Can Psychological Empowerment Prevent Emotional Disorders in Presence of Fear of COVID-19 in Health Workers? A Cross-Sectional Validation Study
Abstract
1. Introduction
1.1. Current Situation of the Fear of COVID-19
1.2. Job Crafting and Psychological Empowerment
2. Materials and Methods
2.1. Participants and Procedure
2.2. Instrument
2.3. Data Analysis
3. Results
3.1. Global Model
3.2. Measurement Model
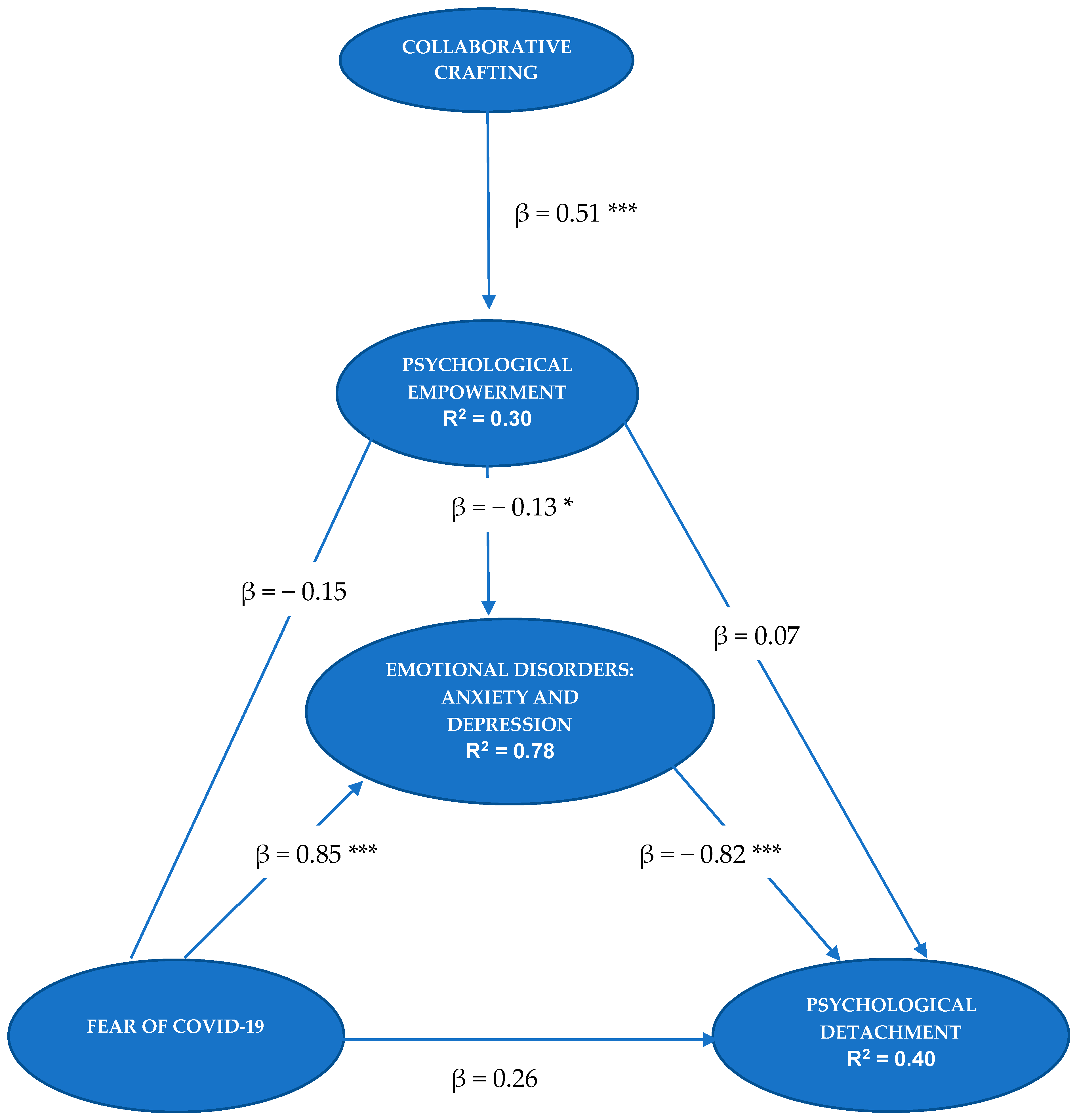
3.3. Structural Model
3.4. MICOM Model: Analysis of the Invariance of the Measurement Model
3.4.1. First Stage: Configuration Invariance
3.4.2. Second Stage: Composite Invariance
3.4.3. Third Stage: Evaluation of Equal Means and Variances of the Composite Variables
4. Discussion
4.1. Limitations
4.2. Future Lines of Research and Practical Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef] [PubMed]
- De Brier, N.; Stroobants, S.; Vandekerckhove, P.; De Buck, E. Factors Affecting Mental Health of Health Care Workers during Coronavirus Disease Outbreaks (SARS, MERS & COVID-19): A Rapid Systematic Review. PLoS ONE 2020, 15, e0244052. [Google Scholar]
- Center for Sociological Research, CIS. Efectos y Consecuencias del Coronavirus (I). Estudio nº 3298. Available online: http://www.cis.es/cis/export/sites/default/-Archivos/Marginales/3280_3299/3298/es3298mar.pdf (accessed on 31 October 2020).
- Center for Sociological Research, CIS. Efectos y Consecuencias del Coronavirus (III). Estudio nº 3305. Available online: http://datos.cis.es/pdf/Es3305marMT_A.pdf. (accessed on 28 December 2020).
- Pastor-Barriuso, R.; Pérez-Gómez, B.; Hernán, M.; Pérez-Olmeda, M.; Yotti, R.; Oteo-Iglesias, J.; Sanmartín, J.; León-Gómez, I.; Fernández-García, A.; Fernández-Navarro, P.; et al. Infection fatality risk for SARS-CoV-2 in community dwelling population of Spain: nationwide seroepidemiological study. BMJ 2020, 371, m4509. [Google Scholar] [CrossRef] [PubMed]
- Royal Spanish Academy. Diccionario de la Lengua Española, 23th ed. Version 23.4 Online. Available online: https://dle.rae.es (accessed on 21 February 2021).
- Goyal, K.; Chauhan, P.; Chhikara, K.; Gupta, P.; Singh, M. Fear of COVID 2019: First Suicidal Case in India. Asian J. Psychiatr. 2020, 49, 101989. [Google Scholar] [CrossRef]
- Pakpour, A.; Griffiths, M. The fear of COVID-19 and its role in preventive behaviors. J. Concurr. Disord. 2020, 2, 58–63. Available online: http://irep.ntu.ac.uk/id/eprint/39561/ (accessed on 10 March 2021).
- Gunnell, D.; Appleby, L.; Arensman, E.; Hawton, K.; John, A.; Kapur, N.; Khan, M.; O’Connor, R.; Pirkis, J.; Appleby, L.; et al. Suicide Risk and Prevention during the COVID-19 Pandemic. Lancet Psychiatry 2020, 7, 468–471. [Google Scholar] [CrossRef]
- Ahorsu, D.; Lin, C.; Imani, V.; Saffari, M.; Griffiths, M.; Pakpour, A. The Fear of COVID-19 Scale: Development and Initial Validation. Int J. Ment Health Addict. 2020, 27, 1–9. [Google Scholar] [CrossRef]
- Tzur Bitan, D.; Grossman-Giron, A.; Bloch, Y.; Mayer, Y.; Shiffman, N.; Mendlovic, S. Fear of COVID-19 scale: Psychometric characteristics, reliability and validity in the Israeli population. Psychiatry Res. 2020, 289, 113100. [Google Scholar] [CrossRef]
- Martínez-Lorca, M.; Martínez-Lorca, A.; Criado-Álvarez, J.J.; Armesilla, M.; Latorre, J.M. The fear of COVID-19 scale: Validation in spanish university students. Psychiatry Res. 2020, 293, 113350. [Google Scholar] [CrossRef]
- Soraci, P.; Ferrari, A.; Abbiati, F.A.; Del Fante, E.; De Pace, R.; Urso, A.; Griffiths, M.D. Validation and Psychometric Evaluation of the Italian Version of the Fear of COVID-19 Scale. Int J. Ment Health Addict. 2020, 4, 1–10. [Google Scholar] [CrossRef]
- Reznik, A.; Gritsenko, V.; Konstantinov, V.; Khamenka, N.; Isralowitz, R. COVID-19 Fear in Eastern Europe: Validation of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Alyami, M.; Henning, M.; Krägeloh, C.U.; Alyami, H. Psychometric Evaluation of the Arabic Version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 2020, 1–14, Advance online publication. [Google Scholar] [CrossRef]
- Sakib, N.; Bhuiyan, A.K.M.I.; Hossain, S.; Al Mamun, F.; Hosen, I.; Abdullah, A.H.; Mamun, M.A.; Mohiuddin, M.S.; Rayhan, I.; Hossain, M.; et al. Psychometric Validation of the Bangla Fear of COVID-19 Scale: Confirmatory Factor Analysis and Rasch Analysis. Int J. Ment Health Addict. 2020, 11, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Pang, N.T.P.; Kamu, A.; Hambali, N.L.B.; Mun, H.C.; Kassim, M.A.; Mohamed, N.H.; Ayu, F.; Rahim, S.S.S.A.; Omar, A.; Jeffree, M.S. Malay Version of the Fear of COVID-19 Scale: Validity and Reliability. Int. J. Ment. Health Addict. 2020, 3, 1–10. [Google Scholar] [CrossRef]
- Satici, B.; Gocet-Tekin, E.; Deniz, M.E.; Satici, S.A. Adaptation of the Fear of COVID-19 Scale: Its Association with Psychological Distress and Life Satisfaction in Turkey. Int. J. Ment. Health Addict. 2020, 1–9, Advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Chi, X.; Chen, S.; Chen, Y.; Chen, D.; Yu, Q.; Guo, T.; Cao, Q.; Zheng, X.; Huang, S.; Hossain, M.; et al. Psychometric Evaluation of the Fear of COVID-19 Scale Among Chinese Population. Int J. Ment. Health Addict. 2020, 11, 1–16. [Google Scholar] [CrossRef]
- Da Silva, F.; Neto, M. Psychiatric symptomatology associated with depression, anxiety, distress, and insomnia in health professionals working in patients affected by COVID-19: A systematic review with meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 104, 110057. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Sanz-Vergel, A.I.; Sebastián, J.; Rodríguez-Muñoz, A.; Garrosa, E.; Moreno-Jiménez, B.; Sonnentag, S. Adaptación del Cuestionario de Experiencias de Recuperación a una muestra española. Psicothema 2010, 22, 990–996. [Google Scholar]
- Sonnentag, S.; Arbeus, H.; Mahn, C.; Fritz, C. Exhaustion and lack of psychological detachment from work during off-job time: Moderator effects of time pressure and leisure experiences. J. Occup. Health Psychol. 2014, 19, 206–216. [Google Scholar] [CrossRef]
- Wrzesniewski, A.; Dutton, J.E. Crafting a job: Revisioning employees as active crafters of their work. Acad Manag. Rev. 2001, 26, 179–201. [Google Scholar] [CrossRef]
- Leana, C.; Appelbaum, E.; Schevchuk, I. Work process and quality of care in early childhood education: The role of job crafting. Acad Manag. J. 2009, 52, 1169–1192. [Google Scholar] [CrossRef]
- Llorente-Alonso, M.; Topa, G. Individual Crafting, Collaborative Crafting, and Job Satisfaction: The Mediator Role of Engagement. J. Work Organ. Psychol. 2019, 35, 217–226. [Google Scholar] [CrossRef]
- Miller, M. Relationships between Job Design, Job Crafting, Idiosyncratic Deals, and Psychological Empowerment. Ph.D.Thesis, Walden University, Minneapolis, MI, USA, 2015. Available online: https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=2362&context=dissertations (accessed on 5 February 2021).
- Harbridge, R.R. Psychological Empowerment and Job Crafting among Registered Nurses Working in Public Health in Ontario, Canada. Ph.D. Thesis, Central Michigan University, Mount Pleasant, MI, USA, 2018. Available online: https://scholarly.cmich.edu/?a=d&d=CMUGR2018-096 (accessed on 23 February 2021).
- Demerouti, E. Design your own job through job crafting. Eur. Psychol. 2014, 19, 237–243. [Google Scholar] [CrossRef]
- Spreitzer, G.M. Psychological Empowerment in the workplace: Dimensions, measurement, and validation. Acad Manag. J. 1995, 38, 1442–1465. [Google Scholar] [CrossRef]
- Thomas, K.W.; Velthouse, B.A. Cognitive elements of empowerment: an ’interpretative’ model of intrinsic task motivation. Acad Manag. Rev. 1990, 15, 666–681. [Google Scholar]
- Schermuly, C.C.; Meyer, B. Good relationships at work: The effects of Leader-Member Exchange and Team-Member Exchange on psychological empowerment, emotional exhaustion, and depression. J. Organ. Behav. 2015, 37, 673–691. [Google Scholar] [CrossRef]
- Laschinger, H.K.S.; Finegan, J.; Shamian, J. Promoting Nurses’ Health: Effect of Empowerment on Job Strain and Work Satisfaction. Nurs. Econ. 2001, 19, 42–52. [Google Scholar]
- Petersen, M.B.; Jørgensen, F.J.; Bor, A. Compliance Without Fear: Predictors of Protective Behavior During the First Wave of the COVID-19 Pandemic. PsyArXiv 2021. Available online: osf.io/asczn (accessed on 3 April 2021).
- Ghosh, D.; Sekiguchi, T.; Fujimoto, Y. Psychological Detachment: A creativity perspective on the link between intrinsic motivation and employee engagement. Pers. Rev. 2020, 49, 1789–1804. [Google Scholar] [CrossRef]
- Sheaffer, Z.; Levy, S.; Navot, E. Fears, discrimination and perceived workplace promotion. Balt. J. Manag. 2018, 13, 2–19. [Google Scholar] [CrossRef]
- Jackson, D.N.; Guthrie, G.M.; Astilla, E.; Elwood, B. The cross-cultural generalizability of personality construct measures. In Human Assessment and Cultural Factors; NATO Conference Series; Berry, J.W., Irvine, S.H., Eds.; Springer: Berlin/Heidelberg, Germany, 1983; pp. 365–375. [Google Scholar]
- Balluerka, N.; Gorostiaga, A.; Alonso-Arbiol, I.; Haranburu, M. La adaptación de instrumentos de medida de unas culturas a otras: Una perspectiva práctica. Psicothema 2007, 19, 124–133. [Google Scholar]
- Albar, M.-J.; García-Ramírez, M.; López, A.M.; Garrido, R. Spanish Adaptation of the Scale of Psychological Empowerment in the Workplace. Span. J. Psychol. 2012, 15, 793–800. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef]
- Sonnentag, S.; Fritz, C. The Recovery Experience Questionnaire: Development and validation of a measure for assessing recuperation and unwinding from work. J. Occup. Health Psychol. 2007, 12, 204–221. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics for Windows; Version 26.0; IBM Corp: New York, NY, USA, 2019. [Google Scholar]
- Reinartz, W.; Haenlein, M.; Henseler, J. An empirical comparison of the efficacy of covariance-based and variance-based SEM. Int. J. Res. Mark. 2009, 26, 332–344. [Google Scholar] [CrossRef]
- Barroso, C.; Cepeda, G.; Roldán, J.L. Applying maximum likelihood and PLS on different sample sizes: Studies on SERVQUAL model and employee behaviour model. In Handbook of Partial Least Squares: Concepts, Methods and Applications; Esposito Vinzi, V., Chin, W.W., Henseler, J., Wang, H., Eds.; Springer-Verlag: Berlin/Heidelberg, Germany, 2010; pp. 427–447. [Google Scholar]
- Dijkstra, T.K.; Henseler, J. Consistent Partial Least Squares Path Modeling. Mis. Q. 2015, 39, 297–316. [Google Scholar] [CrossRef]
- Astrachan, C.B.; Patel, V.K.; Wanzenried, G. A comparative study of CB-SEM and PLS-SEM for theory development in family firm research. J. Fam. Bus. Strategy 2014, 5, 116–128. [Google Scholar] [CrossRef]
- Ringle, C.M.; Wende, S.; Becker, J.M. SmartPLS 3; SmartPLS GmbH: Boenningstedt, Germany, 2015; Available online: http://www.smartpls.com (accessed on 7 January 2021).
- Hair, J.F.; Hult, T.M.; Ringle, C.M.; Sarstedt, M.; Castillo, J.; Cepeda, G.; Roldan, J.L. Manual de Partial Least Squares Structural Equation Modeling (PLS-SEM), 2nd ed.; SAGE Publishing: Thousand Oaks, CA, USA, 2019. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cut-off criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Ringle, C.M. Advanced PLS-SEM Topics: PLS Multigroup Analysis; Working paper; University of Seville: Seville, Spain, 20 November 2016. [Google Scholar]
- Hair, J.F.; Hult, G.T.M.; Ringle, C.; Sarstedt, M. A Primer on Partial Least Squares Structural Equation Modeling (PLS-SEM); SAGE Publications, Inc.: Thousand Oaks, CA, USA, 2014. [Google Scholar]
- Hair, J.F.; Ringle, C.M.; Sarstedt, M. PLS-SEM: Indeed, a silver bullet. J. Mark. Theory Pract. 2011, 19, 139–151. [Google Scholar] [CrossRef]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Horn, J.L.; McArdle, J.J. A Practical and Theoretical Guide to Measurement Invariance in Aging Research. Exp. Aging Res. 1992, 18, 117–144. [Google Scholar] [CrossRef]
- Henseler, J.; Ringle, C.M.; Sarstedt, M. Testing measurement invariance of composites using partial least squares. Int. Mark. Rev. 2016, 33, 405–431. [Google Scholar] [CrossRef]
- Stănculescu, E. Fear of COVID-19 in Romania: Validation of the Romanian Version of the Fear of COVID-19 Scale Using Graded Response Model Analysis. Int J. Ment Health Addict. 2021, 6, 1–16. [Google Scholar] [CrossRef]
- Van den Heuvel, M.; Demerouti, E.; Peeters, M.C.W. The job crafting intervention: Effects on job resources, self-efficacy, and affective well-being. J. Occup. Organ. Psychol. 2015, 88, 511–532. [Google Scholar] [CrossRef]
- Hochwälder, J.; Brucefors, A.B. Psychological empowerment at the workplace as a predictor of ill health. Pers. Individ. Differ. 2005, 39, 1237–1248. [Google Scholar] [CrossRef]
- Pollán, M.; Pérez-Gómez, B.; Pastor-Barriuso, R.; Oteo, J.; A Hernán, M.; Pérez-Olmeda, M.; Sanmartín, J.L.; Fernández-García, A.; Cruz, I.; de Larrea, N.F.; et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet 2020, 396, 535–544. [Google Scholar] [CrossRef]
- Coelho, C.M.; Suttiwan, P.; Arato, N.; Zsido, A.N. On the Nature of Fear and Anxiety Triggered by COVID-19. Front. Psychol. 2020, 11, 3109. [Google Scholar] [CrossRef]
- Kinman, G.; Teoh, K.; Harriss, A. Supporting the well-being of healthcare workers during and after COVID-19. Occup. Med. 2020, 70, 294–296. [Google Scholar] [CrossRef]
| N | % | M | SD | |
|---|---|---|---|---|
| Age | 194 | 45.94 | 12.39 | |
| Gender | ||||
| Female | 162 | 83.5 | ||
| Male | 32 | 16.5 | ||
| Professional category | ||||
| TCAE (nursing assistant) | 24 | 12.4 | ||
| Nurse/Specialist Nurse | 98 | 50.5 | ||
| Specialist graduate | 51 | 26.3 | ||
| Administration | 6 | 3.1 | ||
| Physiotherapy | 7 | 3.6 | ||
| Social work | 3 | 1.5 | ||
| Higher technician | 5 | 2.6 | ||
| Organizational rank | ||||
| Intermediate or higher posts | 46 | 23.7 | ||
| Workers without people in their care | 148 | 76.3 | ||
| Job tenure in the current contract | 12.20 | 12.97 | ||
| Changing tasks or activities during the pandemic: | ||||
| Changes | 89 | 45.9 | ||
| No changes | 105 | 54.1 | ||
| COVID-19 diagnosis | ||||
| Yes | 55 | 28.4 | ||
| No | 139 | 71.6 | ||
| Type of contract | ||||
| Permanent | 101 | 52.1 | ||
| Temporary | 93 | 47.9 | ||
| Workplace during the pandemic | ||||
| COVID Floor or Team | 83 | 42.8 | ||
| Non-COVID Service | 46 | 23.7 | ||
| Health Center | 57 | 29.4 | ||
| Telework/union release/administration | 8 | 4.1 |
| Variables | M | SD | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|---|
| Collaborative Crafting | 3.63 | 0.97 | - | |||
| Psychological Empowerment | 3.90 | 0.70 | 0.48 ** | - | ||
| Fear of COVID-19 | 2.38 | 0.90 | −0.12 | −0.16 * | - | |
| Emotional disorders | 2.36 | 0.83 | −0.17 * | −0.26 ** | 0.77 ** | - |
| Psychological Detachment | 2.92 | 1.20 | 0.16 * | 0.20 ** | −0.43 ** | −0.59 ** |
| Latent Variable | Item | λ | CR | α | Rho_A | AVE |
|---|---|---|---|---|---|---|
| Collaborative Crafting | CC1 | 0.71 | 0.91 | 0.91 | 0.91 | 0.66 |
| CC2 | 0.84 | |||||
| CC3 | 0.68 | |||||
| CC4 | 0.86 | |||||
| CC5 | 0.94 | |||||
| Psychological empowerment | PE3 | 0.51 | 0.84 | 0.84 | 0.85 | 0.44 |
| PE4 | 0.56 | |||||
| PE6 | 0.56 | |||||
| PE8 | 0.71 | |||||
| PE9 | 0.70 | |||||
| PE11 | 0.73 | |||||
| PE12 | 0.77 | |||||
| Fear of COVID-19 | F1 | 0.67 | 0.89 | 0.90 | 0.90 | 0.55 |
| F2 | 0.58 | |||||
| F3 | 0.66 | |||||
| F4 | 0.67 | |||||
| F5 | 0.89 | |||||
| F6 | 0.88 | |||||
| F7 | 0.81 | |||||
| Psychological detachment | PD1 | 0.98 | 0.95 | 0.95 | 0.95 | 0.86 |
| PD2 | 0.91 | |||||
| PD3 | 0.88 | |||||
| Emotional disorders | ED1 | 0.81 | 0.92 | 0.92 | 0.92 | 0.50 |
| ED2 | 0.84 | |||||
| ED3 | 0.74 | |||||
| ED5 | 0.77 | |||||
| ED6 | 0.71 | |||||
| ED7 | 0.82 | |||||
| ED8 | 0.62 | |||||
| ED9 | 0.63 | |||||
| ED10 | 0.67 | |||||
| ED12 | 0.63 | |||||
| ED13 | 0.57 | |||||
| ED14 | 0.60 |
| Beta Coefficients | t Statistics | p Value | |
|---|---|---|---|
| Crafting -> Detachment | 0.091 | 2.228 | 0.026 |
| Crafting -> Emocional Disorders | −0.064 | 2.132 | 0.033 |
| Crafting -> Empowerment | 0.513 | 7.863 | 0.001 |
| Emocional Disorders -> Detachment | −0.822 | 3.975 | 0.001 |
| Empowerment -> Detachment | 0.177 | 2.404 | 0.016 |
| Empowerment -> Emocional Disorders | −0.125 | 2.297 | 0.023 |
| Fear -> Detachment | −0.468 | 8.114 | 0.001 |
| Fear -> Emocional Disorders | 0.866 | 27.97 | 0.001 |
| Fear -> Empowerment | −0.152 | 1.912 | 0.056 |
| Original Correlation | Correlation of Permutation Means | 5.0% | p-Values of the Permutation | |
|---|---|---|---|---|
| Collaborative Crafting | 0.999 | 0.998 | 0.995 | 0.50 |
| Psychological Detachment | 1.000 | 1.000 | 1.000 | 0.95 |
| Emotional Disorders | 0.999 | 0.999 | 0.997 | 0.25 |
| Psychological Empowerment | 0.983 | 0.986 | 0.958 | 0.27 |
| Fear of COVID-19 | 0.999 | 0.999 | 0.997 | 0.31 |
| Mean-Original Differences (Mean-Difference of Permutation Means) | 2.5% | 97.5% | p-Values of the Permutation | Variance-Original Difference (Variance-Difference of Permutation Means) | 2.5% | 97.5% | p-Values of the Permutation | |
|---|---|---|---|---|---|---|---|---|
| Psychological Empowerment | 0.18 (0.002) | −0.28 | 0.28 | 0.19 | −0.18 (−0.004) | −0.42 | 0.43 | 0.40 |
| Collaborative Crafting | 0.18 (0.002) | −0.27 | 0.27 | 0.21 | −0.10 (−0.004) | −0.36 | 0.36 | 0.61 |
| Emotional Disorders | 0.008 (−0.002) | −0.28 | 0.27 | 0.95 | −0.07 (−0.004) | −0.34 | 0.32 | 0.67 |
| Fear of COVID-19 | −0.07 (−0.001) | −0.29 | 0.28 | 0.58 | −0.07 (−0.001) | −0.42 | 0.39 | 0.72 |
| Psychological Detachment | −0.18 (0.002) | −0.29 | 0.28 | 0.21 | −0.02 (−0.002) | −0.27 | 0.27 | 0.88 |
| Path Coefficients | Original 1-Tail p-Value | New p-Value | |
|---|---|---|---|
| Crafting and Empowerment | −0.06 | 0.71 | 0.57 |
| Emotional Disorders and Detachment | −0.16 | 0.78 | 0.42 |
| Empowerment and Detachment | −0.18 | 0.94 | 0.12 |
| Empowerment and Emotional Disorders | 0.08 | 0.18 | 0.37 |
| Fear and Detachment | 0.33 | 0.05 | 0.11 |
| Fear and Emotional Disorders | 0.06 | 0.15 | 0.30 |
| Fear and Empowerment | −0.04 | 0.61 | 0.77 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llorente-Alonso, M.; García-Ael, C.; Topa, G.; Sanz-Muñoz, M.L.; Muñoz-Alcalde, I.; Cortés-Abejer, B. Can Psychological Empowerment Prevent Emotional Disorders in Presence of Fear of COVID-19 in Health Workers? A Cross-Sectional Validation Study. J. Clin. Med. 2021, 10, 1614. https://doi.org/10.3390/jcm10081614
Llorente-Alonso M, García-Ael C, Topa G, Sanz-Muñoz ML, Muñoz-Alcalde I, Cortés-Abejer B. Can Psychological Empowerment Prevent Emotional Disorders in Presence of Fear of COVID-19 in Health Workers? A Cross-Sectional Validation Study. Journal of Clinical Medicine. 2021; 10(8):1614. https://doi.org/10.3390/jcm10081614
Chicago/Turabian StyleLlorente-Alonso, Marta, Cristina García-Ael, Gabriela Topa, María Luisa Sanz-Muñoz, Irene Muñoz-Alcalde, and Beatriz Cortés-Abejer. 2021. "Can Psychological Empowerment Prevent Emotional Disorders in Presence of Fear of COVID-19 in Health Workers? A Cross-Sectional Validation Study" Journal of Clinical Medicine 10, no. 8: 1614. https://doi.org/10.3390/jcm10081614
APA StyleLlorente-Alonso, M., García-Ael, C., Topa, G., Sanz-Muñoz, M. L., Muñoz-Alcalde, I., & Cortés-Abejer, B. (2021). Can Psychological Empowerment Prevent Emotional Disorders in Presence of Fear of COVID-19 in Health Workers? A Cross-Sectional Validation Study. Journal of Clinical Medicine, 10(8), 1614. https://doi.org/10.3390/jcm10081614








