How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Data Collection
2.3. Statistical Analysis
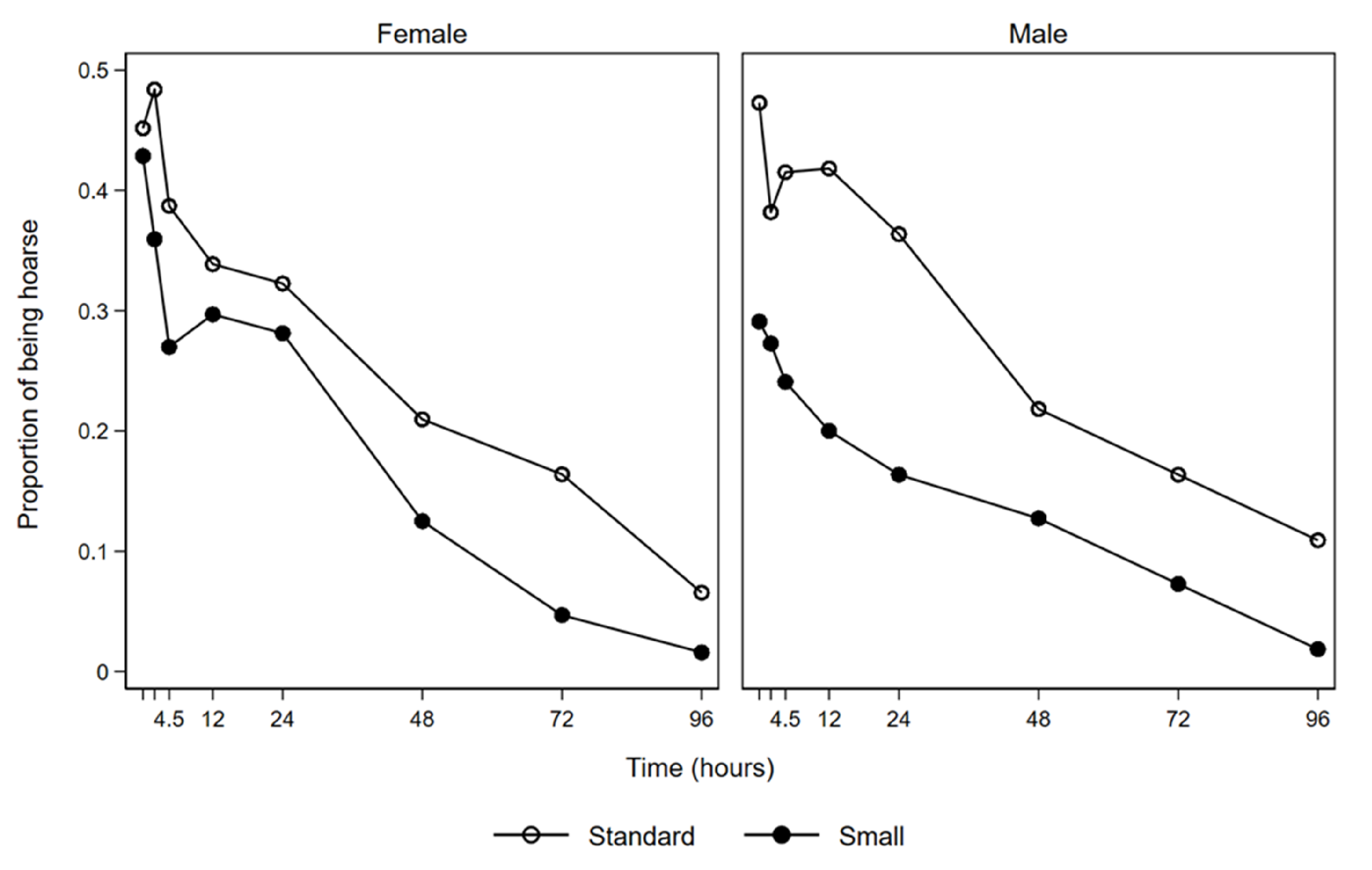
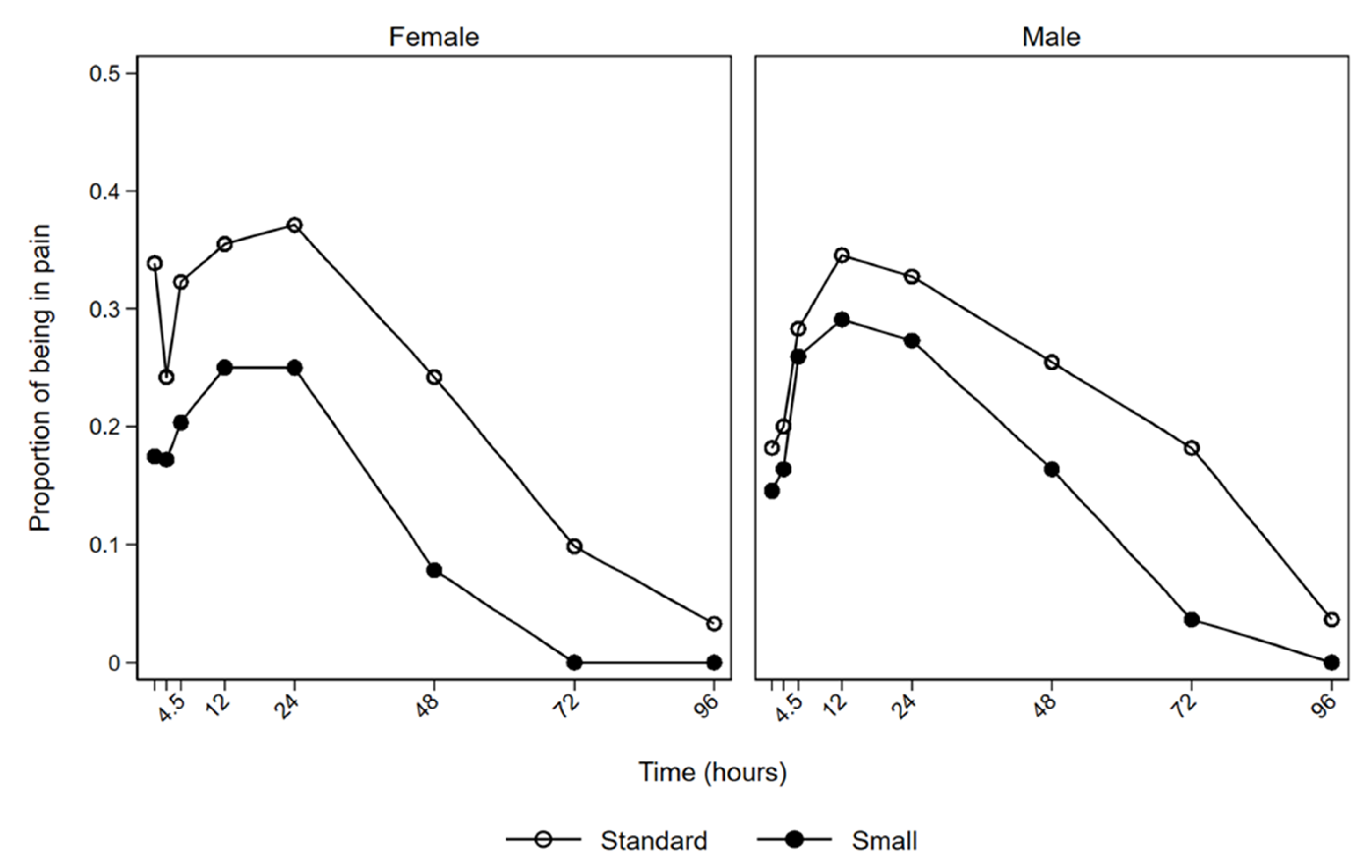
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jaensson, M.; Olowsson, L.L.; Nilsson, U. Endotracheal tube size and sore throat following surgery: A randomized-controlled study. Acta Anaesthesiol. Scand. 2010, 54, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Biro, P.; Seifert, B.; Pasch, T. Complaints of sore throat after tracheal intubation: A prospective evaluation. Eur. J. Anaesthesiol. 2005, 22, 307–311. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El-Boghdadly, K.; Bailey, C.R.; Wiles, M.D. Postoperative sore throat: A systematic review. Anaesthesia 2016, 71, 706–717. [Google Scholar] [CrossRef] [PubMed]
- Jaensson, M.; Gupta, A.; Nilsson, U.G. Risk factors for development of postoperative sore throat and hoarseness after endotracheal intubation in women: A secondary analysis. AANA J. 2012, 80, S67–S73. [Google Scholar] [PubMed]
- Hu, B.; Bao, R.; Wang, X.; Liu, S.; Tao, T.; Xie, Q.; Yu, X.; Li, J.; Bo, L.; Deng, X. The size of endotracheal tube and sore throat after surgery: A systematic review and meta-analysis. PLoS ONE 2013, 8, e74467. [Google Scholar] [CrossRef] [PubMed]
- Farrow, S.; Farrow, C.; Soni, N. Size matters: Choosing the right tracheal tube. Anaesthesia 2012, 67, 815–819. [Google Scholar] [CrossRef] [PubMed]
- Ganason, N.; Sivanaser, V.; Liu, C.Y.; Maaya, M.; Ooi, J.S.M. Post-operative Sore Throat: Comparing the Monitored Endotracheal Tube Cuff Pressure and Pilot Balloon Palpation Methods. Malays. J. Med. Sci. 2019, 26, 132–138. [Google Scholar] [CrossRef] [PubMed]
- Stout, D.M.; Bishop, M.J.; Dwersteg, J.F.; Cullen, B.F. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology 1987, 67, 419–421. [Google Scholar] [CrossRef] [PubMed]
- Jaensson, M.; Gupta, A.; Nilsson, U.G. Gender differences in risk factors for airway symptoms following tracheal intubation. Acta Anaesthesiol. Scand. 2012, 56, 1306–1313. [Google Scholar] [CrossRef] [PubMed]
- Ünsal, Ö.; Seyhun, N.; Türk, B.; Ekici, M.; Dobrucalı, H.; Turgut, S. The Evaluation of Upper Airway Complications Secondary to Intubation: Cuff Pressure Manometer Versus Conventional Palpation Method. Med. Bull. Sisli Etfal Hosp. 2018, 52, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Karmali, S.; Rose, P. Tracheal tube size in adults undergoing elective surgery—A narrative review. Anaesthesia 2020, 75, 1529–1539. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, C.; Artime, C. Airway management in the adult. In Miller’s Anesthesia; Elsevier: New York, NY, USA, 2014; pp. 1647–1683. [Google Scholar]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Independent Variables | Intraoperative Variables | ||
|---|---|---|---|
| Gender | Male/female | CUFF pressure 1 | cm H2O |
| Age | Years | CUFF pressure 2 | cm H2O |
| Length | Cm | Cough during intubation | Yes/no |
| Weight | Kg | Use of stilet | Yes/no |
| Smoker | Yes/no | Use of ventricular probe | Yes/no |
| ASA Score | Grade 1–2 | Visible blood trail at the tube at extubation | Yes/no |
| SARI Score | Grade 0–4 | Experience of the anaesthetic staff | Years |
| Duration of the anaesthesia | Minutes | ||
| PONV prophylaxes with dexamethasone 4 mg iv | Yes/no | ||
| PONV prophylaxes with ondansetron 4 mg iv | Yes/no | ||
| Total N = 236 | Female N = 126 | Male N = 110 | |||||
|---|---|---|---|---|---|---|---|
| Size 7.0 n = 62 | Size 6.0 n = 64 | p-Value | Size 8.0 n = 55 | Size 7.0 n = 55 | p-Value | ||
| Gender (Female) | 126 (53.4) | ||||||
| Age (years) | 50.9 (14.0) | 44.8 (12.4) | 47.0 (12.4) | 0.33 | 55.5 (12.7) | 57.6 (14.4) | 0.41 |
| BMI (kg/m2) | 27.1 (4.3) | 27.6 (4.9) | 26.8 (5.2) | 0.37 | 27.4 (3.5) | 26.6 (3.3) | 0.21 |
| Smoker (yes) | 172 (73.2) | 40 (65.6) | 50 (78.1) | 0.12 | 43 (78.2) | 39 (70.9) | 0.38 |
| ASA score | |||||||
| 1 | 105 (44.5) | 34 (54.8) | 33 (51.6) | 18 (32.7) | 20 (36.4) | ||
| 2 | 131 (55.5) | 28 (45.2) | 31 (48.4) | 0.71 | 37 (67.3) | 35 (63.6) | 0.69 |
| SARI score | |||||||
| 0 | 156 (66.4) | 40 (64.5) | 47 (73.4) | 34 (61.8) | 35 (64.8) | ||
| 1 | 22 (9.4) | 5 (8.1) | 3 (4.7) | 7 (12.7) | 7 (13.0) | ||
| 2 | 35 (14.9) | 10 (16.1) | 9 (14.1) | 7 (12.7) | 9 (16.7) | ||
| 3 | 13 (5.5) | 2 (3.2) | 4 (6.3) | 5 (9.1) | 2 (3.7) | ||
| 4 | 9 (3.8) | 5 (8.1) | 1 (1.6) | 0.35 | 2 (3.6) | 1 (1.9) | 0.76 |
| CUFF pressure 1 | 25.1 (11.2) | 27.0 (11.9) | 25.6 (9.8) | 0.48 | 23.6 (11.9) | 23.7 (10.9) | 0.96 |
| CUFF pressure 2 | 22.8 (9.1) | 23.9 (7.7) | 23.6 (8.1) | 0.81 | 21.8 (10.1) | 21.8 (10.8) | 0.99 |
| Cough during intubation (yes) | 34 (14.5) | 9 (14.5) | 8 (12.5) | 0.74 | 9 (16.4) | 8 (14.8) | 0.82 |
| Use of stilet (yes) | 62 (26.3) | 15 (24.2) | 16 (25.0) | 0.92 | 18 (32.7) | 13 (23.6) | 0.29 |
| Use of ventricular probe (yes) | 121 (52.2) | 45 (72.6) | 41 (65.1) | 0.37 | 17 (32.1) | 18 (33.3) | 0.89 |
| Visible blood trail at the tube at extubation (yes) | 16 (7.0) | 5 (8.1) | 4 (6.6) | 0.75 | 3 (5.7) | 4 (7.4) | 0.71 |
| Experience of the anaesthetic staff (years) | 13.7 (10.2) | 12.2 (9.9) | 13.1 (10.1) | 0.60 | 16.7 (10.6) | 13.3 (9.7) | 0.08 |
| Duration of the anaesthesia (min) | 86.0 (43.5) | 97.0 (49.3) | 84.3 (50.8) | 0.16 | 80.5 (32.5) | 80.9 (34.7) | 0.96 |
| PONV prophylaxes with dexamethasone 4 mg iv (yes) | 69 (29.6) | 25 (41.7) | 26 (41.3) | 0.96 | 8 (14.5) | 10 (18.2) | 0.61 |
| PONV prophylaxes with ondansetron 4 mg iv (yes) | 77 (32.8) | 29 (47.5) | 29 (45.3) | 0.80 | 9 (16.4) | 10 (18.2) | 0.80 |
| RR | Lower 95% CI | Upper 95% CI | p-Value | ||
|---|---|---|---|---|---|
| Females | |||||
| Experiencing pain | Tube size (standard) | 1.00 | 1.00 | 1.00 | |
| Tube size (small) | 0.56 | 0.35 | 0.90 | 0.02 | |
| Experiencing hoarseness | Tube size (standard) | 1.00 | 1.00 | 1.00 | |
| Tube size (small) | 0.75 | 0.51 | 1.11 | 0.16 | |
| Males | |||||
| Experiencing pain | Tube size (standard) | 1.00 | 1.00 | 1.00 | |
| Tube size (small) | 0.74 | 0.43 | 1.26 | 0.27 | |
| Experiencing hoarseness | Tube size (standard) | 1.00 | 1.00 | 1.00 | |
| Tube size (small) | 0.55 | 0.34 | 0.87 | 0.01 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Christiansen, P.; Pedersen, C.H.; Selter, H.; Odder, L.; Riisager, J.P.; Damgaard, K.; Westmark, S.; Bruun, N.H.; Melgaard, D. How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study. J. Clin. Med. 2021, 10, 5846. https://doi.org/10.3390/jcm10245846
Christiansen P, Pedersen CH, Selter H, Odder L, Riisager JP, Damgaard K, Westmark S, Bruun NH, Melgaard D. How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study. Journal of Clinical Medicine. 2021; 10(24):5846. https://doi.org/10.3390/jcm10245846
Chicago/Turabian StyleChristiansen, Pia, Caroline Hornnes Pedersen, Hansjörg Selter, Lillian Odder, Jette Præstholm Riisager, Kjeld Damgaard, Signe Westmark, Niels Henrik Bruun, and Dorte Melgaard. 2021. "How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study" Journal of Clinical Medicine 10, no. 24: 5846. https://doi.org/10.3390/jcm10245846
APA StyleChristiansen, P., Pedersen, C. H., Selter, H., Odder, L., Riisager, J. P., Damgaard, K., Westmark, S., Bruun, N. H., & Melgaard, D. (2021). How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study. Journal of Clinical Medicine, 10(24), 5846. https://doi.org/10.3390/jcm10245846






