Abstract
Data on the clinical outcomes comparing synthetic fluorocarbon polymer polytetrafluoroethylene- (PTFE, GraftMaster) and polyurethane- (Papyrus) covered stents (CSs) to seal coronary artery perforations (CAPs) are limited. We aimed to evaluate 30-day and 1-year clinical outcomes after PCI complicated by CAP and treated with CS. We assessed 106 consecutive patients with successful CAP sealing (122 CSs): GraftMaster (51 patients, 57 CSs) or Papyrus CS (55 patients, 65 CSs). The primary endpoint was the occurrence of major adverse cardiac events (MACE), defined as the composite of cardiac death, target lesion revascularisation (TLR), and myocardial infarction (MI). The mean age of subjects was 69 ± 9.6 years (53.8% males). No significant differences were identified between the GraftMaster and Papyrus groups at the 30-day follow-up for MACE, cardiac death, MI and stent thrombosis (ST), while significantly lower rate of TLR and TVR (p = 0.02) were confirmed in the Papyrus group. At one year, differences remained similar between stents for MACE, a trend towards a lower rate of TLR (p = 0.07), MI (p = 0.08), and ST (p = 0.08), and higher for cardiac death (p = 0.07) was observed in the Papyrus group. This real-life registry of CAP illustrated that the use of Papyrus CS is associated with lower rates of TLR and TVR at 30-day follow-up in comparison to the GraftMaster CSs and no significant differences between both assessed CS at one year of follow-up.
1. Introduction
Coronary artery perforation (CAP) is a rare periprocedural complication, which occurs in 0.17–0.43% of patients during percutaneous coronary intervention (PCI) [1,2]; the incidence increases to 4.1–4.8% in procedures performed on complex lesions [3,4]. The Ellis classification remains a recommended tool that stratifies CAP severity and guides through its management [5]. Mild perforations are usually sufficiently treated with prolonged balloon inflation or additional stent implantation. Advanced techniques that include the use of coagulation reversal agents, blood component transfusion, urgent cardiac surgery, or covered stent (CS) implantation are applied in case of life-threatening CAPs of the large vessels with haemodynamic instability and resistance against standard treatment [6]. In previous research, it was shown that in CSs, satisfactory safety is exhibited as well as efficacy profile for the management of CAPs during PCI [7]. The construction of CS consists of a metallic stent platform covered with a synthetic (expanded polytetrafluoroethylene (GraftMaster) or electrospun polyurethane (Papyrus)) or biological membrane (pericardium) that seals the blood extravasation [7]. The differences in the type of stent cover and structure (sandwich or out-/inlayer cover) impact the endothelialisation process that prolongs stent thrombogenicity potency, similarly to other implantable devices [7,8]. This biocompatibility translates into a significantly higher risk of adverse events with CSs as compared to drug-eluting stents (DES), but not to bare metal stents (BMS) [9,10]. In previous studies, there were no broad reports on the effect of variance within CS structure type. To address this evidence gap, we conducted a study focusing on one-year results and predictors of clinical outcomes of CAP patients treated with GraftMaster and Papyrus implantation.
2. Methods
A detailed description of the multicentre, observational CRACK Registry (NCT04630314) design has been previously presented [11]. The dataset included consecutive patients with iatrogenic, peri-PCI CAP, treated with CS implantation between January 2009 and October 2019, at 8 high-volume PCI centres. Outcome data were obtained from the central database of the National Health Fund Service of the Ministry of Health, asserting follow-up completion for all patients. If re-PCI or coronary artery bypass surgery occurred during the follow-up period, data on target vessel revascularisation (TVR) and target lesion revascularisation (TLR) were collected. Data were anonymised at the level of each centre, merged into a single database, and statistically analysed. The study was approved by the appropriate local ethical committees. The patient’s data were protected according to the requirements of Polish law, General Data Protection Regulation (GDPR) and hospital Standard Operating Procedures. The study was conducted in accordance with the Declaration of Helsinki.
2.1. Evaluated Covered Stents and Structural Insight
Two types of CS were evaluated: GraftMaster CS and Papyrus CS. The main technological differences between the two stents are graft material and stent design. The GraftMaster (Abbott Vascular, Santa Clara, CA, USA) CS is constructed using the sandwich technique, whereby a layer of expanded polytetrafluoroethylene (ePTFE) is placed between two stainless steel stents. The study stent was available in sizes 3–4 mm, 6–7 Fr guide catheter compatible. The PK Papyrus (Biotronik, Bülach, Switzerland) CS is a single layer 90-µm electrospun polyurethane-covered cobalt-chromium stent. The study stent was available in sizes 2.5–5 mm, 5–6 Fr guide catheter compatible.
2.2. Procedure
The PCI procedure with CS implantation and antithrombotic treatment was at the operator’s discretion, in accordance with the recommendations of the guidelines for clinical practice [12].
2.3. Angiography Analysis
Morphology of the stented lesion was defined according to the classification proposed by the ACC/AHA (American College of Cardiology/American Heart Association) [13]. Lesion length, percentage diameter stenosis, and the coronary flow (thrombolysis in myocardial infarction—TIMI classification) were assessed in all patients. Measurements were performed by two experienced interventional cardiologists based on cine coronary angiography at each site, on the angiograph available in catheterization laboratory, and interim quantitative coronary angiography dedicated to the particular angiograph. The three-staged Ellis classification was used to determine the degree of perforation based on angiographic manifestation [5].
2.4. Patient Follow-Up and Study Endpoints
The primary endpoint was the composite of major adverse cardiac events (MACE) defined as cardiac death, target lesion revascularisation (TLR) and myocardial infarction (MI) assessed at 30 days and 1 year from the index procedure. The secondary endpoints were stent thrombosis (ST) and the individual events of the primary composite endpoint. TLR was defined as any revascularisation within the treated lesion. ST was defined as acute (0–24 h post stent implantation), subacute (from 24 h to 30 days post stent implantation), or late (from 30 days to 1 year after stent implantation) [14].
2.5. Statistical Analysis
Categorical variables are presented as numbers and percentages. Continuous variables are expressed as mean ± standard deviation (SD). Normality was assessed by the Shapiro-Wilk test. Equality of variances was assessed using Levene’s test. Differences between groups were compared using the student’s or Welch’s t-test depending on the equality of variances for normally distributed variables. The Mann–Whitney U-test was used for non-normally distributed continuous variables. Ordinal variables were compared using the Cochran–Armitage test for trend or the Mann–Whitney U-test. Nominal variables were compared via Pearson’s chi-squared test or Fisher’s exact test if 20% of cells had an expected count of less than 5.
To analyse event-free survival in selected risk groups, Kaplan–Meier curves were drawn. The log-rank statistic was used to test differences in outcomes between the groups. Determinants of MACE, cardiac death, TLR, TVR, re-PCI, and myocardial infarction were determined by univariate and multivariate Cox regression models. The multivariate models were adjusted according to age, sex and BMI. Statistical analyses were performed with JMP®, Version 16.0.0 (SAS Institute INC., Cary, NC, USA).
3. Results
3.1. Baseline Clinical Characteristics
The registry included 106 patients with CAP, among which 51 (48.1%) received Graft Master CS and 55 (51.9%) Papyrus CS. There were no significant differences in age, gender or concomitant diseases between the GraftMaster and Papyrus groups, except for the atrial fibrillation, which occurred significantly more often in the Papyrus group (11.8% vs. 29.1%, p = 0.03), as well as greater borderline frequency of prior myocardial infarction in the GraftMaster group (43.1% vs. 25.5%, p = 0.05). Moreover, patients from the Papyrus group where qualified for PCI significantly more often due to non ST-segment elevation myocardial infarction (NSTEMI) (32.7% vs. 11.8%, p = 0.01) (Table 1).

Table 1.
General characteristics and left ventricle ejection fraction.
3.2. Angiographic and Culprit Lesion Characteristics
Patients who experienced CAP within the right coronary artery during PCI significantly more often received Papyrus CS PCI when compared to the GraftMaster group (32.7% vs. 15.7%, p = 0.04). There were no differences in any of the remaining selected indices (Table 2).

Table 2.
Coronary angiography and culprit lesion characteristics.
3.3. Procedural Indices
Lesion predilatation was more frequently performed in the GraftMaster compared to Papyrus group (26.5% vs. 5.5%, p = 0.003). The mean maximum pressure of non-CS stent deployment was significantly greater in the Papyrus group (p = 0.01), as well as balloon predilatation mean maximum pressure (p = 0.003). For patients receiving Papyrus CS, the mean stent graft length was greater compared to the GraftMaster group (p = 0.004) (Table 2).
3.4. Coronary Artery Perforation and Periprocedural Complications
There were no significant differences in the class of Ellis type perforation between the GraftMaster and Papyrus groups for class 1 (31.4% vs. 30.9%, p = 0.96), 2 (19.6% vs. 29.1%, p = 0.26), and 3 (49% vs. 40%, p = 0.35). Administration of protamine sulphate was more frequent in the Papyrus group when compared to GraftMaster (30.9% vs. 2%, p < 0.001). Cardiac tamponade occurred in 44 patients (41.5%) at a significantly higher frequently than in the GraftMaster group when compared to the Papyrus group (52.9% vs. 30.9%, p = 0.02) (Table 3).

Table 3.
Characterisation of coronary artery perforation, periprocedural complications, and their treatment.
3.5. Clinical Endpoints and Follow-Up
Considering the number of patients during follow-up, fifteen patients died up to a year (cardiac death from day 0 to day 358), 18 were followed up to a year (less than day 365, day 21 to day 350). This can be seen in the KM charts, because on day 365, 73 patients are at risk.
No statistically significant differences were found between the GraftMaster and Papyrus groups in the occurrence of re-PCI, cardiac death, myocardial infarction or MACE during the 30-day follow-up. Papyrus CS implantation resulted in a significantly lower incidence of TVR and TLR, when compared to GraftMaster CS (Table 4).

Table 4.
Follow-up data according to the stent graft type within 30 and 365 days.
At the 1-year follow-up, there were no statistically significant differences between GraftMaster and Papyrus CSs in the prevalence of MACE or re-PCI, with a trend towards lower rates of TLR, TVR, MI and ST in Papyrus CS. A trend towards a lower rate of cardiac death was observed in the group managed by GraftMaster stent implantation (Table 4). We observed a trend towards a lower overall ST rate in the Papyrus group compared to the GraftMaster group during the 1-year follow-up period (9.8% vs. 1.8%, p = 0.08; Table 4). Kaplan–Meier estimates for the selected clinical endpoints with the follow-up at 30-days and 1-year are presented in Figure 1A–E.
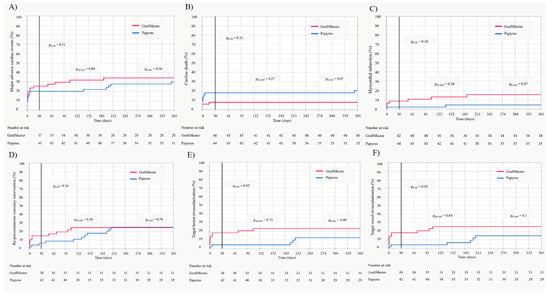
Figure 1.
Kaplan–Meier estimates with the follow-up at 30 days and 1 year. (A) Major adverse cardiac events (MACE); (B) cardiac death; (C) myocardial infarction; (D) recurrent percutaneous coronary intervention (re-PCI); (E) target vessel revascularisation (TVR); (F) target lesion revascularisation (TLR).
3.6. Predictors of Clinical Outcomes
A number of significant predictors of 1-year MACE were confirmed by multivariable analysis (with adjustment for age, sex and BMI): chronic obstructive pulmonary disease, no-reflow phenomenon, treatment with GPIIb/IIIa inhibitor, periprocedural use of left ventricular assist device (IABP [intra-aortic balloon counter-pulsation], Maquet Cardiopulmonary AG, Rastatt, Germany; Impella, CP 5.0 L, Abiomed MA; extracorporeal circulation), pericardiocentesis and stent graft length (Figure 2A). Among significant predictors of cardiac death, the following were found: atrial fibrillation, CAP type 3, no-reflow phenomenon, TIMI flow grade 0 after PCI, periprocedural use of left ventricular assist device, pericardiocentesis, cardiogenic shock, and periprocedural cardiac arrest (Figure 2B). The occurrence of myocardial infarction during the follow-up period was significantly influenced by smoking, cardiac arrest prior to PCI and CAP type 3 (Figure 2C). Predictors of re-PCI included: ACC/AHA lesion type B/C, non-CS implantation to seal the rupture and total length of non-CS stent (Figure 3A). Among predictors of TVR, the following were confirmed: chronic obstructive pulmonary disease, ST-segment elevation myocardial infarction (STEMI), ACC/AHA lesion type B/C, total length of non-CS stent and stent graft number (Figure 3B). Predictors of TLR included STEMI, non-CS implantation to seal rupture, and total length of non-CS stent (Figure 3C).
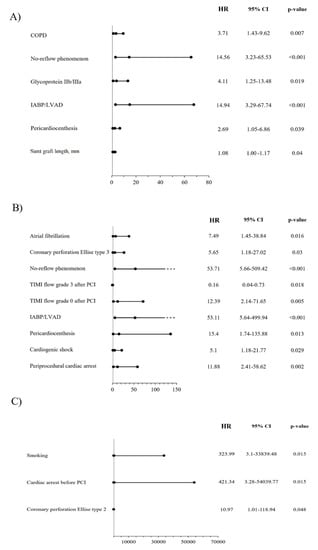
Figure 2.
Predictors of selected clinical outcomes assessed by multivariable analysis-models adjusted for age, sex and BMI; (A) major adverse cardiac events (MACE); COPD, chronic obstructive pulmonary disease; IABP, intra-aortic balloon pump counter-pulsation; LVAD, left ventricle assist device. (B) Cardiac death; IABP, intra-aortic balloon pump counter-pulsation; LVAD, left ventricle assist device; PCI, percutaneous coronary intervention; TIMI, thrombolysis in myocardial infarction. (C) Myocardial infarction; PCI, percutaneous coronary intervention.
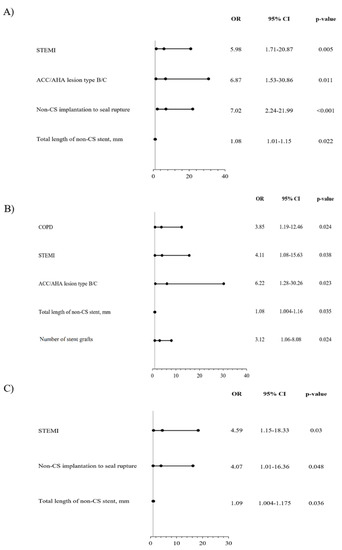
Figure 3.
Predictors of selected clinical outcomes assessed by multivariable analysis-models adjusted for age, sex and BMI; (A) recurrent percutaneous coronary intervention (re-PCI); ACC/AHA, American College of Cardiology/American Heart Association; CS, covered stent; STEMI, ST-segment elevation myocardial infarction. (B) Target vessel revascularisation (TVR); ACC/AHA, American College of Cardiology/American Heart Association; CS, covered stent; COPD, chronic obstructive pulmonary disease, ST- segment elevation myocardial infarction. (C) Target lesion revascularisation (TLR); CS, covered stent; STEMI, ST- segment elevation myocardial infarction.
4. Discussion
The main findings of the presented CRACK-II registry analysis are that: (1) Papyrus CS implantation resulted in a lower 30-day incidence of TVR and TLR when compared to GraftMaster CS; the early occurrence of re-PCI, cardiac death, MI and MACE remained indifferent between the compared groups; (2) at the 1-year follow-up, Papyrus and GraftMaster CSs implantation resulted in a similar prevalence of MACE and re-PCI, with a trend towards lower rate TLR, TVR, MI, and ST rates with the use of Papyrus, and a trend towards a lower rate of cardiac death with GraftMaster CS implantation.
The results of our analysis allowed demonstrating a difference in the prevalence of clinical events between the compared covered stents, both over short- and long-term observation periods. The covered stents did not differ in implantation technique, but in their technical design from which the difference in the prevalence of clinical events may have originated.
The PTFE-covered stent construction predisposes to increased neointimal hyperplasia and subsequent delayed endothelization at the proximal and distal edges, resulting in a magnified risk of in-stent restenosis [15,16,17,18]. In the previous reports, in-stent restenosis was a prevalent complication in patients treated with CS implantation, reaching 31.6% of interventional cases observed at a mean follow-up of 159 ± 49 days, with the edge in-stent restenosis constituting 29.8% out of those cases [15]. In our registry, the significant benefit of Papyrus CS over GraftMaster on TLR and TVR was present over a short-term observation and was no longer maintained during a long-term follow-up, whilst we observed only a trend for this difference. This interventional benefit did not translate into a reduced risk of recurrent PCI or MACE with Papyrus CS, showing that both stents were equally effective with the management of coronary artery perforations and asserted completion of the index procedure. Importantly, based on our previous data, the non-CS implantation to seal the rupture was found to be a predictor of increased re-PCI and TLR rates [11], while in previously published studies, it was suggested that among techniques used for the lower rate of ST and in-stent restenosis, non-CS stent (DES) implantation on the edge of CS could be implemented [19]. In the current study, localisation of non-CS was not aimed at covering the CS edge and it was carried out prior to CS implantation; therefore, it could not be found as deliberate CS stent protection against in-stent restenosis.
In previous studies, it has been demonstrated that equine pericardium-covered stent implantation resulted in a lower rate of ST over the course of treatment compared to PTFE and polyurethane-covered devices [9]. The stents used in the current registry were constructed with electrospun polyurethane-covered cobalt-chromium (Papyrus) and expanded polytetrafluoroethylene (ePTFE, GraftMaster). Literature data are not available for comparisons of treatment outcomes between Papyrus and GraftMaster stents. The current work is the first attempt at such a comparison. Harnek et al. evaluated treatment effects between implanted CSs, but the results did not allow an objective comparison of Papyrus and GraftMaster, as the author focuses mainly on the comparison with equine pericardium-covered stents [9]. Although the groups of patients were larger compared to the study presented by our team (199 GraftMaster and 74 Papyrus CS), the follow-up periods differed in length, which impaired proper interpretation of the results [9]. Nevertheless, from the presented graphs it can be concluded that the mortality rate was higher in the Papyrus group, and the ISR frequency was more prevalent in the GraftMaster group. Taking into account the difference in outcomes between the two assessed stents, the aetiology should be initially sought in the structure of the stent and effect on the endothelialisation rate [8]. While the prevalence of subacute ST in patients after GraftMaster implantation varied in previous studies between 5.7% at 5 months [15] and 3.6% at the 9-month follow-up [19], in our study, lower rates of subacute in-CS ST have been demonstrated. At the same time, the length of dual-antiplatelet therapy was longer in the GraftMaster group when compared to the Papyrus CS, which, considering the difference between event rates, underlines its sub-effective ST management. We explored a number of other factors that could have influenced the ST in the presented study. The frequency of urgent blood transfusion, known for prothrombotic properties, did not differ between CS groups. The use of protamine sulphate also had no influence on the prevalence of ST, as it was significantly more often administered in the Papyrus when compared to the GraftMaster population. The length of CS is another factor potentially influencing the frequency of ST, while the length of the Papyrus stent was significantly greater when compared to the GraftMaster CS, which could potentially increase the rate of ST in Papyrus group, but not in GraftMaster one.
In this study, valuable insight was also provided on the predictors of clinical events in the analysed population. Factors determining angiographic PCI success (no-reflow phenomenon and post-PCI TIMI flow grade) and indicators of patients’ poor periprocedural condition (use of left ventricle support devices, cardiogenic shock, cardiac arrest, or pericardiocentesis) were identified as predictors of cardiac death. The higher rate of cardiac death with Papyrus when compared to GraftMaster CS could result from clinical state of patients treated with CS at baseline. This reflects the significantly greater rate of NSTEMI patients and a trend towards a lower percentage of patients with stable angina in the Papyrus compared to the GraftMaster group. Although CAP 3 type and atrial fibrillation were found to be significant predictors of increased death rate in the current analysis, initially, both analysed groups differed statistically significantly only in the case of atrial fibrillation. The greater proportion of patients with atrial fibrillation at baseline in the Papyrus group may be associated with more frequent use of anticoagulation and a greater risk of periprocedural bleeding complications when compared to the GraftMaster one. Smoking and cardiac arrest before PCI were the two greatest pre-procedural predictors of myocardial infarction at the 1-year follow-up, closely followed by procedural type 2 CAP (according to Ellis classification). While assessing revascularisation outcomes (re-PCI, TVR and TLR), their greater prevalence was predicted by lesion type according to the ACC/AHA classification and stent graft length, non-CS implantation to seal rupture and total length of non-CS, as well as STEMI presentation at baseline.
A number of MACE predictors were identified via multivariable analysis, including occurrence of the no-reflow phenomenon. In some patients, this could be related to greater inflation pressures during stent deployment or post-dilatation, which appears after squeezing of embolic material, mostly during post-dilatation, resulting in distal embolization, and is called the “toothpaste effect” [20]. Moreover, the periprocedural use of glycoprotein IIb/IIIa receptor inhibitors might be related to the no-reflow phenomenon and the following increased rate of MACE components during the follow-up period. Among other factors, indicators of patients’ poorer clinical states were calculated, such as left ventricle support devices or pericardiocentesis. Among the well-known factors of poorer clinical outcomes after PCI with stent implantation, the following was found: stent graft length, a relationship that has been previously demonstrated in several publications [21].
The topic of the modernity of CSs should also be discussed. There is no doubt that Papyrus CS was constructed in a modern way and belong to the group of new CSs, approved for use by the Food and Drug Administration for commercial use in the United States of America in 2018 [22]. Whereas, the GraftMaster CS was designed much earlier, and its sandwich structure dates back much earlier, and was known as Jostent, primarily, while the currently available stents have been approved for commercial use in 2017 by the Food and Drug Administration [23]. Therefore, it could be also considered in comparison different nomenclature: the early double-layer sandwich design GraftMaster versus new generation single layer Papyrus CSs. However, this is not entirely true, as the study covers the period in which the availability of stents was equal and still is, and the selection of stents was random, because as a rule, one catheterisation laboratory is not supplied with both CSs. The factors that determined the comparable consumption and availability of CSs were certainly price, frequency of use, or local preferences and habits.
In conclusion, this real-life registry of CAP illustrated that the use of Papyrus CS is associated with lower rates of TLR and TVR at 30-day follow-up in comparison to the GraftMaster CSs and no significant differences between both assessed CS at one year of follow-up.
Study Limitations
There are several limitations of this study. First, we had no data on intravascular imaging and, thus, the mechanism of recorded ST is unknown. Secondly, there was a lack of quantitative findings, such as reference vessel diameter or minimal lumen diameter, which would have allowed for stratified exploratory data analyses. There was also no central core laboratory or unified quantitative coronary angiography assessment by dedicated software. Moreover, we were not able to assess the extent of endothelialisation and its distribution in the target vessel after CS implantation at selected time points following the PCI. Due to the nature of CS implantation (urgent and salvage mode), a prospective analysis could not be performed. Moreover, among the limitations, are the small sample size, and probably the low number of events that could make it difficult to perform meaningful outcome analyses.
Author Contributions
Conceptualization, R.J. and W.W. (Wojciech Wańha); methodology, R.J., K.P., J.B. and M.K.; software, K.P.; validation, W.W. (Wojciech Wańha), R.J., S.B. and W.W. (Wojciech Wojakowski); formal analysis, R.J., J.B., W.W. (Wojciech Wańha) and K.P.; investigation, R.J., J.B., D.H., M.K., Ł.K., M.T., T.F., T.P., M.G.-K., M.S.-N., A.S., B.T., A.W., J.K., M.J., S.D., A.O., M.G., W.W. (Wojciech Wojakowski), K.R., and W.W. (Wojciech Wańha).; resources, R.J. and W.W. (Wojciech Wańha); data curation, R.J. and W.W. (Wojciech Wańha); writing—original draft preparation, R.J. and J.B.; writing—review and editing, R.J., W.W. (Wojciech Wańha) and M.K.; visualization, R.J. and K.P.; supervision, R.J. and W.W. (Wojciech Wańha); project administration, R.J. and W.W. (Wojciech Wańha); funding acquisition, R.J. All authors have read and agreed to the published version of the manuscript.
Funding
Publication financed by the Ministry of Science and Higher Education in the form of a grant awarded to R.J. (022/RID/2018/19). This was part of a program under the Ministry of Science and Higher Education called ’Regional Initiative of Excellence’ in 2019–2022.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of the Medical University of Silesia in 2020.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Possible disclosure of data is available on personal requests.
Acknowledgments
The Scientific Platform of the “Club 30” of the Polish Cardiac Society initiated the CRACK Registry.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Shimony, A.; Joseph, L.; Mottillo, S.; Eisenberg, M.J. Coronary artery perforation during percutaneous coronary intervention: A systematic review and meta-analysis. Can. J. Cardiol. 2011, 27, 843–850. [Google Scholar] [CrossRef]
- Januszek, R.; Bryniarski, L.; Siudak, Z.; Malinowski, K.P.; Bryniarski, K.L.; Surdacki, A.; Dziewierz, A.; Mika, P.; Wańha, W.; Wojakowski, W.; et al. Five-year report from the Polish national registry on percutaneous coronary interventions with a focus on coronary artery perforations within chronic total occlusions. Postepy Kardiol. Interwencyjnej 2020, 16, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Tajti, P.; Burke, M.N.; Karmpaliotis, D.; Alaswad, K.; Werner, G.S.; Azzalini, L.; Carlino, M.; Patel, M.; Mashayekhi, K.; Egred, M.; et al. Update in the Percutaneous Management of Coronary Chronic Total Occlusions. JACC Cardiovasc. Interv. 2018, 11, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Danek, B.A.; Karatasakis, A.; Tajti, P.; Sandoval, Y.; Karmpaliotis, D.; Alaswad, K.; Jaffer, F.; Yeh, R.W.; Kandzari, D.E.; Lembo, N.J.; et al. Incidence, Treatment, and Outcomes of Coronary Perforation during Chronic Total Occlusion Percutaneous Coronary Intervention. Am. J. Cardiol. 2017, 120, 1285–1292. [Google Scholar] [CrossRef] [PubMed]
- Ellis, S.G.; Ajluni, S.; Arnold, A.Z.; Popma, J.J.; Bittl, J.A.; Eigler, N.L.; Cowley, M.J.; Raymond, R.E.; Safian, R.D.; Whitlow, P.L. Increased coronary perforation in the new device era. Incidence, classification, management, and outcome. Circulation 1994, 90, 2725–2730. [Google Scholar] [CrossRef] [PubMed]
- Lemmert, M.E.; van Bommel, R.J.; Diletti, R.; Wilschut, J.M.; de Jaegere, P.P.; Zijlstra, F.; Daemen, J.; Van Mieghem, N.M. Clinical Characteristics and Management of Coronary Artery Perforations: A Single-Center 11-Year Experience and Practical Overview. J. Am. Heart Assoc. 2017, 6, e007049. [Google Scholar] [CrossRef] [PubMed]
- Kilic, I.D.; Fabris, E.; Serdoz, R.; Caiazzo, G.; Foin, N.; Abou-Sherif, S.; Di Mario, C. Coronary covered stents. EuroIntervention 2016, 12, 1288–1295. [Google Scholar] [CrossRef] [PubMed]
- Takano, M.; Yamamoto, M.; Inami, S.; Xie, Y.; Murakami, D.; Okamatsu, K.; Ohba, T.; Seino, Y.; Mizuno, K. Delayed endothelialization after polytetrafluoroethylene-covered stent implantation for coronary aneurysm. Circ. J. 2009, 73, 190–193. [Google Scholar] [CrossRef]
- Harnek, J.; James, S.K.; Lagerqvist, B. Very long-term outcome of coronary covered stents: A report from the SCAAR registry. EuroIntervention 2019, 14, 1660–1667. [Google Scholar] [CrossRef]
- Schächinger, V.; Hamm, C.W.; Münzel, T.; Haude, M.; Baldus, S.; Grube, E.; Bonzel, T.; Konorza, T.; Köster, R.; Arnold, R.; et al. A randomized trial of polytetrafluoroethylene-membrane-covered stents compared with conventional stents in aortocoronary saphenous vein grafts. J. Am. Coll. Cardiol. 2003, 42, 1360–1369. [Google Scholar] [CrossRef]
- Wańha, W.; Januszek, R.; Kołodziejczak, M.; Gilis-Malinowska, N.; Figatowski, T.; Milewski, M.; Pawlik, A.; Staszczak, B.; Wybraniec, M.; Tomasiewicz, B.; et al. Procedural and 1-year outcomes following large vessel coronary artery perforation treated by covered stents implantation: Multicentre CRACK registry. PLoS ONE 2021, 16, e0249698. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef] [PubMed]
- Ryan, T.J.; Faxon, D.P.; Gunnar, R.M.; Kennedy, J.W.; King, S.B., 3rd; Loop, F.D.; Peterson, K.L.; Reeves, T.J.; Williams, D.O.; Winters, W.L., Jr.; et al. Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty). Circulation 1988, 78, 486–502. [Google Scholar] [PubMed]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; Steg, P.G.; Morel, M.A.; Mauri, L.; Vranckx, P.; et al. Clinical end points in coronary stent trials: A case for standardized definitions. Circulation 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Gercken, U.; Lansky, A.J.; Buellesfeld, L.; Desai, K.; Badereldin, M.; Mueller, R.; Selbach, G.; Leon, M.B.; Grube, E. Results of the Jostent coronary stent graft implantation in various clinical settings: Procedural and follow-up results. Catheter. Cardiovasc. Interv. 2002, 56, 353–360. [Google Scholar] [CrossRef]
- Kimura, T.; Itoh, T.; Sugawara, S.; Fusazaki, T.; Nakamura, M.; Morino, Y. Serial endovascular assessment of polytetrafluoroethylene-covered stent: Capabilities and limitations of intravascular imaging modalities affected by a temporal factor. J. Cardiol. Cases 2014, 11, 91–95. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lukito, G.; Vandergoten, P.; Jaspers, L.; Dendale, P.; Benit, E. Six months clinical, angiographic, and IVUS follow-up after PTFE graft stent implantation in native coronary arteries. Acta Cardiol. 2000, 55, 255–260. [Google Scholar] [CrossRef]
- Araki, M.; Hikita, H.; Sudo, Y.; Hishikari, K.; Takahashi, A. Restenosis of a Polytetrafluoroethylene-Covered Stent Visualized by Coronary Angioscopy and Optical Coherence Tomography: A Case Report. Int. J. Angiol. 2020, 29, 58–62. [Google Scholar] [CrossRef] [PubMed]
- Papafaklis, M.I.; Sianos, G.; Cost, B.; Vaina, S.; Manginas, A.; Dardas, P.S.; Tsikaderis, D.; van Mieghem, C.A.; Michalis, L.K.; Serruys, P.W. Clinical and angiographic follow-up after overlapping implantation of polytetrafluoroethylene covered stents with drug eluting stents. EuroIntervention 2006, 2, 218–223. [Google Scholar] [PubMed]
- Stone, G.W.; Goldberg, S.; O’Shaughnessy, C.; Midei, M.; Siegel, R.M.; Cristea, E.; Dangas, G.; Lansky, A.J.; Mehran, R. 5-year follow-up of polytetrafluoroethylene-covered stents compared with bare-metal stents in aortocoronary saphenous vein grafts the randomized BARRICADE (barrier approach to restenosis: Restrict intima to curtail adverse events) trial. JACC Cardiovasc. Interv. 2011, 4, 300–309. [Google Scholar] [CrossRef]
- Tcheng, J.E.; Lim, I.H.; Srinivasan, S.; Jozic, J.; Gibson, C.M.; O’Shea, J.C.; Puma, J.A.; Simon, D.I. Stent parameters predict major adverse clinical events and the response to platelet glycoprotein IIb/IIIa blockade: Findings of the ESPRIT trial. Circ. Cardiovasc. Interv. 2009, 2, 43–51. [Google Scholar] [CrossRef] [PubMed][Green Version]
- PK Papyrus Covered Coronary Stent System. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfhde/hde.cfm?id=H170004 (accessed on 18 November 2021).
- GRAFT MASTER RX CORONARY STENT GRAFT SYSTM. Available online: https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfhde/hde.cfm?id=396156 (accessed on 18 November 2021).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).