1043. [Google Scholar] [CrossRef] [PubMed]
- Lattanzi, S.; Silvestrini, M. Optimal achieved blood pressure in acute intracerebral hemorrhage: INTERACT2. Neurology 2015, 85, 557–558. [Google Scholar] [CrossRef] [Green Version]
- Suri, M.F.K.; Vazquez, G.; Ezzeddine, M.A.; Qureshi, A.I. A multicenter comparison of outcomes associated with intravenous nitroprusside and nicardipine treatment among patients with intracerebral hemorrhage. Neurocrit. Care 2009, 11, 50–55. [Google Scholar] [CrossRef] [Green Version]
- Pattanshetty, D.J.; Bhat, P.K.; Aneja, A.; Pillai, D.P. Elevated troponin predicts long-term adverse cardiovascular outcomes in hypertensive crisis: A retrospective study. J. Hypertens. 2012, 30, 2410–2415. [Google Scholar] [CrossRef]
- Rosendorff, C.; Lackland, D.T.; Allison, M.; Aronow, W.S.; Black, H.R.; Blumenthal, R.S.; Cannon, C.P.; de Lemos, J.A.; Elliott, W.J.; Findeiss, L.; et al. Treatment of hypertension in patients with coronary artery disease: A scientific statement from the American Heart Association, American College of Cardiology, and American Society of Hypertension. J. Am. Coll. Cardiol. 2015, 65, 1998–2038. [Google Scholar] [CrossRef] [Green Version]
- Collet, J.-P.; Thiele, H.; Barbato, E.; Barthélémy, O.; Bauersachs, J.; Bhatt, D.L.; Dendale, P.; Dorobantu, M.; Edvardsen, T.; Folliguet, T.; et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2021, 42, 1289–1367. [Google Scholar] [CrossRef]
- Chiariello, M.; Gold, H.K.; Leinbach, R.C.; Davis, M.A.; Maroko, P.R. Comparison between the effects of nitroprusside and nitroglycerin on ischemic injury during acute myocardial infarction. Circulation 1976, 54, 766–773. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yao, D.-K.; Jia, S.-Q.; Wang, L.; Li, H.-W.; Zhang, Y.-C.; Wang, Y.-L.; Wang, L.-X. Therapeutic effect of urapidil on myocardial perfusion in patients with ST-elevation acute coronary syndrome. Eur. J. Intern. Med. 2009, 20, 152–157. [Google Scholar] [CrossRef] [PubMed]
- Peacock, W.F.; Chandra, A.; Char, D.; Collins, S.; Der Sahakian, G.; Ding, L.; Dunbar, L.; Fermann, G.; Fonarow, G.; Garrison, N.; et al. Clevidipine in acute heart failure: Results of the A Study of Blood Pressure Control in Acute Heart Failure—A Pilot Study (PRONTO). Am.Heart J. 2014, 167, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Schreiber, W.; Woisetschläger, C.; Binder, M.; Kaff, A.; Raab, H.; Hirschl, M.M. The nitura study—Effect of nitroglycerin or urapidil on hemodynamic, metabolic and respiratory parameters in hypertensive patients with pulmonary edema. Intensive Care Med. 1998, 24, 557–563. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Kim, J.G.; Lim, Y.S.; Ryoo, E.; Hyun, S.Y.; Lee, G. Nicardipine versus nitroprusside infusion as antihypertensive therapy in hypertensive emergencies. J. Int. Med. Res. 2004, 32, 118–123. [Google Scholar] [CrossRef]
- Gawinecka, J.; Schönrath, F.; von Eckardstein, A. Acute aortic dissection: Pathogenesis, risk factors and diagnosis. Swiss Med. Wkly. 2017, 147, w14489. [Google Scholar] [CrossRef]
- Hagan, P.G.; Nienaber, C.A.; Isselbacher, E.M.; Bruckman, D.; Karavite, D.J.; Russman, P.L.; Evangelista, A.; Fattori, R.; Suzuki, T.; Oh, J.K.; et al. The International Registry of Acute Aortic Dissection (IRAD). JAMA 2000, 283, 897. [Google Scholar] [CrossRef]
- Morello, F.; Santoro, M.; Fargion, A.T.; Grifoni, S.; Nazerian, P. Diagnosis and management of acute aortic syndromes in the emergency department. Intern. Emerg. Med. 2021, 16, 171–181. [Google Scholar] [CrossRef]
- Hiratzka, L.F.; Bakris, G.L.; Beckman, J.A.; Bersin, R.M.; Carr, V.F.; Casey, D.E., Jr.; Eagle, K.; Hermann, L.K.; Isselbacher, E.M.; Kazerooni, E.A.; et al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: Executive summary: A report of the american college of cardiology foundation/american heart association task force on pra. Circulation 2010, 121, 266–369. [Google Scholar] [CrossRef]
- Suzuki, T.; Isselbacher, E.M.; Nienaber, C.A.; Pyeritz, R.E.; Eagle, K.A.; Tsai, T.T.; Cooper, J.V.; Januzzi, J.L.; Braverman, A.C.; Montgomery, D.G.; et al. Type-selective benefits of medications in treatment of acute aortic dissection (from the International Registry of Acute Aortic Dissection [IRAD]). Am. J. Cardiol. 2012, 109, 122–127. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Beevers, M.; Beevers, D.G. Do patients with de novo hypertension differ from patients with previously known hypertension when Malignant phase hypertension occurs? Am. J. Hypertens. 2000, 13, 934–939. [Google Scholar] [CrossRef] [Green Version]
- Shantsila, A.; Shantsila, E.; Beevers, D.G.; Lip, G.Y.H. Predictors of 5-year outcomes in malignant phase hypertension: The West Birmingham Malignant Hypertension Registry. J. Hypertens. 2017, 35, 2310–2314. [Google Scholar] [CrossRef] [PubMed]
- Sukumar, S.; Lämmle, B.; Cataland, S.R. Thrombotic thrombocytopenic purpura: Pathophysiology, diagnosis, and management. J. Clin. Med. 2021, 10, 536. [Google Scholar] [CrossRef] [PubMed]
- Sheerin, N.S.; Glover, E. Haemolytic uremic syndrome: Diagnosis and management [version 1; peer review: 3 approved]. F1000Research 2019, 8. [Google Scholar] [CrossRef] [PubMed]
- Rubin, S.; Cremer, A.; Boulestreau, R.; Rigothier, C.; Kuntz, S.; Gosse, P. Malignant hypertension: Diagnosis, treatment and prognosis with experience from the Bordeaux cohort. J. Hypertens. 2019, 37, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Steegers, E.A.P.; Von Dadelszen, P.; Duvekot, J.J.; Pijnenborg, R. Pre-eclampsia. Lancet 2010, 376, 631–644. [Google Scholar] [CrossRef]
- Brown, M.A.; Magee, L.A.; Kenny, L.C.; Karumanchi, S.A.; McCarthy, F.P.; Saito, S.; Hall, D.R.; Warren, C.E.; Adoyi, G.; Ishaku, S.; et al. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 2018, 72, 24–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rezk, M.; Gamal, A.; Emara, M. Maternal and fetal outcome in de novo preeclampsia in comparison to superimposed preeclampsia: A two-year observational study. Hypertens. Pregnancy 2015, 34, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Pregnancy, H.D. INTERIM UPDATE Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period. Obstet. Gynecol. 2019, 133, 2017–2020. [Google Scholar]
- Awaludin, A.; Rahayu, C.; Daud, N.A.A.; Zakiyah, N. Antihypertensive Medications for Severe Hypertension in Pregnancy: A Systematic Review and Meta-Analysis. Healthcare 2022, 10, 325. [Google Scholar] [CrossRef]
- Alavifard, S.; Chase, R.; Janoudi, G.; Chaumont, A.; Lanes, A.; Walker, M.; Gaudet, L. First-line antihypertensive treatment for severe hypertension in pregnancy: A systematic review and network meta-analysis. Pregnancy Hypertens. 2019, 18, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Lenders, J.W.M.; Kerstens, M.N.; Amar, L.; Prejbisz, A.; Robledo, M.; Taieb, D.; Pacak, K.; Crona, J.; Zelinka, T.; Mannelli, M.; et al. Genetics, diagnosis, management and future directions of research of phaeochromocytoma and paraganglioma: A position statement and consensus of the Working Group on Endocrine Hypertension of the European Society of Hypertension. J. Hypertens. 2020, 38, 1443–1456. [Google Scholar] [CrossRef] [PubMed]
- Bravo, E.; Fouad-Tarazi, F.; Rossi, G.; Imamura, M.; Lin, W.W.; A Madkour, M.; Wicker, P.; Cressman, M.D.; Saragoca, M. A reevaluation of the hemodynamics of pheochromocytoma. Hypertension 1990, 15, I-128–I-131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aronson, S. Perioperative hypertensive emergencies. Curr. Hypertens. Rep. 2014, 16, 448. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, A.; Ripollés–Melchor, J.; Casans-Francés, R.; Abad-Gurumeta, A.; Bergese, S.D.; Zuleta-Alarcon, A.; López-Timoneda, F.; Calvo-Vecino, J.M.; Evidence Anesthesia Review Group. Perioperative use of clevidipine: A systematic review and meta-analysis. PLoS ONE 2016, 11, e0150625. [Google Scholar] [CrossRef] [PubMed]
- Aronson, S.; Dyke, C.M.; Stierer, K.A.; Levy, J.H.; Cheung, A.T.; Lumb, P.D.; Kereiakes, D.J.; Newman, M.F. The ECLIPSE trials: Comparative studies of clevidipine to nitroglycerin, sodium nitroprusside, and nicardipine for acute hypertension treatment in cardiac surgery patients. Anesth. Analg. 2008, 107, 1110–1121. [Google Scholar] [CrossRef] [PubMed]
- Blessberger, H.; Lewis, S.R.; Pritchard, M.W.; Fawcett, L.J.; Domanovits, H.; Schlager, O.; Wildner, B.; Kammler, J.; Steinwender, C. Perioperative beta-blockers for preventing surgery-related mortality and morbidity in adults undergoing non-cardiac surgery. Cochrane Database Syst. Rev. 2019, 9, 013483. [Google Scholar] [CrossRef]
- Kabedi, N.N.; Mwanza, J.C.; Lepira, F.B.; Kayembe, T.K.; Kayembe, D.L. Hypertensive retinopathy and its association with cardiovascular, renaland cerebrovascular morbidity in Congolese patients. Cardiovasc. J. Afr. 2014, 25, 228–232. [Google Scholar] [CrossRef] [Green Version]
- Erden, S.; Bicakci, E. Hypertensive retinopathy: Incidence, risk factors, and comorbidities. Clin. Exp. Hypertens. 2012, 34, 397–401. [Google Scholar] [CrossRef]
- Rossi, G.P.; Ceolotto, G.; Rossitto, G.; Seccia, T.M.; Maiolino, G.; Berton, C.; Basso, D.; Plebani, M. Prospective validation automated chemiluminescencebased assay of renin and aldosterone for the workup of arterial hypertension. Clin. Chem. Lab. Med. 2016, 54, 1441–1450. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Balahura, A.-M.; Moroi, Ș.-I.; Scafa-Udrişte, A.; Weiss, E.; Japie, C.; Bartoş, D.; Bădilă, E. The Management of Hypertensive Emergencies—Is There a “Magical” Prescription for All? J. Clin. Med. 2022, 11, 3138. https://doi.org/10.3390/jcm11113138
Balahura A-M, Moroi Ș-I, Scafa-Udrişte A, Weiss E, Japie C, Bartoş D, Bădilă E. The Management of Hypertensive Emergencies—Is There a “Magical” Prescription for All? Journal of Clinical Medicine. 2022; 11(11):3138. https://doi.org/10.3390/jcm11113138
Chicago/Turabian StyleBalahura, Ana-Maria, Ștefan-Ionuț Moroi, Alexandru Scafa-Udrişte, Emma Weiss, Cristina Japie, Daniela Bartoş, and Elisabeta Bădilă. 2022. "The Management of Hypertensive Emergencies—Is There a “Magical” Prescription for All?" Journal of Clinical Medicine 11, no. 11: 3138. https://doi.org/10.3390/jcm11113138
APA StyleBalahura, A.-M., Moroi, Ș.-I., Scafa-Udrişte, A., Weiss, E., Japie, C., Bartoş, D., & Bădilă, E. (2022). The Management of Hypertensive Emergencies—Is There a “Magical” Prescription for All? Journal of Clinical Medicine, 11(11), 3138. https://doi.org/10.3390/jcm11113138






