Prevalence and Predisposing Factors for Recurrence after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Selection Criteria
2.2. Search Strategy
2.3. Data Collection Process and Data Items
2.4. Risk of Bias in Individual Studies
2.5. Summary Measures
2.6. Synthesis of Results
2.7. Risk of Bias across Studies
3. Results
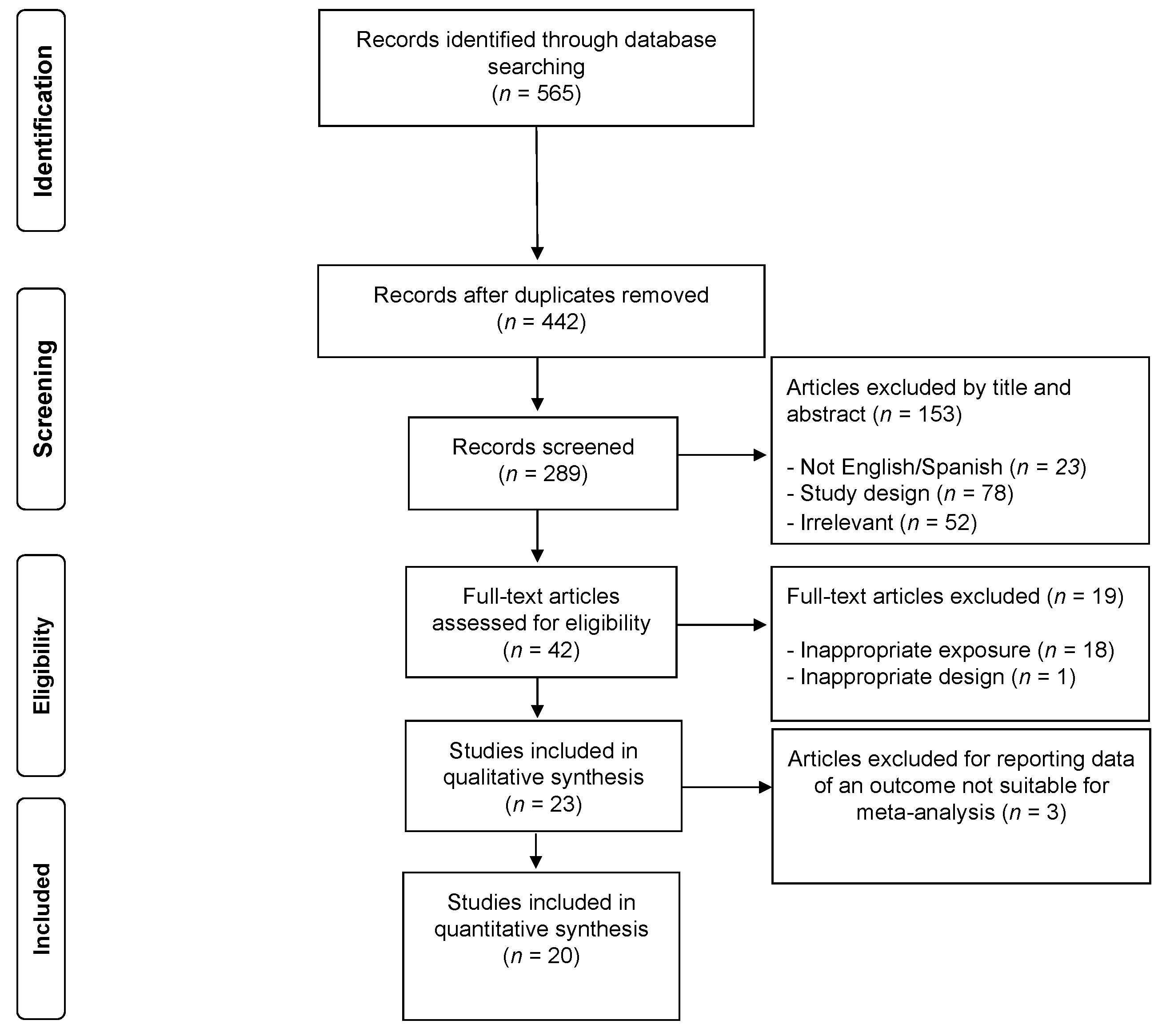
3.1. Study Selection
3.2. Study Characteristics
3.3. Measurements
3.4. Risk of Bias within Studies
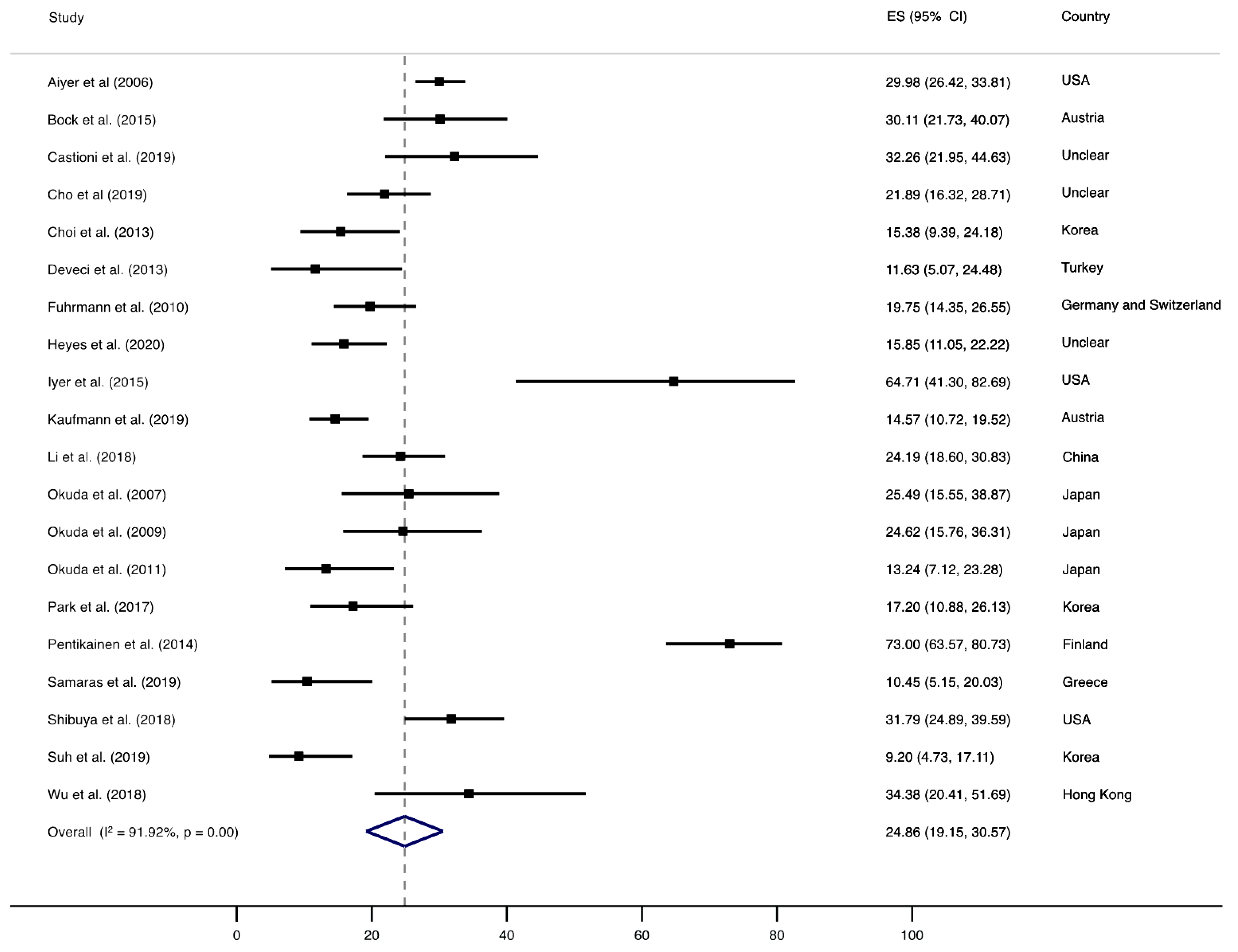
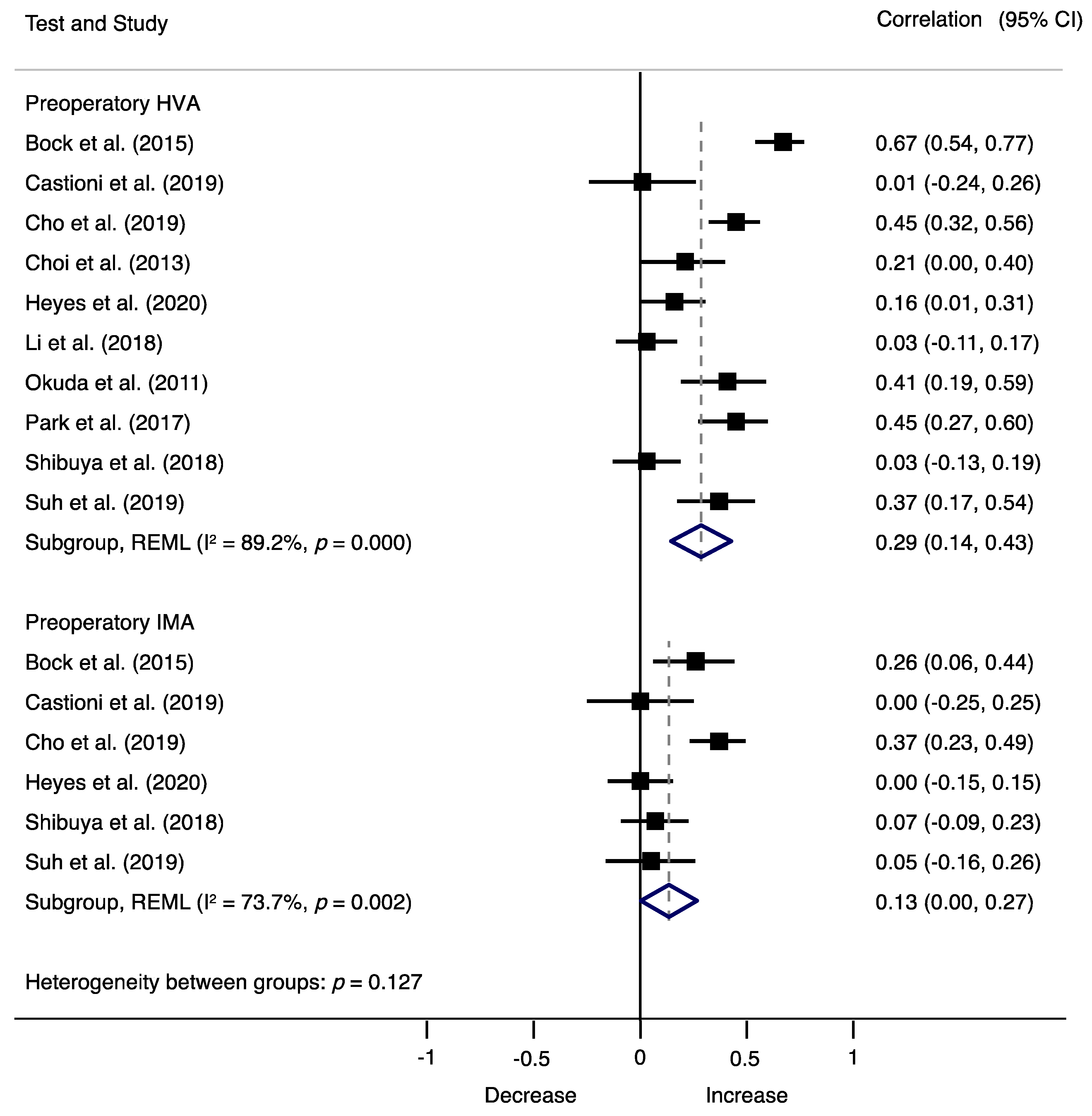
3.5. Synthesis of Results
4. Discussion
Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Nix, S.; Smith, M.; Vicenzino, B. Prevalence of hallux valgus in the general population: A systematic review and meta-analysis. J. Foot Ankle Res. 2010, 3, 21. [Google Scholar] [CrossRef] [Green Version]
- Robinson, A.H.N.; Limbers, J.P. Modern concepts in the treatment of hallux valgus. J. Bone Jt. Surg. Br. Vol. 2005, 87, 1038–1045. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; Rodríguez-Sanz, D.; Calvo-Lobo, C.; López-López, D. Impact of Hallux Valgus Related of Quality of Life in Women. Int. Wound J. 2017, 14, 782–785. [Google Scholar] [CrossRef] [PubMed]
- López, D.L.; Fernández, J.M.V.; Iglesias, M.E.L.; Castro, C.Á.; Lobo, C.C.; Galván, J.R.; Vallejo, R.B.D.B. Influence of depression in a sample of people with hallux valgus. Int. J. Ment. Health Nurs. 2016, 6, 574–578. [Google Scholar] [CrossRef] [PubMed]
- Pentikainen, I.; Ojala, R.; Ohtonen, P.; Piippo, J.; Leppilahti, J. Preoperative Radiological Factors Correlated to Long-Term Recurrence of Hallux Valgus Following Distal Chevron Osteotomy. Foot Ankle Int. 2014, 35, 1262–1267. [Google Scholar] [CrossRef]
- Raikin, S.M.; Miller, A.G.; Daniel, J. Recurrence of Hallux Valgus: A Review. Foot Ankle Clin. 2014, 19, 259–274. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. The shape of the lateral edge of the first metatarsal head as a risk factor for recurrence of hallux valgus. J. Bone Jt. Surg. Am. Vol. 2007, 89, 2163–2172. [Google Scholar] [CrossRef]
- Shibuya, N.; Kyprios, E.M.; Panchani, P.N.; Martin, L.R.; Thorud, J.C.; Jupiter, D.C. Factors Associated with Early Loss of Hallux Valgus Correction. J. Foot Ankle Surg. 2018, 57, 236–240. [Google Scholar] [CrossRef]
- Deveci, A.; Firat, A.; Yilmaz, S.; Oken, O.F.; Yildirim, A.O.; Ucaner, A.; Bozkurt, M. Short-term Clinical and Radiologic Results of the Scarf Osteotomy: What Factors Contribute to Recurrence? J. Foot Ankle Surg. 2013, 52, 771–775. [Google Scholar] [CrossRef]
- National Heart, Lung, and Blood Institute. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 11 October 2021).
- Bring, J. How to standardize regression coefficients. Am. Stat. 1994, 48, 209–213. [Google Scholar]
- Nieminen, P.; Lehtiniemi, H.; Vähäkangas, K.; Huusko, A.; Rautio, A. Standardised regression coefficient as an effect size index in summarising findings in epidemiological studies. Epidemiol. Biostat. Public Health 2013, 10, 1–15. [Google Scholar]
- Peterson, R.A.; Brown, S.P. On the Use of Beta Coefficients in Meta-Analysis. J. Appl. Psychol. 2005, 90, 175–181. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- McGrath, R.E.; Meyer, G.J. When Effect Sizes Disagree: The Case of r and d. Psychol. Methods 2006, 11, 386–401. [Google Scholar] [CrossRef] [Green Version]
- Nyaga, V.N.; Arbyn, M.; Aerts, M. Metaprop: A Stata command to perform meta-analysis of binomial data. Arch. Public Health 2014, 1, 39. [Google Scholar] [CrossRef] [Green Version]
- Newcombe, R.G. Two-sided confidence intervals for the single proportion: Comparison of seven methods. Stat. Med. 1998, 17, 857–872. [Google Scholar] [CrossRef]
- Barendregt, J.J.; Lee, Y.Y.; Norman, R.E.; Vos, T. Meta-analysis of prevalence. J. Epidemiol. Community Health 2013, 67, 974–978. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–561. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef] [PubMed]
- Furuya-Kanamori, L.; Barendregt, J.J.; Doi, S.A. A new improved graphical and quantitative method for detecting bias in meta-analysis. Int. J. Evid.-Based Healthc. 2018, 16, 195–203. [Google Scholar] [CrossRef]
- Iyer, S.; Demetracopoulos, C.A.; Sofka, C.M.; Ellis, S.J. High Rate of Recurrence Following Proximal Medial Opening Wedge Osteotomy for Correction of Moderate Hallux Valgus. Foot Ankle Int. 2015, 36, 756–763. [Google Scholar] [CrossRef]
- Aiyer, A.; Shub, J.; Shariff, R.; Ying, L.; Myerson, M. Radiographic recurrence of deformity after hallux valgus surgery in patients with metatarsus adductus. Foot Ankle Int. 2016, 37, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Cho, B.-K.; Park, J.-K.; Choi, S.-M.; SooHoo, N.F. Is generalized ligamentous laxity a prognostic factor for recurred hallux valgus deformity? Foot Ankle Surg. 2019, 25, 127–131. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Kitano, N.; Shima, H. Postoperative Incomplete Reduction of the Sesamoids as a Risk. Factor for Recurrence of Hallux Valgus. J. Bone Jt. Surg.-Am. Vol. 2009, 91, 1637–1645. [Google Scholar] [CrossRef]
- Okuda, R.; Kinoshita, M.; Yasuda, T.; Jotoku, T.; Shima, H.; Takamura, M. Hallux valgus angle as a predictor of recurrence following proximal metatarsal osteotomy. J. Orthop. Sci. 2011, 6, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.Y.; Lam, E.K.F. Can the Syndesmosis Procedure Prevent Metatarsus Primus Varus and Hallux Valgus Deformity Recurrence? A 5-Year Prospective Study. J. Foot Ankle Surg. 2018, 57, 316–324. [Google Scholar] [CrossRef] [Green Version]
- Seng, C.; Ho, D.C.; Chong, K.W. Restoring Sesamoid Position in Scarf Osteotomy: A Learning Curve. J. Foot Ankle Surg. 2015, 54, 1089–1092. [Google Scholar] [CrossRef]
- Bock, P.; Kluger, R.; Kristen, K.-H.; Mittlböck, M.; Schuh, R.; Trnka, H.-J. The Scarf Osteotomy with Minimally Invasive Lateral Release for Treatment of Hallux Valgus Deformity. J. Bone Jt. Surg.-Am. Vol. 2015, 97, 1238–1245. [Google Scholar] [CrossRef] [PubMed]
- Choi, G.W.; Choi, W.J.; Yoon, H.S.; Lee, J.W. Additional surgical factors affecting the recurrence of hallux valgus after Ludloff osteotomy. Bone Jt. J. 2013, 95, 803–808. [Google Scholar] [CrossRef]
- Park, C.H.; Lee, W.C. Recurrence of Hallux Valgus Can Be Predicted from Immediate Postoperative Non-Weight-Bearing Radiographs. J. Bone Jt. Surg.-Am. Vol. 2017, 99, 1190–1197. [Google Scholar] [CrossRef]
- Suh, J.W.; Kim, S.H.; Park, H.-W. Radiographic Risk Factors of Recurrent Hallux Valgus Deformity after Modified Scarf and Akin Osteotomy. J. Korean Foot Ankle Soc. 2019, 23, 159–165. [Google Scholar] [CrossRef]
- Goh, G.S.; Tay, A.Y.W.; Thever, Y.; Koo, K. Effect of Age on Clinical and Radiological Outcomes of Hallux Valgus Surgery. Foot Ankle Int. 2021, 42, 798–804. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Guo, M.; Zhu, Y.; Xu, X. The excessive length of first ray as a risk factor for hallux valgus recurrence. PLoS ONE 2018, 13, e0205560. [Google Scholar] [CrossRef]
- Kaufmann, G.; Hofmann, M.; Ulmer, H.; Putzer, D.; Hofer, P.; Dammerer, D. Outcomes after scarf osteotomy with and without Akin osteotomy a retrospective comparative study. J. Orthop. Surg. Res. 2019, 14, 193. [Google Scholar] [CrossRef] [Green Version]
- Fuhrmann, R.A.; Zollinger-Kies, H.; Kundert, H.-P. Mid-term Results of Scarf Osteotomy in Hallux Valgus. Int. Orthop. 2010, 34, 981–989. [Google Scholar] [CrossRef] [Green Version]
- Samaras, D.; Gougoulias, N.; Varitimidis, S.; Hantes, M.; Karachalios, T.; Malizos, K.; Dailiana, Z. Midterm Experience of Scarf Osteotomy as a New Technique in a General Orthopaedic Department. Foot 2019, 40, 68–75. [Google Scholar] [CrossRef]
- Deenik, A.R.; de Visser, E.; Louwerens, J.W.; Malefijt, W.; Draijer, F.; de Bie, R.A. Hallux valgus angle as main predictor for correction of hallux valgus. BMC Musculoskelet. Disord. 2008, 9, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Castioni, D.; Fanelli, D.; Gasparini, G.; Iannò, B.; Galasso, O. Scarf osteotomy for the treatment of moderate to severe hallux valgus: Analysis of predictors for midterm outcomes and recurrence. Foot Ankle Surg. 2020, 26, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Heyes, G.J.; Vosoughi, A.R.; Weigelt, L.; Mason, L.; Molloy, A. Pes Planus Deformity and Its Association with Hallux Valgus Recurrence Following Scarf Osteotomy. Foot Ankle Int. 2020, 41, 1212–1218. [Google Scholar] [CrossRef] [PubMed]
- Hatch, D.J.; Santrock, R.D.; Smith, B.; Dayton, P.; Weil, L. Triplane Hallux Abducto Valgus Classification. J. Foot Ankle Surg. 2018, 57, 972–981. [Google Scholar] [CrossRef]
- Collan, L.; Kankare, J.A.; Mattila, K. The biomechanics of the first metatarsal bone in hallux valgus: A preliminary study utilizing a weight bearing extremity CT. Foot Ankle Surg. 2013, 3, 155–161. [Google Scholar] [CrossRef]
- Mortier, J.-P.; Bernard, J.-L.; Maestro, M. Axial rotation of the first metatarsal head in a normal population and hallux valgus patients. Orthop. Traumatol. Surg. Res. 2012, 6, 677–683. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanaka, Y.; Takakura, Y.; Sugimoto, K.; Kumai, T.; Sakamoto, T.; Kadono, K. Precise Anatomic Configuration Changes in the First Ray of the Hallux Valgus Foot. Foot Ankle Int. 2000, 21, 651–656. [Google Scholar] [CrossRef]
- Wagner, E.; Wagner, P. Metatarsal Pronation in Hallux Valgus Deformity: A Review. J. Am. Acad. Orthop. Surg. Glob. Res. Rev. 2020, 4, e20-00091. [Google Scholar] [CrossRef] [PubMed]
- Adam, S.P.; Choung, S.C.; Gu, Y.; O’Malley, M.J. Outcomes after Scarf Osteotomy for Treatment of Adult Hallux Valgus Deformity. Clin. Orthop. Relat. Res. 2011, 469, 854. [Google Scholar] [CrossRef] [Green Version]
- Hardy, R.H.; Clapham, J.C.R. Observations on hallux valgus; based on a controlled series. J. Bone Jt. Surg.-Br. Vol. 1951, 33, 376–391. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, J.S.; Young, K.W.; Naraghi, R.N.; Cho, H.K.; Lee, S.Y. A New Measure of Tibial Sesamoid Position in Hallux Valgus in Relation to the Coronal Rotation of the First Metatarsal in CT Scans. Foot Ankle Int. 2015, 36, 944–952. [Google Scholar] [CrossRef] [PubMed]

| Study | Country | n (Females) | Mean Age (Range) | Follow-Up (Months) | Recurrence Definition | Recurrence Rate | Surgical Procedure |
|---|---|---|---|---|---|---|---|
| Aiyer et al., (2006) | USA | 587 | NR | 12 | HVA > 20° | 30% | Distal first metatarsal osteotomy (chevron), proximal first metatarsal ostetomy (scarf or Ludloff) or a Lapidus procedure |
| Bock et al., (2015) | Austria | 93 (87) | 50 (21–78) | 124 | HVA ≥ 20° | 30% | Scarf osteotomy |
| Castioni et al., (2019) | Unclear | 62 (56) | 57 | 38 | HVA > 20° | 32.8% | Scarf osteotomy |
| Cho et al., (2019) | Unclear | 169 (169) | 38 (18–58) | 46.3 | HVA > 20.0° | 21.7% and 17.1% | Proximal chevron osteotomy |
| Choi et al., (2013) | Korea | 91 (89) | 52 (22–74) | 26 | HVA ≥ 20.0° | 15.50% | Ludloff osteotomy combined with additional procedures |
| Deenik et al., (2008) | The Netherlands | 136 (118) | 43.5 | 28.8 | NR | 12 cases had severe recurrences | Bunionectomy, osteotomy, lateralization of the distal fragment, lateral release and medial capsulorrhaphy |
| Deveci et al., (2013) | Turkey | 43 (36) | 47.7 (21–65) | 26.2 | HVA > 15.0° | 11.62% | Scarf osteotomy |
| Fuhrmann et al., (2010) | Germany and Switzerland | 162 (156) | 53.8 (17–77) | 44.9 | HVA > 20.0° | 19.70% | Scarf osteotomy |
| Goh et al., (2021) | Singapore | 193 (179) | 53.9 (28–82) | 110.4 | HVA ≥ 20.0° | NR | Scarf osteotomy and additional procedures (Akin osteotomy and Weil osteotomy) |
| Heyes et al., (2020) | Unclear | 164 (154) | 52 | 6 | HVA > 15.0° | 16% | Scarf osteotomy |
| Iyer et al., (2015) | USA | 17 (14) | 47.7 (14–71) | 28.8 | Increased > 5° HVA postoperatively | 64.70% | Proximal medial opening wedge osteotomy, and associated procedures (Akin osteotomy, second hammertoe correction and medial sesamoidectomy for osteonecrosis) |
| Kaufmann et al., (2019) | Austria | 247(224) | 52.1 | 45.4 | HVA ≥ 20.0° | 14.70% | Scarf osteotomy (group S, n = 184) and additionally Akin osteotomy (group SA, n = 63 patients) |
| Li et al., (2018) | China | 186 | 56.5 (17–84) | 83.7 | HVA ≥ 20.0° | 24.20% | Chevron osteotomy combined with distal soft tissue procedure, Akin osteotomy, Weil osteotomy |
| Okuda et al., (2007) | Japan | 51 (51) | 53 | 48 | HVA ≥ 20.0° | 25% | Proximal metatarsal osteotomy |
| Okuda et al., (2009) | Japan | 65 (65) | 51 | 45 | HVA ≥ 20.0° | 25% | Proximal metatarsal osteotomy |
| Okuda et al., (2011) | Japan | 68 (68) | 53 | 33 | HVA ≥ 20.0° | 13.90% | Proximal metatarsal osteotomy |
| Park et al., (2017) | Korea | 93 (91) | 51 | 27.5 | HVA ≥ 20.0° | 17.10% | Chevron osteotomy combined with distal soft tissue procedure |
| Pentikainen et al., (2014) | Finland | 100 (92) | 39 | 94.8 | HVA > 15° | 73% | Chevron osteotomy |
| Samaras et al., (2019) | Greece | 67 (65) | 53.6 | 24 | NR | 10.44% | Scarf osteotomy |
| Seng et al., (2015) | Singapore | 71 | 48.7 | 1.5 | NR | NR | Scarf osteotomy |
| Shibuya et al., (2018) | USA | 151 (140) | 57 | 6 | HVA of ≥3° after ≥6 months postoperatively | 32% | Distal metatarsal osteotomy, modified Lapidus procedure and proximal/midshaft/double metatarsal osteotomies |
| Suh et al., (2019) | Korea | 87 | 44 | 20.6 | HVA > 20.0 | 9% | Scarf and Akin osteotomy |
| Wu et al., (2018) | Hong Kong | 32 (32) | 39 (14 to 63) | 63.2 | MPA > 20° | 35% | Syndesmosis procedure |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ezzatvar, Y.; López-Bueno, L.; Fuentes-Aparicio, L.; Dueñas, L. Prevalence and Predisposing Factors for Recurrence after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5753. https://doi.org/10.3390/jcm10245753
Ezzatvar Y, López-Bueno L, Fuentes-Aparicio L, Dueñas L. Prevalence and Predisposing Factors for Recurrence after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(24):5753. https://doi.org/10.3390/jcm10245753
Chicago/Turabian StyleEzzatvar, Yasmin, Laura López-Bueno, Laura Fuentes-Aparicio, and Lirios Dueñas. 2021. "Prevalence and Predisposing Factors for Recurrence after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 24: 5753. https://doi.org/10.3390/jcm10245753
APA StyleEzzatvar, Y., López-Bueno, L., Fuentes-Aparicio, L., & Dueñas, L. (2021). Prevalence and Predisposing Factors for Recurrence after Hallux Valgus Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(24), 5753. https://doi.org/10.3390/jcm10245753







