Biplanar Low-Dose Radiograph Is Suitable for Cephalometric Analysis in Patients Requiring 3D Evaluation of the Whole Skeleton
Abstract
:1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Image Acquisition
2.3. Comparison of BPXR and Lateral Cephalograms
- (1)
- Angles between pairs of lines constructed from the landmark coordinates on the BPXR lateral view (BPXR-L);
- (2)
- Angles between pairs of lines constructed from the landmark coordinates on the BPXR lateral view, as marked with the help of the corresponding PA view (a line indicates the corresponding height of the landmark on the PA view when the landmark is positioned on the lateral view in Idefix; BPXR-LPA);
- (3)
- Angles between pairs of lines drawn directly on the BPXR lateral view, without previous landmark identification (BPXR-A).
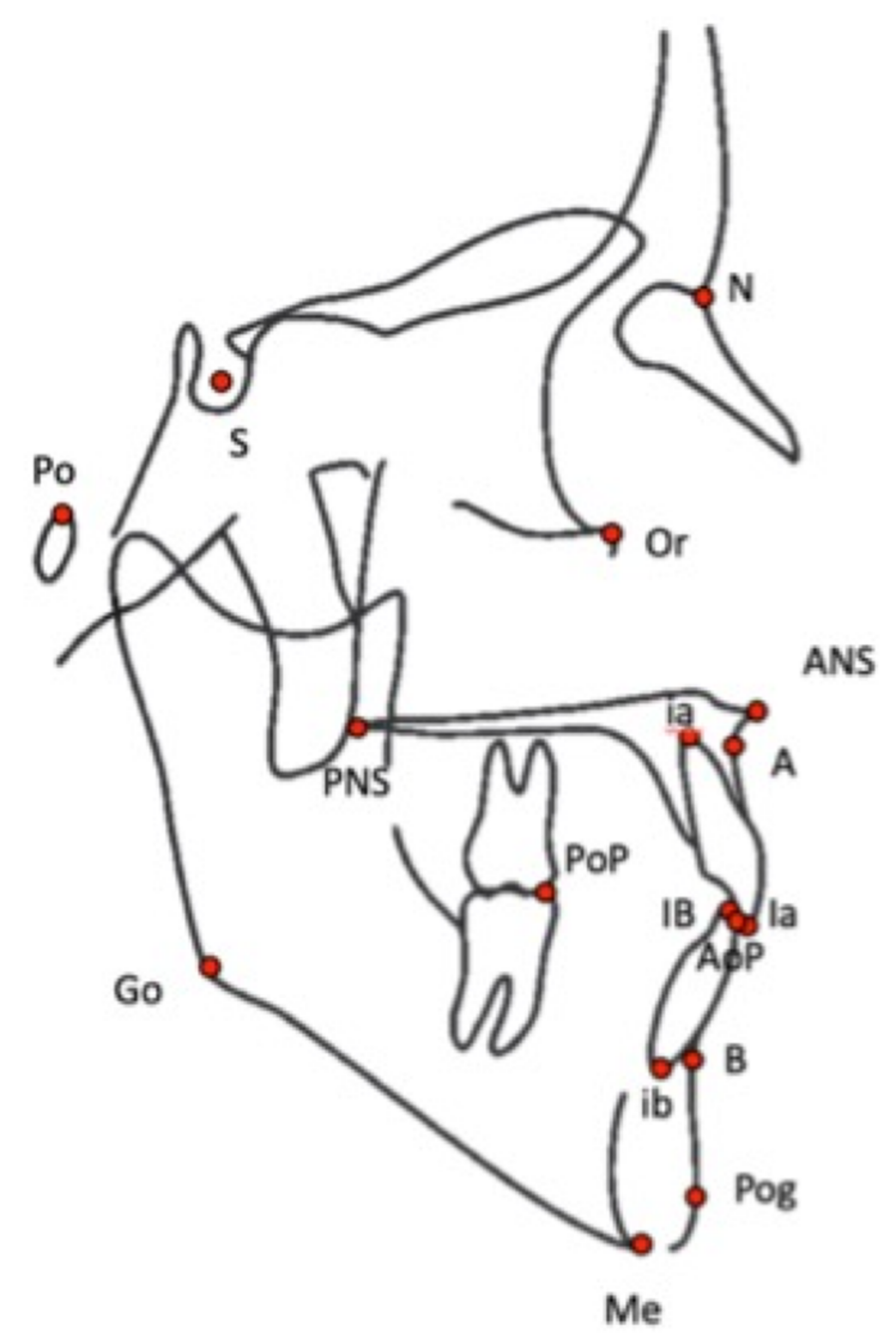
| Angle | Definition |
|---|---|
| SNA | Angle between S, N, and A points |
| SNB | Angle between S, N, and points |
| ANB | Angle between A, N, and B points |
| FMIA | Angle between Frankfort (Or-Po) plane and mandibular incisor axis (Bi-bi) |
| FMA | Angle between Frankfort plane and mandibular plane (Go-Me) |
| IMPA | Angle between mandibular incisor axis and mandibular plane |
| I/SN | Angle between maxillary incisor axis (Ia-ia) and S-N plane |
| I/i | Angle between maxillary incisor axis and mandibular incisor axis |
| SN/Pocc | Angle between S-N plane and occlusal plane (AoP-PoP) |
| Fr/Pocc | Angle between Frankfort plane and occlusal plane |
| Max/Mand | Angle between maxilla plane (ENA-ENP) and mandibular plane |
| Distance | Definition |
| S-N | Distance between S and N |
| ANS-PNS | Distance between ANS and PNS |
| Me-IB | Distance between Me and IB |
| N-ANS | Distance between N and ANS |

2.4. Statistical Analysis
2.4.1. Intraoperator Reliability
2.4.2. Interoperator Reliability
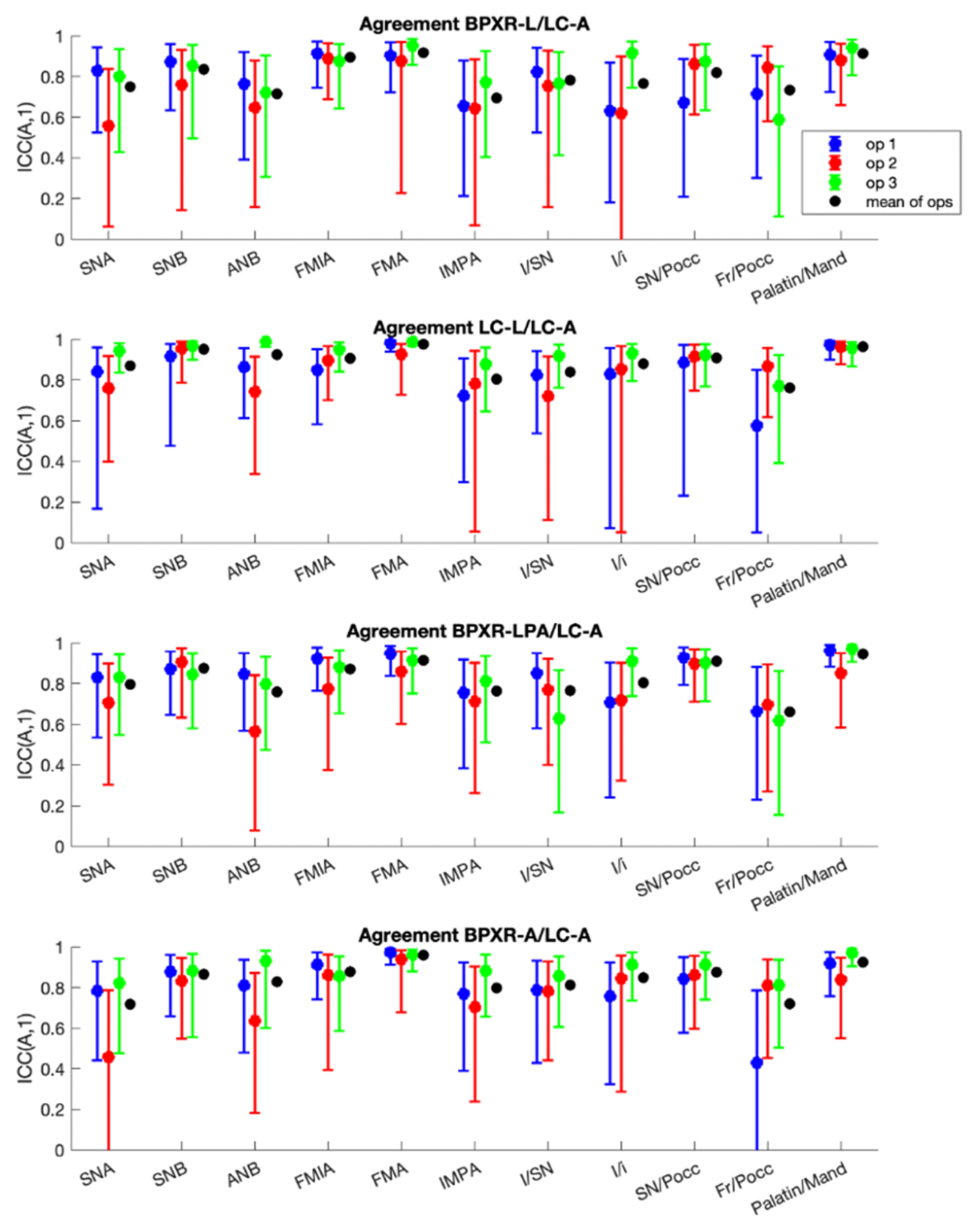
2.4.3. Concordance with the Reference Method
2.4.4. Linear Distances
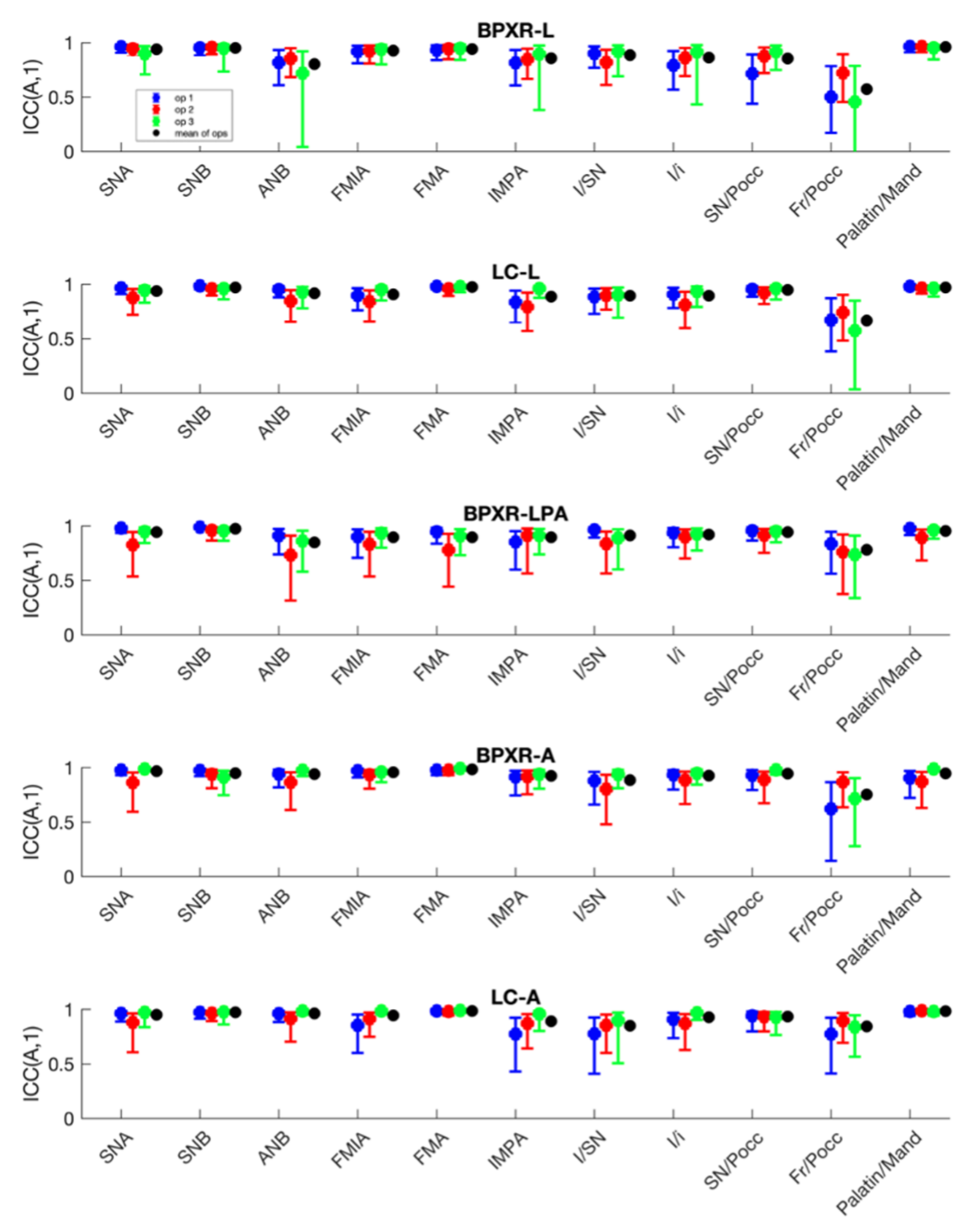
3. Results
3.1. Landmarks
3.2. Distances
3.3. Angles
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tweed, C.H. The Frankfort-mandibular plane angle in orthodontic diagnosis, classification, treatment planning, and prognosis. Am. J. Orthod. Oral Surg. 1946, 32, 175–230. [Google Scholar] [CrossRef]
- Sassouni, V. A roentgenographic cephalometric analysis of cephalo-facio-dental relationships. Am. J. Orthod. 1955, 41, 735–764. [Google Scholar] [CrossRef]
- Chen, S.-K.; Chen, Y.-J.; Yao, C.-C.J.; Chang, H.-F. Enhanced speed and precision of measurement in a computer-assisted digital cephalometric analysis system. Angle Orthod. 2004, 74, 501–507. [Google Scholar] [CrossRef]
- Melhem, E.; Assi, A.; El Rachkidi, R.; Ghanem, I. EOS® biplanar X-ray imaging: Concept, developments, benefits, and limitations. J. Child. Orthop. 2016, 10, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schlatterer, B.; Suedhoff, I.; Bonnet, X.; Catonne, Y.; Maestro, M.; Skalli, W. Skeletal landmarks for TKR implantations: Evaluation of their accuracy using EOS imaging acquisition system. Orthop. Traumatol. Surg. Res. 2009, 95, 2–11. [Google Scholar] [CrossRef] [Green Version]
- Dubousset, J.; Charpak, G.; Dorion, I.; Skalli, W.; Lavaste, F.; de Guise, J.A.; Kalifa, G.; Ferey, S. Le Système EOS. Nouvelle imagerie ostéo-articulaire basse dose en position debout. e-Mém. Acad. Natl. Chir. 2005, 4, 22–27. [Google Scholar] [CrossRef]
- Amabile, C.; Le Huec, J.-C.; Skalli, W. Invariance of head-pelvis alignment and compensatory mechanisms for asymptomatic adults older than 49 years. Eur. Spine J. 2018, 27, 458–466. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ilharreborde, B.; Dubousset, J.; Le Huec, J.-C. Use of EOS imaging for the assessment of scoliosis deformities: Application to postoperative 3D quantitative analysis of the trunk. Eur. Spine J. 2014, 23, S397–S405. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Morel, B.; Moueddeb, S.; Blondiaux, E.; Richard, S.; Bachy, M.; Vialle, R.; Ducou Le Pointe, H. Dose, image quality and spine modeling assessment of biplanar EOS micro-dose radiographs for the follow-up of in-brace adolescent idiopathic scoliosis patients. Eur. Spine J. 2018, 27, 1082–1088. [Google Scholar] [CrossRef] [Green Version]
- Pedersen, P.H.; Vergari, C.; Alzakri, A.; Vialle, R.; Skalli, W. A reduced micro-dose protocol for 3D reconstruction of the spine in children with scoliosis: Results of a phantom-based and clinically validated study using stereo-radiography. Eur. Radiol. 2019, 29, 1874–1881. [Google Scholar] [CrossRef] [Green Version]
- Vergari, C.; Bocahut, N.; Hernandez, T.; Assi, A.; Skalli, W.; Ilharreborde, B. Trunk growth in early-onset idiopathic scoliosis measured with biplanar radiography. Spine Deform. 2019, 7, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Yeung, K.H.; Man, G.C.W.; Skalli, W.; Hu, Z.; Hung, V.W.Y.; Hung, A.L.H.; Lam, T.P.; Ng, B.K.W.; Cheng, J.C.Y.; Vergari, C.; et al. Global sagittal alignment after surgery of right thoracic idiopathic scoliosis in adolescents and adults with and without thoracic hypokyphosis. Sci. Rep. 2021, 11, 6294. [Google Scholar] [CrossRef] [PubMed]
- Kerbrat, A.; Schouman, T.; Decressain, D.; Rouch, P.; Attali, V. Interaction between posture and maxillomandibular deformity: A systematic review. Int. J. Oral Maxillofac. Surg. 2021, S0901502721001703. [Google Scholar] [CrossRef] [PubMed]
- Saccucci, M.; Tettamanti, L.; Mummolo, S.; Polimeni, A.; Festa, F.; Salini, V.; Tecco, S. Scoliosis and dental occlusion: A review of the literature. Scoliosis 2011, 6, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.-Y.; Guilleminault, C.; Chiu, H.-Y.; Sullivan, S.S. Mouth breathing, “nasal disuse”, and pediatric sleep-disordered breathing. Sleep Breath 2015, 19, 1257–1264. [Google Scholar] [CrossRef] [PubMed]
- Clavel, L.; Rémy-Neris, S.; Skalli, W.; Rouch, P.; Lespert, Y.; Similowski, T.; Sandoz, B.; Attali, V. Cervical spine hyperextension and altered posturo-respiratory coupling in patients with obstructive sleep apnea syndrome. Front. Med. 2020, 7, 30. [Google Scholar] [CrossRef]
- Verin, E.; Sériès, F.; Locher, C.; Straus, C.; Zelter, M.; Derenne, J.-P.; Similowski, T. Effects of neck flexion and mouth opening on inspiratory flow dynamics in awake humans. J. Appl. Physiol. 2002, 92, 84–92. [Google Scholar] [CrossRef] [PubMed]
- Berg, B.-I.; Laville, A.; Courvoisier, D.S.; Rouch, P.; Schouman, T. Experiences with a new biplanar low-dose X-ray device for imaging the facial skeleton: A feasibility study. PLoS ONE 2020, 15, e0235032. [Google Scholar] [CrossRef] [PubMed]
- Chaibi, Y.; Cresson, T.; Aubert, B.; Hausselle, J.; Neyret, P.; Hauger, O.; de Guise, J.A.; Skalli, W. Fast 3D reconstruction of the lower limb using a parametric model and statistical inferences and clinical measurements calculation from biplanar X-rays. Comput. Methods Biomech. Biomed. Eng. 2012, 15, 457–466. [Google Scholar] [CrossRef] [PubMed]
- McGraw, K.O.; Wong, S.P. Forming inferences about some intraclass correlation coefficients. Psychol. Methods 1996, 1, 30–46. [Google Scholar] [CrossRef]
- Koo, T.K.; Li, M.Y. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J. Chiropr. Med. 2016, 15, 155–163. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deschênes, S.; Charron, G.; Beaudoin, G.; Labelle, H.; Dubois, J.; Miron, M.-C.; Parent, S. Diagnostic imaging of spinal deformities: Reducing patients radiation dose with a new slot-scanning X-ray imager. Spine 2010, 35, 989–994. [Google Scholar] [CrossRef]
- Charpak, G. La détection des particules. Recherche 1981, 12, 1384–1396. [Google Scholar]
- Wybier, M.; Bossard, P. Musculoskeletal imaging in progress: The EOS imaging system. Jt. Bone Spine 2013, 80, 238–243. [Google Scholar] [CrossRef]
- Rino Neto, J.; Paiva, J.B.D.; Queiroz, G.V.; Attizzani, M.F.; Miasiro, H., Jr. Evaluation of radiographic magnification in lateral cephalograms obtained with different X-ray devices: Experimental study in human dry skull. Dent. Press J. Orthod. 2013, 18, 17e1–17e7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chadwick, J.W.; Prentice, R.N.; Major, P.W.; Lam, E.W.N. Image distortion and magnification of 3 digital CCD cephalometric systems. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontol. 2009, 107, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Chiron, P.; Demoulin, L.; Wytrykowski, K.; Cavaignac, E.; Reina, N.; Murgier, J. Radiation dose and magnification in pelvic X-ray: EOS™ imaging system versus plain radiographs. Orthop. Traumatol. Surg. Res. 2017, 103, 1155–1159. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, M.; Jabour, F.; Sakai, K.; Hatsushikano, S.; Le Huec, J.C.; Hasegawa, K. Sagittal balance measures are more reproducible when measured in 3D vs. in 2D using full-body EOS® images. Eur. Radiol. 2018, 28, 4570–4577. [Google Scholar] [CrossRef] [PubMed]
- Laskowska, M.; Olczak-Kowalczyk, D.; Zadurska, M.; Czubak, J.; Czubak-Wrzosek, M.; Walerzak, M.; Tyrakowski, M. Evaluation of a relationship between malocclusion and idiopathic scoliosis in children and adolescents. J. Child. Orthop. 2019, 13, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Houston, W.J.B.; Maher, R.E.; McElroy, D.; Sherriff, M. Sources of error in measurements from cephalometric radiographs. Eur. J. Orthod. 1986, 8, 149–151. [Google Scholar] [CrossRef]
- Baumrind, S.; Frantz, R.C. The reliability of head film measurements. 1. Landmark identification. Am. J. Orthod. 1971, 60, 111–127. [Google Scholar] [CrossRef]
- Tng, T.T.; Chan, T.C.; Hägg, U.; Cooke, M.S. Validity of cephalometric landmarks. An experimental study on human skulls. Eur. J. Orthod. 1994, 16, 110–120. [Google Scholar] [CrossRef] [PubMed]
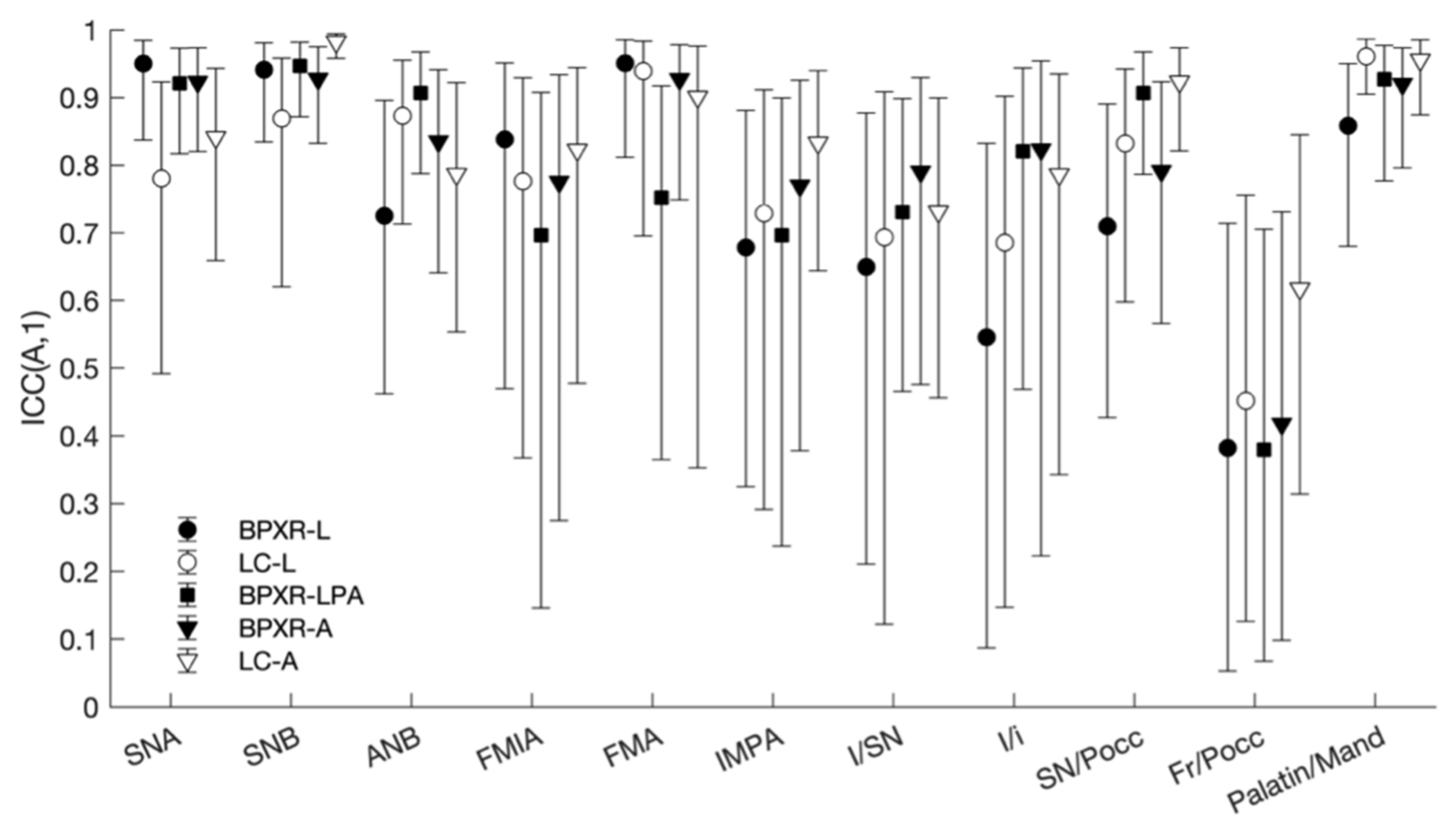
| Angle | LC-A 1 | BPXR-A 2 | BPXR-LPA 3 | LC-L 4 | BPXR-L 5 | Mean |
|---|---|---|---|---|---|---|
| SNA | 0.84 | 0.92 | 0.92 | 0.78 | 0.95 | 0.90 |
| SNB | 0.98 | 0.93 | 0.95 | 0.87 | 0.94 | 0.94 |
| ANB | 0.79 | 0.84 | 0.90 | 0.87 | 0.73 | 0.84 |
| FMIA | 0.82 | 0.78 | 0.70 | 0.78 | 0.84 | 0.79 |
| FMA | 0.90 | 0.93 | 0.75 | 0.94 | 0.95 | 0.91 |
| IMPA | 0.83 | 0.77 | 0.70 | 0.73 | 0.68 | 0.75 |
| I/SN | 0.73 | 0.80 | 0.73 | 0.69 | 0.65 | 0.72 |
| I/i | 0.79 | 0.82 | 0.82 | 0.69 | 0.55 | 0.75 |
| SN/Pocc | 0.92 | 0.79 | 0.91 | 0.83 | 0.71 | 0.85 |
| Fr/Pocc | 0.62 | 0.42 | 0.38 | 0.45 | 0.38 | 0.45 |
| Max/Mand | 0.96 | 0.92 | 0.93 | 0.96 | 0.86 | 0.93 |
| Mean | 0.87 | 0.84 | 0.83 | 0.82 | 0.81 | - |
| Angle | BPXR-A 1 | BPXR-LPA 2 | BPXR-L 3 |
|---|---|---|---|
| SNA | 0.72 | 0.80 | 0.75 |
| SNB | 0.87 | 0.88 | 0.83 |
| ANB | 0.83 | 0.76 | 0.71 |
| FMIA | 0.88 | 0.87 | 0.89 |
| FMA | 0.96 | 0.91 | 0.92 |
| IMPA | 0.80 | 0.76 | 0.70 |
| I/SN | 0.81 | 0.77 | 0.78 |
| I/i | 0.85 | 0.80 | 0.77 |
| SN/Pocc | 0.88 | 0.91 | 0.82 |
| Fr/Pocc | 0.72 | 0.66 | 0.73 |
| Max/Mand | 0.93 | 0.95 | 0.91 |
| Mean | 0.86 | 0.84 | 0.82 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerbrat, A.; Rivals, I.; Dupuy, P.; Dot, G.; Berg, B.-I.; Attali, V.; Schouman, T. Biplanar Low-Dose Radiograph Is Suitable for Cephalometric Analysis in Patients Requiring 3D Evaluation of the Whole Skeleton. J. Clin. Med. 2021, 10, 5477. https://doi.org/10.3390/jcm10235477
Kerbrat A, Rivals I, Dupuy P, Dot G, Berg B-I, Attali V, Schouman T. Biplanar Low-Dose Radiograph Is Suitable for Cephalometric Analysis in Patients Requiring 3D Evaluation of the Whole Skeleton. Journal of Clinical Medicine. 2021; 10(23):5477. https://doi.org/10.3390/jcm10235477
Chicago/Turabian StyleKerbrat, Adeline, Isabelle Rivals, Pauline Dupuy, Gauthier Dot, Britt-Isabelle Berg, Valérie Attali, and Thomas Schouman. 2021. "Biplanar Low-Dose Radiograph Is Suitable for Cephalometric Analysis in Patients Requiring 3D Evaluation of the Whole Skeleton" Journal of Clinical Medicine 10, no. 23: 5477. https://doi.org/10.3390/jcm10235477
APA StyleKerbrat, A., Rivals, I., Dupuy, P., Dot, G., Berg, B.-I., Attali, V., & Schouman, T. (2021). Biplanar Low-Dose Radiograph Is Suitable for Cephalometric Analysis in Patients Requiring 3D Evaluation of the Whole Skeleton. Journal of Clinical Medicine, 10(23), 5477. https://doi.org/10.3390/jcm10235477







