Single or Double Plating for Acromial Type III Fractures: Biomechanical Comparison of Load to Failure and Fragment Motion
Abstract
:1. Introduction
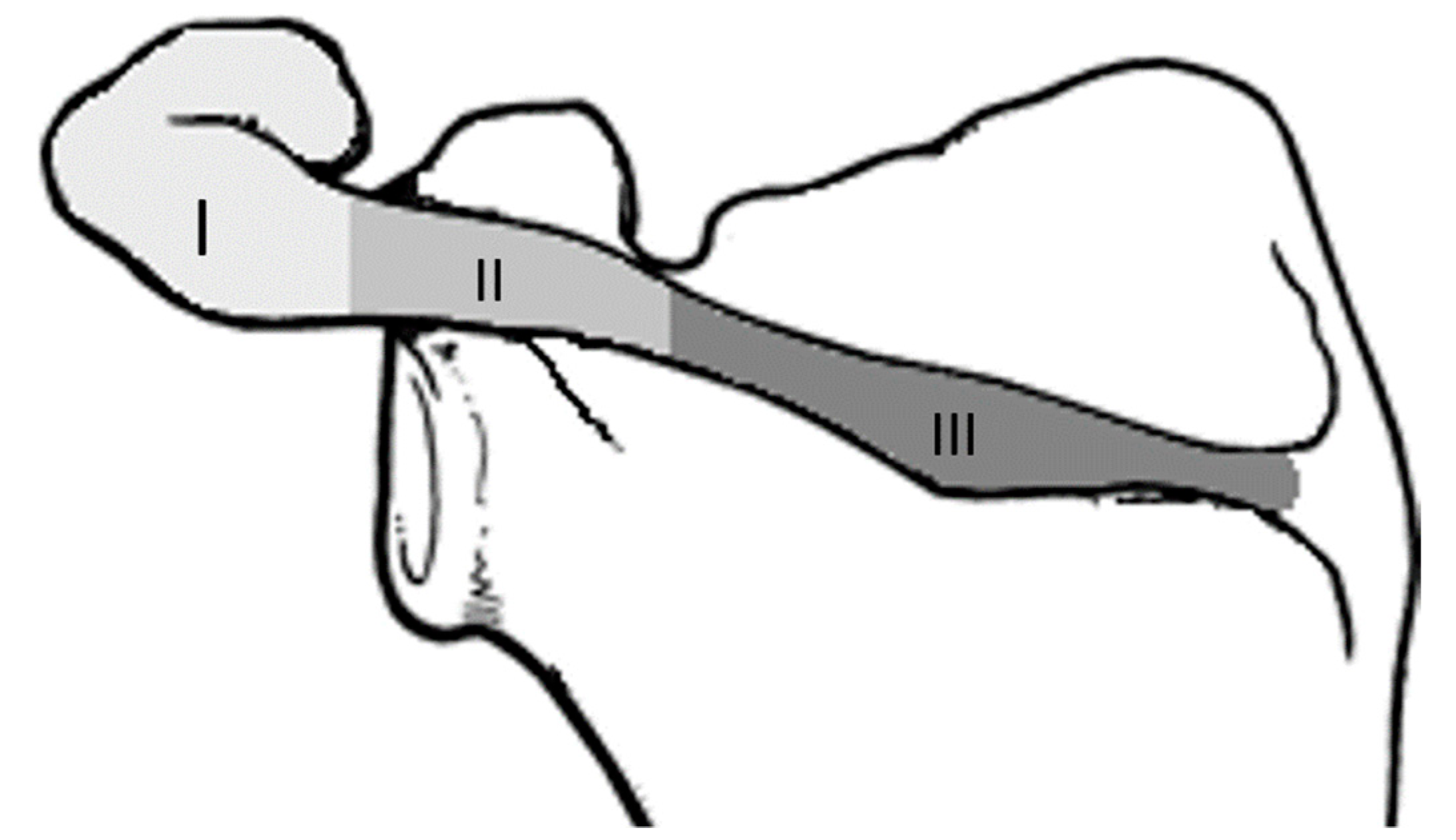
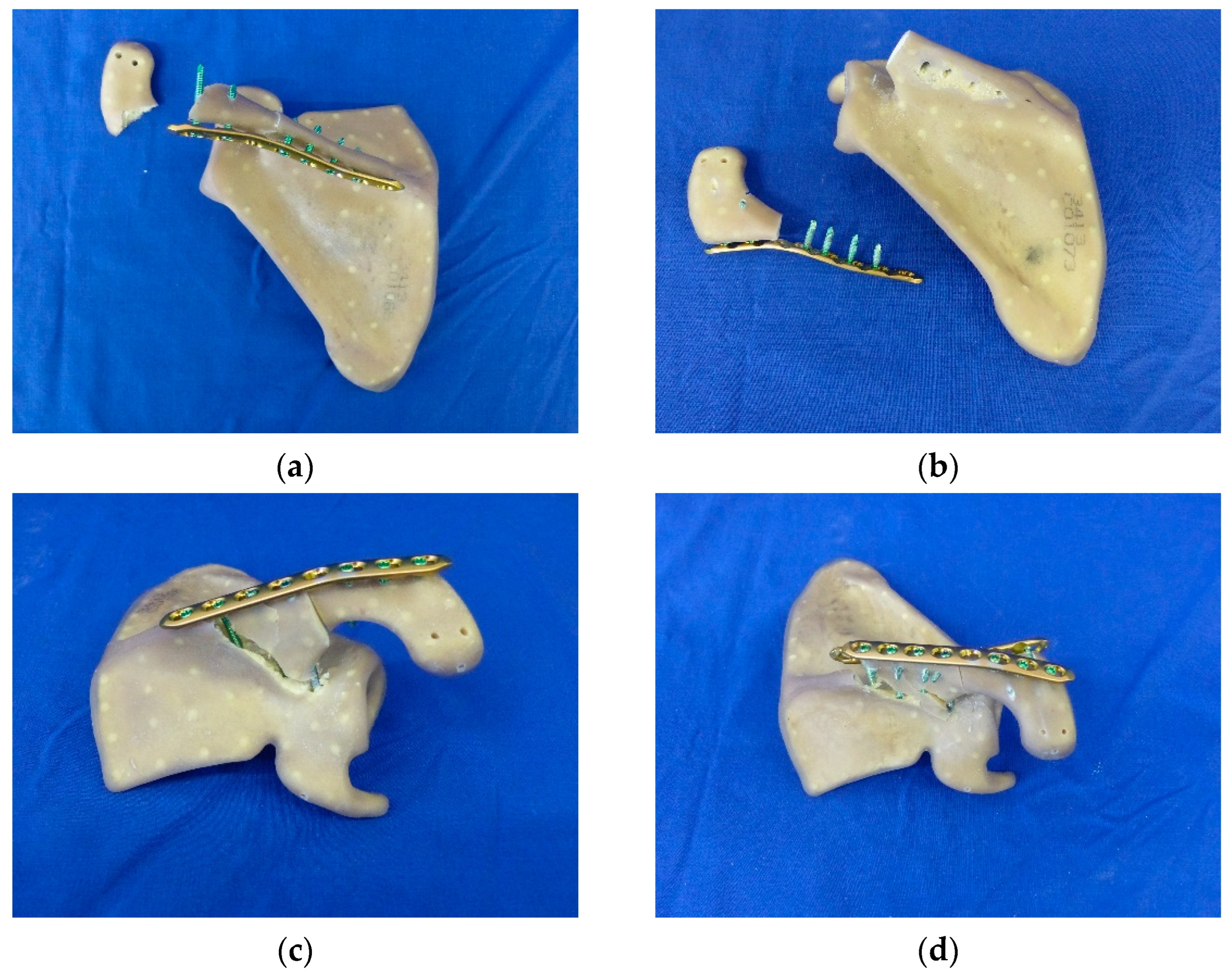
2. Materials and Methods
2.1. Specimen Preparation
2.2. Biomechanical Testing
2.3. Statistical Analysis
3. Results
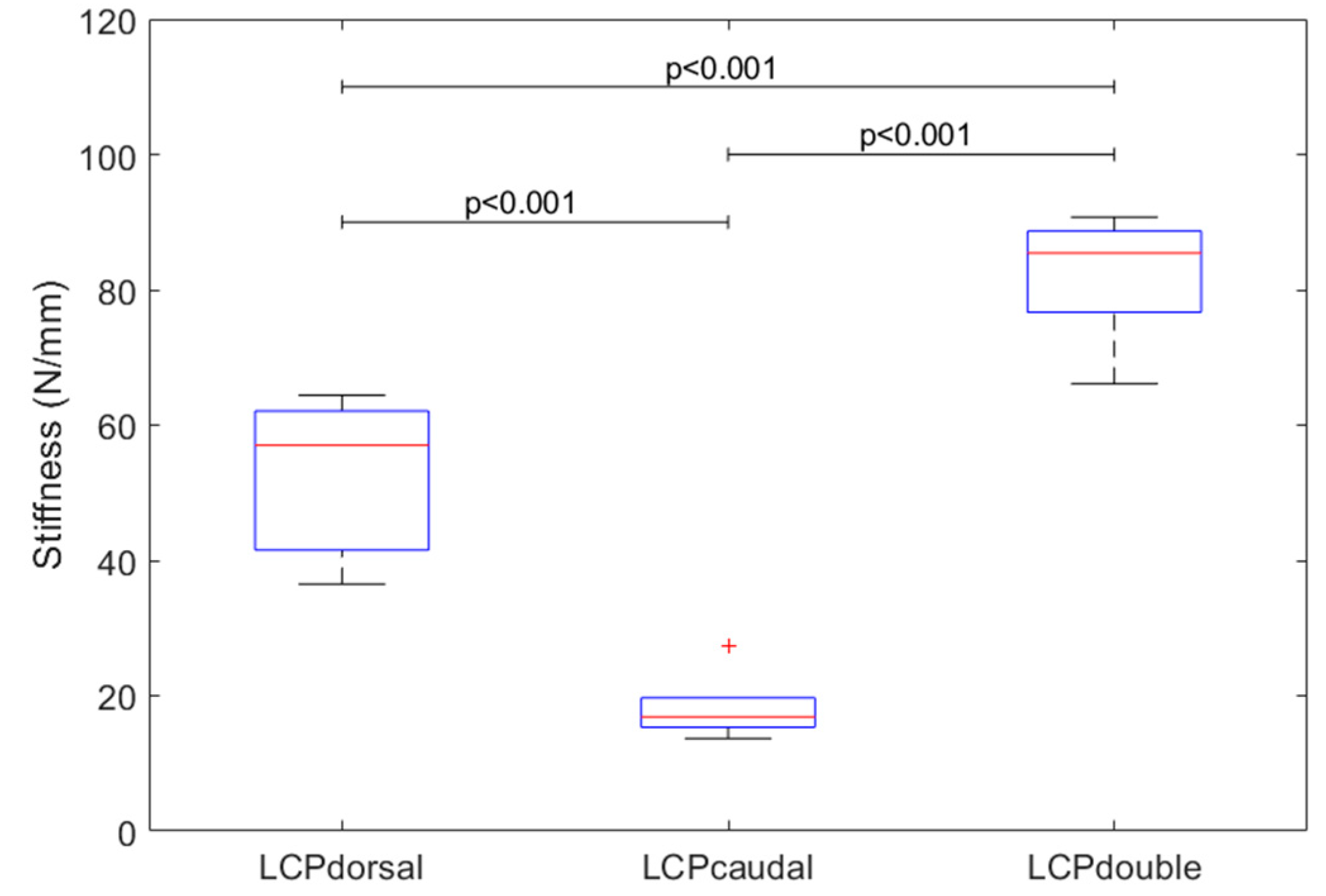
3.1. Stiffness of Constructs
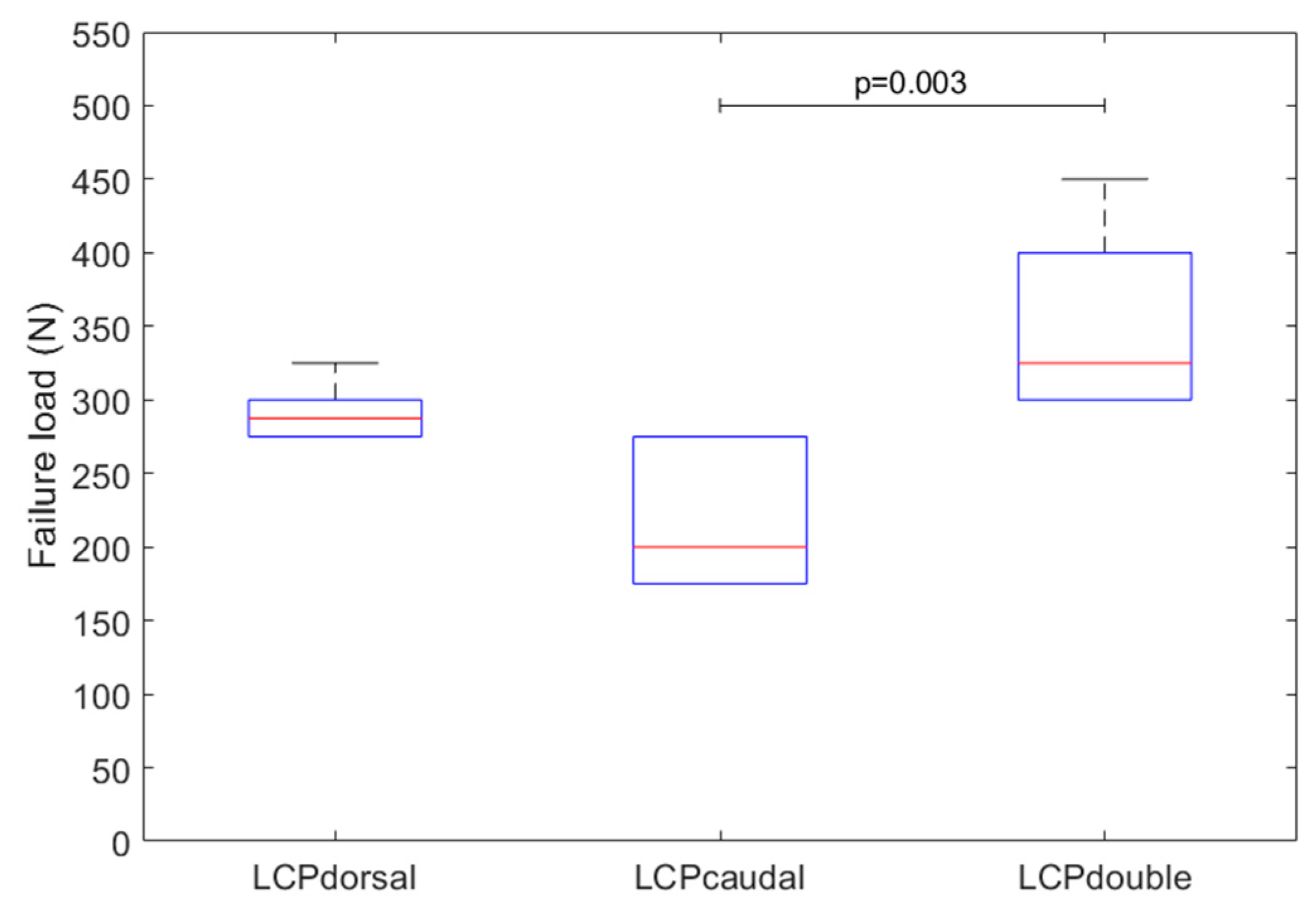
3.2. Failure Load and Cycles
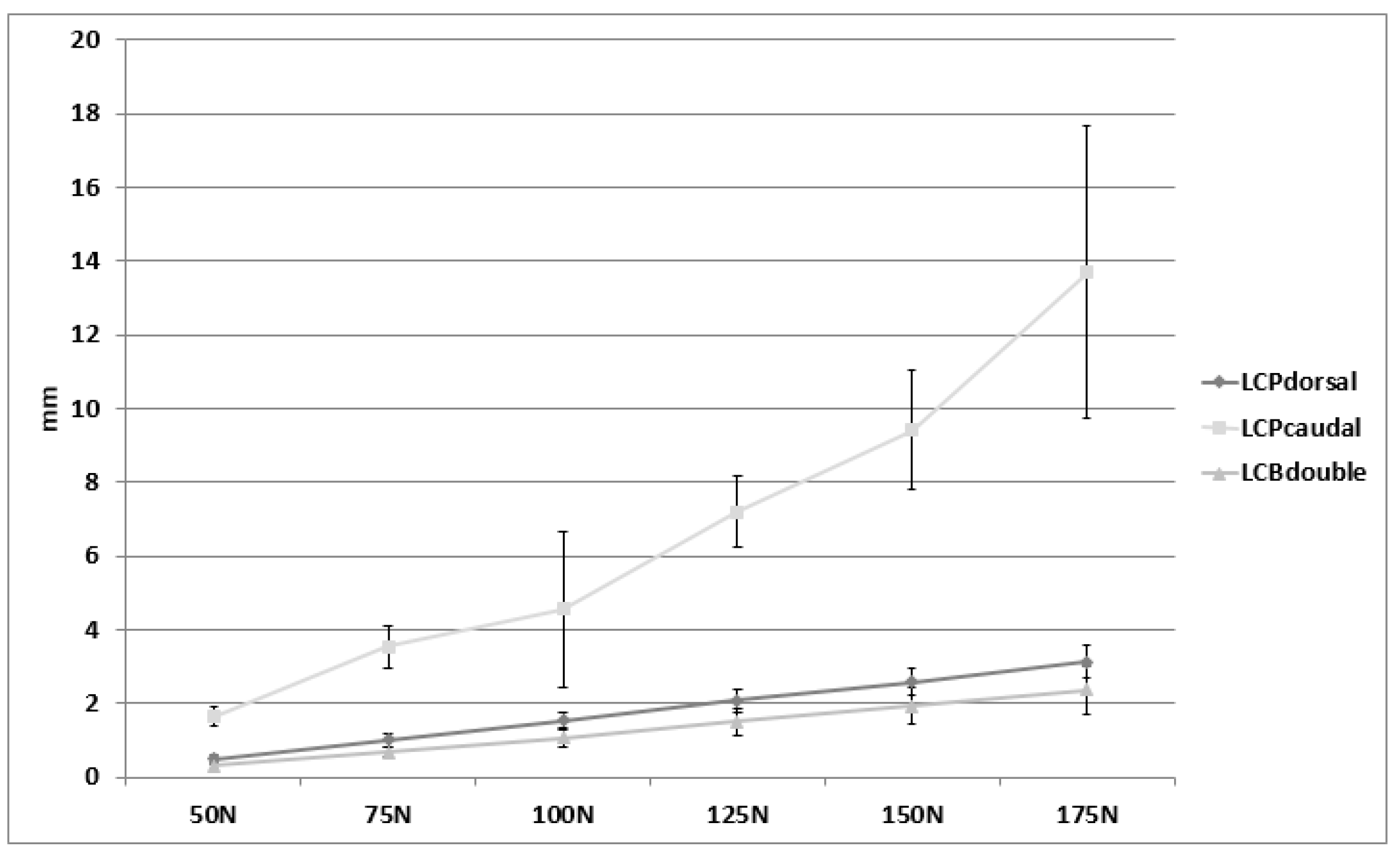
3.3. Motion of Acromial Fragment
3.4. Fracture Patterns and Failure Modes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Correction Statement
References
- Zumstein, M.A.; Pinedo, M.; Old, J.; Boileau, P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J. Shoulder Elb. Surg. 2011, 20, 146–157. [Google Scholar] [CrossRef] [PubMed]
- Hattrup, S.J. The influence of postoperative acromial and scapular spine fractures on the results of reverse shoulder arthroplasty. Orthopedics 2010, 33, 302. [Google Scholar]
- Teusink, M.J.; Otto, R.J.; Cottrell, B.J.; Frankle, M.A. What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J. Shoulder Elb. Surg. 2014, 23, 782–790. [Google Scholar] [CrossRef] [PubMed]
- Ascione, F.; Kilian, C.M.; Laughlin, M.S.; Bugelli, G.; Domos, P.; Neyton, L.; Godeneche, A.; Edwards, T.B.; Walch, G. Increased scapular spine fractures after reverse shoulder arthroplasty with a humeral onlay short stem: An analysis of 485 consecutive cases. J. Shoulder Elb. Surg. 2018, 27, 2183–2190. [Google Scholar] [CrossRef] [PubMed]
- Otto, R.J.; Virani, N.A.; Levy, J.C.; Nigro, P.T.; Cuff, D.J.; Frankle, M.A. Scapular fractures after reverse shoulder arthroplasty: Evaluation of risk factors and the reliability of a proposed classification. J. Shoulder Elb. Surg. 2013, 22, 1514–1521. [Google Scholar] [CrossRef]
- King, J.J.; Dalton, S.S.; Gulotta, L.V.; Wright, T.W.; Schoch, B.S. How common are acromial and scapular spine fractures after reverse shoulder arthroplasty? A systematic review. Bone Jt. J. 2019, 101-b, 627–634. [Google Scholar] [CrossRef]
- Brusalis, C.M.; Taylor, S.A. Periprosthetic Fractures in Reverse Total Shoulder Arthroplasty: Current Concepts and Advances in Management. Curr. Rev. Musculoskelet. Med. 2020, 13, 509–519. [Google Scholar] [CrossRef]
- Levy, J.C.; Anderson, C.; Samson, A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J. Bone Jt. Surg. Am. 2013, 95, e104. [Google Scholar] [CrossRef]
- Nyffeler, R.W.; Altioklar, B.; Bissig, P. Causes of acromion and scapular spine fractures following reverse shoulder arthroplasty: A retrospective analysis and literature review. Int. Orthop. 2020, 44, 2673–2681. [Google Scholar] [CrossRef]
- Schenk, P.; Aichmair, A.; Beeler, S.; Ernstbrunner, L.; Meyer, D.C.; Gerber, C. Acromial Fractures Following Reverse Total Shoulder Arthroplasty: A Cohort Controlled Analysis. Orthopedics 2020, 43, 15–22. [Google Scholar] [CrossRef]
- Mayne, I.P.; Bell, S.N.; Wright, W.; Coghlan, J.A. Acromial and scapular spine fractures after reverse total shoulder arthroplasty. Shoulder Elb. 2016, 8, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Crosby, L.A.; Hamilton, A.; Twiss, T. Scapula fractures after reverse total shoulder arthroplasty: Classification and treatment. Clin. Orthop. Relat. Res. 2011, 469, 2544–2549. [Google Scholar] [CrossRef] [PubMed]
- Patterson, D.C.; Chi, D.; Parsons, B.O.; Cagle, P.J. Acromial spine fracture after reverse total shoulder arthroplasty: A systematic review. J. Shoulder Elb. Surg. 2019, 28, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Neyton, L.; Erickson, J.; Ascione, F.; Bugelli, G.; Lunini, E.; Walch, G. Grammont Award 2018: Scapular fractures in reverse shoulder arthroplasty (Grammont style): Prevalence, functional, and radiographic results with minimum 5-year follow-up. J. Shoulder Elb. Surg. 2019, 28, 260–267. [Google Scholar] [CrossRef]
- Kicinski, M.; Puskas, G.J.; Zdravkovic, V.; Jost, B. Osteosynthesis of type III acromial fractures with locking compression plate, lateral clavicular plate, and reconstruction plate: A biomechanical analysis of load to failure and strain distribution. J. Shoulder Elb. Surg. 2018, 27, 2093–2098. [Google Scholar] [CrossRef]
- Umehara, J.; Yagi, M.; Hirono, T.; Komamura, T.; Nishishita, S.; Ichihashi, N. Relationship between scapular initial position and scapular movement during dynamic motions. PLoS ONE 2019, 14, e0227313. [Google Scholar] [CrossRef]
- Sakoma, Y.; Sano, H.; Shinozaki, N.; Itoigawa, Y.; Yamamoto, N.; Ozaki, T.; Itoi, E. Anatomical and functional segments of the deltoid muscle. J. Anat. 2011, 218, 185–190. [Google Scholar] [CrossRef]
- Spiegl, U.J.; Smith, S.D.; Todd, J.N.; Wijdicks, C.A.; Millett, P.J. Biomechanical evaluation of internal fixation techniques for unstable meso-type os acromiale. J. Shoulder Elb. Surg. 2015, 24, 520–526. [Google Scholar] [CrossRef]
- Ackland, D.C.; Wu, W.; Thomas, R.; Patel, M.; Page, R.; Sangeux, M.; Richardson, M. Muscle and Joint Function After Anatomic and Reverse Total Shoulder Arthroplasty Using a Modular Shoulder Prosthesis. J. Orthop. Res. 2019, 37, 1988–2003. [Google Scholar] [CrossRef]
- Katthagen, J.C.; Sußiek, J.; Frank, A.; Wermers, J.; Schliemann, B.; Raschke, M.J. Double plating is associated with higher fixation strength than single plating in osteoporotic fractures of the scapular spine: A biomechanical study. Arch. Orthop. Trauma Surg. 2021. [Google Scholar] [CrossRef]
- Augat, P.; Hast, M.W.; Schemitsch, G.; Heyland, M.; Trepczynski, A.; Borgiani, E.; Russow, G.; Märdian, S.; Duda, G.N.; Hollensteiner, M.; et al. Biomechanical models: Key considerations in study design. OTA Int. 2021, 4, e099. [Google Scholar] [CrossRef]
- Schünke, M. 5 Schultergürtel und Schultergelenk (I). In Anatomie für Osteopathen; Georg Thieme Verlag: Stuttgart, Germany, 2019. [Google Scholar]
- Gardner, M.J.; Silva, M.J.; Krieg, J.C. Biomechanical testing of fracture fixation constructs: Variability, validity, and clinical applicability. J. Am. Acad. Orthop. Surg. 2012, 20, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Hollensteiner, M.; Sandriesser, S.; Hackl, S.; Augat, P. Custom-made polyurethane-based synthetic bones mimic screw cut-through of intramedullary nails in human long bones. J. Mech. Behav. Biomed. Mater. 2021, 117, 104405. [Google Scholar] [CrossRef] [PubMed]


Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hollensteiner, M.; Sandriesser, S.; Rittenschober, F.; Hochreiter, J.; Augat, P.; Ernstbrunner, L.; Ortmaier, R. Single or Double Plating for Acromial Type III Fractures: Biomechanical Comparison of Load to Failure and Fragment Motion. J. Clin. Med. 2022, 11, 3130. https://doi.org/10.3390/jcm11113130
Hollensteiner M, Sandriesser S, Rittenschober F, Hochreiter J, Augat P, Ernstbrunner L, Ortmaier R. Single or Double Plating for Acromial Type III Fractures: Biomechanical Comparison of Load to Failure and Fragment Motion. Journal of Clinical Medicine. 2022; 11(11):3130. https://doi.org/10.3390/jcm11113130
Chicago/Turabian StyleHollensteiner, Marianne, Sabrina Sandriesser, Felix Rittenschober, Josef Hochreiter, Peter Augat, Lukas Ernstbrunner, and Reinhold Ortmaier. 2022. "Single or Double Plating for Acromial Type III Fractures: Biomechanical Comparison of Load to Failure and Fragment Motion" Journal of Clinical Medicine 11, no. 11: 3130. https://doi.org/10.3390/jcm11113130
APA StyleHollensteiner, M., Sandriesser, S., Rittenschober, F., Hochreiter, J., Augat, P., Ernstbrunner, L., & Ortmaier, R. (2022). Single or Double Plating for Acromial Type III Fractures: Biomechanical Comparison of Load to Failure and Fragment Motion. Journal of Clinical Medicine, 11(11), 3130. https://doi.org/10.3390/jcm11113130





