The Prognostic Role of Early Skeletal Muscle Mass Depletion in Multimodality Management of Patients with Advanced Gastric Cancer Treated with First Line Chemotherapy: A Pilot Experience from Modena Cancer Center
Abstract
1. Introduction
2. Materials and Methods
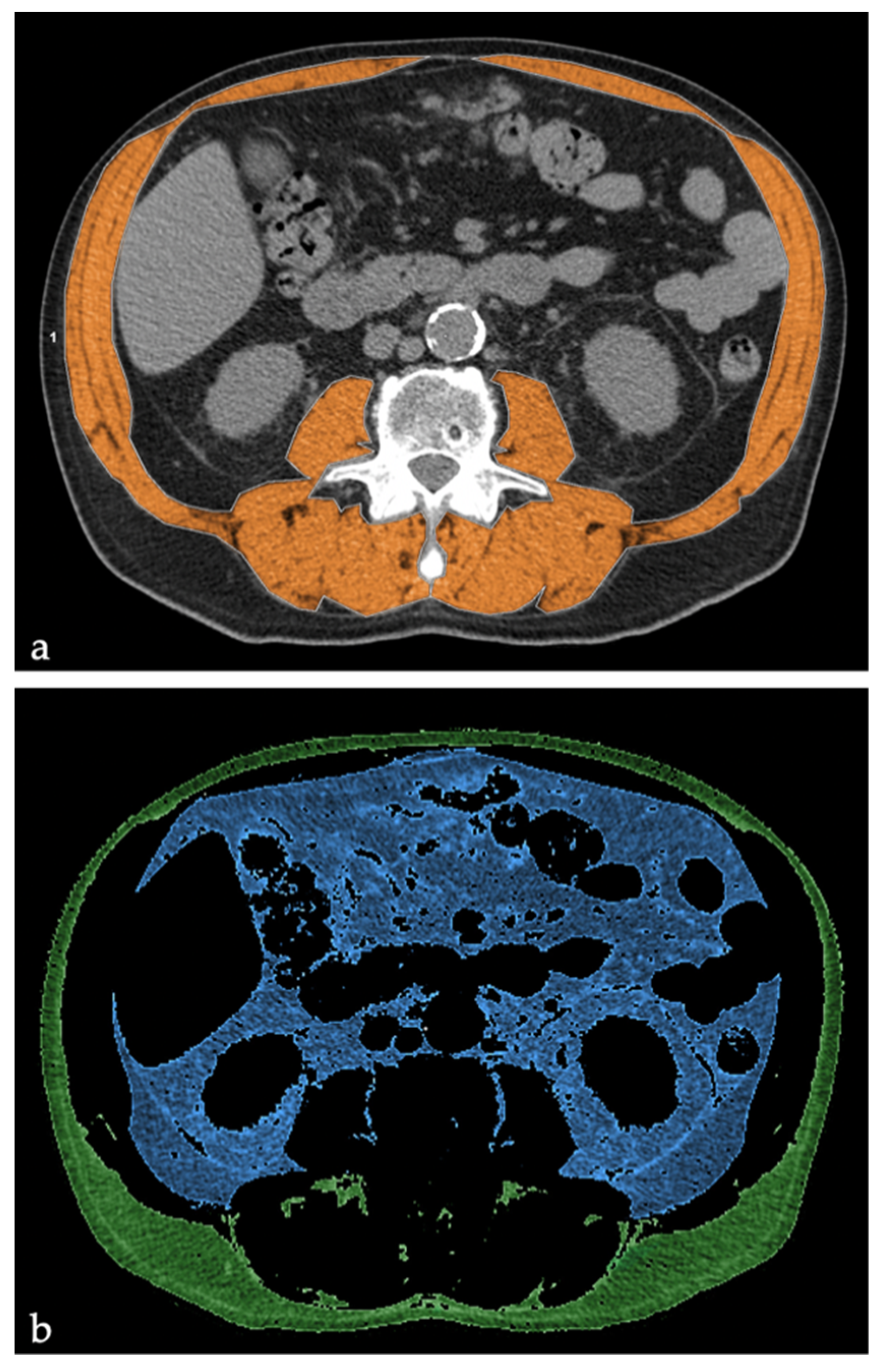
2.1. Body Composition Parameter Measurements
2.2. Statistical Analysis
3. Results
3.1. Patients Characteristics
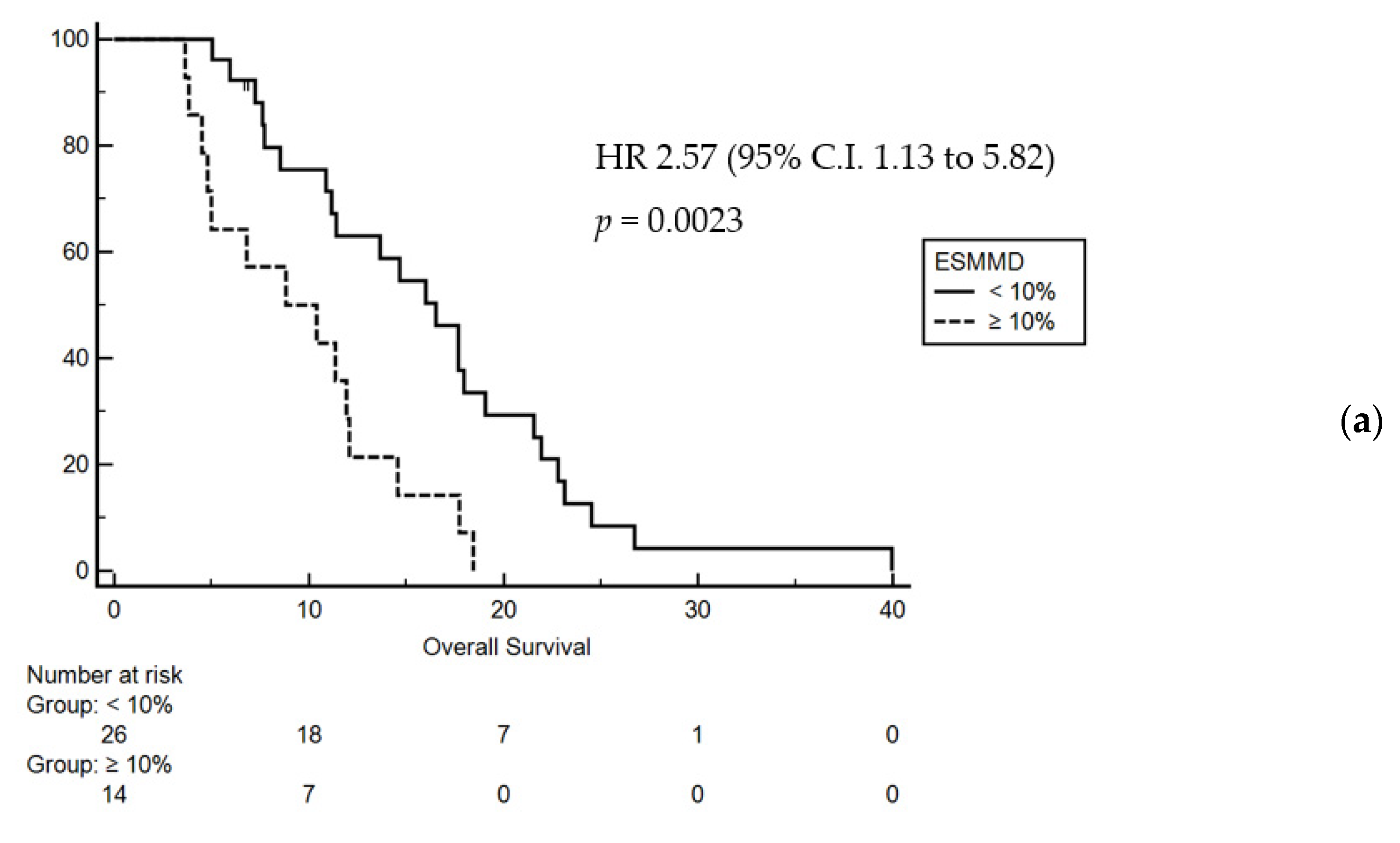
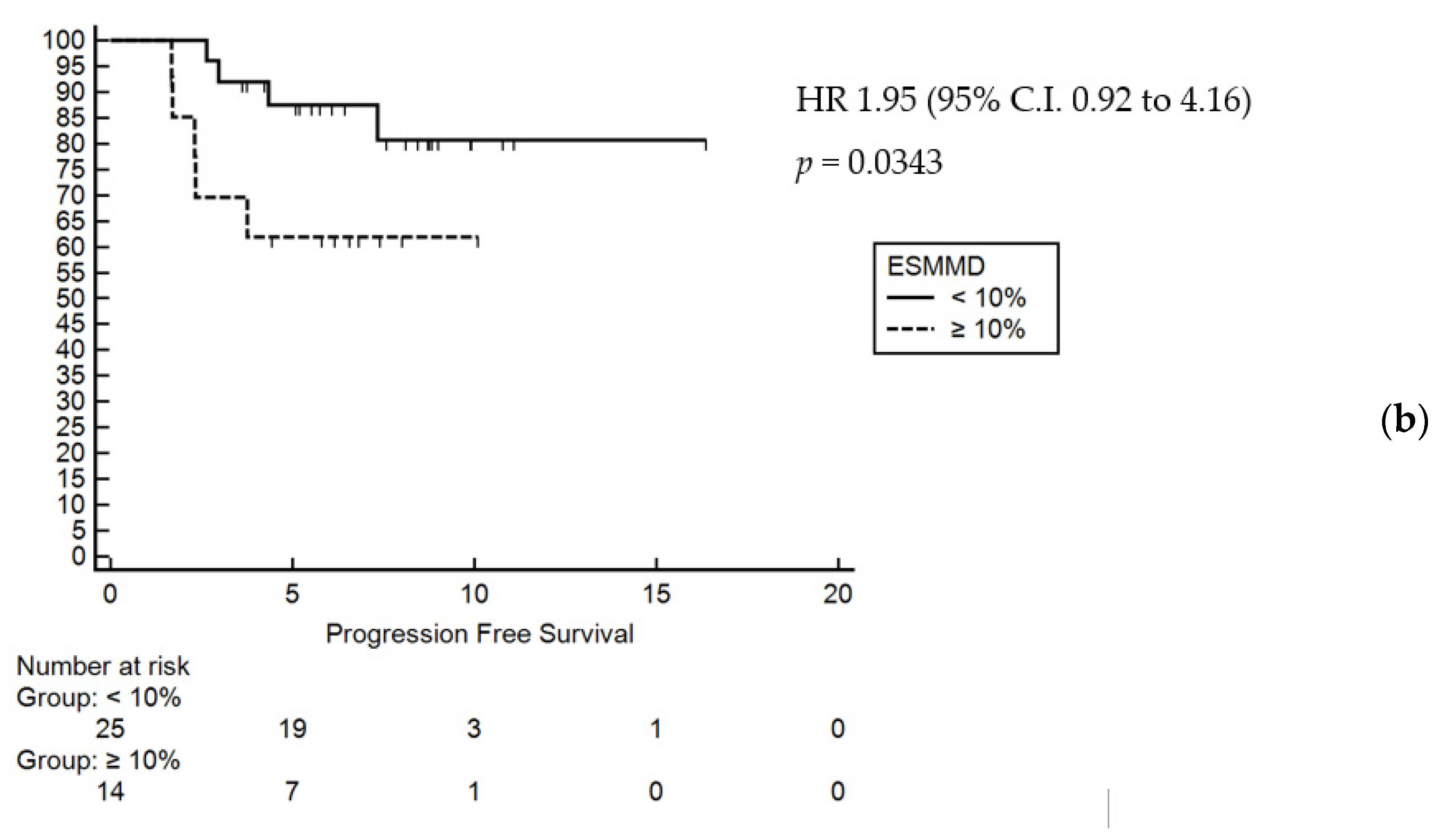
3.2. Prognostic Factors
3.3. Role of Nutritional Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Salati, M.; Di Emidio, K.; Tarantino, V.; Cascinu, S. Second-line treatments: Moving towards an opportunity to improve survival in advanced gastric cancer? ESMO Open 2017, 2, e000206. [Google Scholar] [CrossRef]
- Wagner, A.D.; Syn, N.L.X.; Moehler, M.; Grothe, W.; Yong, W.P.; Tai, B.-C.C.; Ho, J.; Unverzagt, S.; Wagner, D.A.; Syn, L.X.N.; et al. Chemotherapy for advanced gastric cancer Systematic Review. Cochrane Database Syst. Rev. 2017, 2017, 8. [Google Scholar] [CrossRef]
- Shitara, K.; Bang, Y.-J.; Iwasa, S.; Sugimoto, N.; Ryu, M.-H.; Sakai, D.; Chung, H.-C.; Kawakami, H.; Yabusaki, H.; Lee, J.; et al. Trastuzumab Deruxtecan in Previously Treated HER2-Positive Gastric Cancer. N. Engl. J. Med. 2020, 382, 2419–2430. [Google Scholar] [CrossRef]
- Shitara, K.; Van Cutsem, E.; Bang, Y.J.; Fuchs, C.; Wyrwicz, L.; Lee, K.W.; Kudaba, I.; Garrido, M.; Chung, H.C.; Lee, J.; et al. Efficacy and Safety of Pembrolizumab or Pembrolizumab Plus Chemotherapy vs Chemotherapy Alone for Patients with First-line, Advanced Gastric Cancer: The KEYNOTE-062 Phase 3 Randomized Clinical Trial. JAMA Oncol. 2020, 6, 1571–1580. [Google Scholar] [CrossRef] [PubMed]
- Wilke, H.; Muro, K.; Van Cutsem, E.; Oh, S.C.; Bodoky, G.; Shimada, Y.; Hironaka, S.; Sugimoto, N.; Lipatov, O.; Kim, T.Y.; et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): A double-blind, randomised phase 3 trial. Lancet Oncol. 2014, 15, 1224–1235. [Google Scholar] [CrossRef]
- Fuchs, C.S.; Tomasek, J.; Yong, C.J.; Dumitru, F.; Passalacqua, R.; Goswami, C.; Safran, H.; dos Santos, L.V.; Aprile, G.; Ferry, D.R.; et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): An international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet 2014, 383, 31–39. [Google Scholar] [CrossRef]
- Bang, Y.-J.; Van Cutsem, E.; Feyereislova, A.; Chung, H.C.; Shen, L.; Sawaki, A.; Lordick, F.; Ohtsu, A.; Omuro, Y.; Satoh, T.; et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): A phase 3, open-label, randomised controlled trial. Lancet 2010, 376, 687–697. [Google Scholar] [CrossRef]
- Demirelli, B.; Babacan, N.A.; Ercelep, Ö.; Öztürk, M.A.; Kaya, S.; Tanrıkulu, E.; Khalil, S.; Hasanov, R.; Alan, Ö.; Telli, T.A.; et al. Modified Glasgow Prognostic Score, Prognostic Nutritional Index and ECOG Performance Score Predicts Survival Better than Sarcopenia, Cachexia and Some Inflammatory Indices in Metastatic Gastric Cancer. Nutr. Cancer 2021, 73, 230–238. [Google Scholar] [CrossRef]
- Ter Veer, E.; van Kleef, J.J.; Schokker, S.; van der Woude, S.O.; Laarman, M.; Mohammad, N.H.; Sprangers, M.A.; van Oijen, M.G.; van Laarhoven, H.W. Prognostic and predictive factors for overall survival in metastatic oesophagogastric cancer: A systematic review and meta-analysis. Eur. J. Cancer 2018, 103, 214–226. [Google Scholar] [CrossRef]
- Casadei-Gardini, A.; Scarpi, E.; Ulivi, P.; Palladino, M.A.; Accettura, C.; Bernardini, I.; Spallanzani, A.; Gelsomino, F.; Corbelli, J.; Marisi, G.; et al. Prognostic role of a new inflammatory index with neutrophil-to-lymphocyte ratio and lactate dehydrogenase (CII: Colon Inflammatory Index) in patients with metastatic colorectal cancer: Results from the randomized Italian Trial in Advanced Colorectal Cancer. Cancer Manag. Res. 2019, 11, 4357–4369. [Google Scholar] [CrossRef]
- Grenader, T.; Waddell, T.; Peckitt, C.; Oates, J.; Starling, N.; Cunningham, D.; Bridgewater, J. Prognostic value of neutrophil-to-lymphocyte ratio in advanced oesophago-gastric cancer: Exploratory analysis of the REAL-2 trial. Ann. Oncol. 2016, 27, 687–692. [Google Scholar] [CrossRef]
- Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Fearon, K.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN guidelines on nutrition in cancer patients. Clin. Nutr. 2017, 36, 11–48. [Google Scholar] [CrossRef]
- Cushen, S.J.; Power, D.G.; Murphy, K.P.; McDermott, R.; Griffin, B.T.; Lim, M.; Daly, L.; MacEneaney, P.; O’Sullivan, K.; Prado, C.M.; et al. Impact of body composition parameters on clinical outcomes in patients with metastatic castrate-resistant prostate cancer treated with docetaxel. Clin. Nutr. ESPEN 2016, 13, e39–e45. [Google Scholar] [CrossRef]
- Martin, L.; Birdsell, L.; MacDonald, N.; Reiman, T.; Clandinin, M.T.; McCargar, L.J.; Murphy, R.; Ghosh, S.; Sawyer, M.B.; Baracos, V.E. Cancer Cachexia in the Age of Obesity: Skeletal Muscle Depletion Is a Powerful Prognostic Factor, Independent of Body Mass Index. J. Clin. Oncol. 2013, 31, 1539–1547. [Google Scholar] [CrossRef]
- Ryan, A.M.; Prado, C.M.; Sullivan, E.S.; Power, D.G.; Daly, L.E. Effects of weight loss and sarcopenia on response to chemotherapy, quality of life, and survival. Nutrition 2019, 67–68, 110539. [Google Scholar] [CrossRef]
- Omarini, C.; Palumbo, P.; Pecchi, A.; Draisci, S.; Balduzzi, S.; Nasso, C.; Barbolini, M.; Isca, C.; Bocconi, A.; Moscetti, L.; et al. Predictive Role of Body Composition Parameters in Operable Breast Cancer Patients Treated with Neoadjuvant Chemotherapy. Cancer Manag. Res. 2019, 11, 9563–9569. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Rinninella, E.; Cintoni, M.; Raoul, P.; Pozzo, C.; Strippoli, A.; Bria, E.; Tortora, G.; Gasbarrini, A.; Mele, M.C. Effects of nutritional interventions on nutritional status in patients with gastric cancer: A systematic review and meta-analysis of randomized controlled trials. Clin. Nutr. ESPEN 2020, 38, 28–42. [Google Scholar] [CrossRef]
- Hamaguchi, Y.; Kaido, T.; Okumura, S.; Kobayashi, A.; Shirai, H.; Yagi, S.; Kamo, N.; Okajima, H.; Uemoto, S. Impact of Skeletal Muscle Mass Index, Intramuscular Adipose Tissue Content, and Visceral to Subcutaneous Adipose Tissue Area Ratio on Early Mortality of Living Donor Liver Transplantation. Transplantation 2017, 101, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Waki, Y.; Irino, T.; Makuuchi, R.; Notsu, A.; Kamiya, S.; Tanizawa, Y.; Bando, E.; Kawamura, T.; Terashima, M. Impact of Preoperative Skeletal Muscle Quality Measurement on Long-Term Survival After Curative Gastrectomy for Locally Advanced Gastric Cancer. World J. Surg. 2019, 43, 3083–3093. [Google Scholar] [CrossRef]
- Ebadi, M.; Martin, L.; Ghosh, S.; Field, C.J.; Lehner, R.; Baracos, E.V.; Mazurak, V.C. Subcutaneous adiposity is an independent predictor of mortality in cancer patients. Br. J. Cancer 2017, 117, 148–155. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.X.; Lin, J.P.; Xie, J.; Wang, J.; Lu, J.; Chen, Q.; Cao, L.; Lin, M.; Tu, R.; Zheng, C.; et al. Prognostic Value and Association of Sarcopenia and Systemic Inflammation for Patients with Gastric Cancer Following Radical Gastrectomy. Oncologist 2019, 24. [Google Scholar] [CrossRef] [PubMed]
- Sugiyama, K.; Narita, Y.; Mitani, S.; Honda, K.; Masuishi, T.; Taniguchi, H.; Kadowaki, S.; Ura, T.; Ando, M.; Tajika, M.; et al. Baseline Sarcopenia and Skeletal Muscle Loss During Chemotherapy Affect Survival Outcomes in Metastatic Gastric Cancer. Anticancer. Res. 2018, 38, 5859–5866. [Google Scholar] [CrossRef] [PubMed]
- Rinninella, E.; Cintoni, M.; Raoul, P.; Pozzo, C.; Strippoli, A.; Bria, E.; Tortora, G.; Gasbarrini, A.; Mele, M.C. Muscle mass, assessed at diagnosis by L3-CT scan as a prognostic marker of clinical outcomes in patients with gastric cancer: A systematic review and meta-analysis. Clin. Nutr. 2020, 39, 2045–2054. [Google Scholar] [CrossRef]
- Dijksterhuis, W.P.M.; Pruijt, M.J.; Van Der Woude, S.O.; Klaassen, R.; Kurk, S.A.; Van Oijen, M.G.H.; Van Laarhoven, H.W.M. Association between body composition, survival, and toxicity in advanced esophagogastric cancer patients receiving palliative chemotherapy. J. Cachex Sarcopenia Muscle 2019, 10, 199–206. [Google Scholar] [CrossRef]
- Choi, Y.; Oh, D.-Y.; Kim, T.-Y.; Lee, K.-H.; Han, S.-W.; Im, S.-A.; Bang, Y.-J. Skeletal Muscle Depletion Predicts the Prognosis of Patients with Advanced Pancreatic Cancer Undergoing Palliative Chemotherapy, Independent of Body Mass Index. PLoS ONE 2015, 10, e0139749. [Google Scholar] [CrossRef]
- Blauwhoff-Buskermolen, S.; Versteeg, K.S.; De Van Der Schueren, M.A.E.; Braver, N.R.D.; Berkhof, J.; Langius, J.A.E.; Verheul, H.M.W. Loss of Muscle Mass During Chemotherapy Is Predictive for Poor Survival of Patients with Metastatic Colorectal Cancer. J. Clin. Oncol. 2016, 34, 1339–1344. [Google Scholar] [CrossRef]
- Basile, D.; Parnofiello, A.; Vitale, M.G.; Cortiula, F.; Gerratana, L.; Fanotto, V.; Lisanti, C.; Pelizzari, G.; Ongaro, E.; Bartoletti, M.; et al. The IMPACT study: Early loss of skeletal muscle mass in advanced pancreatic cancer patients. J. Cachex. Sarcopenia Muscle 2019, 10, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Rier, H.N.; Jager, A.; Sleijfer, S.; van Rosmalen, J.; Kock, M.C.; Levin, M.-D. Low muscle attenuation is a prognostic factor for survival in metastatic breast cancer patients treated with first line palliative chemotherapy. Breast 2017, 31, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Antoun, S.; Lanoy, E.; Iacovelli, R.; Albiges-Sauvin, L.; Loriot, Y.; Merad-Taoufik, M.; Fizazi, K.; Di Palma, M.; Baracos, V.E.; Escudier, B. Skeletal muscle density predicts prognosis in patients with metastatic renal cell carcinoma treated with targeted therapies. Cancer 2013, 119, 3377–3384. [Google Scholar] [CrossRef] [PubMed]
- Ataseven, B.; Luengo, T.G.; Du Bois, A.; Waltering, K.-U.; Traut, A.; Heitz, F.; Alesina, P.F.; Prader, S.; Meier, B.; Schneider, S.; et al. Skeletal Muscle Attenuation (Sarcopenia) Predicts Reduced Overall Survival in Patients with Advanced Epithelial Ovarian Cancer Undergoing Primary Debulking Surgery. Ann. Surg. Oncol. 2018, 25, 3372–3379. [Google Scholar] [CrossRef]
- Van Dijk, D.; Bakens, M.; Coolsen, M.; Rensen, S.; Van Dam, R.; Bours, M.; Weijenberg, M.; De Jong, C.; Damink, S.O. Reduced survival in pancreatic cancer patients with low muscle attenuation index. HPB 2016, 18, e756. [Google Scholar] [CrossRef][Green Version]
- Feliciano, E.M.C.; Kroenke, C.H.; Meyerhardt, J.A.; Prado, C.M.; Bradshaw, P.T.; Kwan, M.L.; Xiao, J.; Alexeeff, S.; Corley, D.; Weltzien, E.; et al. Association of Systemic Inflammation and Sarcopenia with Survival in Nonmetastatic Colorectal Cancer: Results From the C SCANS Study. JAMA Oncol. 2017, 3, e172319. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.Y.; Kim, Y.S.; Seo, J.-Y.; Park, I.; Ahn, H.K.; Jeong, Y.M.; Kim, J.H.; Kim, N. The Relationship between Sarcopenia and Systemic Inflammatory Response for Cancer Cachexia in Small Cell Lung Cancer. PLoS ONE 2016, 11, e0161125. [Google Scholar] [CrossRef] [PubMed]
- Da Fonseca, G.W.P.; Farkas, J.; Dora, E.; Von Haehling, S.; Lainscak, M. Cancer Cachexia and Related Metabolic Dysfunction. Int. J. Mol. Sci. 2020, 21, 2321. [Google Scholar] [CrossRef] [PubMed]
- Caccialanza, R.; Cereda, E.; Caraccia, M.; Klersy, C.; Nardi, M.; Cappello, S.; Borioli, V.; Turri, A.; Imarisio, I.; Lasagna, A.; et al. Early 7-day supplemental parenteral nutrition improves body composition and muscle strength in hypophagic cancer patients at nutritional risk. Clin. Nutr. 2018, 37, S14. [Google Scholar] [CrossRef]
- De Waele, E.; Mattens, S.; Honoré, P.M.; Spapen, H.; De Grève, J.; Pen, J.J. Nutrition therapy in cachectic cancer patients. The Tight Caloric Control (TiCaCo) pilot trial. Appetite 2015, 91, 298–301. [Google Scholar] [CrossRef]
- Kapoor, N.D.; Twining, P.K.; Groot, O.Q.; Pielkenrood, B.J.; Bongers, M.E.R.; Newman, E.T.; Verlaan, J.J.; Schwab, J.H. Adipose tissue density on CT as a prognostic factor in patients with cancer: A systematic review. Acta Oncol. 2020, 59, 1488–1495. [Google Scholar] [CrossRef]
- Okumura, S.; Kaido, T.; Hamaguchi, Y.; Kobayashi, A.; Shirai, H.; Yao, S.; Yagi, S.; Kamo, N.; Hatano, E.; Okajima, H.; et al. Visceral Adiposity and Sarcopenic Visceral Obesity are Associated with Poor Prognosis After Resection of Pancreatic Cancer. Ann. Surg. Oncol. 2017, 24, 3732–3740. [Google Scholar] [CrossRef]
- Okumura, S.; Kaido, T.; Hamaguchi, Y.; Kobayashi, A.; Shirai, H.; Fujimoto, Y.; Iida, T.; Yagi, S.; Taura, K.; Hatano, E.; et al. Impact of Skeletal Muscle Mass, Muscle Quality, and Visceral Adiposity on Outcomes Following Resection of Intrahepatic Cholangiocarcinoma. Ann. Surg. Oncol. 2016, 24, 1037–1045. [Google Scholar] [CrossRef]
- Park, H.S.; Kim, H.S.; Beom, S.H.; Rha, S.Y.; Chung, H.C.; Kim, J.H.; Chun, Y.J.; Lee, S.W.; Choe, E.-A.; Heo, S.J.; et al. Marked Loss of Muscle, Visceral Fat, or Subcutaneous Fat After Gastrectomy Predicts Poor Survival in Advanced Gastric Cancer: Single-Center Study from the CLASSIC Trial. Ann. Surg. Oncol. 2018, 25, 3222–3230. [Google Scholar] [CrossRef]
- Guiu, B.; Petit, J.M.; Bonnetain, F.; Ladoire, S.; Guiu, S.; Cercueil, J.-P.; Krausé, D.; Hillon, P.; Borg, C.; Chauffert, B.; et al. Visceral fat area is an independent predictive biomarker of outcome after first-line bevacizumab-based treatment in metastatic colorectal cancer. Gut 2009, 59, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Brandl, A. Prognostischer Einfluss von Fettgewebsdichte und Muskelmasse beim fortgeschrittenen kolorektalen Karzinom. Prognostic value of adipose tissue and muscle mass in advanced colorectal cancer. Coloproctology 2019, 41, 218–219. [Google Scholar] [CrossRef]
| Variable | N(%) |
|---|---|
| Age | |
| <70 years | 33 (82.5%) |
| ≥70 years | 7 (17.5%) |
| Gender | |
| Male | 24 (60.0%) |
| Female | 16 (40.0%) |
| Site of primary tumor | |
| Gastroesophageal junction | 5 (12.5%) |
| Fundus | 3 (7.5%) |
| Body | 12 (30.0%) |
| Fundus and body | 4 (10.0%) |
| GE junction, fundus and body | 1 (2.5%) |
| Antrum | 7 (17.5%) |
| Body and antrum | 6 (15.0%) |
| Diffuse/linitis | 2 (5.0%) |
| Previous gastrectomy | |
| Yes | 6 (15.0%) |
| No | 34 (85%) |
| Eastern Cooperative Oncology Group Performace Status (ECOG PS) at 1^line chemotherapy start | |
| 0–1 | 35 (87.5%) |
| ≥2 | 5 (12.5%) |
| N° of metastatic sites at 1^line chemotherapy start | |
| 1 | 12 (30.0%) |
| ≥2 | 27 (67.5%) |
| Unknown | 1 (2.5%) |
| Metastatic site at 1^line chemotherapy start | |
| Liver | 5 (12.5%) |
| Nodes | 11 (27.5%) |
| Peritoneum | 24 (60.0%) |
| Lung | 4 (10.0%) |
| Bone | 11 (27.5%) |
| Others | 5 (12.5%) |
| Body mass index—BMI (kg/m2) | |
| <25 | 28 (70.0%) |
| ≥25 | 12 (30.0%) |
| Prognostic nutritional index—PNI | |
| <38.6 | 8 (20.0%) |
| ≥38.6 | 18 (45.0%) |
| Unknown | 14 (35.0%) |
| Type of first line treatment | |
| Single agent | 2 (5.0%) |
| Combination | 38 (95.0%) |
| Laboratory parameter at first-line chemotherapy start | |
| Neutrophil-lymphocyte Ratio—NLR (Mean ± standard deviation) | 5.1 ± 3.5 |
| <4.8 | 17 (42.5%) |
| ≥4.8 | 11 (27.5%) |
| Unknown | 12 (30.0%) |
| Platelet-lymphocyte ratio—PLR (Mean ± standard deviation) | 260.8 ± 127.1 |
| <217 | 12 (30.0%) |
| ≥217 | 16 (40.0%) |
| Unknown | 12 (30.0%) |
| Lymphocyte-monocyte ratio—LMR (Mean ± standard deviation) | 3.0 ± 1.4 |
| ≤2.1 | 7 (17.5%) |
| >2.1 | 21 (52.5%) |
| Unknown | 12 (30.0%) |
| Systemic Immune-Inflammation Index (SII) (Mean ± standard deviation) (×103 cells/µL | 1465 ± 1041 |
| ≤1110 | 20 (30.0%) |
| >1110 | 16 (40.0%) |
| Unknown | 12 (30.0%) |
| Albumine (Mean ± standard deviation) (g/dL) | 3.6 ± 0.5 |
| ≤3.5 | 19 (47.5%) |
| >3.5 | 17 (42.5%) |
| Unknown | 4 (10.0%) |
| C reactive Protein—PCR (Mean ± standard deviation) (mg/dL) | 3,2 ± 4,6 |
| <2.2 | 13 (32.5%) |
| ≥2.2 | 8 (20.0%) |
| Unknown | 19 (47.5%) |
| Carcinoembryonic antigen—CEA (Mean ± standard deviation) (ng/mL) | 201.6 ± 683.2 |
| ≤5 | 23 (57.5%) |
| >5 | 14 (35.0%) |
| Unknown | 3 (7.5%) |
| Carbohydrate antigen 19.9—Ca 19.9 (Mean ± standard deviation) (U/mL) | 622 ± 1856 |
| ≤37 | 20 (50.0%) |
| >37 | 17 (42.5%) |
| Unknown | 3 (7.5%) |
| Univariate | Multivariate | ||
|---|---|---|---|
| HR (95% CI) | p | ||
| Age (≥65 vs. <65 years) | 1.08 (0.57–2.07) | 0.8110 | |
| ECOG PS (2 vs. 0–1) | 12.75 (0.67–243.86) | <0.0001 | 0.0001 |
| Site of M (>1 vs. 1) | 1.92 (0.90–4.11) | 0.058 | |
| NLR (≥4.8 vs. <4.8) | 2.00 (0.84–4.75) | 0.0711 | |
| LMR (<2.1 vs. ≥2.1) | 3.03 (0.88–10.46) | 0.0060 | |
| PCR (≥2.2 vs. <2.2 mg/dL) | 3.1 (0.98–9.78) | 0.0055 | |
| CEA (≥5 vs. <5 ng/mL) | 0.67 (0.33 to 1.36) | 0.2763 | |
| PNI (≥38.6 vs. <38.6) | 0.34 (0.11–1.06) | 0.0058 | |
| SII (≥1110 vs. <1110 (×103 cells/µL) | 0.95 (0.44–2.07) | 0.9104 | |
| BMI (<25 vs. ≥25 kg/m2) | 0.79 (0–37–1.70) | 0.5215 | |
| IMAC (≤−0.33 vs. >−0.33) | 0.67 (0.34–1.32) | 0.2233 | |
| VFI (≥52.9 cm2/m2 in males and 51.5 cm2/m2 in females vs. <52.9 cm2/m2 in males and 51.5 cm2/m2 in females) | 1.24 (0.66–2.36) | 0.5010 | |
| SFI (≤50 cm2/m2 in males and 42 cm2/m2 in females vs. >50 cm2/m2 in males and 42 cm2/m2 in females) | 0.76 (0.40–1.43) | 0.3921 | |
| Sarcopenia sec. Martin (Yes vs. No) | 1.40 (0.72–2.73) | 0.3058 | |
| Sarcopenia at revaluation sec. Martin (Yes vs. No) | 2.24 (1.07–4.69 | 0.0117 | |
| ESMMD (≥10% vs. <10%) | 2.57 (1.13–5.83) | 0.0036 | 0.0375 |
| Occasional Nutritional Evaluation (n = 20) | Systematic Nutritional Evaluation (n = 20) | p | |
|---|---|---|---|
| Age | |||
| <70 years | 16 (80%) | 17 (85%) | 1.00 |
| ≥70 years | 4 (20%) | 3 (15%) | |
| Gender | |||
| Male | 13 (65%) | 11 (55%) | 0.54 |
| Female | 7 (35%) | 9 (45%) | |
| Site of primary tumor | |||
| Gastroesophageal junction | 4 (20%) | 1 (5%) | 0.2334 |
| Fundus | 3 (15%) | 0 | |
| Body | 4 (20%) | 8 (40%) | |
| Fundus and body | 2 (10%) | 2 (10%) | |
| GE junction, fundus and body | 1 (5%) | 0 | |
| Antrum | 3 (15%) | 4 (20%) | |
| Body and antrum | 3 (15%) | 3 (15%) | |
| Diffuse/linitis | 0 | 2 (10%) | |
| Previous gastrectomy | |||
| Yes | 3 (15%) | 3 (15%) | |
| No | 17 (85%) | 17 (85%) | |
| ECOG PS at 1^line chemotherapy start | |||
| 0–1 | 19 (95%) | 16 (80%) | 0.3416 |
| ≥2 | 1 (5%) | 4 (20%) | |
| N° of metastatic sites at 1^line chemotherapy start | |||
| 1 | 7 (35%) | 5 (25%) | 0.7311 |
| ≥2 | 13 (65%) | 14 (70%) | |
| Unknown | 0 | 1 (5%) | |
| Metastatic site at 1^line chemotherapy start | |||
| Liver | 1 (5%) | 4 (20%) | 0.1173 |
| Nodes | 8 (40%) | 3 (15%) | |
| Peritoneum | 11 (55%) | 13 (65%) | |
| Lung | 1 (5%) | 3 (15%) | |
| Bone | 8 (40%) | 3 (15%) | |
| Others | 4 (20%) | 1 (5%) | |
| Body mass index—BMI (kg/m2) | |||
| <25 | 14 (70%) | 14 (70%) | 1.00 |
| ≥25 | 6 (30%) | 6 (30%) | |
| Prognostic nutritional index—PNI | |||
| <38.6 | 2 (10%) | 6 (30%) | 0.2077 |
| ≥38.6 | 9 (45%) | 9 (45%) | |
| Unknown | 9 (45%) | 5 (25%) | |
| Type of first line treatment | |||
| Single agent | 1 (5%) | 1 (5%) | 1.00 |
| Combination | 19 (95%) | 19 (95%) | |
| Laboratory parameter at first-line chemotherapy start | |||
| Neutrophil-lymphocyte Ratio— NLR (Mean ± standard deviation) | 4.6 ± 1.9 | 5.5 ± 4.2 | |
| <4.8 | 7 (35%) | 10 (50%) | 0.3765 |
| ≥4.8 | 5 (25%) | 6 (30%) | |
| Unknown | 8 (40%) | 4 (20%) | |
| Platelet-lymphocyte ratio— PLR (Mean ± standard deviation) | 240.4 ± 81.9 | 276.1 ± 150.6 | |
| <217 | 5 (25%) | 7 (35%) | 0.3835 |
| ≥217 | 7 (35%) | 9 (45%) | |
| Unknown | 8 (40%) | 4 (20%) | |
| Lymphocyte-monocyte ratio— LMR (Mean ± standard deviation) | 2.8 ± 1.4 | 3.1 ± 1.5 | |
| ≤2.1 | 3 (15%) | 4 (20%) | 0.3858 |
| >2.1 | 9 (45%) | 12 (60%) | |
| Unknown | 8 (40%) | 4 (20%) | |
| Lactate dehydrogenase— LDH (Mean ± standard deviation) (U/L) | 631 ± 460 | 505 ± 661 | |
| ≤460 | 8 (40%) | 15 (75%) | 0.0769 |
| >460 | 6 (30%) | 2 (10%) | |
| Unknown | 6 (30%) | 3 (15%) | |
| Albumine (Mean ± standard deviation) (g/dL) | 3,7 ± 0,5 | 3,4 ± 0,5 | |
| ≤ 3.5 | 8 (40%) | 11 (55%) | 0.6056 |
| > 3.5 | 10 (50%) | 7 (35%) | |
| Unknown | 2 (10%) | 2 (10%) | |
| C reactive Protein— PCR (Mean ± standard deviation) (mg/dL) | 3.7 ± 5.2 | 3.0 ± 4.2 | |
| <2.2 | 4 (20%) | 9 (45%) | 0.0820 |
| ≥2.2 | 3 (15%) | 5 (25%) | |
| Unknown | 13 (65%) | 6 (30%) | |
| Carcinoembryonic antigen— CEA (Mean ± standard deviation) (ng/mL) | 178.5 ± 537.3 | 216.2 ± 744.4 | |
| ≤5 | 11 (55%) | 12 (60%) | 0.8283 |
| >5 | 7 (35%) | 7 (35%) | |
| Unknown | 2 (10%) | 1 (5%) | |
| Carbohydrate antigen 19.9— Ca 19.9 (Mean ± standard deviation) (U/mL) | 646.7 ± 1013.6 | 604.9 ± 2217.4 | |
| ≤37 | 9 (45%) | 11 (55%) | 0.529 |
| >37 | 9 (45%) | 8 (40%) | |
| Unknown | 2 (10%) | 1 (5%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rimini, M.; Pecchi, A.; Prampolini, F.; Bussei, C.; Salati, M.; Forni, D.; Martelli, F.; Valoriani, F.; Canino, F.; Bocconi, A.; et al. The Prognostic Role of Early Skeletal Muscle Mass Depletion in Multimodality Management of Patients with Advanced Gastric Cancer Treated with First Line Chemotherapy: A Pilot Experience from Modena Cancer Center. J. Clin. Med. 2021, 10, 1705. https://doi.org/10.3390/jcm10081705
Rimini M, Pecchi A, Prampolini F, Bussei C, Salati M, Forni D, Martelli F, Valoriani F, Canino F, Bocconi A, et al. The Prognostic Role of Early Skeletal Muscle Mass Depletion in Multimodality Management of Patients with Advanced Gastric Cancer Treated with First Line Chemotherapy: A Pilot Experience from Modena Cancer Center. Journal of Clinical Medicine. 2021; 10(8):1705. https://doi.org/10.3390/jcm10081705
Chicago/Turabian StyleRimini, Margherita, Annarita Pecchi, Francesco Prampolini, Chiara Bussei, Massimiliano Salati, Daniela Forni, Francesca Martelli, Filippo Valoriani, Fabio Canino, Alessandro Bocconi, and et al. 2021. "The Prognostic Role of Early Skeletal Muscle Mass Depletion in Multimodality Management of Patients with Advanced Gastric Cancer Treated with First Line Chemotherapy: A Pilot Experience from Modena Cancer Center" Journal of Clinical Medicine 10, no. 8: 1705. https://doi.org/10.3390/jcm10081705
APA StyleRimini, M., Pecchi, A., Prampolini, F., Bussei, C., Salati, M., Forni, D., Martelli, F., Valoriani, F., Canino, F., Bocconi, A., Gelsomino, F., Reverberi, L., Benatti, S., Piacentini, F., Menozzi, R., Dominici, M., Luppi, G., & Spallanzani, A. (2021). The Prognostic Role of Early Skeletal Muscle Mass Depletion in Multimodality Management of Patients with Advanced Gastric Cancer Treated with First Line Chemotherapy: A Pilot Experience from Modena Cancer Center. Journal of Clinical Medicine, 10(8), 1705. https://doi.org/10.3390/jcm10081705






