Is There a Correlation between Multiparametric Assessment in Ultrasound and Intrinsic Subtype of Breast Cancer?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
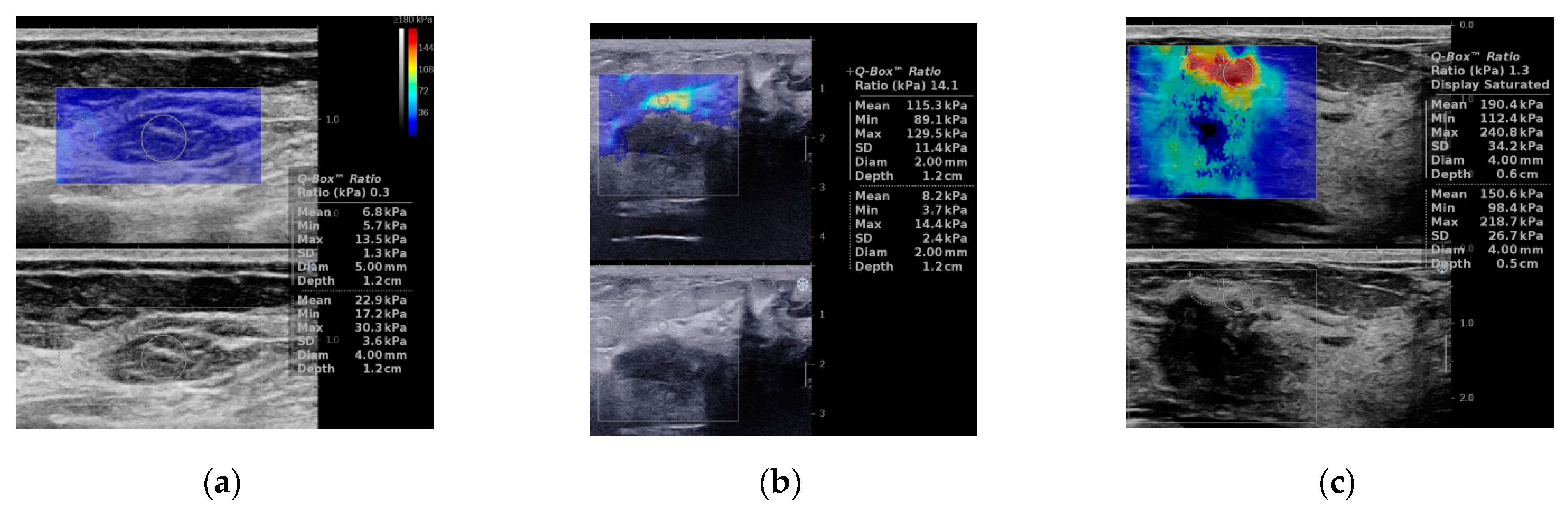
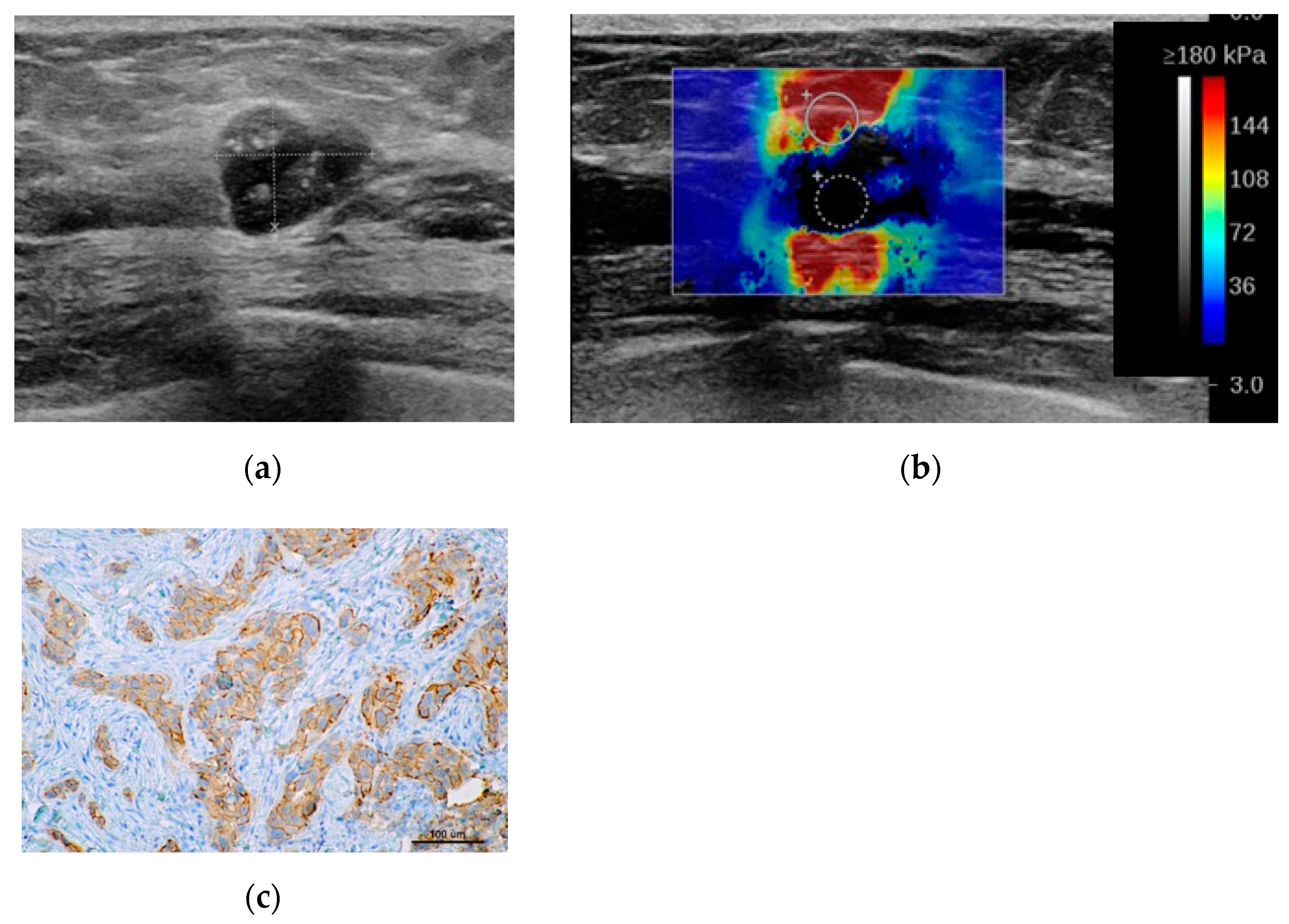
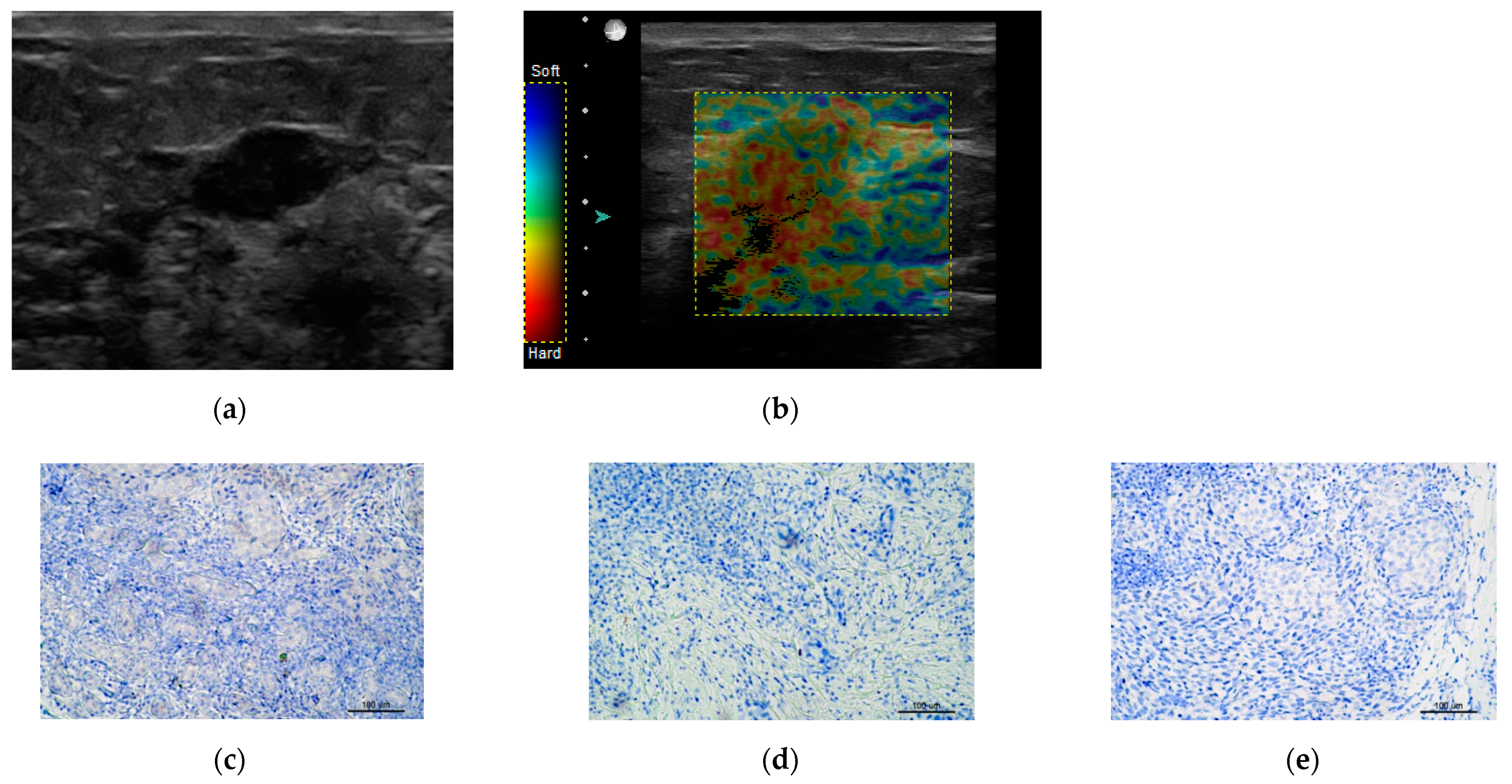
2.2. Sonoelastography
- Soft (incorporate: Tsukuba1,Tsukuba2, E max < 80 kPa)
- Intermediate (incorporate: Tsukuba3, E max > 80 kPa < 160 kPa)
- Hard (incorporate: Tsukuba 4,Tsukuba5, E max > 160 kPa)
2.3. Histopathological Verification
2.4. Statistical Analysis
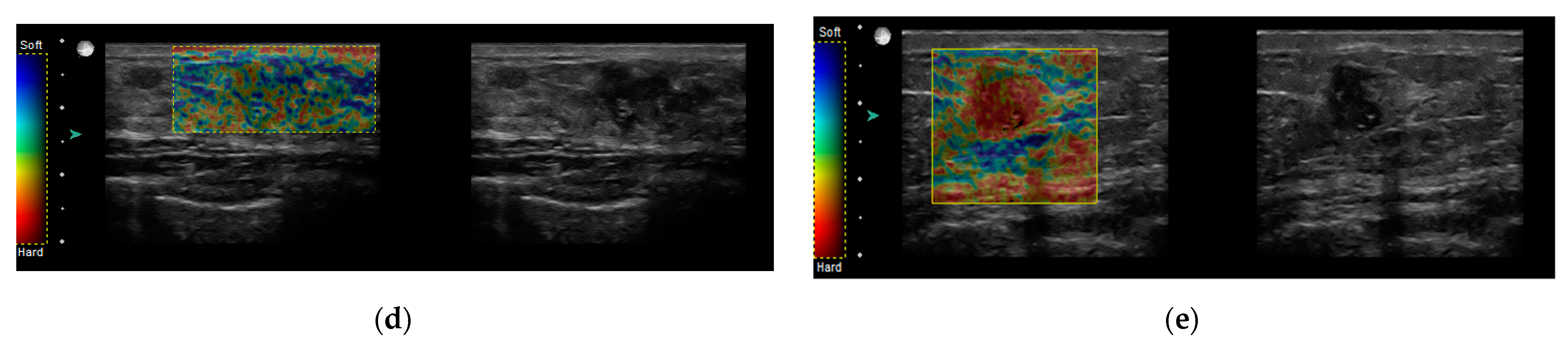
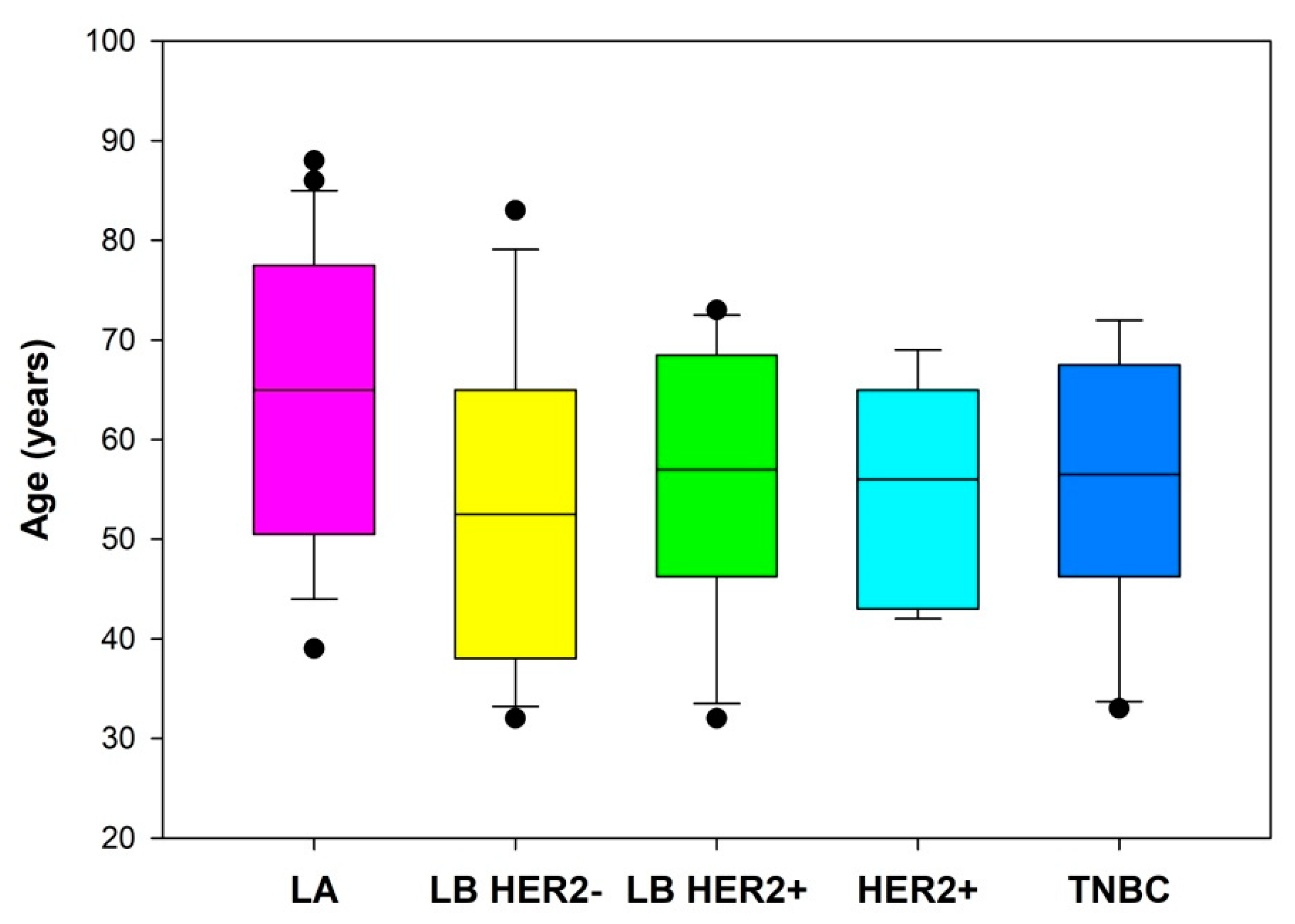
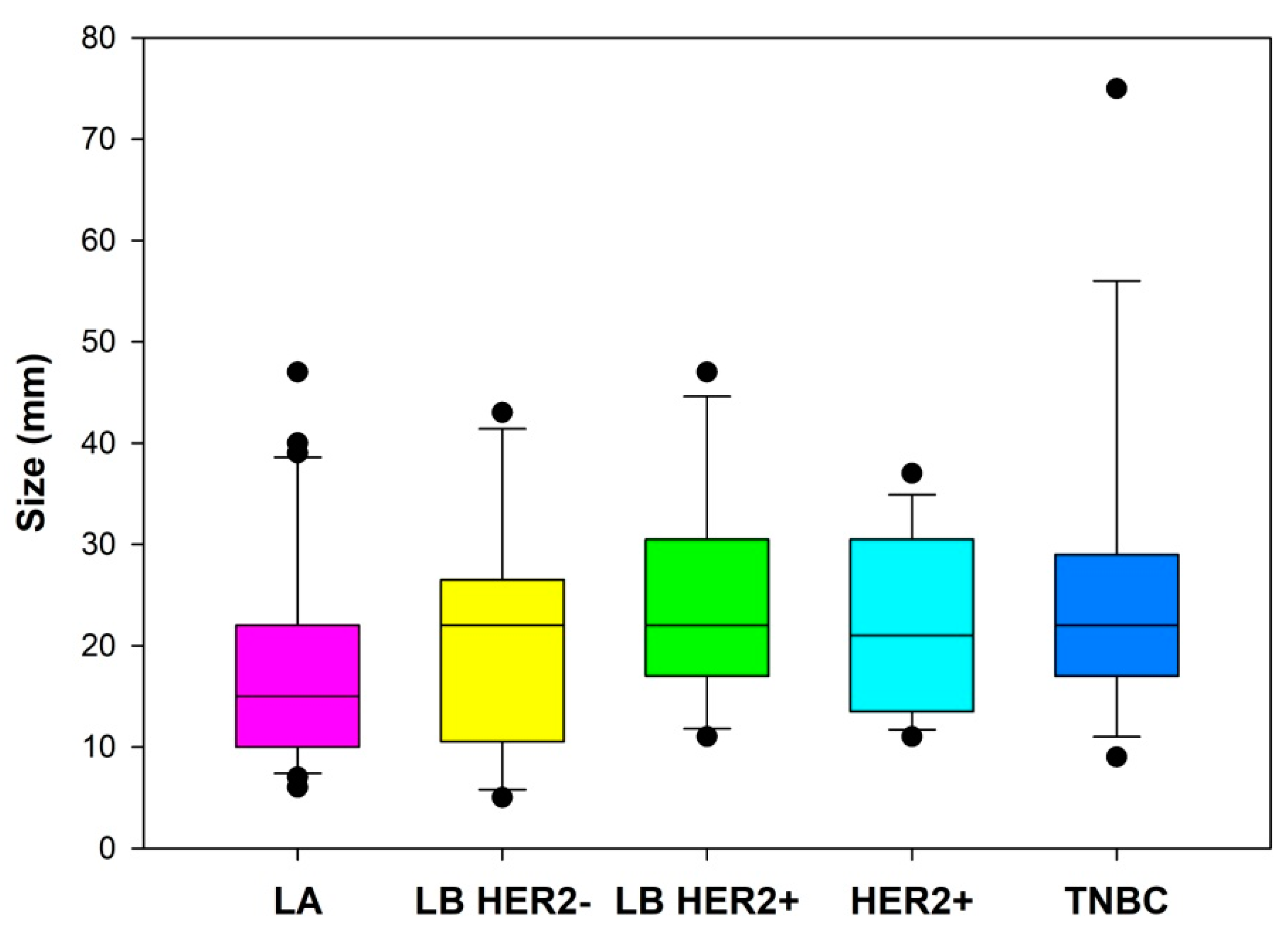
3. Results
- Aggressive subtypes, including: LB HER2+, HER2+ and TNBC
- Luminal, including subtypes: LA and LB HER2−
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Jassem, J.; Krzakowski, M.; Bobek-Billewicz, B.; Duchnowska, R.; Jeziorski, A.; Olszewski, W.; Senkus-Konefka, E.; Tchórzewska-Korba, H.; Wysocki, P. Rak piersi. Onkol. Prakt. Klin. Edu. 2020, 6, 297–352. [Google Scholar]
- Taneja, S.; Evans, A.J.; Rakha, E.A.; Green, A.R.; Ball, G.; Ellis, I.O. The mammographic correlations of a new immunohistochemical classification of invasive breast cancer. Clin. Radiol. 2008, 63, 1228–1235. [Google Scholar] [CrossRef]
- Sohn, Y.-M.; Han, K.; Seo, M. Immunohistochemical Subtypes of Breast Cancer: Correlation with Clinicopathological and Radiological Factors. Iran. J. Radiol. 2016, 13, e31386. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dilorenzo, G.; Telegrafo, M.; la Forgia, D.; Stabile Ianora, A.A.; Moschetta, M. Breast MRI background parenchymal enhancement as an imaging bridge to molecular cancer sub-type. Eur. J. Radiol. 2019, 113, 148–152. [Google Scholar] [CrossRef]
- Montemezzi, S.; Camera, L.; Giri, M.G.; Pozzetto, A.; Caliò, A.; Meliadò, G.; Caumo, F.; Cavedon, C. Is there a correlation between 3T multiparametric MRI and molecular subtypes of breast cancer? Eur. J. Radiol. 2018, 108, 120–127. [Google Scholar] [CrossRef]
- Mango, V.; Rahbar, H.; Friedlander, L.; Nguyen, D.; Ha, R. Breast Malignancy. In Breast MRI Teaching Atlas; Springer: New York, NY, USA, 2017; pp. 99–238. [Google Scholar] [CrossRef]
- Yang, Q.; Liu, H.-Y.; Liu, D.; Song, Y.-Q. Ultrasonographic Features of Triple-Negative Breast Cancer: A Comparison with Other Breast Cancer Subtypes. Asian Pac. J. Cancer Prev. 2015, 16, 3229–3232. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Tian, J.; Wang, X.; Wang, Y.; Wang, Z.; Zhang, L.; Jing, H.; Wu, T. Differences in Multi-Modal Ultrasound Imaging between Triple Negative and Non-Triple Negative Breast Cancer. Ultrasound Med. Biol. 2016, 42, 882–890. [Google Scholar] [CrossRef]
- Li, J.; Zhang, K.; Shi, Z.; Zhang, X.; Xie, J.; Liu, J.; Chang, C. Triple-negative invasive breast carcinoma: The association between the sonographic appearances with clinicopathological feature. Sci. Rep. 2018, 8, 9040. [Google Scholar] [CrossRef]
- Liu, H.; Wan, J.; Xu, G.; Xiang, L.-H.; Fang, Y.; Ding, S.-S.; Jiang, X.; Sun, L.-P.; Zhang, Y.-F. Conventional US and 2-D Shear Wave Elastography of Virtual Touch Tissue Imaging Quantification: Correlation with Immunohistochemical Subtypes of Breast Cancer. Ultrasound Med. Biol. 2019, 45, 2612–2622. [Google Scholar] [CrossRef]
- Evans, A.; Sim, Y.T.; Thomson, K.; Jordan, L.; Purdie, C.; Vinnicombe, S.J. Shear wave elastography of breast cancer: Sensitivity according to histological type in a large cohort. Breast 2016, 26, 115–118. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Li, J.; Xiao, Y.; Cui, H.; Du, G.; Wang, Y.; Li, Z.; Wu, T.; Li, X.; Tian, J. Identifying ultrasound and clinical features of breast cancer molecular subtypes by ensemble decision. Sci. Rep. 2015, 5, 11085. [Google Scholar] [CrossRef]
- Mendelson, E.B.; Böhm-Vélez, M.; Berg, W.A.; Whitman, G.J.; Feldman, M.I.; Madjar, H.; Rizzatto, G.; Baker, J.A.; Zuley, M.; Stavros, A.T.; et al. ACR BI-RADS® Ultrasound. In ACR BI-RADS® Atlas, Breast Imaging Reporting and Data System; American College of Radiology: Reston, VA, USA, 2013. [Google Scholar]
- Jakubowski, W.; Dobruch-Sobczak, K.; Migda, B. Standards of the Polish Ultrasound Society—Update. Sonomammography examination. J. Ultrason. 2012, 12, 245–261. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Săftoiu, A.; Gilja, O.H.; Sidhu, P.S.; Dietrich, C.F.; Cantisani, V.; Amy, D.; Bachmann-Nielsen, M.; Bob, F.; Bojunga, J.; Brock, M.; et al. The EFSUMB Guidelines and Recommendations for the Clinical Practice of Elastography in Non-Hepatic Applications: Update 2018. Ultraschall Med. 2019, 40, 425–453. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barr, R.G.; Nakashima, K.; Amy, D.; Cosgrove, D.; Farrokh, A.; Schafer, F.; Bamber, J.C.; Castera, L.; Choi, B.I.; Chou, Y.H.; et al. WFUMB guidelines and recommendations for clinical use of ultrasound elastography: Part 2: Breast. Ultrasound Med. Biol. 2015, 41, 1148–1160. [Google Scholar] [CrossRef] [Green Version]
- Allred, D.; Harvey, J.; Berardo, M.; Clark, G. Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod. Pathol. 1998, 11, 155–168. [Google Scholar]
- Prat, A.; Pineda, E.; Adamo, B.; Galván, P.; Fernández, A.; Gaba, L.; Díez, M.; Viladot, M.; Arance, A.; Muñoz, M. Clinical implications of the intrinsic molecular subtypes of breast cancer. Breast 2015, 24, 26–35. [Google Scholar] [CrossRef] [Green Version]
- Criscitiello, C.; Azim, H.A.; Schouten, P.C.; Linn, S.C.; Sotiriou, C. Understanding the biology of triple-negative breast cancer. Ann. Oncol. 2012, 23, 13–18. [Google Scholar] [CrossRef]
- Morigi, C. Highlights from the 15th St Gallen International Breast Cancer Conference 15–18 March, 2017, Vienna: Tailored treatments for patients with early breast cancer. Ecancer 2017, 11, 732. [Google Scholar] [CrossRef] [Green Version]
- Li, Y.; Yang, D.; Chen, P.; Yin, X.; Sun, J.; Li, H.; Ren, G. Efficacy and safety of neoadjuvant chemotherapy regimens for triple-negative breast cancer: A network meta-analysis. Aging 2019, 11, 6286–6311. [Google Scholar] [CrossRef]
- Chaudhary, L.N.; Wilkinson, K.H.; Kong, A. Triple-Negative Breast Cancer. Surg. Oncol. Clin. N. Am. 2018, 27, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Dogan, B.E.; Gonzalez-Angulo, A.M.; Gilcrease, M.; Dryden, M.J.; Yang, W.T. Multimodality Imaging of Triple Receptor–Negative Tumors with Mammography, Ultrasound, and MRI. Am. J. Roentgenol. 2010, 194, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Raza, S.; Goldkamp, A.L.; Chikarmane, S.A.; Birdwell, R.L. US of breast masses categorized as BI-RADS 3, 4, and 5: Pictorial review of factors influencing clinical management. Radiographics 2010, 30, 1199–1213. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ko, E.S.; Lee, B.H.; Kim, H.-A.; Noh, W.-C.; Kim, M.S.; Lee, S.-A. Triple-negative breast cancer: Correlation between imaging and pathological findings. Eur. Radiol. 2010, 20, 1111–1117. [Google Scholar] [CrossRef]
- Elias, S.G.; Adams, A.; Wisner, D.J.; Esserman, L.J.; van’t Veer, L.J.; Mali, W.P.T.M.; Gilhuijs, K.G.A.; Hylton, N.M. Imaging Features of HER2 Overexpression in Breast Cancer: A Systematic Review and Meta-analysis. Cancer Epidemiol. Biomark. Prev. 2014, 23, 1–24. [Google Scholar] [CrossRef] [Green Version]
- Yoo, J.; Seo, B.K.; Park, E.K.; Kwon, M.; Jeong, H.; Cho, K.R.; Woo, O.H.; Song, S.E.; Cha, J. Tumor stiffness measured by shear wave elastography correlates with tumor hypoxia as well as histologic biomarkers in breast cancer. Cancer Imaging 2020, 20, 85. [Google Scholar] [CrossRef] [PubMed]
| MMG | |
| US |
|
| MR |
| Shape | Oval |
| Round | |
| Irregular | |
| Orientation | Parallel |
| Non-parallel | |
| Margin | Circumscribed |
| Non-circumscribed | |
| Indistinct | |
| Micro/macrolobulated | |
| Angular | |
| Spiculated | |
| Echo pattern | Anechoic |
| Hyperechoic | |
| Complex cystic and solid | |
| Hypoechoic | |
| Isoechoic | |
| Heterogeneous | |
| Postrior features | No posterior features |
| Enhancement | |
| Shadowing | |
| Combined pattern | |
| Calcifications | Absent |
| In a mass | |
| Outside of a mass | |
| Intraductal | |
| Hyperechogenic foci | |
| Skin | Normal |
| Thickening > 2 mm | |
| Edema | Absent |
| Present | |
| Vascularity | Absent |
| Internal | |
| Vessels in a rim | |
| Outside of a mass | |
| Elastography | Soft < 80 kPa |
| Intermediate 80–160 kPa | |
| Hard > 160 kPa |
| LA | ER+ and PR ≥ 20% HER2− Ki-67 < 20% | |
| LB | LB HER2− | LB HER2+ |
| HER2− ER+ and any of the following: Ki-67 ≥ 20% and/or PR− or <20% | HER2+ ER+ Any Ki-67 and PR | |
| HER2+ | ER and PR- HER2+ | |
| Basal-like (TNBC) | ER and PR− HER2− | |
| Special Types | ER+ (cribriform, tubular, mucous) ER− (apocrine, medullary, adenoid cystic carcinoma, metaplastic) | |
| LA | LB HER2− | LB HER2+ | HER2+ | TNBC | ||
|---|---|---|---|---|---|---|
| Shape | ||||||
| Oval | 0/33 (0%) | 0/17 (0%) | 0/17 (0%) | 1/16 (6%) | 0/19 (0%) | |
| Round | 2/33 (6%) | 0/17 (0%) | 0/17 (0%) | 0/16 (0%) | 0/19 (0%) | |
| Irregular | 31/33 (94%) | 17/17 (100%) | 17/17 (100%) | 15/16 (94%) | 19/19 (100%) | |
| Orientation | ||||||
| Parallel | 25/33 (76%) | 16/17 (94%) | 16/17 (94%) | 15/16 (94%) | 15/19 (79%) | |
| Non-parallel | 8/33 (24%) | 1/17 (6%) | 1/17 (6%) | 1/16 (6%) | 4/19 (21%) | |
| Margin | ||||||
| Circumscribed | 0/33 (0%) | 0/17 (0%) | 0/17 (0%) | 2/16 (12.5%) | 0/19 (0%) | |
| Not circumscribed | Indistinct | 9/33 (27%) | 4/17 (24%) | 4/17 (24%) | 2/16 (12.5%) | 8/19 (42%) |
| Angular/ spiculated | 21/33 (64%) | 13/17 (76%) | 11/17 (64%) | 10/16 (62.5%) | 9/19 (47%) | |
| Micro/ macrolobulated | 3/33 (9%) | 0/17 (0%) | 2/17 (12%) | 2/16 (12.5%) | 2/19 (11%) | |
| Echo pattern | ||||||
| Complex/hypoechoic | 29/33 (88%) | 16/17 (94%) | 16/17 (94%) | 14/16 (87,5%) | 19/19 (100%) | |
| Hyper/isoechoic | 4/33 (12%) | 1/17 (6%) | 1/17 (6%) | 2/16 (12,5) | 0/19 (0%) | |
| Posterior features | ||||||
| No Posterior Features | 13/33 (39%) | 5/17 (29%) | 3/17 (18%) | 3/16 (19%) | 2/19 (11%) | |
| Enhancement | 0/33 (0%) | 1/17 (6%) | 3/17 (18%) | 6/16 (37.5%) | 4/19 (21%) | |
| Shadowing | 7/33 (22%) | 4/17 (23%) | 8/17 (47%) | 2/16 (12.5%) | 5/19 (26%) | |
| Combined Pattern | 13/33 (39%) | 7/17 (41%) | 3/17 (18%) | 5/16 (31%) | 8/19 (42%) | |
| Calcifications | ||||||
| Present | 13/33 (39%) | 12/17 (71%) | 13/17 (76.5%) | 12/16 (75%) | 4/19 (21%) | |
| Absent | 20/33 (61%) | 5/17 (29%) | 4/17 (23.5%) | 4/16 (25%) | 15/19 (79%) | |
| Additional features | ||||||
| Skin changes | 4/33 (12%) | 6/17 (35%) | 6/17 (35%) | 2/16 (12.5%) | 3/19 (16%) | |
| Edema | 24/33 (73%) | 10/17 (59%) | 12/17 (71%) | 9/16 (56%) | 14/19 (74%) | |
| Vascularity | 28/33 (85%) | 17/17 (100%) | 16/17 (94%) | 15/16 (94%) | 18/19 (95%) | |
| Elastography | ||||||
| Soft | 7/33 (21%) | 1/17 (6%) | 1/17 (6%) | 3/16 (19%) | 2/19 (10%) | |
| Intermediate | 12/33 (36%) | 5/17 (29%) | 6/17 (35%) | 2/16 (12%) | 10/19 (53%) | |
| Hard | 14/33 (42%) | 11/17 (65%) | 10/17 (59%) | 11/16 (69%) | 7/19 (37%) | |
| OR | p-Value | CI | |
|---|---|---|---|
| LA | 1.046 | 0.005 | 1.015–1.082 |
| LB HER2− | 0.975 | 0.1744 | 0.9375–1.0107 |
| LB HER2+ | 0.987 | 0.4653 | 0.9505–1.0228 |
| HER2+ | 0.988 | 0.516 | 0.9508–1.0249 |
| TNBC | 0.985 | 0.3866 | 0.9501–1.0193 |
| HER2+ vs. Other | OR | p-Value | CI |
|---|---|---|---|
| Shadowing | 0.639 | 0.6402 | 0.0786–4.1934 |
| Combined Pattern | 1.237 | 0.7856 | 0.2747–6.5233 |
| Enhancement | 5.750 | 0.0324 | 1.2257–32.8005 |
| Aggressive vs. Lum | OR | p-Value | CI |
|---|---|---|---|
| Shadowing | 3.068 | 0.0539 | 1.0043–9.9807 |
| Combined Pattern | 1.8 | 0.2776 | 0.6331–5.3802 |
| Enhancement | 29.250 | 0.0026 | 4.651–579.583 |
| HER2+ (HER2+ and LB HER2+) vs. Other | OR | p-Value | CI |
|---|---|---|---|
| Calcifications | 3.125 | 0.03 | 0.0917–5.87 |
| TNBC vs. Other | OR | p-Value | CI |
|---|---|---|---|
| Calcifications | 0.176 | 0.0041 | 0.0469–0.5335 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gumowska, M.; Mączewska, J.; Prostko, P.; Roszkowska-Purska, K.; Dobruch-Sobczak, K. Is There a Correlation between Multiparametric Assessment in Ultrasound and Intrinsic Subtype of Breast Cancer? J. Clin. Med. 2021, 10, 5394. https://doi.org/10.3390/jcm10225394
Gumowska M, Mączewska J, Prostko P, Roszkowska-Purska K, Dobruch-Sobczak K. Is There a Correlation between Multiparametric Assessment in Ultrasound and Intrinsic Subtype of Breast Cancer? Journal of Clinical Medicine. 2021; 10(22):5394. https://doi.org/10.3390/jcm10225394
Chicago/Turabian StyleGumowska, Magdalena, Joanna Mączewska, Piotr Prostko, Katarzyna Roszkowska-Purska, and Katarzyna Dobruch-Sobczak. 2021. "Is There a Correlation between Multiparametric Assessment in Ultrasound and Intrinsic Subtype of Breast Cancer?" Journal of Clinical Medicine 10, no. 22: 5394. https://doi.org/10.3390/jcm10225394
APA StyleGumowska, M., Mączewska, J., Prostko, P., Roszkowska-Purska, K., & Dobruch-Sobczak, K. (2021). Is There a Correlation between Multiparametric Assessment in Ultrasound and Intrinsic Subtype of Breast Cancer? Journal of Clinical Medicine, 10(22), 5394. https://doi.org/10.3390/jcm10225394






