Elderly People’s Access to Emergency Departments during the COVID-19 Pandemic: Results from a Large Population-Based Study in Italy
Abstract
:1. Introduction
2. Methods
2.1. Context
2.2. Materials
2.3. Statistical Analysis
2.4. Ethical Statement
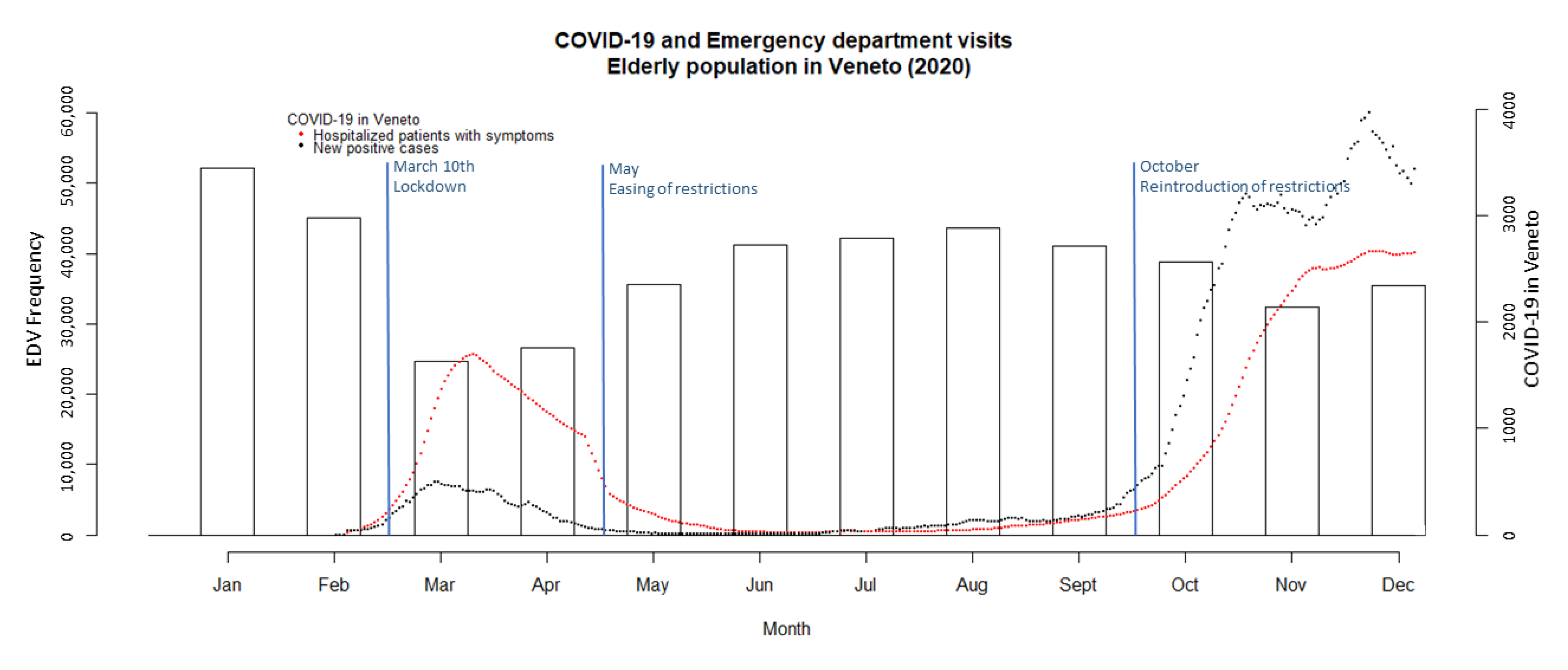
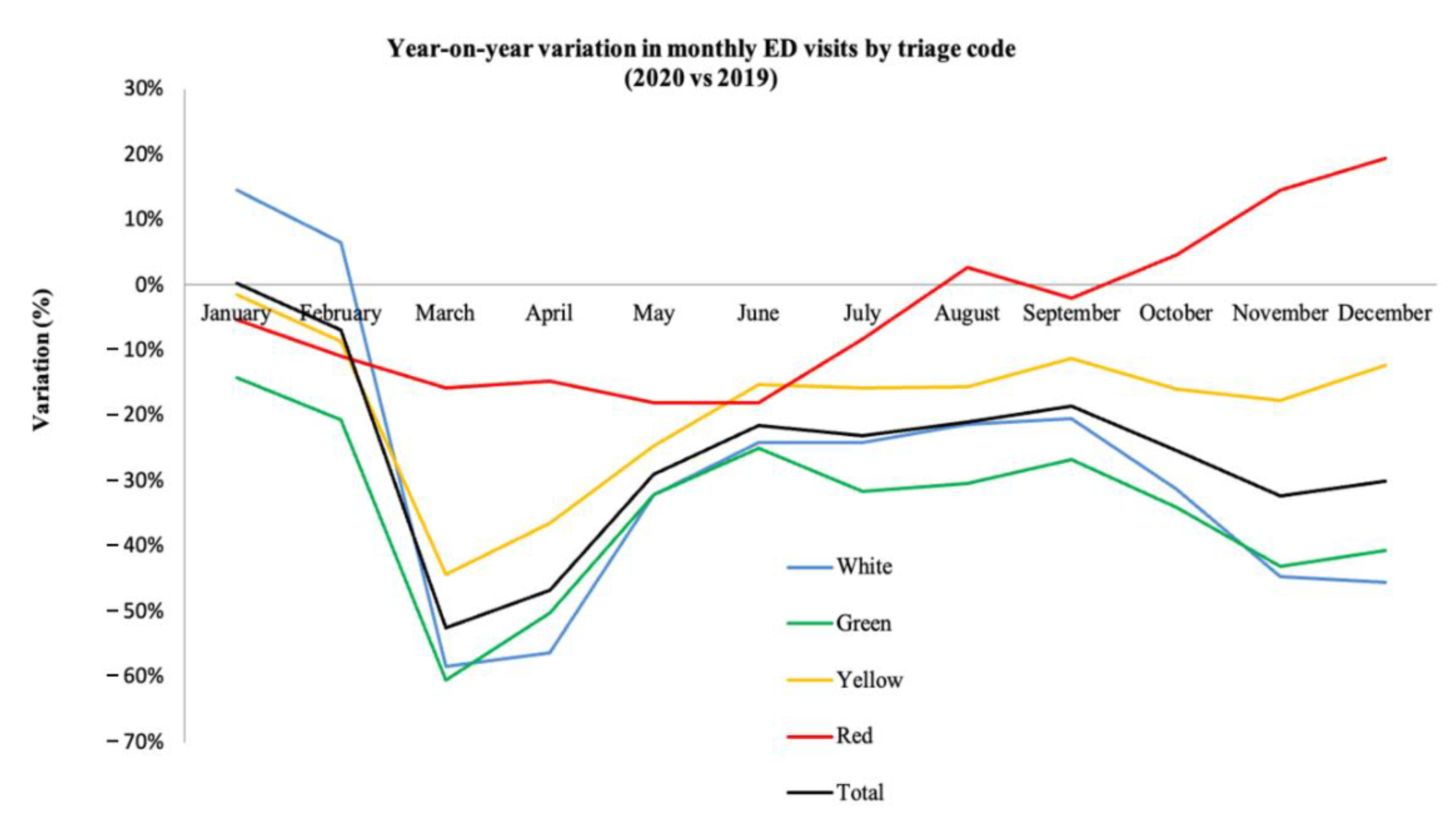
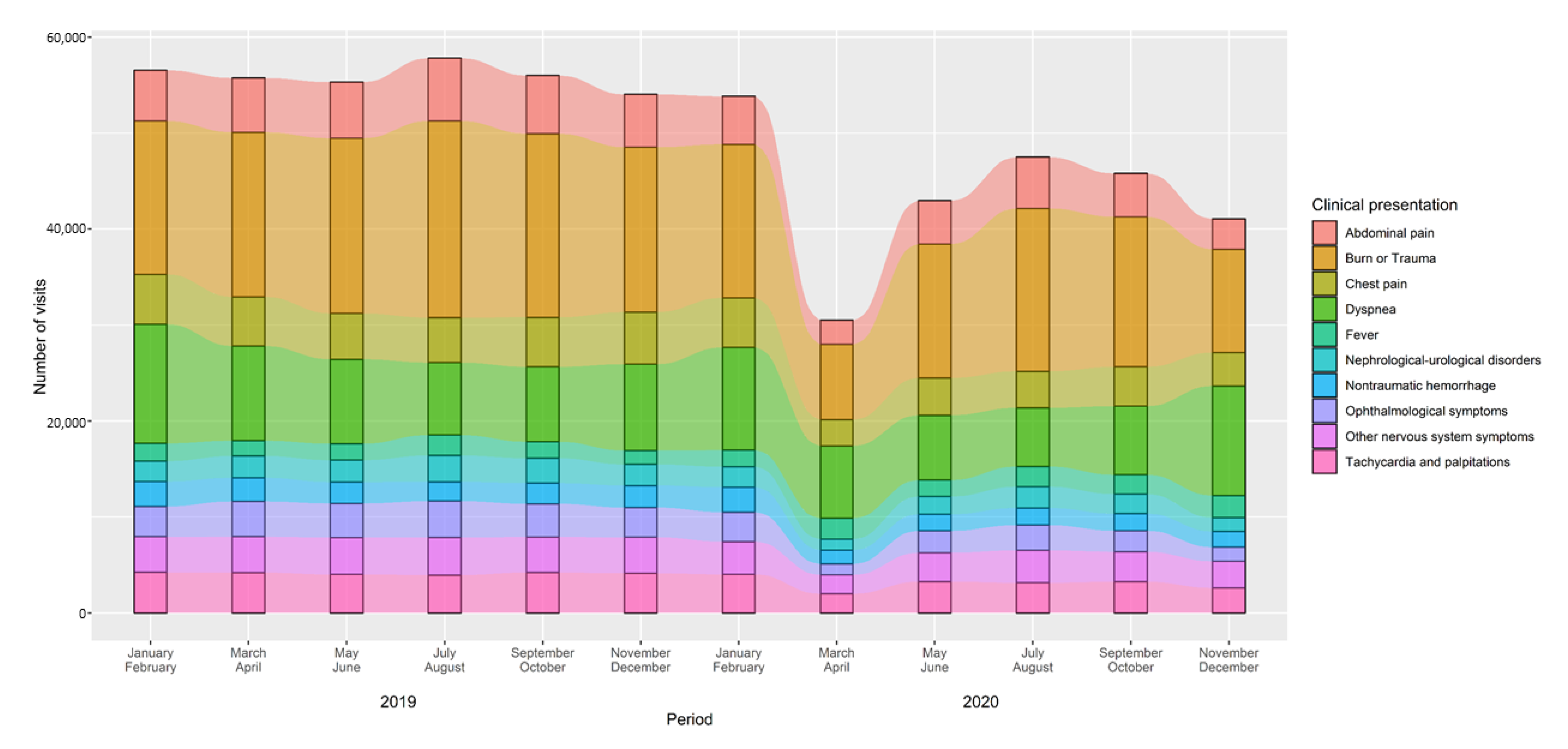
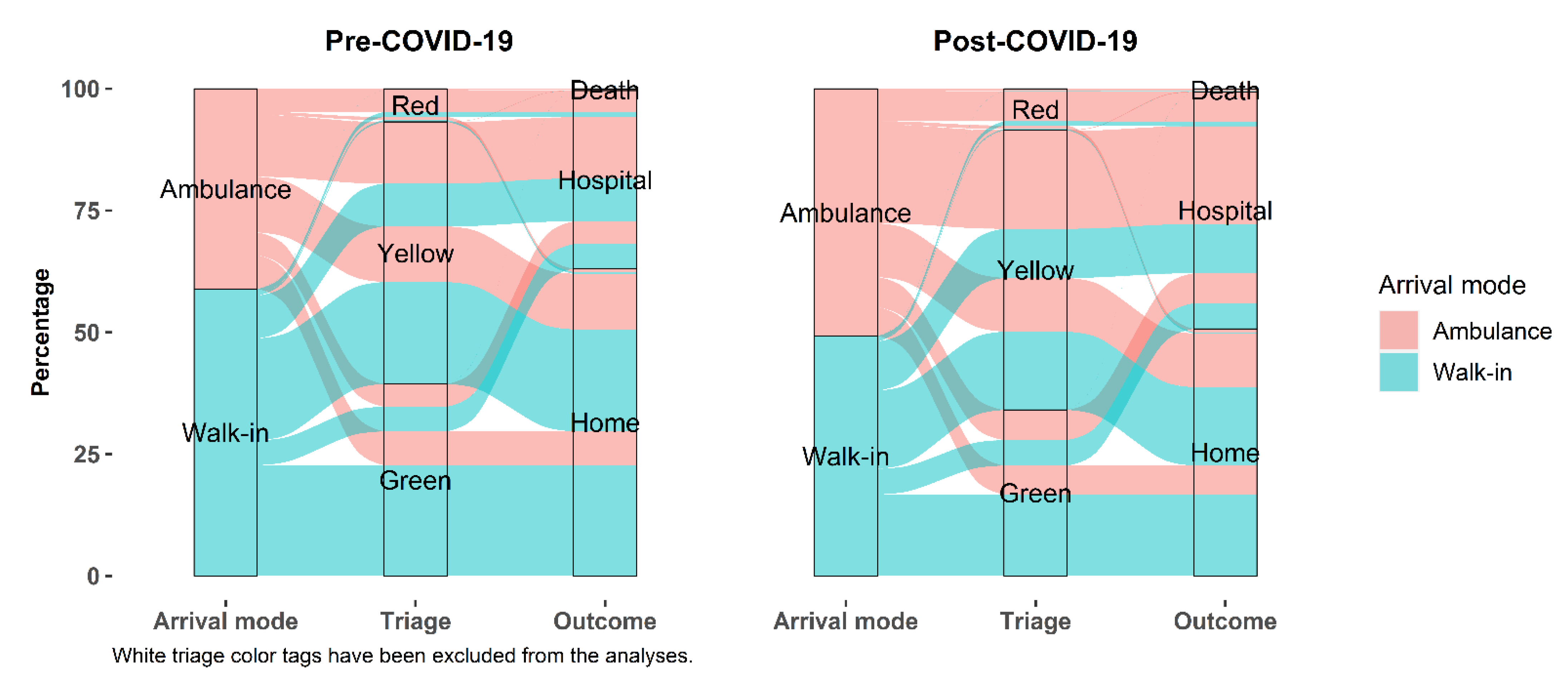
3. Results
4. Discussion
4.1. Overview on Emergency Department Visits
4.2. Outcomes of Emergency Department Visits
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Coronavirus Pandemic (COVID-19). Available online: https://ourworldindata.org/coronavirus (accessed on 1 October 2021).
- Epicentro, Istituto Superiore di Sanità. Dati della Sorveglianza Integrata COVID-19 in Italia. Available online: https://www.epicentro.iss.it/coronavirus/sars-cov-2-dashboard (accessed on 1 May 2021.).
- Russo, F.; Pitter, G.; Da Re, F.; Tonon, M.; Avossa, F.; Bellio, S.; Fedeli, U.; Gubian, L.; Monetti, D.; Saia, M.; et al. Epidemiology and public health response in early phase of COVID-19 pandemic, Veneto Region, Italy, 21 February to 2 April 2020. Eurosurveillance 2020, 25, 2000548. [Google Scholar] [CrossRef] [PubMed]
- Michalowsky, B.; Hoffmann, W.; Bohlken, J.; Kostev, K. Effect of the COVID-19 lockdown on disease recognition and utilisation of healthcare services in the older population in Germany: A cross-sectional study. Age Ageing 2021, 50, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Kapsner, L.A.; Kampf, M.O.; Seuchter, S.A.; Gruendner, J.; Gulden, C.; Mate, S.; Mang, J.M.; Schüttler, C.; Deppenwiese, N.; Krause, L.; et al. Reduced Rate of Inpatient Hospital Admissions in 18 German University Hospitals During the COVID-19 Lockdown. Front. Public Health 2021, 8, 594117. [Google Scholar] [CrossRef] [PubMed]
- Westgard, B.C.; Morgan, M.W.; Vazquez-Benitez, G.; Erickson, L.O.; Zwank, M.D. An Analysis of Changes in Emergency Department Visits after a State Declaration During the Time of COVID-19. Ann. Emerg. Med. 2020, 76, 595–601. [Google Scholar] [CrossRef]
- Wyatt, S.; A Mohammed, M.; Fisher, E.; McConkey, R.; Spilsbury, P. Impact of the SARS-CoV-2 pandemic and associated lockdown measures on attendances at emergency departments in English hospitals: A retrospective database study. Lancet Reg. Health-Eur. 2021, 2, 100034. [Google Scholar] [CrossRef]
- Kuitunen, I.; Ponkilainen, V.T.; Launonen, A.P.; Reito, A.; Hevonkorpi, T.P.; Paloneva, J.; Mattila, V.M. The effect of national lockdown due to COVID-19 on emergency department visits. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 1–8. [Google Scholar] [CrossRef]
- Baldi, E.; Sechi, G.M.; Mare, C.; Canevari, F.; Brancaglione, A.; Primi, R.; Klersy, C.; Palo, A.; Contri, E.; Ronchi, V.; et al. COVID-19 kills at home: The close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur. Heart J. 2020, 41, 3045–3054. [Google Scholar] [CrossRef]
- Chen, Q.; Zheng, Z.; Zhang, C.; Zhang, X.; Wu, H.; Wang, J.; Wang, S.; Zheng, C. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Tai-zhou, Zhejiang, China. Infection 2020, 48, 543–551. [Google Scholar] [CrossRef]
- E Lithander, F.; Neumann, S.; Tenison, E.; Lloyd, K.; Welsh, T.; Rodrigues, J.; Higgins, J.; Scourfield, L.; Christensen, H.; Haunton, V.; et al. COVID-19 in older people: A rapid clinical review. Age Ageing 2020, 49, 501–515. [Google Scholar] [CrossRef]
- De Leo, D.; Trabucchi, M. COVID-19 and the Fears of Italian Senior Citizens. Int. J. Environ. Res. Public Health 2020, 17, 3572. [Google Scholar] [CrossRef]
- Nourazari, S.; Davis, S.R.; Granovsky, R.; Austin, R.; Straff, D.J.; Joseph, J.W.; Sanchez, L.D. Decreased hospital admissions through emergency departments during the COVID-19 pandemic. Am. J. Emerg. Med. 2021, 42, 203–210. [Google Scholar] [CrossRef]
- ISTAT (Italian National Institute of Statistics). Available online: https://www.istat.it/it/files//2018/12/Report_Conti-regionali_2017.pdf (accessed on 1 November 2021).
- Pasin, L.; Sella, N.; Correale, C.; Boscolo, A.; Rosi, P.; Saia, M.; Mantoan, D.; Navalesi, P. Regional COVID-19 Network for Coordination of SARS-CoV-2 outbreak in Veneto, Italy. J. Cardiothorac. Vasc. Anesth. 2020, 34, 2341–2345. [Google Scholar] [CrossRef]
- Dipartimento della Protezione Civile. COVID-19 Monitoraggio Situazione: Dati di Dettaglio Relativi alla Regione del Veneto. Available online: https://dati.veneto.it/opendata/COVID_19_Monitoraggio_situazione_Dati_di_dettaglio_nel_Veneto (accessed on 1 May 2021).
- Pattern of emergency department referral during the COVID-19 outbreak in Italy. Panminerva Med. 2020. [CrossRef]
- Garrafa, E.; Levaggi, R.; Miniaci, R.; Paolillo, C. When fear backfires: Emergency department accesses during the Covid-19 pandemic. Health Policy 2020, 124, 1333–1339. [Google Scholar] [CrossRef]
- Ojetti, V.; Covino, M.; Brigida, M.; Petruzziello, C.; Saviano, A.; Migneco, A.; Candelli, M.; Franceschi, F. Non-COVID Diseases during the Pandemic: Where Have All Other Emergencies Gone? Medicina 2020, 56, 512. [Google Scholar] [CrossRef]
- Borch, C. The Exclusion of the Crowd. Eur. J. Soc. Theory 2006, 9, 83–102. [Google Scholar] [CrossRef] [Green Version]
- Ferry, A.V.; Keanie, C.; Denvir, M.A.; Mills, N.L.; Strachan, F.E. Chest pain presentations to hospital during the COVID-19 lockdown: Lessons for public health media campaigns. PLoS ONE 2021, 16, e0249389. [Google Scholar] [CrossRef]
- Harmon, K.J.; Fliss, M.D.; Marshall, S.W.; Peticolas, K.; Proescholdbell, S.K.; Waller, A.E. The impact of the COVID-19 pandemic on the utilization of emergency department services for the treatment of injuries. Am. J. Emerg. Med. 2021, 47, 187–191. [Google Scholar] [CrossRef]
- D’Ascenzi, F.; Cameli, M.; Forni, S.; Gemmi, F.; Szasz, C.; Di Fabrizio, V.; Mechi, M.T.; Nocci, M.; Mondillo, S.; Valente, S. Reduction of Emergency Calls and Hospitalizations for Cardiac Causes: Effects of COVID-19 Pandemic and Lockdown in Tuscany Region. Front. Cardiovasc. Med. 2021, 8, 625569. [Google Scholar] [CrossRef]
- Fedeli, U.; Schievano, E.; Avossa, F.; Pitter, G.; Barbiellini Amidei, C.; Grande, E.; Grippo, F. Different approaches to the analysis of causes of death during the COVID-19 epidemic. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 3610–3613. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, M.; Barbi, E.; Apicella, A.; Marchetti, F.; Cardinale, F.; Trobia, G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc. Health 2020, 4, e10–e11. [Google Scholar] [CrossRef]
- Folino, A.F.; Zorzi, A.; Cernetti, C.; Marchese, D.; Pasquetto, G.; Roncon, L.; Saccà, S.; Themistoclakis, S.; Turiano, G.; Verlato, R.; et al. Impact of COVID-19 epidemic on coronary care unit accesses for acute coronary syndrome in Veneto region, Italy. Am. Heart J. 2020, 226, 26–28. [Google Scholar] [CrossRef]
- Stella, F.; Alexopoulos, C.; Scquizzato, T.; Zorzi, A. Impact of the COVID-19 outbreak on emergency medical system missions and emergency department visits in the Venice area. Eur. J. Emerg. Med. 2020, 27, 298–300. [Google Scholar] [CrossRef]
- Lange, S.J.; Ritchey, M.D.; Goodman, A.B.; Dias, T.; Twentyman, E.; Fuld, J.; Schieve, L.A.; Imperatore, G.; Benoit, S.R.; Kite-Powell, A.; et al. Potential Indirect Effects of the COVID-19 Pandemic on Use of Emergency Departments for Acute Life-Threatening Conditions—United States, January–May 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 795–800. [Google Scholar] [CrossRef]
- Hartnett, K.P.; Kite-Powell, A.; Devies, J.; Coletta, M.A.; Boehmer, T.K.; Adjemian, J.; Gundlapalli, A.V. National Syndromic Surveillance Program Community of Practice Impact of the COVID-19 Pandemic on Emergency Department Visits—United States, January 1, 2019–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 699–704. [Google Scholar] [CrossRef]
- Fusco, M.; Buja, A.; Furlan, P. Older adults in Emergency Department: Management by clinical severity at triage. Ann Ig 2014, 26, 409–417. [Google Scholar]
- Legramante, J.M.; Morciano, L.; Lucaroni, F.; Gilardi, F.; Caredda, E.; Pesaresi, A.; Coscia, M.; Orlando, S.; Brandi, A.; Giovagnoli, G.; et al. Frequent Use of Emergency Departments by the Elderly Population When Continuing Care Is Not Well Established. PLoS ONE 2016, 11, e0165939. [Google Scholar] [CrossRef]
- Salvi, F.; Morichi, V.; Grilli, A.; Giorgi, R.; De Tommaso, G.; Dessì-Fulgheri, P. The elderly in the emergency department: A critical review of problems and solutions. Intern. Emerg. Med. 2007, 2, 292–301. [Google Scholar] [CrossRef]
- Gruneir, A.; Silver, M.J.; Rochon, P.A. Review: Emergency Department Use by Older Adults: A Literature Review on Trends, Appropriateness, and Consequences of Unmet Health Care Needs. Med Care Res. Rev. 2010, 68, 131–155. [Google Scholar] [CrossRef]
- Katayama, Y.; Kiyohara, K.; Kitamura, T.; Hayashida, S.; Shimazu, T. Influence of the COVID-19 pandemic on an emergency medical service system: A population-based, descriptive study in Osaka, Japan. Acute Med. Surg. 2020, 7, e534. [Google Scholar] [CrossRef]
| 2019 | 2020 | ∆ 2019–2020 | |||
|---|---|---|---|---|---|
| n | % | n | % | % | |
| TOTAL | 614,612 | 458,813 | −25.3% | ||
| Sex * | |||||
| Male | 283,302 | 46.1% | 218,331 | 47.6% | −22.9% |
| Female | 331,308 | 53.9% | 240,482 | 52.4% | −27.4% |
| Age | |||||
| 65–74 years | 217,198 | 35.3% | 161,105 | 35.1% | −25.8% |
| 75–84 years | 249,306 | 40.6% | 184,369 | 40.2% | −26.0% |
| ≥85 years | 148,108 | 24.1% | 113,339 | 24.7% | −23.5% |
| Month | |||||
| January | 51,988 | 8.5% | 52,187 | 11.4% | 0.4% |
| February | 48,408 | 7.9% | 45,047 | 9.8% | −6.9% |
| March | 51,697 | 8.4% | 24,633 | 5.4% | −52.4% |
| April | 49,526 | 8.1% | 26,598 | 5.8% | −46.3% |
| May | 50,021 | 8.1% | 35,643 | 7.8% | −28.7% |
| June | 52,383 | 8.5% | 41,263 | 9.0% | −21.2% |
| July | 54,820 | 8.9% | 42,272 | 9.2% | −22.9% |
| August | 55,397 | 9.0% | 43,643 | 9.5% | −21.2% |
| September | 50,330 | 8.2% | 41,054 | 9.0% | −18.4% |
| October | 51,876 | 8.4% | 38,761 | 8.5% | −25.3% |
| November | 47,634 | 7.8% | 32,331 | 7.1% | −32.1% |
| December | 50,532 | 8.2% | 35,381 | 7.7% | −30.0% |
| Triage code | |||||
| Red | 24,928 | 4.1% | 23,841 | 5.2% | −4.4% |
| Yellow | 200,309 | 32.6% | 163,946 | 35.7% | −18.2% |
| Green | 149,753 | 24.4% | 99,042 | 21.6% | −33.9% |
| White | 237,447 | 38.6% | 169,624 | 37.0% | −28.6% |
| Not indicated ** | 2175 | 0.4% | 2360 | 0.5% | 8.5% |
| Arrival mode *** | |||||
| Ambulance | 182,436 | 29.8% | 167,738 | 36.9% | −8.1% |
| Walk-in | 430,444 | 70.2% | 287,324 | 63.1% | −33.2% |
| Clinical Presentation (Chief Complaint) * | 2019 | 2020 | ∆ 2019–2020 | ||
|---|---|---|---|---|---|
| n | % | n | % | % | |
| Dermatological symptoms | 8153 | 1.3% | 4740 | 1.0% | −41.9% |
| Odontostomatological diseases | 845 | 0.1% | 520 | 0.1% | −38.5% |
| Ophthalmological symptoms | 20,685 | 3.4% | 12,767 | 2.8% | −38.3% |
| Allergic reactions | 2748 | 0.5% | 1716 | 0.4% | −37.6% |
| Ear, nose and throat disorders | 9538 | 1.6% | 6023 | 1.3% | −36.9% |
| Hypertension | 5220 | 0.9% | 3485 | 0.8% | −33.2% |
| Forensic/legal medicine | 202 | 0.0% | 137 | 0.0% | −32.2% |
| Other symptoms | 224,629 | 36.7% | 158,084 | 34.7% | −29.6% |
| Abdominal pain | 34,914 | 5.7% | 25,049 | 5.5% | −28.3% |
| Poisoning | 723 | 0.1% | 523 | 0.1% | −27.7% |
| Gynecological disorders | 1382 | 0.2% | 1010 | 0.2% | −26.9% |
| Tachycardia and palpitations | 24,727 | 4.0% | 18,199 | 4.0% | −26.4% |
| Burn or trauma | 108,187 | 17.7% | 81,190 | 17.8% | −25.0% |
| Shock | 6006 | 1.0% | 4576 | 1.0% | −23.8% |
| Nephrological-urological disorders | 14,213 | 2.3% | 10,833 | 2.4% | −23.8% |
| Chest pain | 30,384 | 5.0% | 23,161 | 5.1% | −23.8% |
| Other nervous system symptoms | 22,684 | 3.7% | 17,715 | 3.9% | −21.9% |
| Nontraumatic hemorrhage | 13,764 | 2.3% | 10,982 | 2.4% | −20.2% |
| Acute neurological syndrome | 11,149 | 1.8% | 9166 | 2.0% | −17.8% |
| Coma | 5221 | 0.9% | 4319 | 1.0% | −17.3% |
| Dyspnea | 55,430 | 9.1% | 49,700 | 10.9% | −10.3% |
| Social problems | 222 | 0.0% | 205 | 0.0% | −7.7% |
| Fever | 10,462 | 1.7% | 12,029 | 2.6% | 15.0% |
| TOTAL | 611,488 | 100% | 456,129 | 100% | −25.4% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bardin, A.; Buja, A.; Barbiellini Amidei, C.; Paganini, M.; Favaro, A.; Saia, M.; Baldo, V. Elderly People’s Access to Emergency Departments during the COVID-19 Pandemic: Results from a Large Population-Based Study in Italy. J. Clin. Med. 2021, 10, 5563. https://doi.org/10.3390/jcm10235563
Bardin A, Buja A, Barbiellini Amidei C, Paganini M, Favaro A, Saia M, Baldo V. Elderly People’s Access to Emergency Departments during the COVID-19 Pandemic: Results from a Large Population-Based Study in Italy. Journal of Clinical Medicine. 2021; 10(23):5563. https://doi.org/10.3390/jcm10235563
Chicago/Turabian StyleBardin, Andrea, Alessandra Buja, Claudio Barbiellini Amidei, Matteo Paganini, Andrea Favaro, Mario Saia, and Vincenzo Baldo. 2021. "Elderly People’s Access to Emergency Departments during the COVID-19 Pandemic: Results from a Large Population-Based Study in Italy" Journal of Clinical Medicine 10, no. 23: 5563. https://doi.org/10.3390/jcm10235563
APA StyleBardin, A., Buja, A., Barbiellini Amidei, C., Paganini, M., Favaro, A., Saia, M., & Baldo, V. (2021). Elderly People’s Access to Emergency Departments during the COVID-19 Pandemic: Results from a Large Population-Based Study in Italy. Journal of Clinical Medicine, 10(23), 5563. https://doi.org/10.3390/jcm10235563








