Association between Masseter Muscle Area and Thickness and Outcome after Carotid Endarterectomy: A Retrospective Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Outcome Parameters
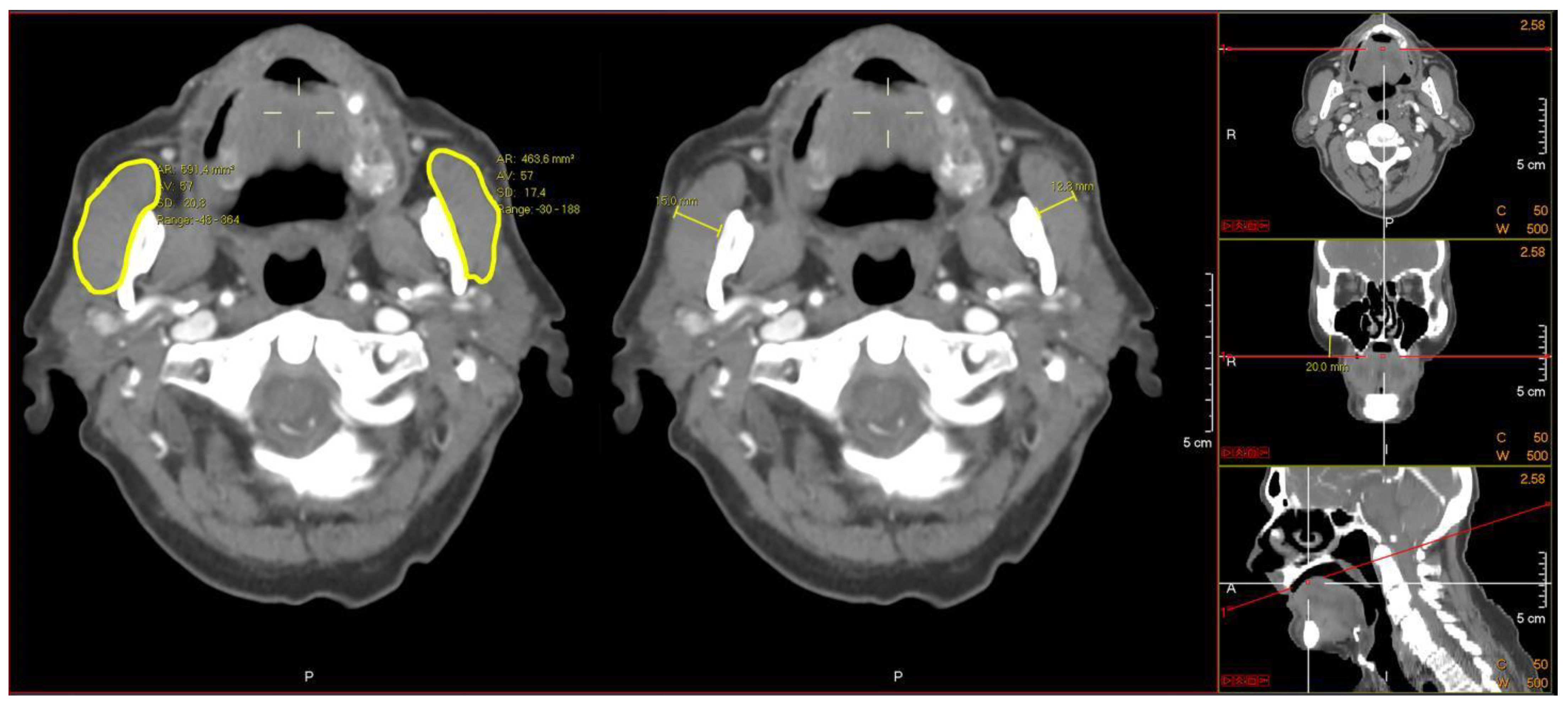
2.3. Masseter Measurements
2.4. Statistical Analysis
3. Results
3.1. Demographics
3.2. Masseter Area
3.3. Masseter Thickness
3.4. Association of Masseter Muscle Area and Thickness with Clinical Outcome Parameters
3.5. Association of Masseter Muscle Area and Thickness with GFI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Alhaidar, M.; Algaeed, M.; Amdur, R.; Algahtani, R.; Majidi, S.; Sigounas, D.; Leon Guerrero, C.R. Early Outcomes after Carotid Endarterectomy and Carotid Artery Stenting for Carotid Stenosis in the ACS-NSQIP Database. J. Vasc. Interv. Neurol. 2018, 10, 52–56. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jones, K.I.; Doleman, B.; Scott, S.; Lund, J.N.; Williams, J.P. Simple Psoas Cross-Sectional Area Measurement Is a Quick and Easy Method to Assess Sarcopenia and Predicts Major Surgical Complications. Color. Dis. 2015, 17, O20–O26. [Google Scholar] [CrossRef] [PubMed]
- Banning, L.B.D.D.; El Moumni, M.; Visser, L.; van Leeuwen, B.L.; Zeebregts, C.J.; Pol, R.A. Frailty Leads to Poor Long-Term Survival in Patients Undergoing Elective Vascular Surgery. J. Vasc. Surg. 2021, 73, 2132–2139.e2. [Google Scholar] [CrossRef] [PubMed]
- Pol, R.A.; Van Leeuwen, B.L.; Visser, L.; Izaks, G.J.; Van Den Dungen, J.J.A.M.; Tielliu, I.F.J.; Zeebregts, C.J. Standardised Frailty Indicator as Predictor for Postoperative Delirium after Vascular Surgery: A Prospective Cohort Study. Eur. J. Vasc. Endovasc. Surg. 2011, 42, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, G.A.; Georgiadis, G.S.; Georgakarakos, E.I.; Antoniou, S.A.; Bessias, N.; Smyth, J.V.; Murray, D.; Lazarides, M.K. Meta-Analysis and Meta-Regression Analysis of Outcomes of Carotid Endarterectomy and Stenting in the Elderly. JAMA Surg. 2013, 148, 1140–1152. [Google Scholar] [CrossRef]
- Dua, A.; Romanelli, M.; Upchurch, G.R.J.; Pan, J.; Hood, D.; Hodgson, K.J.; Desai, S.S. Predictors of Poor Outcome after Carotid Intervention. J. Vasc. Surg. 2016, 64, 663–670. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Kiesswetter, E.; Drey, M.; Sieber, C.C. Nutrition, Frailty, and Sarcopenia. Aging Clin. Exp. Res. 2017, 29, 43–48. [Google Scholar] [CrossRef]
- Cesari, M.; Landi, F.; Vellas, B.; Bernabei, R.; Marzetti, E. Sarcopenia and Physical Frailty: Two Sides of the Same Coin. Front. Aging Neurosci. 2014, 6, 192. [Google Scholar] [CrossRef]
- Ghaffarian, A.A.; Foss, W.T.; Donald, G.; Kraiss, L.W.; Sarfati, M.; Griffin, C.L.; Smith, B.K.; Brooke, B.S. Prognostic Implications of Diagnosing Frailty and Sarcopenia in Vascular Surgery Practice. J. Vasc. Surg. 2019, 70, 892–900. [Google Scholar] [CrossRef]
- Shen, W.; Punyanitya, M.; Wang, Z.M.; Gallagher, D.; St.-Onge, M.P.; Albu, J.; Heymsfield, S.B.; Heshka, S. Total Body Skeletal Muscle and Adipose Tissue Volumes: Estimation from a Single Abdominal Cross-Sectional Image. J. Appl. Physiol. 2004, 97, 2333–2338. [Google Scholar] [CrossRef] [PubMed]
- Boer, B.C.; de Graaff, F.; Brusse-Keizer, M.; Bouman, D.E.; Slump, C.H.; Slee-Valentijn, M.; Klaase, J.M. Skeletal Muscle Mass and Quality as Risk Factors for Postoperative Outcome after Open Colon Resection for Cancer. Int. J. Colorectal Dis. 2016, 31, 1117–1124. [Google Scholar] [CrossRef] [PubMed]
- Kays, J.K.; Liang, T.W.; Zimmers, T.A.; Milgrom, D.P.; Abduljabar, H.; Young, A.; Kim, B.J.; Bell, T.M.; Fajardo, A.; Murphy, M.P.; et al. Sarcopenia Is a Significant Predictor of Mortality after Abdominal Aortic Aneurysm Repair. JCSM Clin. Rep. 2018, 176, 139–148. [Google Scholar] [CrossRef]
- Reinders, I.; Murphy, R.A.; Brouwer, I.A.; Visser, M.; Launer, L.; Siggeirsdottir, K.; Eiriksdottir, G.; Gudnason, V.; Jonsson, P.V.; Lang, T.F.; et al. Muscle Quality and Myosteatosis: Novel Associations with Mortality Risk. Am. J. Epidemiol. 2016, 183, 53–60. [Google Scholar] [CrossRef]
- Berkel, A.E.M.; Klaase, J.M.; De Graaff, F.; Brusse-Keizer, M.G.J.; Bongers, B.C.; Van Meeteren, N.L.U. Patient’s Skeletal Muscle Radiation Attenuation and Sarcopenic Obesity Are Associated with Postoperative Morbidity after Neoadjuvant Chemoradiation and Resection for Rectal Cancer. Dig. Surg. 2019, 36, 376–383. [Google Scholar] [CrossRef]
- Matsubara, Y.; Matsumoto, T.; Aoyagi, Y.; Tanaka, S.; Okadome, J.; Morisaki, K.; Shirabe, K.; Maehara, Y. Sarcopenia Is a Prognostic Factor for Overall Survival in Patients with Critical Limb Ischemia. J. Vasc. Surg. 2015, 61, 945–950. [Google Scholar] [CrossRef]
- Newton, D.H.; Kim, C.; Lee, N.; Wolfe, L.; Pfeifer, J.; Amendola, M. Sarcopenia Predicts Poor Long-Term Survival in Patients Undergoing Endovascular Aortic Aneurysm Repair. J. Vasc. Surg. 2018, 67, 453–459. [Google Scholar] [CrossRef]
- Wallace, J.D.; Calvo, R.Y.; Lewis, P.R.; Brill, J.B.; Shackford, S.R.; Sise, M.J.; Sise, C.B.; Bansal, V. Sarcopenia as a Predictor of Mortality in Elderly Blunt Trauma Patients: Comparing the Masseter to the Psoas Using Computed Tomography. J. Trauma Acute Care Surg. 2017, 82, 65–70. [Google Scholar] [CrossRef]
- Yamaguchi, K.; Tohara, H.; Hara, K.; Nakane, A.; Yoshimi, K.; Nakagawa, K.; Minakuchi, S. Factors Associated with Masseter Muscle Quality Assessed from Ultrasonography in Community-Dwelling Elderly Individuals: A Cross-Sectional Study. Arch. Gerontol. Geriatr. 2019, 82, 128–132. [Google Scholar] [CrossRef]
- Oksala, N.K.J.; Lindström, I.; Khan, N.; Pihlajaniemi, V.J.; Lyytikäinen, L.P.; Pienimäki, J.P.; Hernesniemi, J. Pre-Operative Masseter Area Is an Independent Predictor of Long-Term Survival after Carotid Endarterectomy. Eur. J. Vasc. Endovasc. Surg. 2019, 57, 331–338. [Google Scholar] [CrossRef]
- Hwang, Y.; Lee, Y.H.; Cho, D.H.; Kim, M.; Lee, D.S.; Cho, H.J. Applicability of the Masseter Muscle as a Nutritional Biomarker. Medicine 2020, 99, e19069. [Google Scholar] [CrossRef] [PubMed]
- Visser, L.; Banning, L.B.D.; El Moumni, M.; Zeebregts, C.J.; Pol, R.A. The Effect of Frailty on Outcome after Vascular Surgery. Eur. J. Vasc. Endovasc. Surg. 2019, 58, 762–769. [Google Scholar] [CrossRef] [PubMed]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of Surgical Complications: A New Proposal with Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Slankamenac, K.; Graf, R.; Barkun, J.; Puhan, M.A.; Clavien, P.A. The Comprehensive Complication Index: A Novel Continuous Scale to Measure Surgical Morbidity. Ann. Surg. 2013, 258, 1–7. [Google Scholar] [CrossRef]
- Baitar, A.; Van Fraeyenhove, F.; Vandebroek, A.; De Droogh, E.; Galdermans, D.; Mebis, J.; Schrijvers, D. Evaluation of the Groningen Frailty Indicator and the G8 Questionnaire as Screening Tools for Frailty in Older Patients with Cancer. J. Geriatr. Oncol. 2013, 4, 32–38. [Google Scholar] [CrossRef]
- Peters, L.L.; Boter, H.; Buskens, E.; Slaets, J.P.J. Measurement Properties of the Groningen Frailty Indicator in Home-Dwelling and Institutionalized Elderly People. J. Am. Med. Dir. Assoc. 2012, 13, 546–551. [Google Scholar] [CrossRef]
- Peters, L.L.; Burgerhof, J.G.M.; Boter, H.; Wild, B.; Buskens, E.; Slaets, J.P.J. Predictive Validity of a Frailty Measure (GFI) and a Case Complexity Measure (IM-E-SA) on Healthcare Costs in an Elderly Population. J. Psychosom. Res. 2015, 79, 404–411. [Google Scholar] [CrossRef]
- Hu, P.; Uhlich, R.; White, J.; Kerby, J.; Bosarge, P. Sarcopenia Measured Using Masseter Area Predicts Early Mortality Following Severe Traumatic Brain Injury. J. Neurotrauma 2018, 35, 2400–2406. [Google Scholar] [CrossRef]
- Newton, J.P.; Yemm, R.; Abel, R.W.; Menhinick, S. Changes in Human Jaw Muscles with Age and Dental State. Gerodontology 1993, 10, 16–22. [Google Scholar] [CrossRef]
- Oza, R.; Rundell, K.; Garcellano, M. Recurrent Ischemic Stroke: Strategies for Prevention. Am. Fam. Physician 2017, 96, 436–440. [Google Scholar]
- Waduud, M.A.; Ul-Hassan, A.; Naveed, T.; Adusumilli, P.; Slater, T.A.; Straw, S.; Hammond, C.; Ashbridge Scott, D.J. Comparison of Quantity and Quality of Muscle as Clinical Prognostic Markers in Patients Undergoing Carotid Endarterectomy. Br. J. Radiol. 2020, 93, 20200136. [Google Scholar] [CrossRef] [PubMed]
- Madden, K.M.; Feldman, B.; Arishenkoff, S.; Meneilly, G.S. A Rapid Point-of-Care Ultrasound Marker for Muscle Mass and Muscle Strength in Older Adults. Age Ageing 2021, 50, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Madden, K.M.; Feldman, B.; Arishenkoff, S.; Meneilly, G.S. Point-of-Care Ultrasound Measures of Muscle and Frailty Measures. Eur. Geriatr. Med. 2021, 12, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Arinze, N.; Farber, A.; Levin, S.R.; Cheng, T.W.; Rybin, D.; Siracuse, J.J. The Association of Body Mass Index with Outcomes after Carotid Endarterectomy. Ann. Vasc. Surg. 2021, 77, 7–15. [Google Scholar] [CrossRef]
- Benson, R.; McGregor, G.; Shehata, M.; Imray, C. Optimising Fitness for Major Vascular Surgery. BMJ 2019, 366, l5002. [Google Scholar] [CrossRef]
- Poscia, A.; Milovanovic, S.; La Milia, D.I.; Duplaga, M.; Grysztar, M.; Landi, F.; Moscato, U.; Magnavita, N.; Collamati, A.; Ricciardi, W. Effectiveness of Nutritional Interventions Addressed to Elderly Persons: Umbrella Systematic Review with Meta-Analysis. Eur. J. Public Health 2018, 28, 275–283. [Google Scholar] [CrossRef]
- Barakat, H.M.; Shahin, Y.; Khan, J.A.; McCollum, P.T.; Chetter, I.C. Preoperative Supervised Exercise Improves Outcomes after Elective Abdominal Aortic Aneurysm Repair: A Randomized Controlled Trial. Ann. Surg. 2016, 264, 47–53. [Google Scholar] [CrossRef]
- Ballotta, E.; Meneghetti, G.; Da Giau, G.; Manara, R.; Saladini, M.; Baracchini, C. Carotid Endarterectomy within 2 Weeks of Minor Ischemic Stroke: A Prospective Study. J. Vasc. Surg. 2008, 48, 595–600. [Google Scholar] [CrossRef]
- Abbas, K.; Vohra, R.S.; Salhab, M.; Sinclair, M.D.; Kent, P.J.; Gough, M.J. A Strategy to Meet the “two-Week” Target for Carotid Endarterectomy in Symptomatic Patients. Clin. Med. J. R. Coll. Phys. Lond. 2011, 11, 452–455. [Google Scholar] [CrossRef]
- Van Vugt, J.L.A.; Coebergh van den Braak, R.R.J.; Schippers, H.J.W.; Veen, K.M.; Levolger, S.; de Bruin, R.W.F.; Koek, M.; Niessen, W.J.; IJzermans, J.N.M.; Willemsen, F.E.J.A. Contrast-Enhancement Influences Skeletal Muscle Density, but Not Skeletal Muscle Mass, Measurements on Computed Tomography. Clin. Nutr. 2018, 37, 1707–1714. [Google Scholar] [CrossRef]
- Lindström, I.; Protto, S.; Khan, N.; Hernesniemi, J.; Sillanpää, N.; Oksala, N. Association of Masseter Area and Radiodensity with Three-Month Survival after Proximal Anterior Circulation Occlusion. J. Neurointerv. Surg. 2021, 13, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Tanabe, C.; Reed, M.J.; Pham, T.N.; Penn, K.; Bentov, I.; Kaplan, S.J. Association of Brain Atrophy and Masseter Sarcopenia with 1-Year Mortality in Older Trauma Patients. JAMA Surg. 2019, 154, 716–723. [Google Scholar] [CrossRef] [PubMed]
| Demographics | Masseter Muscle Area | Masseter Muscle Thickness | |||||
|---|---|---|---|---|---|---|---|
| All Patients (n = 123) | AMA (n = 101) | LMA (n = 22) | p Value | AMT (n = 105) | LMT (n = 18) | p Value | |
| Sex | |||||||
| Male | 90 (73.2%) | 74 (73.3%) | 16 (72.7%) | 0.959 | 76 (72.4%) | 14 (77.8%) | 0.633 |
| Female | 33 (26.8%) | 27 (26.7%) | 6 (27.3%) | 0.959 | 29 (27.6%) | 4 (22.2%) | 0.633 |
| Age—y | 68 (9.7) | 68 (9.9) | 71 (8.7) | 0.652 | 68 (10.3) | 69 (6.1) | 0.475 |
| BMI—kg/m2 | 27.2 (4.5) | 27.6 (4.5) | 25.1 (3.1) | 0.014 | 27.6 (4.6) | 24.9 (3.1) | 0.021 |
| Smoking status | |||||||
| Current | 33 (26.8%) | 24 (23.8%) | 9 (40.9%) | 0.087 | 23 (21.9%) | 10 (55.6%) | 0.005 |
| History | 38 (30.9%) | 35 (34.7%) | 3 (13.6%) | 0.041 | 34 (32.4%) | 4 (22.2%) | 0.389 |
| Never | 52 (42.3%) | 42 (41.6%) | 10 (45.5%) | 0.814 | 48 (45.7%) | 4 (22.2%) | 0.051 |
| ASA ≥ 3 | 60 (48.7%) | 45 (44.6%) | 15 (68.1%) | 0.037 | 45 (42.9%) | 15 (83.3%) | 0.001 |
| Charlson Comorbidity Index—median (IQR) | 5 (3–6) | 5 (3–6) | 5 (4–5) | 0.806 | 4 (3–6) | 5 (4–5) | 0.496 |
| Partial or full dental prosthesis | 65 (52.8%) | 54 (53.5%) | 11 (50.0%) | 0.446 | 53 (50.5%) | 12 (66.7%) | 0.234 |
| GFI | 2 (1–4) | 2 (1–4) | 2 (1–5) | 0.827 | 2 (1–4) | 2 (1–5.25) | 0.233 |
| GFI > 3 | 34 (27.6%) | 28 (27.7%) | 6 (27.3%) | 0.966 | 28 (26.7%) | 6 (33.3%) | 0.559 |
| Indication | |||||||
| Asymptomatic | 19 (15.4%) | 16 (15.8%) | 3 (13.6%) | 0.795 | 18 (17.1%) | 1 (5.6%) | 0.209 |
| Amaurosis | 17 (13.8%) | 16 (15.8%) | 1 (4.5%) | 0.164 | 15 (14.3%) | 2 (11.1%) | 0.718 |
| Transient ischemic attack | 41 (33.3%) | 33 (32.7%) | 8 (36.4%) | 0.739 | 37 (35.2%) | 4 (22.2%) | 0.279 |
| Minor ischemic stroke | 46 (37.4%) | 36 (35.6%) | 10 (45.5%) | 0.389 | 35 (33.3%) | 11 (61.1%) | 0.024 |
| Ipsilateral stenosis (%) | |||||||
| <50% | 2 (1.6%) | 1 (1.0%) | 1 (4.5%) | 0.232 | 1 (1%) | 1 (5.6%) | 0.154 |
| 50–70% | 22 (17.9%) | 17 (16.8%) | 5 (22.7%) | 0.513 | 22 (21%) | 0 (0%) | 0.032 |
| >70% | 99 (80.5%) | 83 (82.2%) | 16 (72.7%) | 0.311 | 82 (78%) | 17 (94.4%) | 0.106 |
| Clinical Outcomes | Masseter Muscle Area | Masseter Muscle Thickness | |||||
|---|---|---|---|---|---|---|---|
| All Patients (n = 123) | AMA (n = 101) | LMA (n = 22) | p Value | AMT (n = 105) | LMT (n = 18) | p Value | |
| Complications within 30 days | 41 (33.3%) | 30 (29.7) | 11 (50.0%) | 0.067 | 34 (32.4%) | 7 (38.9%) | 0.588 |
| Cardiac complication | 6 (4.9%) | 4 (4.1%) | 2 (9.1%) | 0.311 | 1 (5.0%) | 1 (5.6%) | 0.885 |
| Hyper/hypotension | 9 (7.3%) | 5 (5.0%) | 4 (18.2%) | 0.031 | 6 (5.7%) | 3 (16.7%) | 0.099 |
| Stroke | 6 (4.9%) | 4 (4.0%) | 2 (9.1%) | 0.311 | 4 (3.8%) | 2 (11.1%) | 0.184 |
| Wound | 8 (6.5%) | 7 (6.9%) | 1 (4.5%) | 0.681 | 7 (6.7%) | 1 (5.6%) | 0.860 |
| Nerve injury | 15 (12.2%) | 13 (12.9%) | 2 (9.1%) | 0.623 | 15 (14.3%) | 0 (0%) | 0.087 |
| Other | 3 (2.4%) | 2 (2.0%) | 1 (4.5%) | 0.480 | 3 (2.9%) | 0 (0%) | 0.468 |
| Complications in CCI, median (IQR) | 0 (0–8.7) | 0 (0–8.7) | 0 (0–20.9) | 0.082 | 0 (0–8.7) | 0 (0–20.9) | 0.624 |
| Length of hospital stay (days), median (IQR) | 4 (4–5) | 4.50 (4–5) | 5.5 (4–7) | 0.011 | 4 (4–5) | 4 (4–7.25) | 0.621 |
| Hospital stay ≥ 7 days | 15 (12.2%) | 9 (8.9%) | 6 (27.3%) | 0.017 | 10 (9.5%) | 5 (27.8%) | 0.029 |
| Readmission within 30 days | 6 (4.9%) | 5 (5.0%) | 1 (4.5%) | 0.708 | 5 (4.8%) | 1 (5.6%) | 0.62 |
| Recurrent stroke within 5 years (beyond 30 days) | 8 (6.6%) | 6 (5.9%) | 2 (9.1%) | 0.587 | 5 (4.8%) | 3 (16.7%) | 0.058 |
| Transient ischemic attack | 4 (3.3%) | 3 (3.0%) | 1 (4.5%) | 0.706 | 3 (2.9%) | 1 (5.6%) | 0.551 |
| Ischemic stroke | 4 (3.3%) | 3 (3.0%) | 1 (4.5%) | 0.706 | 2 (1.9%) | 2 (11.1%) | 0.042 |
| 5-year survival | 102 (83.9%) | 85 (84.2%) | 17 (77.2%) | 0.531 | 88 (83.8%) | 14 (77.8%) | 0.368 |
| Low Masseter Muscle Area | Low Masseter Muscle Thickness | |||||||
|---|---|---|---|---|---|---|---|---|
| Outcome Parameter | Effect Size | 95%-CI | p Value | Effect Size | 95%-CI | p Value | ||
| Lower | Upper | Lower | Upper | |||||
| Complications (CCI) | ||||||||
| Univariable analysis | 5.23 | 0.31 | 10.14 | 0.037 | 2.92 | −2.48 | 8.32 | 0.287 |
| Multivariable analysis * | 4.26 | −1.26 | 9.79 | 0.129 | 1.15 | −4.99 | 7.29 | 0.712 |
| Hospital stay ≥7 days | ||||||||
| Univariable analysis | OR 3.80 | 1.20 | 12.24 | 0.023 | OR 3.65 | 1.08 | 12.38 | 0.037 |
| Multivariable analysis ** | OR 4.73 | 1.13 | 19.73 | 0.033 | OR 8.78 | 1.15 | 66.85 | 0.036 |
| 5-year recurrent stroke risk (beyond 30 days) | ||||||||
| Univariable analysis | HR 1.70 | 0.34 | 8.4 | 0.518 | HR 4.04 | 0.96 | 16.93 | 0.056 |
| Multivariable analysis * | HR 2.05 | 0.29 | 14.62 | 0.473 | HR 12.40 | 1.83 | 84.09 | 0.010 |
| 5-year survival | ||||||||
| Univariable analysis | HR 1.56 | 0.58 | 4.31 | 0.374 | HR 1.54 | 0.52 | 4.59 | 0.436 |
| Multivariable analysis ** | HR 1.25 | 0.38 | 4.14 | 0.714 | HR 1.63 | 0.47 | 5.72 | 0.443 |
| Author (Year) Country [Citation] | Population | Sample | Masseter Measurements | Results | ||
|---|---|---|---|---|---|---|
| Type of Measurements | Mean | Outcome Parameters | Effect Size [95%-CI] | |||
| Lindström et al. (2021) Finland [41] | Pre-operative before mechanical thrombectomy in acute ischemic stroke patients | 312 | Masseter area | M 450 mm2 F 360 mm2 | 3-month survival | OR 0.57 [0.35–0.91] p = 0.02 |
| Masseter density | M 65.5 HUF 61 HU | 3-month survival | OR 0.61 [0.41–0.92] p = 0.02 | |||
| Waduud et al. (2020) United Kingdom [31] | Pre-operative before carotid endarterectomy | 149 | Masseter area | - | 30-day survival | HR 0.14 [0–5.44] p = 0.29 |
| 1-year survival | HR 0.51 [0.13–2.07] p = 0.35 | |||||
| 4-year survival | HR 0.36 [0.13–1.04] p = 0.06 | |||||
| Overall survival | HR 0.38 [0.15–0.97] p = 0.04 | |||||
| Masseter density | - | 30-day survival | HR 1.03 [0.95–1.10] p = 0.52 | |||
| 1-year survival | HR 0.98 [0.95–1.01] p = 0.31 | |||||
| 4-year survival | HR 0.98 [0.96–1.01] p = 0.24 | |||||
| Overall survival | HR 0.97 [0.95–1.00] p = 0.11 | |||||
| Masseter area × masseter density | - | 30-day survival | HR 0.99 [0.97–1.02] p = 0.57 | |||
| 1-year survival | HR 0.99 [0.98–1.00] p = 0.20 | |||||
| 4-year survival | HR 0.99 [0.98–1.00] p = 0.07 | |||||
| Overall survival | HR 0.99 [0.99–1.00] p = 0.04 | |||||
| Tanabe et al. (2019) United States of America [42] | Geriatric trauma patients (≥65 years) admitted to the traumatic ICU | 327 | Masseter area | M 439 mm2 F 348 mm2 | 1-year mortality | HR 2 [1.20–3.10] p = 0.005 |
| Oksala et al. (2019) Japan [20] | Pre-operative before carotid endarterectomy | 242 | Masseter area | M 420 mm2 F 349 mm2 | Long-term survival—Median follow-up 68 months | HR 0.75 [0.58–0.97] p = 0.03 |
| Masseter density | M 55 HU F 49 HU | Long-term survival—Median follow up 68 months | HR 0.92 [0.76–1.12] p = 0.43 | |||
| Hu et al. (2018) United States of America [28] | Geriatric trauma patients (≥55 years) with sTBI | 108 | Masseter area | M 455 mm2 F 337 mm2 | 30-day mortality | HR 0.78 [0.62–0.97] p = 0.04 |
| Masseter area 1SD below sex-based mean | - | Discharge disposition to home | 0% vs. 13%, p = 0.04 | |||
| 30-day mortality | OR 2.95 [1.03–8.49] p = 0.05 | |||||
| Wallace et al. (2016) United States of America [18] | Blunt-injured trauma geriatric patients (≥65 years) | 357 | Masseter area | M 418 mm2 F 343 mm2 | 2-year mortality | HR 0.76 [0.60–0.96] p = 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hogenbirk, R.N.M.; Banning, L.B.D.; Visser, A.; Jager-Wittenaar, H.; Pol, R.A.; Zeebregts, C.J.; Klaase, J.M. Association between Masseter Muscle Area and Thickness and Outcome after Carotid Endarterectomy: A Retrospective Cohort Study. J. Clin. Med. 2022, 11, 3087. https://doi.org/10.3390/jcm11113087
Hogenbirk RNM, Banning LBD, Visser A, Jager-Wittenaar H, Pol RA, Zeebregts CJ, Klaase JM. Association between Masseter Muscle Area and Thickness and Outcome after Carotid Endarterectomy: A Retrospective Cohort Study. Journal of Clinical Medicine. 2022; 11(11):3087. https://doi.org/10.3390/jcm11113087
Chicago/Turabian StyleHogenbirk, Rianne N. M., Louise B. D. Banning, Anita Visser, Harriet Jager-Wittenaar, Robert A. Pol, Clark J. Zeebregts, and Joost M. Klaase. 2022. "Association between Masseter Muscle Area and Thickness and Outcome after Carotid Endarterectomy: A Retrospective Cohort Study" Journal of Clinical Medicine 11, no. 11: 3087. https://doi.org/10.3390/jcm11113087
APA StyleHogenbirk, R. N. M., Banning, L. B. D., Visser, A., Jager-Wittenaar, H., Pol, R. A., Zeebregts, C. J., & Klaase, J. M. (2022). Association between Masseter Muscle Area and Thickness and Outcome after Carotid Endarterectomy: A Retrospective Cohort Study. Journal of Clinical Medicine, 11(11), 3087. https://doi.org/10.3390/jcm11113087







