Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures
Abstract
:1. Introduction
2. Materials and Methods
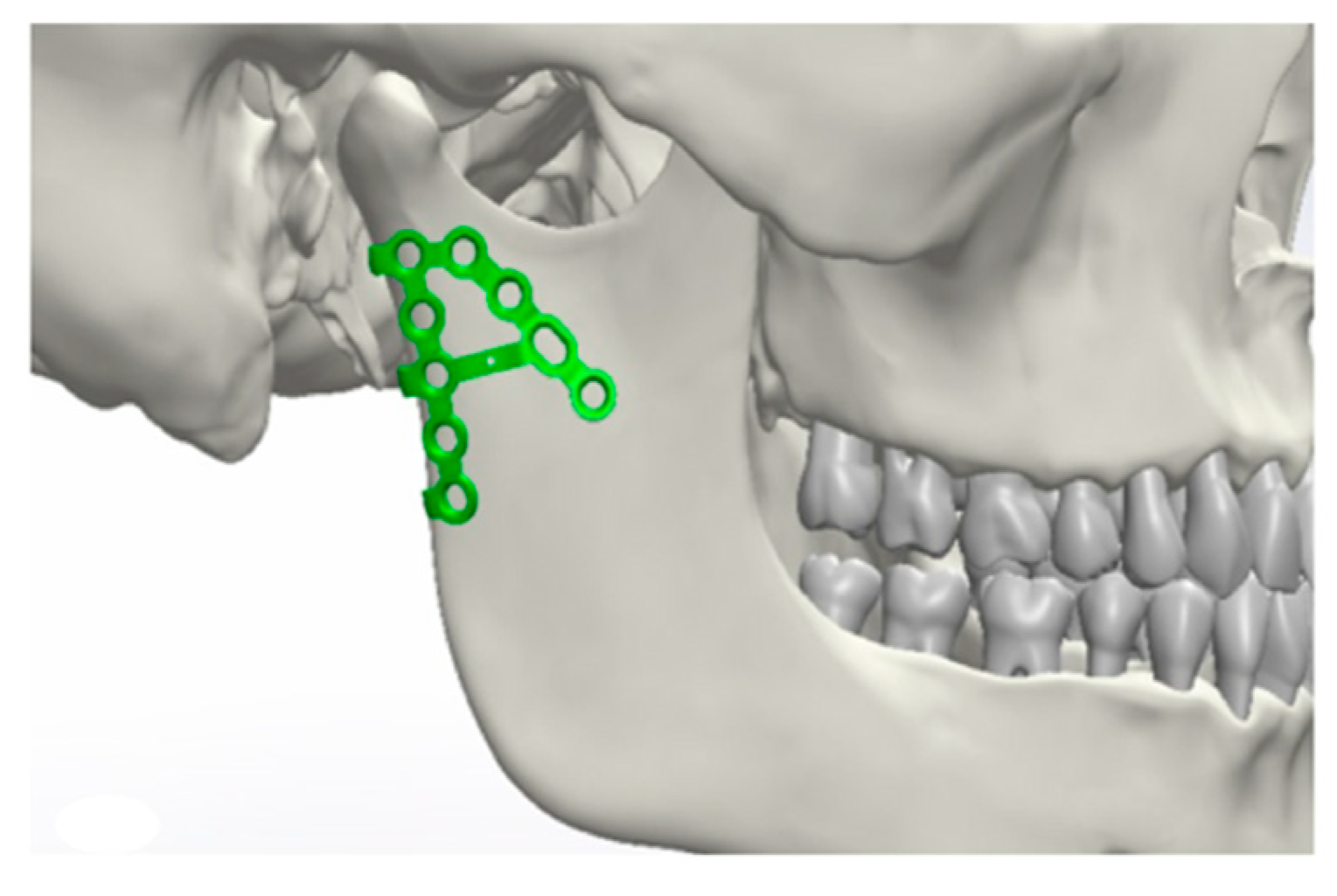
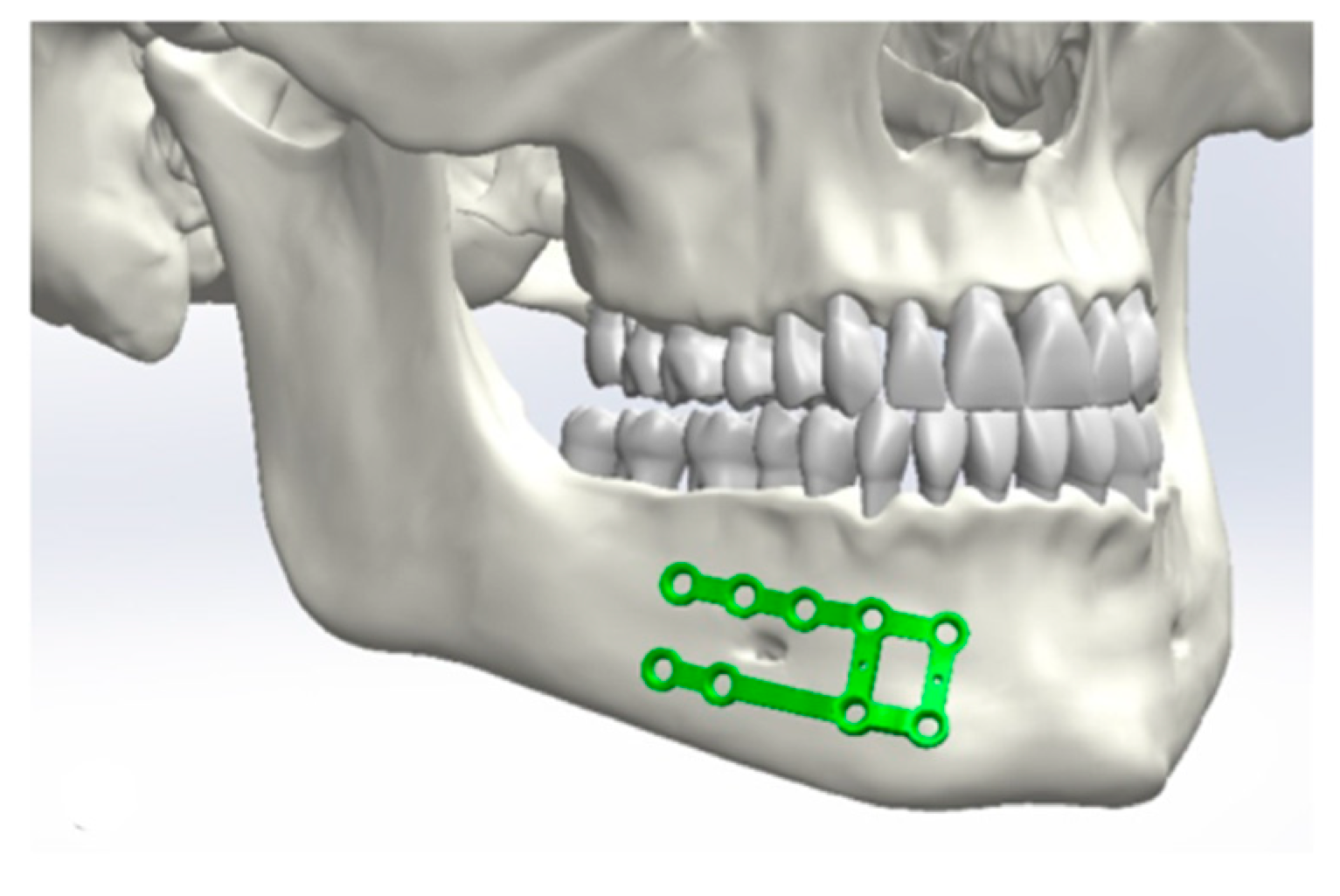
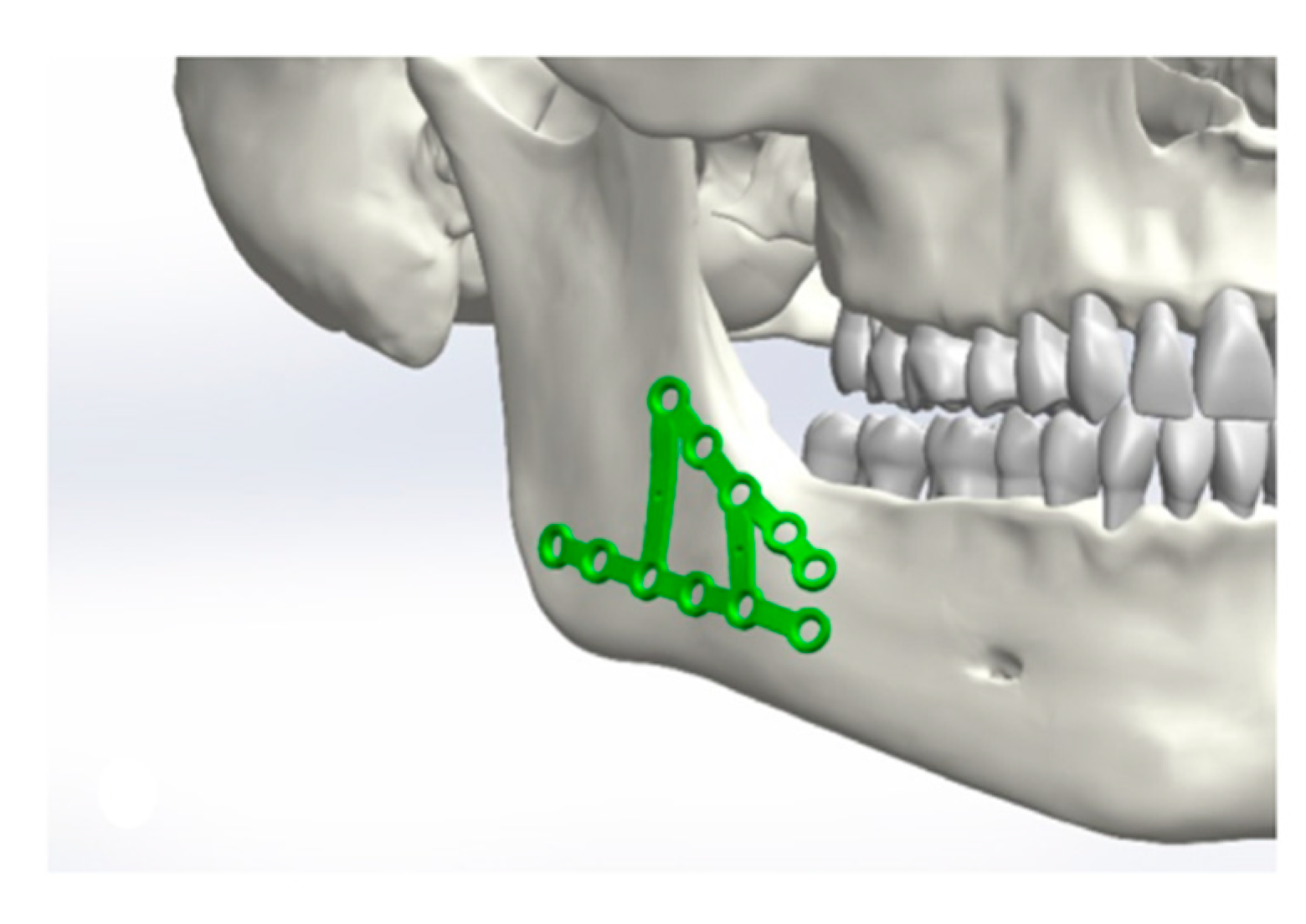
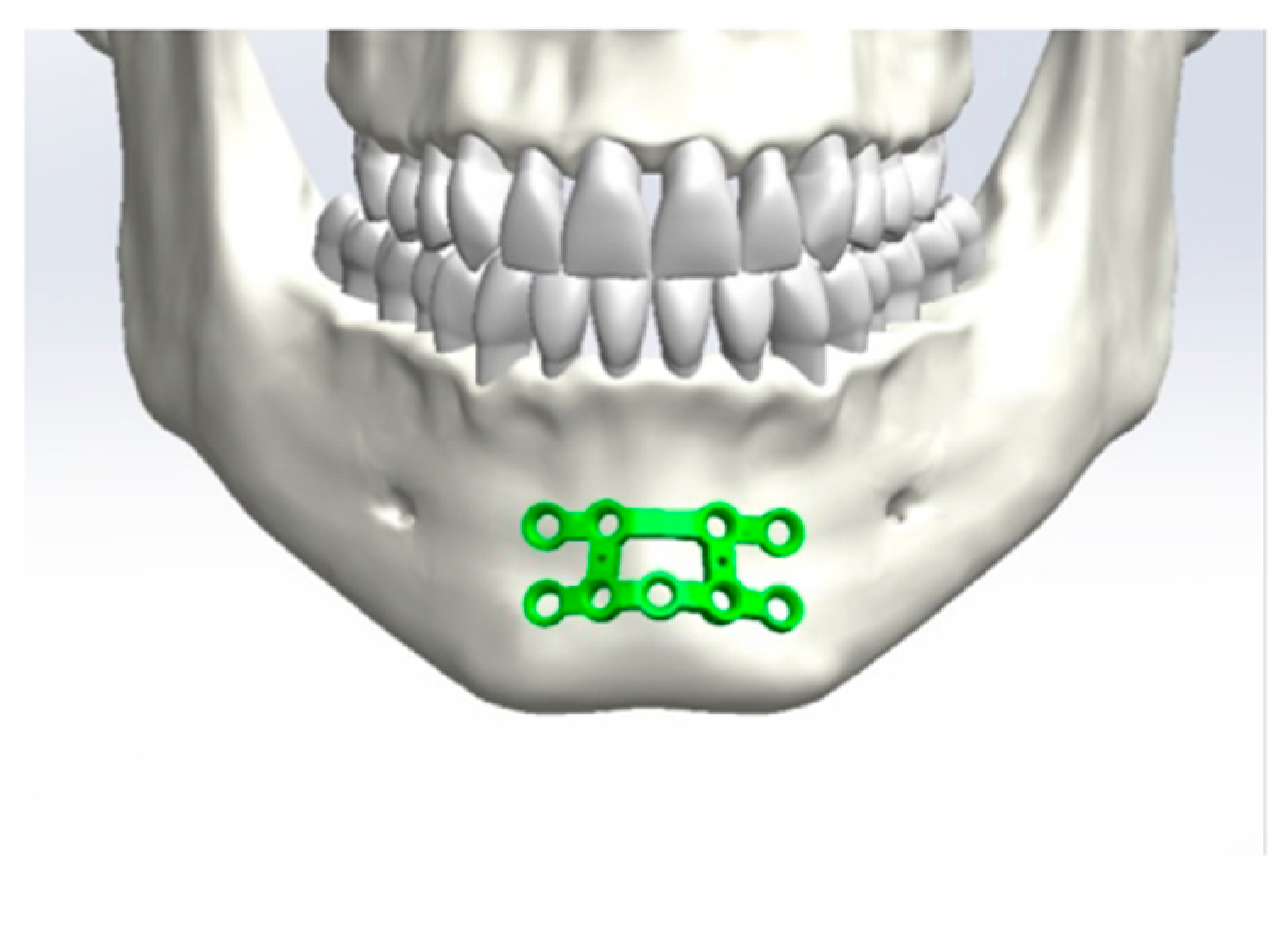
2.1. Design of the Plates
2.2. Analysis of the Accuracy of the Plate
3. Results
Application of the Plates
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adi, M.; Ogden, G.R.; Chisholm, D.M. An analysis of mandibular fractures in Dundee, Scotland (1977 to 1985). Br. J. Oral Maxillofac. Surg. 1990, 28, 194–199. [Google Scholar] [CrossRef]
- Boffano, P.; Kommers, S.C.; Karagozoglu, K.H.; Forouzanfar, T. Aetiology of maxillofacial fractures: A review of published studies during the last 30 years. Br. J. Oral Maxillofac. Surg. 2014, 52, 901–906. [Google Scholar] [CrossRef]
- Bormann, K.-H.; Wild, S.; Gellrich, N.-C.; Kokemüller, H.; Stühmer, C.; Schmelzeisen, R.; Schön, R. Five-year retrospective study of mandibular fractures in Freiburg, Germany: Incidence, etiology, treatment, and complications. J. Oral Maxillofac. Surg. 2009, 67, 1251–1255. [Google Scholar] [CrossRef]
- Chrcanovic, B.R.; Abreu, M.H.N.G.; Freire-Maia, B.; Souza, L.N. 1,454 mandibular fractures: A 3-year study in a hospital in Belo Horizonte, Brazil. J. Cranio-Maxillofac. Surg. 2012, 40, 116–123. [Google Scholar] [CrossRef]
- Bak, M.J.; Doerr, T.D. Craniomaxillofacial fractures during recreational baseball and softball. J. Oral Maxillofac. Surg. 2004, 62, 1209–1212. [Google Scholar] [CrossRef]
- Afrooz, P.N.; Bykowski, M.R.; James, I.B.; Daniali, L.N.; Clavijo-Alvarez, J.A. The Epidemiology of Mandibular Fractures in the United States, Part 1: A Review of 13,142 Cases from the US National Trauma Data Bank. J. Oral Maxillofac. Surg. 2015, 73, 2361–2366. [Google Scholar] [CrossRef]
- Al-Khateeb, T.; Abdullah, F.M. Craniomaxillofacial Injuries in the United Arab Emirates: A Retrospective Study. J. Oral Maxillofac. Surg. 2007, 65, 1094–1101. [Google Scholar] [CrossRef]
- Hlawitschka, M.; Eckelt, U. Clinical, radiological and axiographic examination after conservative functional treatment of intracapsular temporomandibular joint fractures. Mund Kiefer Gesichtschir. 2002, 6, 241–248. [Google Scholar] [CrossRef]
- Zachariades, N.; Mezitis, M.; Mourouzis, C.; Papadakis, D.; Spanou, A. Fractures of the mandibular condyle: A review of 466 cases. Literature review, reflections on treatment and proposals. J. Cranio-Maxillofac. Surg. 2006, 34, 421–432. [Google Scholar] [CrossRef]
- Chrcanovic, B.R. Open versus closed reduction: Diacapitular fractures of the mandibular condyle. Oral Maxillofac. Surg. 2012, 16, 257–265. [Google Scholar] [CrossRef]
- Neff, A.; Kolk, A.; Meschke, F.; Deppe, H.; Horch, H.-H. Small fragment screws vs. plate osteosynthesis in condylar head fractures. Mund Kiefer Gesichtschir. 2005, 9, 80–88. [Google Scholar] [CrossRef]
- Koulocheris, P.; Sakkas, N.; Otten, J.-E. Maxillomandibular fixation with Otten mini-hooks. Br. J. Oral Maxillofac. Surg. 2007, 45, 679–680. [Google Scholar] [CrossRef]
- Ellis, E.; Miles, B.A. Fractures of the mandible: A technical perspective. Plast. Reconstr. Surg. 2007, 120, 76S–89S. [Google Scholar] [CrossRef]
- Sauerbier, S.; Schön, R.; Otten, J.-E.; Schmelzeisen, R.; Gutwald, R. The development of plate osteosynthesis for the treatment of fractures of the mandibular body—A literature review. J. Cranio-Maxillofac. Surg. 2008, 36, 251–259. [Google Scholar] [CrossRef]
- Bhatnagar, A.; Bansal, V.; Kumar, S.; Mowar, A. Comparative analysis of osteosynthesis of mandibular anterior fractures following open reduction using “stainless steel lag screws and mini plates”. J. Maxillofac. Oral Surg. 2013, 12, 133–139. [Google Scholar] [CrossRef] [Green Version]
- De Oliveira, J.C.S.; Moura, L.B.; de Menezes, J.D.S.; Gabrielli, M.A.C.; Pereira Filho, V.A.; Hochuli-Vieira, E. Three-dimensional strut plate for the treatment of mandibular fractures: A systematic review. Int. J. Oral Maxillofac. Surg. 2018, 47, 330–338. [Google Scholar] [CrossRef] [Green Version]
- Metzger, M.C.; Schön, R.; Schulze, D.; Carvalho, C.; Gutwald, R.; Schmelzeisen, R. Individual preformed titanium meshes for orbital fractures. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2006, 102, 442–447. [Google Scholar] [CrossRef]
- Metzger, M.C.; Vogel, M.; Hohlweg-Majert, B.; Mast, H.; Fan, X.; Rudell, A.; Schlager, S. Anatomical shape analysis of the mandible in Caucasian and Chinese for the production of preformed mandible reconstruction plates. J. Cranio-Maxillofac. Surg. 2011, 39, 393–400. [Google Scholar] [CrossRef]
- Probst, F.A.; Mast, G.; Ermer, M.; Gutwald, R.; Schmelzeisen, R.; Pautke, C.; Otto, S.; Schiel, S.; Ehrenfeld, M.; Cornelius, C.-P.; et al. MatrixMANDIBLE preformed reconstruction plates—A two-year two-institution experience in 71 patients. J. Oral Maxillofac. Surg. 2012, 70, e657–e666. [Google Scholar] [CrossRef]
- Schiel, S.; Otto, S.; Pautke, C.; Cornelius, C.-P.; Probst, F.A. Simplified transoral load-bearing osteosynthesis with preformed mandible reconstruction plates. Craniomaxillofac. Trauma Reconstr. 2013, 6, 211–214. [Google Scholar] [CrossRef] [Green Version]
- Strong, E.B.; Fuller, S.C.; Wiley, D.F.; Zumbansen, J.; Wilson, M.D.; Metzger, M.C. Preformed vs Intraoperative Bending of Titanium Mesh for Orbital Reconstruction. Otolaryngol. Neck Surg. 2013, 149, 60–66. [Google Scholar] [CrossRef] [PubMed]
- 3D Printed Simulation Models Based on Real Patient Situations for Hands-On Practice-Kröger-2017-European Journal of Dental Education-Wiley Online Library. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/eje.12229 (accessed on 17 October 2021).
- De Medeiros, R.C.; Sigua, E.A.; Navarro, P.; Olate, S.; Albergaria Barbosa, J.R. In Vitro Mechanical Analysis of Different Techniques of Internal Fixation of Combined Mandibular Angle and Body Fractures. J. Oral Maxillofac. Surg. 2016, 74, 778–785. [Google Scholar] [CrossRef]
- De Medeiros, R.C.; de Moura, A.L.; Sawazaki, R.; Fernandes Moreira, R.W. Comparative in vitro mechanical evaluation of techniques using a 2.0 mm locking fixation system for simulated fractures of the mandibular body. J. Cranio-Maxillofac. Surg. 2015, 43, 302–305. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Cheng, K.-J.; Liu, Y.-F.; Fan, Y.-Y.; Wang, J.H.; Wang, R.; Baur, D.A.; Jiang, X.-F.; Dong, X.-T. Experimental validation of finite element simulation of a new custom-designed fixation plate to treat mandibular angle fracture. Biomed. Eng. Online 2021, 20, 15. [Google Scholar] [CrossRef] [PubMed]
- Schlager, S.; Rüdell, A. Sexual Dimorphism and population affinity in the human zygomatic structure—Comparing surface to outline data. Anat. Rec. 2017, 300, 226–237. [Google Scholar] [CrossRef] [Green Version]
- R Foundation for Statistical Computing. A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2008. [Google Scholar]
- Schlager, S. Morpho and Rvcg—Shape Analysis in R: R-Packages for Geometric Morphometrics, Shape Analysis and Surface Manipulations. In Statistical Shape and Deformation Analysis; Zheng, G., Li, S., Székely, G., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 217–256. ISBN 978-0-12-810493-4. Available online: http://www.sciencedirect.com/science/article/pii/B9780128104934000110 (accessed on 4 October 2019).
- Schlager, S. RvtkStatismo: Integrating Statismo and R Using the Vtkstandardmeshrepresenter. 2015. Available online: https://www.researchgate.net/publication/331926435_RvtkStatismo_Integrating_statismo_and_R_using_the_vtkStandardMeshRepresenter (accessed on 21 October 2021).
- Goodall, C. Procrustes methods in the statistical analysis of shape. J. R. Stat. Soc. Ser. B Methodol. 1991, 53, 285–321. [Google Scholar] [CrossRef]
- Ostas, D.; Hedesiu, M.; Roman, C.R.; Cosma, C.; Ciurea, M.; Rotaru, H. Design Workflow for Mandibular Reconstruction. Opportunities and Limitations of In-house Virtual Surgical Planning. J. Med. Biol. Eng. 2021, 41, 482–493. [Google Scholar] [CrossRef]
- Acock, A.C. Discovering Structural Equation Modeling Using Stata; Stata Press Books; StataCorp LP: College Station, TX, USA, 2013; Available online: https://ideas.repec.org/b/tsj/spbook/dsemus.html (accessed on 21 October 2021).
- Ahmad, M.; Nanda, R.; Bajwa, A.S.; Candal-Couto, J.; Green, S.; Hui, A.C. Biomechanical testing of the locking compression plate: When does the distance between bone and implant significantly reduce construct stability? Injury 2007, 38, 358–364. [Google Scholar] [CrossRef]
- Chole, R.H.; Patil, R.N.; Balsaraf Chole, S.; Gondivkar, S.; Gadbail, A.R.; Yuwanati, M.B. Association of mandible anatomy with age, gender, and dental status: A radiographic study. Int. Sch. Res. Not. 2013, 2013, 453763. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tkany, L.; Hofstätter, B.; Petersik, A.; Miehling, J.; Wartzack, S.; Sesselmann, S. New Design Process for Anatomically Enhanced Osteosynthesis Plates. J. Orthop. Res. 2019, 37, 1508–1517. [Google Scholar] [CrossRef]
- Schmutz, B.; Wullschleger, M.E.; Kim, H.; Noser, H.; Schütz, M.A. Fit Assessment of Anatomic Plates for the Distal Medial Tibia. J. Orthop. Trauma 2008, 22, 258–263. [Google Scholar] [CrossRef] [Green Version]
- Schmutz, B.; Rathnayaka, K.; Albrecht, T. Anatomical fitting of a plate shape directly derived from a 3D statistical bone model of the tibia. J. Clin. Orthop. Trauma 2019, 10, S236–S241. [Google Scholar] [CrossRef]
- Ponvel, K.; Panneerselvam, E.; Balasubramanian, S.; Krishna Kumar Raja, V.B. Evaluation of labial versus labio-inferior lines of osteosynthesis using 3D miniplate for fractures of anterior mandible: A finite element analysis with a pilot clinical trial. Chin. J. Traumatol. Zhonghua Chuang Shang Za Zhi 2019, 22, 261–269. [Google Scholar] [CrossRef] [PubMed]
- Duttenhoefer, F.; Probst, F.A.; Vach, K.; Cornelius, C.-P.; Zens, M.; Schmelzeisen, R.; Metzger, M.C. Clinical analysis of MatrixMANDIBLE Preformed Reconstruction Plate design. J. Cranio-Maxillofac. Surg. 2017, 45, 1521–1525. [Google Scholar] [CrossRef]
- Liu, Y.-F.; Fan, Y.-Y.; Jiang, X.-F.; Baur, D.A. A customized fixation plate with novel structure designed by topological optimization for mandibular angle fracture based on finite element analysis. Biomed. Eng. Online 2017, 16, 131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Huang, J.I.; Toogood, P.; Chen, M.R.; Wilber, J.H.; Cooperman, D.R. Clavicular anatomy and the applicability of precontoured plates. J. Bone Joint Surg. Am. 2007, 89, 2260–2265. [Google Scholar] [CrossRef]
- Datarkar, A.; Tayal, S.; Thote, A.; Galie, M. An in-vitro evaluation of a novel design of miniplate for fixation of fracture segments in the transition zone of parasymphysis-body region of mandible using finite element analysis. J. Cranio-Maxillofac. Surg. 2019, 47, 99–105. [Google Scholar] [CrossRef] [PubMed]
- Champy, M.; Loddé, J.P.; Schmitt, R.; Jaeger, J.H.; Muster, D. Mandibular osteosynthesis by miniature screwed plates via a buccal approach. J. Maxillofac. Surg. 1978, 6, 14–21. [Google Scholar] [CrossRef]
- Ronga, M.; Shanmugam, C.; Longo, U.G.; Oliva, F.; Maffulli, N. Minimally Invasive Osteosynthesis of Distal Tibial Fractures Using Locking Plates. Orthop. Clin. N. Am. 2009, 40, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Schütz, M.; Südkamp, N.P. Revolution in plate osteosynthesis: New internal fixator systems. J. Orthop. Sci. 2003, 8, 252–258. [Google Scholar] [CrossRef]
- Gottsauner, M.; Reichert, T.; Koerdt, S.; Wieser, S.; Klingelhoeffer, C.; Kirschneck, C.; Hoffmann, J.; Ettl, T.; Ristow, O. Comparison of additive manufactured models of the mandible in accuracy and quality using six different 3D printing systems. J. Cranio-Maxillofac. Surg. 2021, 49, 855–866. [Google Scholar] [CrossRef] [PubMed]
- Poxleitner, P.; Steybe, D.; Bublitz, B.; Schlager, S.; Fuessinger, M.A.; Voss, P.J.; Schmelzeisen, R.; Cornelius, C.-P.; Metzger, M. Analysis of the accuracy of a novel preformed osteosynthesis plate for the reduction and fixation of zygomaticomaxillary complex fractures. J. Cranio-Maxillofac. Surg. 2019, 47, 951–958. [Google Scholar] [CrossRef] [PubMed]
- Voss, J.O.; Varjas, V.; Raguse, J.D.; Thieme, N.; Richards, R.G.; Kamer, L. Computed tomography-based virtual fracture reduction techniques in bimandibular fractures. J. Cranio-Maxillofac. Surg. 2016, 44, 177–185. [Google Scholar] [CrossRef]


| Size L | Size M | Size S | Total | |
|---|---|---|---|---|
| Condyle plate | 74 | 85 | 75 | 78 |
| Body plate | 65 | 68 | 80 | 71 |
| Ramus plate | 47 | 60 | 53 | 53 |
| Symphysis plate | 84 | 90 | - | 87 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fuessinger, M.A.; Gass, M.; Woelm, C.; Cornelius, C.-P.; Zimmerer, R.M.; Poxleitner, P.; Schlager, S.; Metzger, M.C. Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures. J. Clin. Med. 2021, 10, 5975. https://doi.org/10.3390/jcm10245975
Fuessinger MA, Gass M, Woelm C, Cornelius C-P, Zimmerer RM, Poxleitner P, Schlager S, Metzger MC. Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures. Journal of Clinical Medicine. 2021; 10(24):5975. https://doi.org/10.3390/jcm10245975
Chicago/Turabian StyleFuessinger, Marc Anton, Mathieu Gass, Caroline Woelm, Carl-Peter Cornelius, Ruediger M. Zimmerer, Philipp Poxleitner, Stefan Schlager, and Marc Christian Metzger. 2021. "Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures" Journal of Clinical Medicine 10, no. 24: 5975. https://doi.org/10.3390/jcm10245975
APA StyleFuessinger, M. A., Gass, M., Woelm, C., Cornelius, C.-P., Zimmerer, R. M., Poxleitner, P., Schlager, S., & Metzger, M. C. (2021). Analyzing the Fitting of Novel Preformed Osteosynthesis Plates for the Reduction and Fixation of Mandibular Fractures. Journal of Clinical Medicine, 10(24), 5975. https://doi.org/10.3390/jcm10245975






