Risk Factors for Non-Union after Open Reduction and Internal Fixation in Patients with Distal Humerus Fractures
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection and Methods
2.2. Patient Demographic Factors
2.3. Surgical Factors
2.4. Operative Techniques and Rehabilitation
2.5. Statistical Analysis
3. Results
3.1. Comparison of Demographic Factors between Non-Union Group and Union Group
3.2. Comparison of Surgical Factors between Non-Union Group and Union Group
3.3. Independent Risk Factors for Non-Union
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Court-Brown, C.M.; Caesar, B. Epidemiology of adult fractures: A review. Injury 2006, 37, 691–697. [Google Scholar] [CrossRef] [PubMed]
- Moursy, M.; Wegmann, K.; Wichlas, F.; Tauber, M. Distal humerus fracture in patients over 70 years of age: Results of open reduction and internal fixation. Arch. Orthop. Trauma. Surg. 2020, 142, 157–164. [Google Scholar] [CrossRef] [PubMed]
- Cho, E.; Weber, M.B.; Opel, D.; Lee, A.; Hoyen, H.; Bafus, B.T. Complications and functional outcomes after transolecranon distal humerus fracture. J. Shoulder Elb. Surg. 2020, 30, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Helfet, D.L.; Kloen, P.; Anand, N.; Rosen, H.S. Open reduction and internal fixation of delayed unions and nonunions of fractures of the distal part of the humerus. J. Bone Jt. Surg. Am. 2003, 85, 33–40. [Google Scholar] [CrossRef]
- Vauclair, F.; Goetti, P.; Nguyen, N.T.V.; Sanchez-Sotelo, J. Distal humerus nonunion: Evaluation and management. EFORT Open Rev. 2020, 5, 289–298. [Google Scholar] [CrossRef]
- Zaidenberg, E.E.; Cesca, F.J.; Pastrana, M.J.; Zaidenberg, C.R. Pedicled Vascularized Bone Graft of the Distal Radius for Recalcitrant Nonunion of the Distal Humerus. J. Orthop. Trauma 2018, 32, e394–e399. [Google Scholar] [CrossRef]
- Korner, J.; Lill, H.; Müller, L.P.; Hessmann, M.; Kopf, K.; Goldhahn, J.; Gonschorek, O.; Josten, C.; Rommens, P.M. Distal humerus fractures in elderly patients: Results after open reduction and internal fixation. Osteoporos. Int. 2004, 16, S73–S79. [Google Scholar] [CrossRef]
- Ring, D.; Gulotta, L.; Jupiter, J.B. Unstable nonunions of the distal part of the humerus. J. Bone Jt. Surg. Am. 2003, 85, 1040–1046. [Google Scholar] [CrossRef]
- Claessen, F.M.; Braun, Y.; Peters, R.M.; Kolovich, G.P.; Ring, D. Plate and Screw Fixation of Bicolumnar Distal Humerus Fractures: Factors Associated With Loosening or Breakage of Implants or Nonunion. J. Hand Surg. Am. 2015, 40, 2045–2051.e2. [Google Scholar] [CrossRef]
- Patel, J.; Motwani, G.; Shah, H.; Daveshwar, R. Outcome after internal fixation of intraarticular distal humerus (AO type B & C) fractures: Preliminary results with anatomical distal humerus LCP system. J. Clin. Orthop. Trauma 2017, 8, 63–67. [Google Scholar] [CrossRef] [Green Version]
- Gustilo, R.B.; Anderson, J.T. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J. Bone Joint Surg. Am. 1976, 58, 453–458. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Peters, R.M.; Claessen, F.M.; Doornberg, J.N.; Kolovich, G.P.; Diercks, R.L.; Bekerom, M.P.V.D. Union rate after operative treatment of humeral shaft nonunion—A systematic review. Injury 2015, 46, 2314–2324. [Google Scholar] [CrossRef] [PubMed]
- Robinson, C.M.; Hill, R.M.F.; Jacobs, N.; Dall, G.; Court-Brown, C.M. Adult Distal Humeral Metaphyseal Fractures: Epidemiology and Results of Treatment. J. Orthop. Trauma 2003, 17, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Ziran, B.H.; Smith, W.R.; Balk, M.L.; Manning, C.M.; Agudelo, J.F. A True Triceps-Splitting Approach for Treatment of Distal Humerus Fractures: A Preliminary Report. J. Trauma 2005, 58, 70–75. [Google Scholar] [CrossRef]
- Lauder, A.; Richard, M.J. Management of distal humerus fractures. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 745–762. [Google Scholar] [CrossRef]
- Yadav, V.; Sharma, P.; Gohiya, A. Functional outcome of intraarticular distal humerus fracture fixation using triceps-sparing paratricipital approach. Indian J. Orthop. 2016, 50, 595–601. [Google Scholar] [CrossRef]
- Wu, Z.-Z.; Wang, J.-D.; Ji, X.-X.; Ma, Z.-J.; Wu, J.-H.; Wang, Q.-G. Surgical exposures of the distal humeral fractures: An anatomical study of the anterior, posterior, medial and lateral approaches. Chin. J. Traumatol. 2018, 21, 356–359. [Google Scholar] [CrossRef]
- Wei, L.; Xu, H.; An, Z. In intra-articular distal humeral fractures: Can combined medial-lateral approach gain better outcomes than olecranon osteotomy? Ulus Travma. Acil Cerrahi Derg. 2020, 26, 586–592. [Google Scholar] [CrossRef]
- Theivendran, K.; Duggan, P.J.; Deshmukh, S.C. Surgical treatment of complex distal humeral fractures: Functional outcome after internal fixation using precontoured anatomic plates. J. Shoulder Elb. Surg. 2010, 19, 524–532. [Google Scholar] [CrossRef]
- Chalidis, B.; Dimitriou, C.; Papadopoulos, P.; Petsatodis, G.; Giannoudis, P. Total elbow arthroplasty for the treatment of insufficient distal humeral fractures. A retrospective clinical study and review of the literature. Injury 2009, 40, 582–590. [Google Scholar] [CrossRef]
- Hak, D.J.; Fitzpatrick, D.; Bishop, J.A.; Marsh, J.L.; Tilp, S.; Schnettler, R.; Simpson, H.; Alt, V. Delayed union and nonunions: Epidemiology, clinical issues, and financial aspects. Injury 2014, 45, S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Zura, R.; Xiong, Z.; Einhorn, T.; Watson, J.T.; Ostrum, R.F.; Prayson, M.J.; Della Rocca, G.J.; Mehta, S.; McKinley, T.; Wang, Z.; et al. Epidemiology of Fracture Nonunion in 18 Human Bones. JAMA Surg. 2016, 151, e162775. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ali, A.; Douglas, H.; Stanley, D. Revision surgery for nonunion after early failure of fixation of fractures of the distal humerus. J. Bone Jt. Surgery. Br. Vol. 2005, 87, 1107–1110. [Google Scholar] [CrossRef] [Green Version]
- Kokly, S.; Castagna, A.; Mohamadreza, M. Modified Tension Band Wiring in Adult Distal Humeral Fracture Types A2 and C1. Arch. Bone Jt. Surg. 2019, 7, 325–330. [Google Scholar] [PubMed]
- Rahman, M.M.; Islam, N.S.; Kabir, S.J.; Islam, M.S.; Rahman, M.M.; Islam, M.A.; Kabir, K.M.; Islam, M.N.; Hossain, M.A. Outcome of Double Tension Band Wiring Method for the Treatment of Intercondylar Fractures of Humerus. Mymensingh Med. J. 2020, 29, 78–85. [Google Scholar] [PubMed]
- Doğramaci, Y.; Esen, E.; Kürklü, M.; Kirici, Y.; O Atahan, A.; Kömürcü, M. Double plate osteosynthesis provides better biomechanical stabilization than double tension band technique in distal humerus fractures. Eklem Hastalik. Cerrahisi 2010, 21, 44–49. [Google Scholar]



| Demographic Factors | |
|---|---|
| No. of patients | 155 |
| Age, years | 52.6 ± 21.3 |
| Sex, male/female, n | 53/102 |
| Side, right/left, n | 62/93 |
| BMI (kg/m2) | 22.9 ± 3.4 |
| Comorbidities, n | |
| Hypertension | 50 |
| Diabetes mellitus, HbA1c level | 25, 7.6 ± 0.9 |
| Angina or myocardial infarction | 8 |
| Cancer | 4 |
| Smoking, n | 16 |
| Alcohol, n | 34 |
| Injury mechanism, low/high | 95/59 |
| Injury to operation interval (days) | 6.1 ± 6.6 |
| Combined fracture, n | 21 |
| Gustilo and Anderson classification 1 | 5 |
| Preop neurologic symptom | 9 |
| Follow up period, months (range) | 33.9 ± 30.1 (22–312) |
| Non-union, n | 12 |
| Surgical factors | |
| AO fracture classification, A/B/C | 68/11/76 |
| Combined fracture operation, n | 14 |
| Surgical approach, posterior/medial/lateral/dual incision, n | 118/4/27/6 |
| Olecranon osteotomy/triceps split/triceps sparing paracipital ‡, n | 87/14/17 |
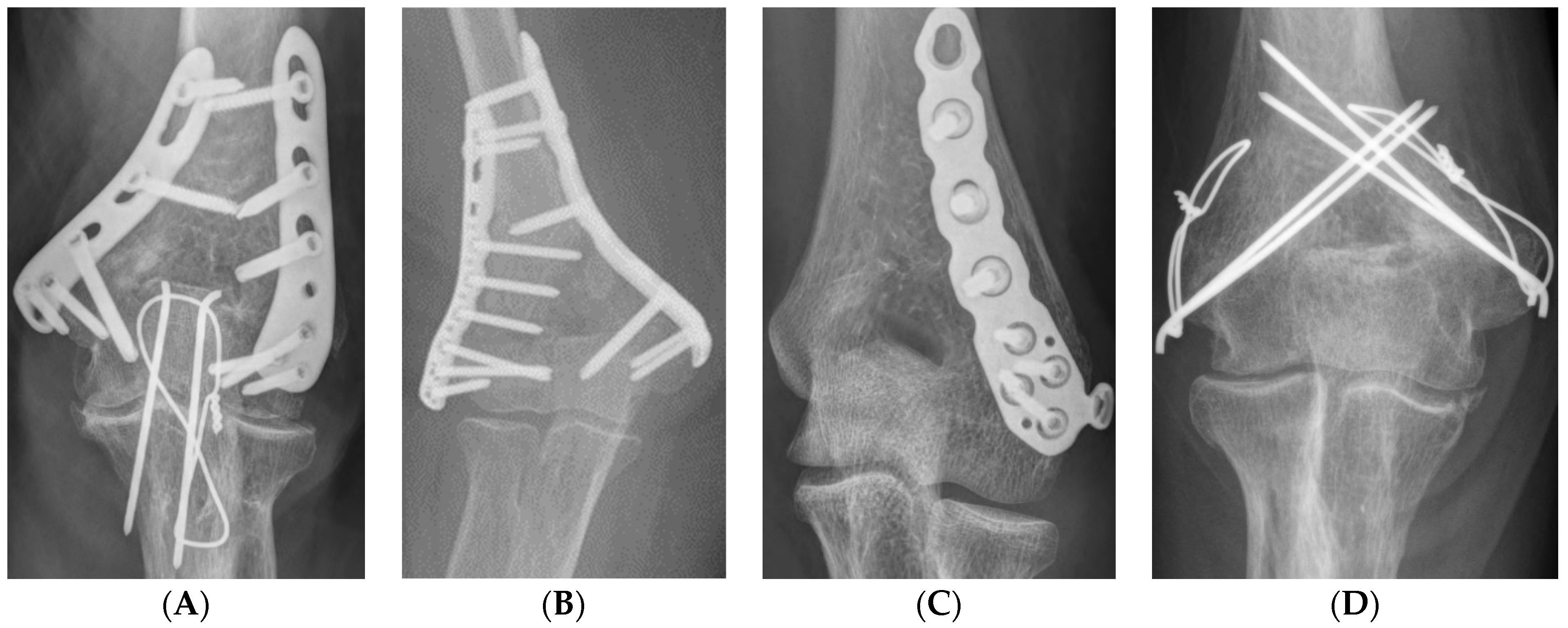
| Fixation method, orthogonal plate/parallel/single/TBW, n | 87/8/44/16 |
| Ulnar nerve anterior transposition, n | 76 |
| Operation, time, minutes | 124.2 ± 50.5 |
| Demographic Factors | Non-Union (n = 13) | Union (n = 142) | p Value |
|---|---|---|---|
| Age, years | 63.1 ± 19.4 | 51.7 ± 21.3 | 0.065 |
| Sex, male/female, n | 7/6 | 46/96 | 0.135 |
| Side, right/left, n | 6/7 | 56/86 | 0.636 |
| BMI (kg/m2) | 24.9 ± 3.2 | 22.7 ± 3.4 | 0.028 |
| Comorbidities, n (%) | |||
| Hypertension | 6 | 44 | 0.352 |
| Diabetes mellitus | 5 (38.5) | 20 (14.1) | 0.038 |
| Angina or myocardial infarction | 1 | 7 | 0.512 |
| Cancer | 0 | 4 | 1.000 |
| Smoking, n (%) | 2 (15.4) | 14 (9.9) | 0.626 |
| Alcohol, n (%) | 2 (15.4) | 32 (22.5) | 0.735 |
| Injury mechanism, low/high, n | 8/5 | 87/54 | 1.000 |
| Injury to operation interval (days) | 7.3 ± 11.8 | 6.0 ± 6.0 | 0.728 |
| Combined fracture, n | 5 | 16 | 0.018 |
| Gustilo and Anderson classification 1 | 1 | 4 | 0.359 |
| Preop neurologic symptom, n | 1 | 8 | 0.555 |
| Follow-up period, months | 37.2 ± 27.1 | 33.5 ± 30.9 | 0.678 |
| Surgical Factors | Non-Union (n = 13) | Union (n = 142) | p Value |
|---|---|---|---|
| AO fracture classification, A/B/C, n | 8/1/4 | 60/10/72 | 0.371 |
| Combined fracture operation, n (%) | 5 (38.5) | 9 (6.3) | 0.002 |
| Ulnar nerve anterior transposition, n (%) | 3 (23.1) | 73 (51.4) | 0.080 |
| Operation, time, minutes | 93.8 ± 32.2 | 125.9 ± 50.9 | 0.131 |
| Surgical Factors | Non-Union (n = 13) | Union (n = 142) | p Value |
|---|---|---|---|
| Surgical approach, n | |||
| Posterior | 9 | 109 | 0.170 |
| Medial | 0 | 4 | |
| Lateral | 2 | 25 | |
| Dual incision | 2 | 4 | |
| Olecranon osteotomy/triceps split/paracipital ‡ | 8/1/0 | 79/13/17 | 0.626 |
| Fixation method, n (%) | |||
| Orthogonal plate | 3 (23.1) | 84 (59.2) | 0.005 |
| parallel | 1 (7.7) | 7 (4.9) | |
| single | 4 (30.8) | 40 (28.2) | |
| TBW | 5 (38.5) | 11 (7.7) |
| Multivariate Analysis | Odds Ratio | 95% CI | p Value |
|---|---|---|---|
| BMI | 1.092 | 0.893–1.335 | 0.393 |
| Diabetes mellitus | 3.528 | 0.864–14.403 | 0.079 |
| Combined fracture | 2.464 | 0.266–22.855 | 0.427 |
| Combined fracture operation | 10.467 | 1.880–58.257 | 0.007 |
| Fixation method § | |||
| Parallel plate (ref. orthogonal) | 5.850 | 0.422–81.107 | 0.188 |
| Single plate (ref. orthogonal) | 5.200 | 0.889–30.430 | 0.067 |
| TBW (ref. orthogonal) | 9.176 | 1.474–57.135 | 0.018 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, K.-H.; Baek, J.-H.; Kim, M.-S. Risk Factors for Non-Union after Open Reduction and Internal Fixation in Patients with Distal Humerus Fractures. J. Clin. Med. 2022, 11, 2679. https://doi.org/10.3390/jcm11102679
Ku K-H, Baek J-H, Kim M-S. Risk Factors for Non-Union after Open Reduction and Internal Fixation in Patients with Distal Humerus Fractures. Journal of Clinical Medicine. 2022; 11(10):2679. https://doi.org/10.3390/jcm11102679
Chicago/Turabian StyleKu, Ki-Hyeok, Jong-Hun Baek, and Myung-Seo Kim. 2022. "Risk Factors for Non-Union after Open Reduction and Internal Fixation in Patients with Distal Humerus Fractures" Journal of Clinical Medicine 11, no. 10: 2679. https://doi.org/10.3390/jcm11102679
APA StyleKu, K.-H., Baek, J.-H., & Kim, M.-S. (2022). Risk Factors for Non-Union after Open Reduction and Internal Fixation in Patients with Distal Humerus Fractures. Journal of Clinical Medicine, 11(10), 2679. https://doi.org/10.3390/jcm11102679







