Diabetes, Vascular Aging and Stroke: Old Dogs, New Tricks?
Abstract
1. Introduction
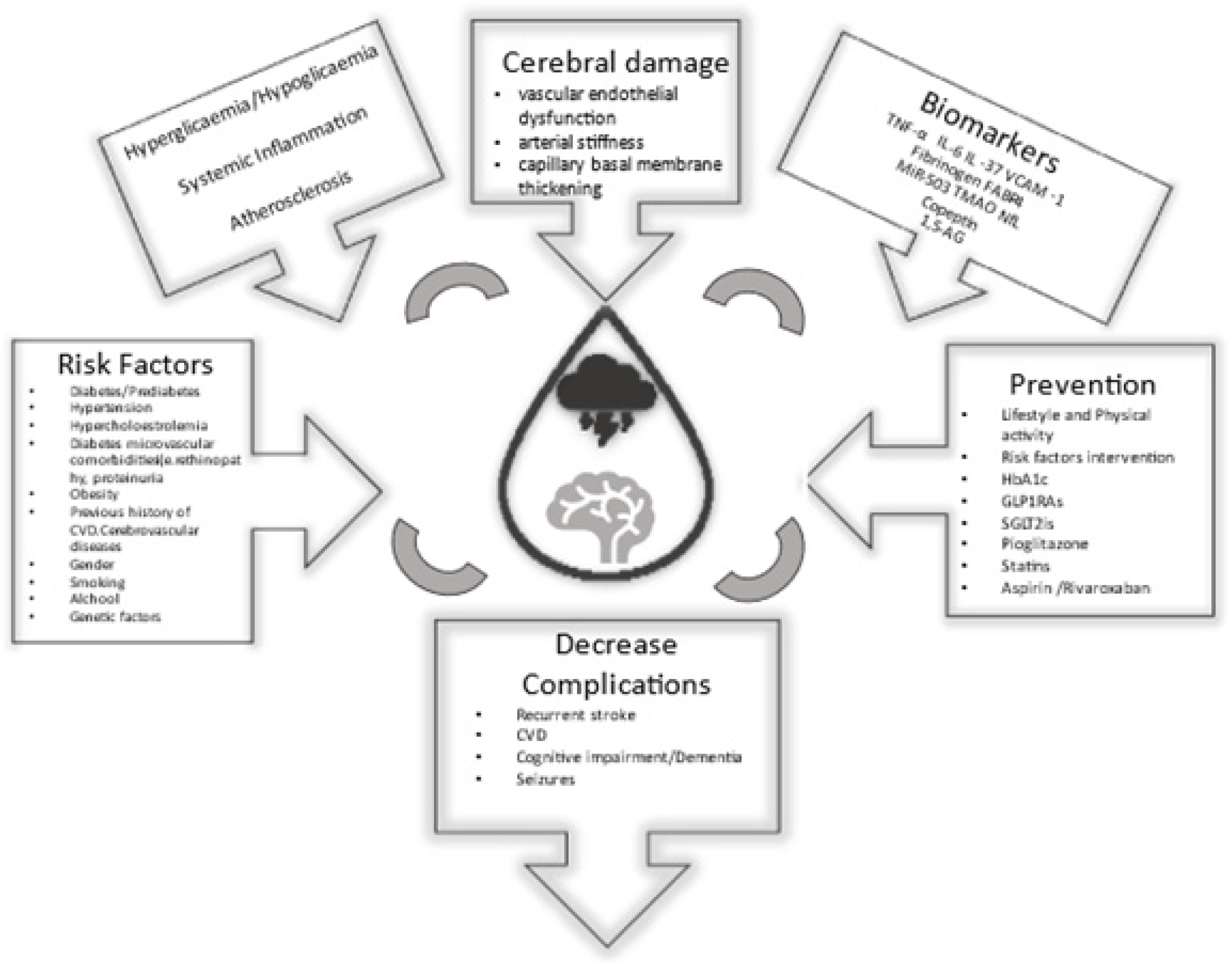
2. Epidemiology and Risk Factors
3. Clinical Manifestation
4. Pathophysiology
5. Management of Hyperglycaemia during Acute Stroke
6. Prevention
7. Emerging Biomarkers
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DM | Diabetes Mellitus |
| T2DM | type 2 DM |
| T1DM | type 1 DM |
| MI | myocardial infarction |
| BMI | body-mass index |
| HRs | hazard ratios |
| CI | confidence Interval |
| MCA | middle cerebral artery |
| FFAs | free fatty acids |
| ROS | reactive oxygen species |
| TFR | Transferrin receptor |
| P13k | P13 kinase |
| NO | nitric oxide |
| NF-κΒ | nuclear factor kappa-light-chain-enhancer of activated B cells |
| PKC | protein kinase C |
| ET-1 | endothelin-1 |
| COX-2 | cyclo-oxygenase 2 |
| TXA2 | thromboxane A2 |
| PGI2 | prostacyclin |
| AGEs | advanced glycation end products |
| RAGE | Receptor for advanced glycation endproducts |
| AHA | American Heart Association |
| GLP-1RAs | glucagon-like peptide 1 receptor agonists |
| REWIND | Researching Cardiovascular Events With a Weekly Incretin in Diabetes trial |
| ELIXA | Evaluation of Lixisenatide in Acute Coronary Syndrome trial |
| LEADER | Liraglutide Effect and Action in Diabetes: Evaluation of Cardiovascular Outcome Results |
| SUSTAIN | Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes |
| EXCEL | Exenatide Study of Cardiovascular Event Lowering Trial |
| HARMONY | Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease |
| PIONEER | Oral Semaglutide and Cardiovascular Outcomes in Patients with Type 2 Diabetes trial |
| SGLT-2is | sodium-glucose cotransporter-2 inhibitors |
| ROCKET AF | (Rivaroxaban Once-daily, Oral, Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation trial |
| DCCT/EDIC | Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications |
| UKPDS | United Kingdom Prospective Diabetes Study |
| BP | blood pressure |
| HbA1c | Glycated haemoglobin |
| ACCORD | Action to Control Cardiovascular Risk in Diabetes |
| TNF-α | Tumour necrosis factor-alpha |
| IL-6 | Interleukin-6 |
| IL-37 | interleukin-37 |
| VCAM-1 | Vascular cell adhesion molecule 1 |
| MiR-503 | micro-ribonucleic acid 503 |
| FABP-4 | Adipocyte fatty acid-binding protein 4 |
| TMAO | Trimethylamine N-Oxide |
| NfL | neurofilament light chain |
| 1,5-AG | 1,5-anhydroglucitol |
References
- Cho, N.; Shaw, J.; Karuranga, S.; Huang, Y.; Fernandes, J.D.R.; Ohlrogge, A.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Viigimaa, M.; Sachinidis, A.; Toumpourleka, M.; Koutsampasopoulos, K.; Alliksoo, S.; Titma, T. Macrovascular Complications of Type 2 Diabetes Mellitus. Curr. Vasc. Pharmacol. 2020, 18, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Faselis, C.; Katsimardou, A.; Imprialos, K.; Deligkaris, P.; Kallistratos, M.S.; Dimitriadis, K. Microvascular Complications of Type 2 Diabetes Mellitus. Curr. Vasc. Pharmacol. 2020, 18, 117–124. [Google Scholar] [CrossRef] [PubMed]
- Teliti, M.; Cogni, G.; Sacchi, L.; Dagliati, A.; Marini, S.; Tibollo, V.; De Cata, P.; Bellazzi, R.; Chiovato, L. Risk factors for the development of micro-vascular complications of type 2 diabetes in a single-centre cohort of patients. Diabetes Vasc. Dis. Res. 2018, 15, 424–432. [Google Scholar] [CrossRef]
- Laing, S.P.; Swerdlow, A.; Slater, S.D.; Burden, A.; Morris, A.; Waugh, N.R.; Gatling, W.; Bingley, P.J.; Patterson, C. Mortality from heart disease in a cohort of 23,000 patients with insulin-treated diabetes. Diabetologia 2003, 46, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Buyken, A.E.; Von Eckardstein, A.; Schulte, H.; Cullen, P.; Assmann, G. Type 2 diabetes mellitus and risk of coronary heart disease: Results of the 10-year follow-up of the PROCAM study. Eur. J. Cardiovasc. Prev. Rehabil. 2007, 14, 230–236. [Google Scholar] [CrossRef]
- Nichols, G.A.; Brown, J.B. The Impact of Cardiovascular Disease on Medical Care Costs in Subjects with and without Type 2 Diabetes. Diabetes Care 2002, 25, 482–486. [Google Scholar] [CrossRef]
- Kalofoutis, C.; Piperi, C.; Kalofoutis, A.; Harris, F.; Phoenix, D.; Singh, J. Type II diabetes mellitus and cardiovascular risk factors: Current therapeutic approaches. Exp. Clin. Cardiol. 2007, 12, 17–28. [Google Scholar]
- Chen, R.; Ovbiagele, B.; Feng, W. Diabetes and Stroke: Epidemiology, Pathophysiology, Pharmaceuticals and Outcomes. Am. J. Med Sci. 2016, 351, 380–386. [Google Scholar] [CrossRef]
- Boehme, A.K.; Esenwa, C.; Elkind, M.S.V. Stroke Risk Factors, Genetics, and Prevention. Circ. Res. 2017, 120, 472–495. [Google Scholar] [CrossRef]
- Kamalesh, M.; Shen, J.; Eckert, G.J. Long Term Postischemic Stroke Mortality in Diabetes: A veteran cohort analysis. Stroke 2008, 39, 2727–2731. [Google Scholar] [CrossRef]
- Einarson, T.R.; Acs, A.; Ludwig, C.; Panton, U.H. Prevalence of cardiovascular disease in type 2 diabetes: A systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc. Diabetol. 2018, 17, 83. [Google Scholar] [CrossRef]
- Jørgensen, H.; Nakayama, H.; Raaschou, H.O.; Olsen, T.S. Stroke in patients with diabetes. The Copenhagen Stroke Study. Stroke 1994, 25, 1977–1984. [Google Scholar] [CrossRef]
- Lee, M.; Saver, J.; Hong, K.-S.; Song, S.; Chang, K.-H.; Ovbiagele, B. Effect of pre-diabetes on future risk of stroke: Meta-analysis. BMJ 2012, 344, e3564. [Google Scholar] [CrossRef]
- Liu, A.; Carmichael, K.A.; Schallom, M.E.; Riley, M.J.; Klinkenberg, W.D. Detecting and Managing Diabetes Mellitus and Prediabetes in Patients with Acute Stroke. Diabetes Educ. 2015, 41, 592–598. [Google Scholar] [CrossRef] [PubMed]
- Venketasubramanian, N.; Yoon, B.W.; Pandian, J.; Navarro, J.C. Stroke Epidemiology in South, East, and South-East Asia: A Review. J. Stroke 2017, 19, 286–294. [Google Scholar] [CrossRef] [PubMed]
- Martin, S.; Schramm, W.; Schneider, B.; Neeser, K.; Weber, C.; Lodwig, V.; Heinemann, L.; Scherbaum, W.; Kolb, H. Epidemiology of Complications and Total Treatment Costs from Diagnosis of Type 2 Diabetes in Germany (ROSSO 4). Exp. Clin. Endocrinol. Diabetes 2007, 115, 495–501. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, C.; Moon, Y.P.; Paik, M.C.; Rundek, T.; Mora-McLaughlin, C.; Vieira, J.R.; Sacco, R.L.; Elkind, M.S. Duration of Diabetes and Risk of Ischemic Stroke: The Northern Manhattan Study. Stroke 2012, 43, 1212–1217. [Google Scholar] [CrossRef] [PubMed]
- Fuller, J.; the WHO Multinational Study Group; Stevens, L.; Wang, S.-L. Risk factors for cardiovascular mortality and morbidity: The WHO multinational study of vascular disease in diabetes. Diabetologia 2001, 44, S54–S64. [Google Scholar] [CrossRef] [PubMed]
- Melgaard, L.; Gorst-Rasmussen, A.; Søgaard, P.; Rasmussen, L.H.; Lip, G.Y.; Larsen, T.B. Diabetes mellitus and risk of ischemic stroke in patients with heart failure and no atrial fibrillation. Int. J. Cardiol. 2016, 209, 1–6. [Google Scholar] [CrossRef]
- Janghorbani, M.; Hu, F.B.; Willett, W.C.; Li, T.Y.; Manson, J.E.; Logroscino, G.; Rexrode, K. Prospective Study of Type 1 and Type 2 Diabetes and Risk of Stroke Subtypes: The Nurses’ Health Study. Diabetes Care 2007, 30, 1730–1735. [Google Scholar] [CrossRef] [PubMed]
- Sundquist, K.; Li, X. Type 1 diabetes as a risk factor for stroke in men and women aged 15–49: A nationwide study from Sweden. Diabet. Med. 2006, 23, 1261–1267. [Google Scholar] [CrossRef] [PubMed]
- Peters, S.; Huxley, R.R.; Woodward, M. Diabetes as a risk factor for stroke in women compared with men: A systematic review and meta-analysis of 64 cohorts, including 775 385 individuals and 12 539 strokes. Lancet 2014, 383, 1973–1980. [Google Scholar] [CrossRef]
- Huxley, R.R.; Peters, S.A.E.; Mishra, G.D.; Woodward, M. Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2015, 3, 198–206. [Google Scholar] [CrossRef]
- Aziz, S.; Ghadzi, S.M.S.; Abidin, N.E.; Tangiisuran, B.; Zainal, H.; Looi, I.; Ibrahim, K.A.; Sidek, N.N.; Wei, L.K.; Keng-Yee, L.; et al. Gender Differences and Risk Factors of Recurrent Stroke in Type 2 Diabetic Malaysian Population with History of Stroke: The Observation from Malaysian National Neurology Registry. J. Diabetes Res. 2019, 2019, 1794267. [Google Scholar] [CrossRef]
- Dhamoon, M.S.; Liang, J.W.; Zhou, L.; Stamplecoski, M.; Kapral, M.K.; Shah, B.R. Sex Differences in Outcomes after Stroke in Patients with Diabetes in Ontario, Canada. J. Stroke Cerebrovasc. Dis. 2017, 27, 210–220. [Google Scholar] [CrossRef]
- Duan, D.; Li, H.; Xu, J.; Wong, L.P.; Xu, G.; Kong, F.; Li, S.; Gong, Q.; Zhang, X.; Zhao, J.; et al. Does Body Mass Index and Height Influence the Incident Risk of Ischemic Stroke in Newly Diagnosed Type 2 Diabetes Subjects? J. Diabetes Res. 2019, 2019, 2591709. [Google Scholar] [CrossRef]
- Li, W.; Katzmarzyk, P.; Horswell, R.; Zhang, Y.; Zhao, W.; Wang, Y.; Johnson, J.; Hu, G. Body Mass Index and Stroke Risk Among Patients with Type 2 Diabetes Mellitus. Stroke 2015, 46, 164–169. [Google Scholar] [CrossRef]
- Eeg-Olofsson, K.; Cederholm, J.; Nilsson, P.M.; Zethelius, B.; Nunez, L.; Gudbjörnsdóttir, S.; Eliasson, B. Risk of cardiovascular disease and mortality in overweight and obese patients with type 2 diabetes: An observational study in 13,087 patients. Diabetologia 2009, 52, 65–73. [Google Scholar] [CrossRef]
- Hainer, V.; Aldhoon-Hainerová, I. Obesity Paradox Does Exist. Diabetes Care 2013, 36, S276–S281. [Google Scholar] [CrossRef]
- Khan, S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of Body Mass Index with Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Oreopoulos, A.; Padwal, R.; Kalantar-Zadeh, K.; Fonarow, G.C.; Norris, C.M.; McAlister, F.A. Body mass index and mortality in heart failure: A meta-analysis. Am. Heart J. 2008, 156, 13–22. [Google Scholar] [CrossRef]
- Romero-Corral, A.; Montori, V.; Somers, V.K.; Korinek, J.; Thomas, R.; Allison, T.G.; Mookadam, F.; Lopez-Jimenez, F. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. Lancet 2006, 368, 666–678. [Google Scholar] [CrossRef]
- Wang, L.; Liu, W.; He, X.; Chen, Y.; Lu, J.; Liu, K.; Cao, K.; Yin, P. Association of overweight and obesity with patient mortality after acute myocardial infarction: A meta-analysis of prospective studies. Int. J. Obes. 2016, 40, 220–228. [Google Scholar] [CrossRef]
- Quiñones-Ossa, G.A.; Lobo, C.; Garcia-Ballestas, E.; Florez, W.A.; Moscote-Salazar, L.R.; Agrawal, A. Obesity and Stroke: Does the Paradox Apply for Stroke? Neurointervention 2021, 16, 9–19. [Google Scholar] [CrossRef]
- Wohlfahrt, P.; Lopez-Jimenez, F.; Krajcoviechova, A.; Jozifova, M.; Mayer, O.; Vanek, J.; Filipovsky, J.; Llano, E.M.; Cífková, R. The Obesity Paradox and Survivors of Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2015, 24, 1443–1450. [Google Scholar] [CrossRef]
- Tobias, D.K.; Manson, J.E. The Obesity Paradox in Type 2 Diabetes and Mortality. Am. J. Lifestyle Med. 2016, 12, 244–251. [Google Scholar] [CrossRef]
- Horwich, T.B.; Fonarow, G.C.; Clark, A.L. Obesity and the Obesity Paradox in Heart Failure. Prog. Cardiovasc. Dis. 2018, 61, 151–156. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, C.K.; Jung, S.; Yoon, B.-W.; Lee, S.-H. Obesity-stroke paradox and initial neurological severity. J. Neurol. Neurosurg. Psychiatry 2015, 86, 743–747. [Google Scholar] [CrossRef]
- Olofindayo, J.; Peng, H.; Liu, Y.; Li, H.; Zhang, M.; Wang, A.; Zhang, Y. The interactive effect of diabetes and central obesity on stroke: A prospective cohort study of inner Mongolians. BMC Neurol. 2015, 15, 65. [Google Scholar] [CrossRef][Green Version]
- Lee, K.S.; Moser, D.K.; Lennie, T.A.; Pelter, M.M.; Nesbitt, T.; Southard, J.A.; Dracup, K. Obesity Paradox: Comparison of Heart Failure Patients with and without Comorbid Diabetes. Am. J. Crit. Care 2017, 26, 140–148. [Google Scholar] [CrossRef]
- Lindholm, L.H.; Ibsen, H.; Dahlöf, B.; Devereux, R.B.; Beevers, G.; de Faire, U.; Fyhrquist, F.; Julius, S.; Kjeldsen, S.E.; Kristiansson, K.; et al. Cardiovascular morbidity and mortality in patients with diabetes in the Losartan Intervention for Endpoint reduction in hypertension study (LIFE): A randomised trial against atenolol. Lancet 2002, 359, 1004–1010. [Google Scholar] [CrossRef]
- Cushman, W.C.; Evans, G.W.; Byington, R.P.; Goff, D.C.; Grimm, R.H.; Cutler, J.A.; Simons-Morton, D.G.; Basile, J.N.; Corson, M.A.; Probstfield, J.L.; et al. Effects of Intensive Blood-Pressure Control in Type 2 Diabetes Mellitus. N. Engl. J. Med. 2010, 362, 1575–1585. [Google Scholar] [CrossRef]
- Liao, C.-C.; Shih, C.-C.; Yeh, C.-C.; Chang, Y.-C.; Hu, C.-J.; Lin, J.-G.; Chen, T.-L. Impact of Diabetes on Stroke Risk and Outcomes: Two nationwide retrospective cohort studies. Medicine 2015, 94, e2282. [Google Scholar] [CrossRef] [PubMed]
- Nyström, T.; Holzmann, M.J.; Sartipy, U. Long-Term Risk of Stroke in Patients with Type 1 and Type 2 Diabetes Following Coronary Artery Bypass Grafting. J. Am. Heart Assoc. 2015, 4, e002411. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.J.; Xavier, D.; Liu, L.; Zhang, H.; Chin, S.L.; Rao-Melacini, P.; Rangarajan, S.; Islam, S.; Pais, P.; McQueen, M.J.; et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): A case-control study. Lancet 2010, 376, 112–123. [Google Scholar] [CrossRef]
- Chen, Y.-L.; Weng, S.-F.; Yang, C.-Y.; Wang, J.-J.; Tien, K.-J. Long-term risk of stroke in type 2 diabetes patients with diabetic ketoacidosis: A population-based, propensity score-matched, longitudinal follow-up study. Diabetes Metab. 2017, 43, 223–228. [Google Scholar] [CrossRef]
- Harjutsalo, V.; Thomas, M.C.; Forsblom, C.; Groop, P.-H.; On Behalf of the FinnDiane Study Group. Risk of coronary artery disease and stroke according to sex and presence of diabetic nephropathy in type 1 diabetes. Diabetes Obes. Metab. 2018, 20, 2759–2767. [Google Scholar] [CrossRef]
- Lou, H.; Dong, Z.; Zhang, P.; Shao, X.; Li, T.; Zhao, C.; Zhang, X.; Lou, P. Interaction of diabetes and smoking on stroke: A population-based cross-sectional survey in China. BMJ Open 2018, 8, e017706. [Google Scholar] [CrossRef]
- Pan, A.; Wang, Y.; Talaei, M.; Hu, F.B. Relation of Smoking with Total Mortality and Cardiovascular Events Among Patients with Diabetes Mellitus: A meta-analysis and systematic review. Circulation 2015, 132, 1795–1804. [Google Scholar] [CrossRef]
- Feodoroff, M.; Harjutsalo, V.; Forsblom, C.; Groop, P.-H. Dose-dependent effect of smoking on risk of coronary heart disease, heart failure and stroke in individuals with type 1 diabetes. Diabetologia 2018, 61, 2580–2589. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.B.; Florez, J.C. Genetics of diabetes mellitus and diabetes complications. Nat. Rev. Nephrol. 2020, 16, 377–390. [Google Scholar] [CrossRef] [PubMed]
- Mühlenbruch, K.; Menzel, J.; Dörr, M.; Ittermann, T.; Meisinger, C.; Peters, A.; Kluttig, A.; Medenwald, D.; Bergmann, M.; Boeing, H.; et al. Association of familial history of diabetes or myocardial infarction and stroke with risk of cardiovascular diseases in four German cohorts. Sci. Rep. 2020, 10, 15373. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.-W.; Kung, P.-T.; Chou, W.-Y.; Tsai, W.-C. Pay-for-performance programmes reduce stroke risks in patients with type 2 diabetes: A national cohort study. BMJ Open 2019, 9, e026626. [Google Scholar] [CrossRef] [PubMed]
- Drinkwater, J.J.; Davis, T.M.E.; Hellbusch, V.; Turner, A.W.; Bruce, D.; Davis, W. Retinopathy predicts stroke but not myocardial infarction in type 2 diabetes: The Fremantle Diabetes Study Phase II. Cardiovasc. Diabetol. 2020, 19, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Wang, A.; Jiang, R.; Su, Z.; Zhang, J.; Zhao, X.; Wu, S.; Guo, X. Association of Persistent, Incident, and Remittent Proteinuria with Stroke Risk in Patients with Diabetes Mellitus or Prediabetes Mellitus. J. Am. Heart Assoc. 2017, 6, e006178. [Google Scholar] [CrossRef]
- The Emerging Risk Factors Collaboration. Diabetes Mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef]
- Chi, Y.; Lu, Z.-N. Association between patency of the circle of Willis and diabetes mellitus in patients with cerebral ischaemic stroke. J. Int. Med. Res. 2017, 45, 723–732. [Google Scholar] [CrossRef]
- Suri, M.F.K.; Johnston, S.C. Epidemiology of Intracranial Stenosis. J. Neuroimaging 2009, 19, 11S–16S. [Google Scholar] [CrossRef]
- Carvalho, M.; Oliveira, A.; Azevedo, E.; Bastos-Leite, A.J. Intracranial Arterial Stenosis. J. Stroke Cerebrovasc. Dis. 2014, 23, 599–609. [Google Scholar] [CrossRef]
- Bae, H.-J.; Lee, J.; Park, J.-M.; Kwon, O.; Koo, J.-S.; Kim, B.-K.; Pandey, D. Risk Factors of Intracranial Cerebral Atherosclerosis among Asymptomatics. Cerebrovasc. Dis. 2007, 24, 355–360. [Google Scholar] [CrossRef] [PubMed]
- Uehara, T.; Tabuchi, M.; Mori, E. Risk factors for occlusive lesions of intracranial arteries in stroke-free Japanese. Eur. J. Neurol. 2005, 12, 218–222. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.W.; Guo, M.H.; Lin, R.J.; Chen, Y.L.; Luo, Q.; Zhang, Y.; Wong, K.S.L. Prevalence and Risk Factors of Middle Cerebral Artery Stenosis in Asymptomatic Residents in Rongqi County, Guangdong. Cerebrovasc. Dis. 2007, 24, 111–115. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.N.; Chen, X.-Y.; Lin, J.W.; Tomlinson, B.; Lam, W.W.; Liu, R.; Yeung, V.T.; Chan, J.C.; Wong, K.S. Middle Cerebral Artery Stenosis Increased the Risk of Vascular Disease Mortality among Type 2 Diabetic Patients. Cerebrovasc. Dis. 2008, 25, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.N.; Lin, J.W.; Lam, W.W.; Tomlinson, B.; Yeung, V.; Chan, J.; Wong, K.S.L. Middle Cerebral Artery Stenosis in Type II Diabetic Chinese Patients Is Associated with Conventional Risk Factors but Not with Polymorphisms of the Renin-Angiotensin System Genes. Cerebrovasc. Dis. 2003, 16, 217–223. [Google Scholar] [CrossRef] [PubMed]
- Ferris, J.K.; Peters, S.; Brown, K.E.; Tourigny, K.; Boyd, L.A. Type-2 diabetes mellitus reduces cortical thickness and decreases oxidative metabolism in sensorimotor regions after stroke. Br. J. Pharmacol. 2018, 38, 823–834. [Google Scholar] [CrossRef]
- Yu, X.; Song, R.; Jiaerken, Y.; Yuan, L.; Huang, P.; Lou, M.; Jiang, Q.; Zhang, M. White matter injury induced by diabetes in acute stroke is clinically relevant: A preliminary study. Diabetes Vasc. Dis. Res. 2017, 14, 40–46. [Google Scholar] [CrossRef]
- Wisse, L.E.; de Bresser, J.; Geerlings, M.I.; Reijmer, Y.D.; Portegies, M.L.; Brundel, M.; Kappelle, L.J.; van der Graaf, Y.; Biessels, G.J. Global brain atrophy but not hippocampal atrophy is related to type 2 diabetes. J. Neurol. Sci. 2014, 344, 32–36. [Google Scholar] [CrossRef]
- Chen, Z.; Li, L.; Sun, J.; Ma, L. Mapping the brain in type II diabetes: Voxel-based morphometry using DARTEL. Eur. J. Radiol. 2012, 81, 1870–1876. [Google Scholar] [CrossRef]
- Espeland, M.A.; Bryan, R.N.; Goveas, J.S.; Robinson, J.G.; Siddiqui, M.S.; Liu, S.; Hogan, P.E.; Casanova, R.; Coker, L.H.; Yaffe, K.; et al. Influence of Type 2 Diabetes on Brain Volumes and Changes in Brain Volumes: Results from the Women’s Health Initiative Magnetic Resonance Imaging Studies. Diabetes Care 2013, 36, 90–97. [Google Scholar] [CrossRef]
- Tun, N.N.; Arunagirinathan, G.; Munshi, S.K.; Pappachan, J.M. Diabetes mellitus and stroke: A clinical update. World J. Diabetes 2017, 8, 235–248. [Google Scholar] [CrossRef]
- Huang, D.; Refaat, M.; Mohammedi, K.; Jayyousi, A.; Al Suwaidi, J.; Khalil, C.A. Macrovascular Complications in Patients with Diabetes and Prediabetes. BioMed Res. Int. 2017, 2017, 7839101. [Google Scholar] [CrossRef]
- Shukla, V.; Shakya, A.K.; Perez-Pinzon, M.A.; Dave, K.R. Cerebral ischemic damage in diabetes: An inflammatory perspective. J. Neuroinflamm. 2017, 14, 21. [Google Scholar] [CrossRef]
- Du, X.L.; Edelstein, D.; Dimmeler, S.; Ju, Q.; Sui, C.; Brownlee, M. Hyperglycemia inhibits endothelial nitric oxide synthase activity by posttranslational modification at the Akt site. J. Clin. Investig. 2001, 108, 1341–1348. [Google Scholar] [CrossRef]
- Schrieks, I.C.; Nozza, A.; Stähli, B.E.; Buse, J.B.; Henry, R.R.; Malmberg, K.; Neal, B.; Nicholls, S.J.; Ryden, L.; Mellbin, L.; et al. Adiponectin, Free Fatty Acids, and Cardiovascular Outcomes in Patients with Type 2 Diabetes and Acute Coronary Syndrome. Diabetes Care 2018, 41, 1792–1800. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Chakraborty, D.; Bhattacharya, P.; Sarmah, D.; Koch, S.; Dave, K.R. Exposure to hypoglycemia and risk of stroke. Ann. N. Y. Acad. Sci. 2018, 1431, 25–34. [Google Scholar] [CrossRef] [PubMed]
- Du, X.; Edelstein, D.; Obici, S.; Higham, N.; Zou, M.-H.; Brownlee, M. Insulin resistance reduces arterial prostacyclin synthase and eNOS activities by increasing endothelial fatty acid oxidation. J. Clin. Investig. 2006, 116, 1071–1080. [Google Scholar] [CrossRef] [PubMed]
- Jauch, E.C.; Saver, J.; Adams, H.P.; Bruno, A.; Connors, J.; Demaerschalk, B.M.; Khatri, P.; McMullan, P.W.; Qureshi, A.; Rosenfield, K.; et al. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 870–947. [Google Scholar] [CrossRef]
- Nunes, A.P.; Iglay, K.; Radican, L.; Engel, S.S.; Yang, J.; Doherty, M.C.; Dore, D. Hypoglycaemia seriousness and weight gain as determinants of cardiovascular disease outcomes among sulfonylurea users. Diabetes Obes. Metab. 2017, 19, 1425–1435. [Google Scholar] [CrossRef]
- Moheet, A.; Seaquist, E.R. Hypoglycemia as a Driver of Cardiovascular Risk in Diabetes. Curr. Atheroscler. Rep. 2013, 15, 351. [Google Scholar] [CrossRef]
- Hacke, W.; Kaste, M.; Bogousslavsky, J.; Brainin, M.; Chamorro, A.; Lees, K.; Leys, D.; Kwiacinski, H.; Toni, D. European Stroke Initiative Recommendations for Stroke Management—Update 2003. Cerebrovasc. Dis. 2003, 16, 311–337. [Google Scholar] [CrossRef]
- Dungan, K.M.; Braithwaite, S.S.; Preiser, J.C. Stress hyperglycaemia. Lancet 2009, 373, 1798–1807. [Google Scholar] [CrossRef]
- Capes, S.E.; Hunt, D.; Malmberg, K.; Pathak, P.; Gerstein, H.C. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: A systematic overview. Stroke 2001, 32, 2426–2432. [Google Scholar] [CrossRef]
- Li, J.; Quan, K.; Wang, Y.; Zhao, X.; Li, Z.; Pan, Y.; Li, H.; Liu, L.; Wang, Y. Effect of Stress Hyperglycemia on Neurological Deficit and Mortality in the Acute Ischemic Stroke People with and without Diabetes. Front. Neurol. 2020, 11, 576895. [Google Scholar] [CrossRef] [PubMed]
- Pan, Y.; Cai, X.; Jing, J.; Meng, X.; Li, H.; Wang, Y.; Zhao, X.; Liu, L.; Wang, D.; Johnston, S.C.; et al. Stress Hyperglycemia and Prognosis of Minor Ischemic Stroke and Transient Ischemic Attack: The CHANCE Study (Clopidogrel in High-Risk Patients with Acute Nondisabling Cerebrovascular Events). Stroke 2017, 48, 3006–3011. [Google Scholar] [CrossRef]
- Bruno, A.; Kent, T.; Coull, B.M.; Shankar, R.R.; Saha, C.; Becker, K.; Kissela, B.M.; Williams, L.S. Treatment of Hyperglycemia in Ischemic Stroke (THIS). Stroke 2008, 39, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Johnston, K.C.; Hall, C.E.; Kissela, B.M.; Bleck, T.; Conaway, M.R. Glucose Regulation in Acute Stroke Patients (GRASP) Trial: A randomized pilot trial. Stroke 2009, 40, 3804–3809. [Google Scholar] [CrossRef]
- Gray, C.S.; Hildreth, A.J.; Sandercock, P.A.; O’Connell, J.E.; Johnston, D.E.; Cartlidge, N.E.; Bamford, J.M.; James, O.F.; Alberti, K.G.M. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: The UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol. 2007, 6, 397–406. [Google Scholar] [CrossRef]
- Johnston, K.C.; Bruno, A.; Pauls, Q.; Hall, C.E.; Barrett, K.M.; Barsan, W.; Fansler, A.; Van De Bruinhorst, K.; Janis, S.; Durkalski-Mauldin, V.L.; et al. Intensive vs Standard Treatment of Hyperglycemia and Functional Outcome in Patients with Acute Ischemic Stroke: The SHINE randomized clinical trial. JAMA 2019, 322, 326–335. [Google Scholar] [CrossRef]
- Tsioufis, C.; Andrikou, E.; Thomopoulos, C.; Papanas, N.; Tousoulis, D.; Tsioufis, E.A.C. Oral Glucose-lowering Drugs and Cardiovascular Outcomes: From the Negative RECORD and ACCORD to Neutral TECOS and Promising EMPA-REG. Curr. Vasc. Pharmacol. 2017, 15, 457–468. [Google Scholar] [CrossRef]
- Andrikou, E.; Tsioufis, C.; Andrikou, I.; Leontsinis, I.; Tousoulis, D.; Papanas, N. GLP-1 receptor agonists and cardiovascular outcome trials: An update. Hell. J. Cardiol. 2019, 60, 347–351. [Google Scholar] [CrossRef]
- Gerstein, H.C.; Colhoun, H.M.; Dagenais, G.R.; Diaz, R.; Lakshmanan, M.; Pais, P.; Probstfield, J.; Riesmeyer, J.S.; Riddle, M.C.; Rydén, L.; et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): A double-blind, randomised placebo-controlled trial. Lancet 2019, 394, 121–130. [Google Scholar] [CrossRef]
- Gerstein, H.C.; Hart, R.; Colhoun, H.M.; Diaz, R.; Lakshmanan, M.; Botros, F.T.; Probstfield, J.; Riddle, M.C.; Rydén, L.; Atisso, C.M.; et al. The effect of dulaglutide on stroke: An exploratory analysis of the REWIND trial. Lancet Diabetes Endocrinol. 2020, 8, 106–114. [Google Scholar] [CrossRef]
- Pfeffer, M.A.; Claggett, B.; Diaz, R.; Dickstein, K.; Gerstein, H.; Køber, L.V.; Lawson, F.C.; Ping, L.; Wei, X.; Lewis, E.F.; et al. Lixisenatide in Patients with Type 2 Diabetes and Acute Coronary Syndrome. N. Engl. J. Med. 2015, 373, 2247–2257. [Google Scholar] [CrossRef] [PubMed]
- Marso, S.P.; Daniels, G.H.; Brown-Frandsen, K.; Kristensen, P.; Mann, J.F.; Nauck, M.A.; Nissen, S.E.; Pocock, S.; Poulter, N.R.; Ravn, L.S.; et al. Liraglutide and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 311–322. [Google Scholar] [CrossRef]
- Aroda, V.R.; Ahmann, A.; Cariou, B.; Chow, F.; Davies, M.J.; Jódar, E.; Mehta, R.; Woo, V.; Lingvay, I. Comparative efficacy, safety, and cardiovascular outcomes with once-weekly subcutaneous semaglutide in the treatment of type 2 diabetes: Insights from the SUSTAIN 1–7 trials. Diabetes Metab. 2019, 45, 409–418. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.R.; Bethel, M.A.; Mentz, R.J.; Thompson, V.P.; Lokhnygina, Y.; Buse, J.; Chan, J.; Choi, J.; Gustavson, S.M.; Iqbal, N.; et al. Effects of Once-Weekly Exenatide on Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 1228–1239. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, A.F.; Green, J.B.; Janmohamed, S.; D’Agostino, R.B.; Granger, C.B.; Jones, N.P.; Leiter, L.A.; Rosenberg, A.E.; Sigmon, K.N.; Somerville, M.C.; et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): A double-blind, randomised placebo-controlled trial. Lancet 2018, 392, 1519–1529. [Google Scholar] [CrossRef]
- Thethi, T.K.; Pratley, R.; Meier, J.J. Efficacy, safety and cardiovascular outcomes of once-daily oral semaglutide in patients with type 2 diabetes: The PIONEER programme. Diabetes Obes. Metab. 2020, 22, 1263–1277. [Google Scholar] [CrossRef]
- Bethel, M.A.; Patel, R.A.; Merrill, P.; Lokhnygina, Y.; Buse, J.B.; Mentz, R.J.; Pagidipati, N.J.; Chan, J.C.; Gustavson, S.M.; Iqbal, N.; et al. Cardiovascular outcomes with glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes: A meta-analysis. Lancet Diabetes Endocrinol. 2018, 6, 105–113. [Google Scholar] [CrossRef]
- Bellastella, G.; Maiorino, M.I.; Longo, M.; Scappaticcio, L.; Chiodini, P.; Esposito, K.; Giugliano, D. Glucagon-Like Peptide-1 Receptor Agonists and Prevention of Stroke Systematic Review of Cardiovascular Outcome Trials with Meta-Analysis. Stroke 2020, 51, 666–669. [Google Scholar] [CrossRef] [PubMed]
- Zelniker, T.A.; Wiviott, S.D.; Raz, I.; Im, K.; Goodrich, E.; Furtado, R.H.M.; Bonaca, M.P.; Mosenzon, O.; Kato, E.; Cahn, A.; et al. Comparison of the Effects of Glucagon-Like Peptide Receptor Agonists and Sodium-Glucose Cotransporter 2 Inhibitors for Prevention of Major Adverse Cardiovascular and Renal Outcomes in Type 2 Diabetes Mellitus. Circulation 2019, 139, 2022–2031. [Google Scholar] [CrossRef] [PubMed]
- Buse, J.B.; Wexler, D.J.; Tsapas, A.; Rossing, P.; Mingrone, G.; Mathieu, C.; D’Alessio, D.A.; Davies, M.J. 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020, 63, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Lugner, M.; Sattar, N.; Miftaraj, M.; Ekelund, J.; Franzén, S.; Svensson, A.-M.; Eliasson, B. Cardiorenal and other diabetes related outcomes with SGLT-2 inhibitors compared to GLP-1 receptor agonists in type 2 diabetes: Nationwide observational study. Cardiovasc. Diabetol. 2021, 20, 67. [Google Scholar] [CrossRef]
- Bansilal, S.; Bloomgarden, Z.; Halperin, J.L.; Hellkamp, A.S.; Lokhnygina, Y.; Patel, M.R.; Becker, R.C.; Breithardt, G.; Hacke, W.; Hankey, G.J.; et al. Efficacy and safety of rivaroxaban in patients with diabetes and nonvalvular atrial fibrillation: The Rivaroxaban Once-daily, Oral, Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF Trial). Am. Heart J. 2015, 170, 675–682. [Google Scholar] [CrossRef]
- Patti, G.; Di Gioia, G.; Cavallari, I.; Nenna, A. Safety and efficacy of nonvitamin K antagonist oral anticoagulants versus warfarin in diabetic patients with atrial fibrillation: A study-level meta-analysis of phase III randomized trials. Diabetes/Metabolism Res. Rev. 2017, 33, e2876. [Google Scholar] [CrossRef]
- American Diabetes Association 8. Cardiovascular Disease and Risk Management. Diabetes Care 2016, 39, S60–S71. [Google Scholar] [CrossRef]
- Casagrande, S.S.; Fradkin, J.E.; Saydah, S.H.; Rust, K.F.; Cowie, C.C. The Prevalence of Meeting A1C, Blood Pressure, and LDL Goals Among People with Diabetes, 1988–2010. Diabetes Care 2013, 36, 2271–2279. [Google Scholar] [CrossRef] [PubMed]
- Raum, E.; Lietzau, S.; Stegmaier, C.; Brenner, H.; Rothenbacher, D. For the majority of patients with diabetes blood pressure and lipid management is not in line with recommendations. Results from a large population-based cohort in Germany. Pharmacoepidemiol. Drug Saf. 2008, 17, 485–494. [Google Scholar] [CrossRef]
- Rückert, I.-M.; Schunk, M.; Holle, R.; Schipf, S.; Völzke, H.; Kluttig, A.; Greiser, K.-H.; Berger, K.; Müller, G.; Ellert, U.; et al. Blood pressure and lipid management fall far short in persons with type 2 diabetes: Results from the DIAB-CORE Consortium including six German population-based studies. Cardiovasc. Diabetol. 2012, 11, 50. [Google Scholar] [CrossRef] [PubMed]
- Pappachan, J.M.; Viswanath, A.K. Medical Management of Diabesity: Do We Have Realistic Targets? Curr. Diabetes Rep. 2017, 17, 4. [Google Scholar] [CrossRef]
- Sjöström, L.; Peltonen, M.; Jacobson, P.; Sjöström, C.D.; Karason, K.; Wedel, H.; Ahlin, S.; Anveden, A.; Bengtsson, C.; Bergmark, G.; et al. Bariatric Surgery and Long-term Cardiovascular Events. JAMA 2012, 307, 56–65. [Google Scholar] [CrossRef]
- Zhao, B.; Zeng, L.; Zhao, J.; Wu, Q.; Dong, Y.; Zou, F.; Gan, L.; Wei, Y.; Zhang, W. Association of magnesium intake with type 2 diabetes and total stroke: An updated systematic review and meta-analysis. BMJ Open 2020, 10, e032240. [Google Scholar] [CrossRef]
- Mitsios, J.P.; Ekinci, E.I.; Mitsios, G.P.; Churilov, L.; Thijs, V. Relationship Between Glycated Hemoglobin and Stroke Risk: A Systematic Review and Meta-Analysis. J. Am. Heart Assoc. 2018, 7, e007858. [Google Scholar] [CrossRef]
- The Diabetes Control and Complications Trial (DCCT)/Epidemiology of Diabetes Interventions and Complications (EDIC) Study Research Group. Intensive Diabetes Treatment and Cardiovascular Outcomes in Type 1 Diabetes: The DCCT/EDIC Study 30-Year Follow-up. Diabetes Care 2016, 39, 686–693. [Google Scholar] [CrossRef]
- Turnbull, F.M.; Abraira, C.; Anderson, R.J.; Byington, R.P.; Chalmers, J.; Duckworth, W.C.; Evans, G.W.; Gerstein, H.; Holman, R.R.; Moritz, T.E.; et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia 2009, 52, 2288–2298. [Google Scholar] [CrossRef]
- Patel, A.; MacMahon, S.; Chalmers, J.; Neal, B.; Billot, L.; Joshi, R.; Woodward, M.; Marre, M.; Travert, F.; Cooper, M.; et al. Intensive Blood Glucose Control and Vascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 2560–2572. [Google Scholar] [CrossRef]
- Gæde, P.; Vedel, P.; Larsen, N.; Jensen, G.V.H.; Parving, H.-H.; Pedersen, O. Multifactorial Intervention and Cardiovascular Disease in Patients with Type 2 Diabetes. N. Engl. J. Med. 2003, 348, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Chamberlain, J.J.; Rhinehart, A.S.; Shaefer, C.F.; Neuman, A. Diagnosis and Management of Diabetes: Synopsis of the 2016 American Diabetes Association Standards of Medical Care in Diabetes. Ann. Intern. Med. 2016, 164, 542–552. [Google Scholar] [CrossRef] [PubMed]
- Holman, R.R.; Paul, S.; Bethel, M.A.; Matthews, D.R.; Neil, H.A.W. 10-Year Follow-up of Intensive Glucose Control in Type 2 Diabetes. N. Engl. J. Med. 2008, 359, 1577–1589. [Google Scholar] [CrossRef] [PubMed]
- Bangalore, S.; Kumar, S.; Lobach, I.; Messerli, F.H. Blood Pressure Targets in Subjects with Type 2 Diabetes Mellitus/Impaired Fasting Glucose: Observations from traditional and bayesian ran-dom-effects meta-analyses of randomized trials. Circulation 2011, 123, 2799–2810. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.; Armitage, J.; Parish, S.; Sleigh, P.; Peto, R. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: A randomised placebo-controlled trial. Lancet 2003, 361, 2005–2016. [Google Scholar] [CrossRef]
- Colhoun, H.M.; Betteridge, D.J.; Durrington, P.N.; Hitman, G.A.; Neil, H.A.W.; Livingstone, S.J.; Thomason, M.; Mackness, M.I.; Charlton-Menys, V.; Fuller, J.H. Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): Multicentre randomised placebo-controlled trial. Lancet 2004, 364, 685–696. [Google Scholar] [CrossRef]
- Cannon, C.P.; Blazing, M.A.; Giugliano, R.; McCagg, A.; White, J.A.; Theroux, P.; Darius, H.; Lewis, B.S.; Ophuis, T.O.; Jukema, J.W.; et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N. Engl. J. Med. 2015, 372, 2387–2397. [Google Scholar] [CrossRef] [PubMed]
- Qin, Z.-Y.; Yang, X.-F.; Lian, C.-Y.; Yan, X.-J.; Lin, M.-S.; Bundhun, P.K.; Lao, Y.-Y. Aspirin Versus Clopidogrel Monotherapy for the Secondary Prevention of Recurrent Cerebrovascular Attack Following Previous Ischemic Stroke in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis. Diabetes Ther. 2020, 11, 1091–1101. [Google Scholar] [CrossRef]
- Woo, M.-H.; Lee, H.S.; Kim, J. Effect of pioglitazone in acute ischemic stroke patients with diabetes mellitus: A nested case–control study. Cardiovasc. Diabetol. 2019, 18, 67. [Google Scholar] [CrossRef] [PubMed]
- Young, L.H.; Viscoli, C.M.; Curtis, J.P.; Inzucchi, S.E.; Schwartz, G.G.; Lovejoy, A.M.; Furie, K.L.; Gorman, M.J.; Conwit, R.; Abbott, J.D.; et al. Cardiac Outcomes after Ischemic Stroke or Transient Ischemic Attack: Effects of pioglitazone in patients with insulin resistance without diabetes mellitus. Circulation 2017, 135, 1882–1893. [Google Scholar] [CrossRef]
- Yaghi, S.; Furie, K.L.; Viscoli, C.M.; Kamel, H.; Gorman, M.; Dearborn, J.; Young, L.H.; Inzucchi, S.E.; Lovejoy, A.M.; Kasner, S.E.; et al. Pioglitazone Prevents Stroke in Patients with a Recent Transient Ischemic Attack or Ischemic Stroke: A planned sec-ondary analysis of the iris trial (insulin resistance intervention after stroke). Circulation 2018, 137, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Saver, J.L.; Liao, H.-W.; Lin, C.-H.; Ovbiagele, B. Pioglitazone for Secondary Stroke Prevention: A systematic review and meta-analysis. Stroke 2017, 48, 388–393. [Google Scholar] [CrossRef] [PubMed]
- Borggrefe, J.; Glück, B.; Maus, V.; Onur, O.; Abdullayev, N.; Barnikol, U.; Kabbasch, C.; Fink, G.R.; Mpotsaris, A. Clinical Outcome after Mechanical Thrombectomy in Patients with Diabetes with Major Ischemic Stroke of the Anterior Circulation. World Neurosurg. 2018, 120, e212–e220. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.Y.; Kim, W.-J.; Kwon, J.H.; Kim, B.J.; Kim, J.-T.; Lee, J.; Cha, J.K.; Kim, D.-H.; Cho, Y.-J.; Hong, K.-S.; et al. Prestroke Glucose Control and Functional Outcome in Patients with Acute Large Vessel Occlusive Stroke and Diabetes after Thrombectomy. Diabetes Care 2021, 44, 2140–2148. [Google Scholar] [CrossRef]
- Fang, H.-J.; Pan, Y.-S.; Wang, Y.-J.; Wang, C.-X.; Wang, Y.-L.; Zhong, L.-Y. Prognostic value of admission hyperglycemia on outcomes of thrombolysis in ischemic stroke patients with or without diabetes. Chin. Med. J. 2020, 133, 2244–2246. [Google Scholar] [CrossRef]
- Desilles, J.-P.; Meseguer, E.; Labreuche, J.; Lapergue, B.; Sirimarco, G.; Gonzalez-Valcarcel, J.; Lavallée, P.; Cabrejo, L.; Guidoux, C.; Klein, I.; et al. Diabetes Mellitus, Admission Glucose, and Outcomes after Stroke Thrombolysis: A registry and systematic review. Stroke 2013, 44, 1915–1923. [Google Scholar] [CrossRef]
- Papachristou, S.; Pafili, K.; Papanas, N. Skin AGEs and diabetic neuropathy. BMC Endocr. Disord. 2021, 21, 28. [Google Scholar] [CrossRef]
- Singh, V.P.; Bali, A.; Singh, N.; Jaggi, A.S. Advanced Glycation End Products and Diabetic Complications. Korean J. Physiol. Pharmacol. 2014, 18, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Heier, M.; Margeirsdottir, H.D.; Gaarder, M.; Stensaeth, K.H.; Brunborg, C.; Torjesen, P.A.; Seljeflot, I.; Hanssen, K.F.; Dahl-Jørgensen, K. Soluble RAGE and atherosclerosis in youth with type 1 diabetes: A 5-year follow-up study. Cardiovasc. Diabetol. 2015, 14, 126. [Google Scholar] [CrossRef] [PubMed]
- Vendrell, J.; Fernández-Real, J.M.; Gutierrez, C.; Zamora, A.; Simon, I.; Bardaji, A.; Ricart, W.; Richart, C. A polymorphism in the promoter of the tumor necrosis factor-α gene (−308) is associated with coronary heart disease in type 2 diabetic patients. Atherosclerosis 2003, 167, 257–264. [Google Scholar] [CrossRef]
- Yudkin, J.S.; Kumari, M.; Humphries, S.E.; Mohamed-Ali, V. Inflammation, obesity, stress and coronary heart disease: Is interleukin-6 the link? Atherosclerosis 2000, 148, 209–214. [Google Scholar] [CrossRef]
- Chai, M.; Guangjin, G.; Zhang, H.; Zhou, Y.; Yang, Q.; Zhou, Y.; Guo, G.; Liu, W.; Han, W.; Yang, L.; et al. The Protective Effect of Interleukin-37 on Vascular Calcification and Atherosclerosis in Apolipoprotein E-Deficient Mice with Diabetes. J. Interf. Cytokine Res. 2015, 35, 530–539. [Google Scholar] [CrossRef]
- Soedamah-Muthu, S.S.; Chaturvedi, N.; Schalkwijk, C.G.; Stehouwer, C.D.; Ebeling, P.; Fuller, J.H. Soluble vascular cell adhesion molecule-1 and soluble E-selectin are associated with micro- and macrovascular complications in Type 1 diabetic patients. J. Diabetes Complicat. 2006, 20, 188–195. [Google Scholar] [CrossRef] [PubMed]
- Jude, E.B.; Douglas, J.T.; Anderson, S.G.; Young, M.J.; Boulton, A.J. Circulating cellular adhesion molecules ICAM-1, VCAM-1, P- and E-selectin in the prediction of cardiovascular disease in diabetes mellitus. Eur. J. Intern. Med. 2002, 13, 185–189. [Google Scholar] [CrossRef]
- Hutcheson, R.; Innes, K.; Conway, B. Perfluoroalkyl substances and likelihood of stroke in persons with and without diabetes. Diabetes Vasc. Dis. Res. 2020, 17, 1479164119892223. [Google Scholar] [CrossRef]
- Lee, S.-J.; Hong, J.M.; Lee, S.E.; Kang, D.R.; Ovbiagele, B.; Demchuk, A.M.; Lee, J.S. Association of fibrinogen level with early neurological deterioration among acute ischemic stroke patients with diabetes. BMC Neurol. 2017, 17, 101. [Google Scholar] [CrossRef]
- Sheikhbahaei, S.; Manizheh, D.; Mohammad, S.; Hasan, T.M.; Saman, N.; Laleh, R.; Mahsa, M.; Sanaz, A.K.; Shaghayegh, H.J. Can MiR-503 be used as a marker in diabetic patients with ischemic stroke? BMC Endocr. Disord. 2019, 19, 42. [Google Scholar] [CrossRef]
- Aleksandrova, K.; Drogan, D.; Weikert, C.; Schulze, M.B.; Fritsche, A.; Boeing, H.; Pischon, T. Fatty Acid-Binding Protein 4 and Risk of Type 2 Diabetes, Myocardial Infarction and Stroke: A Prospective Cohort Study. J. Clin. Endocrinol. Metab. 2019, 104, 5991–6002. [Google Scholar] [CrossRef]
- Winther, S.A.; Øllgaard, J.C.; Tofte, N.; Tarnow, L.; Wang, Z.; Ahluwalia, T.S.; Jorsal, A.; Theilade, S.; Parving, H.-H.; Hansen, T.; et al. Utility of Plasma Concentration of Trimethylamine N-Oxide in Predicting Cardiovascular and Renal Complications in Individuals with Type 1 Diabetes. Diabetes Care 2019, 42, 1512–1520. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Klipfell, E.; Bennett, B.J.; Koeth, R.A.; Levison, B.; Dugar, B.; Feldstein, A.E.; Britt, E.B.; Fu, X.; Chung, Y.-M.; et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011, 472, 57–63. [Google Scholar] [CrossRef]
- Koeth, R.A.; Wang, Z.; Levison, B.S.; Buffa, J.A.; Org, E.; Sheehy, B.T.; Britt, E.B.; Fu, X.; Wu, Y.; Li, L.; et al. Intestinal microbiota metabolism of l-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 2013, 19, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Korley, F.K.; Goldstick, J.; Mastali, M.; Van Eyk, J.E.; Barsan, W.; Meurer, W.J.; Sussman, J.; Falk, H.; Levine, D. Serum NfL (Neurofilament Light Chain) Levels and Incident Stroke in Adults with Diabetes Mellitus. Stroke 2019, 50, 1669–1675. [Google Scholar] [CrossRef] [PubMed]
- Jiao, L.; Chu, C.; Zhou, S. Prognostic value of copeptin in patients with acute stroke. Expert Rev. Neurother. 2015, 15, 563–570. [Google Scholar] [CrossRef] [PubMed]
- Katan, M.; Fluri, F.; Morgenthaler, N.G.; Schuetz, P.; Zweifel, C.; Bingisser, R.; Müller, K.; Meckel, S.; Gass, A.; Kappos, L.; et al. Copeptin: A novel, independent prognostic marker in patients with ischemic stroke. Ann. Neurol. 2009, 66, 799–808. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.-B.; Zong, M.; Lu, S.-Q.; Tian, Z. Plasma copeptin and functional outcome in patients with ischemic stroke and type 2 diabetes. J. Diabetes Complicat. 2016, 30, 1532–1536. [Google Scholar] [CrossRef] [PubMed]
- Shiga, Y.; Kuriyama, M.; Kanaya, Y.; Takeshima, S.; Takemaru, M.; Takamatsu, K.; Shimoe, Y.; Fujikawa, Y.; Nishigaki, M. Serum 1,5-Anhydroglucitol: Risk Factor of Acute Ischemic Stroke and Transient Ischemic Attack in Well-Controlled Diabetes. Cerebrovasc. Dis. 2017, 44, 325–329. [Google Scholar] [CrossRef] [PubMed]

| Trial | Duration | Participants | Drug | Dose | HR (95% Cl) | p Value |
|---|---|---|---|---|---|---|
| REWIND | 2 years | 9901 | Dulaglutide | 1.5 mg/week | 0.76 | 0.01 |
| ELIXA | 2.1 years | 6068 | Lixisenatide | 20 μg/day | 1.12 | 0.54 |
| LEADER | 3.8 years | 9340 | Liraglutide | 1.8 mg/day | 0.86 | 0.16 |
| SUSTAIN 6 | 2.1 years | 3297 | Semaglutide | 0.5 mg or 1 mg/week | 0.65 | 0.06 |
| HARMONY | 1.5 years | 9463 | Albiglutide | 30 mg or 50 mg/week | 0.86 | 0.30 |
| EMPA-REG | 3.1 years | 7020 | Empagliflozin | 10 mg or 25 mg/day | 1.18 | 0.26 |
| CANVAS | 188.2 weeks | 10,142 | Canagliflozin | 100 mg or 300 mg/day | 0.87 | 0.02 |
| Article Highlights |
|---|
Epidemiology and Risk Factors
|
| Clinical manifestations |
Pathophysiology
|
Management of hyperglycaemia during acute stroke
|
Prevention
|
| Emerging Biomarkers |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Penlioglou, T.; Stoian, A.P.; Papanas, N. Diabetes, Vascular Aging and Stroke: Old Dogs, New Tricks? J. Clin. Med. 2021, 10, 4620. https://doi.org/10.3390/jcm10194620
Penlioglou T, Stoian AP, Papanas N. Diabetes, Vascular Aging and Stroke: Old Dogs, New Tricks? Journal of Clinical Medicine. 2021; 10(19):4620. https://doi.org/10.3390/jcm10194620
Chicago/Turabian StylePenlioglou, Theano, Anca Pantea Stoian, and Nikolaos Papanas. 2021. "Diabetes, Vascular Aging and Stroke: Old Dogs, New Tricks?" Journal of Clinical Medicine 10, no. 19: 4620. https://doi.org/10.3390/jcm10194620
APA StylePenlioglou, T., Stoian, A. P., & Papanas, N. (2021). Diabetes, Vascular Aging and Stroke: Old Dogs, New Tricks? Journal of Clinical Medicine, 10(19), 4620. https://doi.org/10.3390/jcm10194620








