Abstract
Airway care interventions may prevent accumulation of airway secretions and promote their evacuation, but evidence is scarce. Interventions include heated humidification, nebulization of mucolytics and/or bronchodilators, manual hyperinflation and use of mechanical insufflation-exsufflation (MI-E). Our aim is to identify current airway care practices for invasively ventilated patients in intensive care units (ICU) in the Netherlands. A self–administered web-based survey was sent to a single pre–appointed representative of all ICUs in the Netherlands. Response rate was 85% (72 ICUs). We found substantial heterogeneity in the intensity and combinations of airway care interventions used. Most (81%) ICUs reported using heated humidification as a routine prophylactic intervention. All (100%) responding ICUs used nebulized mucolytics and/or bronchodilators; however, only 43% ICUs reported nebulization as a routine prophylactic intervention. Most (81%) ICUs used manual hyperinflation, although only initiated with a clinical indication like difficult oxygenation. Few (22%) ICUs used MI-E for invasively ventilated patients. Use was always based on the indication of insufficient cough strength or as a continuation of home use. In the Netherlands, use of routine prophylactic airway care interventions is common despite evidence of no benefit. There is an urgent need for evidence of the benefit of these interventions to inform evidence-based guidelines.
1. Introduction
Critically ill patients receiving invasive ventilation are at risk for retention of airway secretions [1]. The relatively dry gases used during invasive ventilation cause mucosa in the airways to produce more mucus. Moreover, the presence of the endotracheal tube hampers mucociliary clearance [1,2]. Critically ill patients frequently have an impaired cough reflex due to depressed levels of consciousness, sedation, or muscle weakness. For these reasons, intensive care nurses apply interventions that help with evacuation of airway secretions in patients receiving invasive ventilation.
Within the domain of intensive care nursing, several interventions aiming at prevention of airway secretion accumulation or promotion of airway secretion evacuation have become part of daily care for critically ill invasively ventilated patients. Active humidification i.e., use of heated humidification, helps to prevent production and thickening of airway secretions [3]. Nebulization of mucoactive agents is thought to reduce accumulation of thick and sticky airway secretions [4]. Mucoactive agents are often used in combination with bronchodilators to enhance mobilization of mucus by opening the airways [5,6,7]. Manual hyperinflation [8,9,10] or mechanical in–exsufflation (MI–E), (commonly referred to as cough assist) [8,11,12], may be helpful techniques in mobilizing airway secretions from smaller to larger airways, where it can be removed using suctioning. In the Netherlands, these interventions are mainly performed by intensive care nurses, while involvement by physiotherapists is rare; they focus more on the traditional rehabilitation procedures. Despite common, and in some cases daily use of these airway care interventions, there is a remarkable lack of evidence for clinical benefit [10,12,13,14]. Current practice guidelines [15,16] are primarily based on expert opinion. This lack of evidence may lead to variable use of airway care interventions in daily practice based on local preferences. Our objective was to determine current airway care practices within the domain of intensive care nursing for (1) heated humidification; (2) nebulization therapy; (3) manual hyperinflation; and (4) MI-E in adult intensive care units (ICUs) in the Netherlands. A secondary objective was to investigate perceptions of safety, necessity, and efficacy of these interventions. Our hypothesis was that current practice of, and perceptions towards airway care interventions would be highly variable due to the lack of evidence.
2. Materials and Methods
2.1. Study Design
We used a self–report web–based cross-sectional survey design.
2.2. Survey Development and Formatting
The research team, with extensive experience in invasive ventilation and airway care for critically ill patients, iteratively developed the survey. We generated potential items by searching for relevant studies in the MEDLINE and Cochrane databases. During the selection of items we focused on interventions within the domain of intensive care nursing. We did not include chest physiotherapy, like rib cage compression and other techniques aimed at flow augmentation. Previous surveys on this topic were also used to generate items [9,17]. Item reduction occurred through discussion among the research team.
This survey comprised of 58 items, four related to ICU demographics and the remainder grouped within the airway care interventions of interest. We used skip logic when appropriate to enable provision of questions based on participant responses to preceding questions. Questions comprised intensity of use, indications and contraindications, specifics on how the intervention was applied, and how ICU team members were trained in the interventions. For MI-E, we asked additional questions on years of experience with its use in their ICU, who would prescribe and/or apply MI-E, and barriers to use. Intensity of use consisted of three categories. (1) “Routine”, defined as an intervention used prophylactically in all invasively ventilated patients and ordered with a set frequency per day; (2) “on indication”, defined as initiated based on individual patient clinical characteristics; (3) “never”, defined as never used in their ICU.
Perceptions on the safety, necessity, or efficacy of airway interventions were assessed using six statements with a visual analogue scale ranging from 0 to 100 mm.
2.3. Survey Pilot Testing
The survey was loaded on to SurveyMonkeyTM [18] and was pilot tested by four ICU nurses and one intensivist from 3 different hospitals [19]. All four had experience in ICU for more than 5 years and were currently working clinically. Every pilot tester returned a checklist after testing with questions on face and construct validity including clarity, redundancy, and completeness of items; suggestions for additional items required time to complete. After pilot testing minor revisions were made, skip logic was corrected, and pictures of nebulizer types were added for clarity.
2.4. Sample
Our sample comprised all adult ICUs in the Netherlands. We contacted each ICU by telephone in November 2017 to identify one senior healthcare professional who would take responsibility for survey completion on behalf of their ICU. This person was responsible for invasive ventilation policy and procedures, and either an ICU nurse, advanced ventilation nurse specialist, or physician. Advanced ventilation nurse specialists complete an additional education 14 month program on mechanical ventilation 240 study hours: 1.4 European Credit Transfer and Accumulation System (ECTS).
2.5. Survey Administration
We sent an email with instructions and the secure survey link to participants on March 2018, with 3 survey completion reminders sent over 6 weeks. Survey instructions explicitly stated the respondent was to report on current practices in their ICU (i.e., not their personal preferences). For statements regarding perceptions of the efficacy and safety of airway care interventions, we instructed respondents to provide their personal view.
2.6. Analysis Plan
Frequencies and proportions were used to describe categorical data. Proportions were reported as percentages. A heat map was constructed to visualize the variability in practice of airway care interventions [20]. Airway care interventions and intensity of their use were displayed. Perceptions of respondents on statements were visualized in boxplots with means and interquartile ranges. A score of 50 was used as a threshold for agreement or disagreement. In a posthoc analysis, differences in use of airway care interventions were compared between academic-teaching hospitals and general hospitals, as well as in ICUs with ≤20 beds compared to >20 beds. In addition, associations of hospital type or ICU size on the use of airway care interventions were explored by separate logistic regression models (e-supplement). Analyses were performed using SPSS (IBM SPSS Statistics 25) and R language and environment for statistical computing [21].
2.7. Ethical Considerations
The Institutional Review Board of the Amsterdam University Medical Centers, confirmed that the Medical Research Involving Humans Subjects Acts (WMO) did not apply, waiving the need for official approval (W18_024#18.035). Survey participation was voluntary and consent was implied through return of survey.
3. Results
3.1. Participants and Responses
All 85 ICUs in the Netherlands expressed interest in participation of whom 72/85 (85%) provided survey responses. Individuals responding on behalf of their ICUs were most commonly nurses (66/72, 92%); of whom 35/72 (49%) were advanced ventilation nurse specialists (Table 1). All ICUs were mixed medical/surgical, and both academic and non-academic hospitals were represented in the survey responses.

Table 1.
Demographic characteristics of respondents and Dutch ICUs (N = 72).
3.2. Airway Care Practices
Airway care intervention combinations used in each ICU are displayed as a heatmap (Figure 1). We found substantial heterogeneity across ICUs in intervention combinations and in the intensity of their use (i.e., routine, as indicated or never).

Figure 1.
Heatmap airway care interventions in Dutch ICUs (N = 72). Current practice of heated humidification (HH), nebulization therapy, manual hyperinflation (MH) and MI-E in Dutch ICUs is graphically displayed in a heatmap. Each vertical bar is one ICU. Intensity of use of the airway care interventions is visualized by different shadings of grey according to the legend.
3.3. Heated Humidification
Most ICUs (58/72, 81%) reported prophylactic use of heated humidification as a routine intervention in all invasively ventilated patients. A minority (11/72, 15%) used heated humidification as an ‘on indication’ treatment, with the indication defined as presence of viscous mucus. Few (3/72, 4%) ICUs never used heated humidification.
3.4. Nebulization Therapy
All responding ICUs reported using nebulization of bronchodilators and/or mucolytics. In 43% (31/72) this was as a routine prophylactic intervention for bronchospasm and mucus retention with 74% (23/31) reporting routine prophylactic nebulization therapy 4 times daily. Nine (29%) of these 31 ICUs reported more frequent administration. When used “on indication”, bronchospasm or audible wheeze were the most commonly reported indications. Bronchodilators were the most commonly used drug class, independent of intensity of use. Metered dose inhalers (MDI) (37/72, 51%) or jet nebulizers (40/72, 56%) were most frequently used for nebulization therapy. Details on indications, contraindications and medication used are provided in Table 2 and Figure 1.

Table 2.
Airway care interventions.
Although nebulization therapy was used in all responding ICUs, perception as to efficacy (17%) or necessity (28%) of prophylactic nebulization was low. Those ICUs using nebulization as a routine prophylactic intervention perceived efficacy to be higher than respondents from ICUs that used nebulization only on clinical indication (Figure 2).
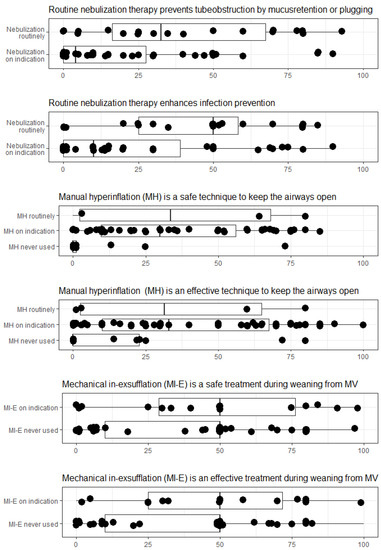
Figure 2.
Perceptions of efficacy and safety of airway care interventions. Respondents could rate their perceptions on safety and efficacy of airway care interventions on a visual analogue scale from 0 (totally disagree) to 100 (totally agree). Results are grouped by reported intensity of use in their ICU.
3.5. Manual Hyperinflation
Most responding ICUs (58/72, 81%) reported using manual hyperinflation; most commonly (53/72, 74%) as on indication only. Those ICUs identified indications to include difficult oxygenation, presumed mucus presence, and decreased tidal volume. Unstable hemodynamics and active pneumothorax were the most important contraindications. Ten ICUs (10/58, 17%) reported to have no contraindications to manual hyperinflation.
Most ICUs reported using a Mapleson CTM circuit (41/58, 71%) for manual hyperinflation. Forty-three ICUs (74%) indicated an expiration valve was used to adjust PEEP. Twenty-five ICUs (43%) ICUs using manual hyperinflation stated a predefined PEEP target was set. Few (10/58, 17%) ICUs reported using a manometer in the circuit to measure and control for high peak airway pressures. Details on indications, contraindications and materials used for manual hyperinflation are provided in Table 2 and Figure 1. Most respondents disagreed with the statement manual hyperinflation to be a safe (74%) or effective (64%) airway care intervention in invasively ventilated patients, independent of local use. (Figure 2).
3.6. Mechanical Insufflation-Exsufflation
Few (16/72, 21%) ICUs reported using MI-E, with use only in response to a clinical indication such as insufficient cough strength (16/16,100%) or use of MI-E at home (10/16, 63%). MI-E was applied 2 to 3 times daily or more depending on clinical indication. Intensivists were the primary MI-E prescriber (14/16, 88%) but MI-E was applied by all ICU team members; mostly ICU nurses (15/16, 94%) and advanced ventilation nurse specialists (8/16, 50%). Years of MI-E use in the ICU setting ranged from very recent (<1 year) (3/16, 19% ICUs), 1–5 years (9/16, 56% ICUs), and 6–10 years (4/16, 25% ICUs). The majority of respondents disagreed that MI-E is a safe (75%) or effective (75%) intervention in all invasive ventilated patients, independent of local use. (Figure 2). Details on reported MI-E practices are provided in Table 2 and Figure 1.
3.7. Training and Education
Most respondents described having a local protocol for nebulization therapy (57/72, 79%), manual hyperinflation (35/58, 60%) and MI-E (12/16, 75%). In 25 of the 59 (46%) ICUs that used manual hyperinflation, nurses received annual training from an expert colleague. Bedside training was the most frequently employed education method for manual hyperinflation (35/58, 60%) and MI-E (12/16, 75%).
In the post hoc analysis no differences were found in use of airway care interventions between type of hospitals or size of ICU (Supplementary Tables S1 and S2). Both types of hospitals, academic-teaching and general hospitals were associated with routine use of heated humidification. The size of the ICU was not associated with its use. There were no associations of hospital type or ICU-size regarding the use of nebulization therapy. Both general and academic-teaching hospitals showed a positive association with manual hyperinflation use and ICUs > 20 beds were associated with more manual hyperinflation use. Both hospital types were associated with low use of MI-E. There was no association with size of ICU regarding MI-E (Supplementary Table S3).
4. Discussion
This is the first survey describing current practice of four airway care interventions within the domain of intensive care nursing for adult patients admitted to an ICU in the Netherlands. The main findings of this survey indicate substantial heterogeneity regarding the combination of airway care interventions and their intensity of use, regardless of hospital type or ICU size. This means the type of airway care received by patients depends on where in the Netherlands they are admitted.
This survey reports a high proportion of ICUs using heated humidification as routine prophylactic therapy for all ventilated patients. This is in line with previous studies in other countries [6,8,22]. However, heated humidification may not only increase workload and cost [23], but may also not be more effective compared to heat and moisture exchangers (HME) in prevention of complications. A 2017 Cochrane systematic review suggests no difference in the incidence of artificial airway occlusion, pneumonia or mortality comparing heated humidification to HME in adults and children [13]. A second systematic review in critically ill adults only confirms these findings [24]. Our data suggest knowledge translation work is needed in the Netherlands to change airway care practice from routine prophylactic use of heated humidification in all ventilated patients to use of HMEs.
Use of routine prophylactic nebulization therapy in all ventilated patients was reported by 43% of responding ICUs. Again, evidence to support this practice is limited. This practice also increases costs and nursing workload. One multi-centre randomized controlled trial comparing routine nebulization of mucolytics and bronchodilators with nebulization only on indication, showed no difference in the number of days alive and ventilator free [14]. In addition, medication side effects such as agitation occurred more frequently with prophylactic nebulizer use [14].
Our results show that manual hyperinflation is commonly used in the Netherlands, both as a routine prophylactic intervention or as indicated. However, the number of ICUs reporting its use has declined since a previous survey in 2009 [9]. Although alveolar recruitment and mobilization of airway secretions are cited as benefits of manual hyperinflation [10], efficacy as a routine prophylactic intervention in all invasively ventilated patients is not confirmed by evidence [25]. Furthermore, manual hyperinflation is a difficult technique to perform and, as such, may potentially harm the patient [26]. Concerns about safety of manual hyperinflation were reflected by our survey respondents.
We found use of MI-E in invasively ventilated patients uncommon in the Netherlands (21%) compared to Canada (64% of the ICUs) [17] and the United Kingdom (98% of the ICUs) [27]. These surveys report MI-E to be used for invasively ventilated patients during weaning from invasive ventilation [17,27]. There appears to be increasing adoption of MI-E for invasively ventilated patients outside the Netherlands possibly due to the need for a safe and effective way to mobilize mucus from the lower airways. However, further research is needed as to the efficacy of MI-E in invasively ventilated critically ill patients [12].
Strength and Limitations
Strength of our study is the excellent response rate meaning our data are highly generalizable to the current practice of airway care interventions of ICUs in the Netherlands. Our response rate can be attributed to following survey conduct recommendations [19], including contact by telephone prior to the survey distribution, and identification of a key respondent. Study limitations pertain to the use of a web-based self-report survey. First, by having one individual report on the practice of an ICU, responses may be reflective of perceived versus actual practice or relate to the individual’s practice rather than that of the ICU. Second, the questionnaire was designed using previous reports of airway care interventions with a focus on the domain of intensive care nursing [9,17]. Third, since we only included respondents from the Netherlands and focused on the interventions within the domain of intensive care nursing, we cannot report on other interventions applied by other health care professionals, e.g., physiotherapists. The organization of care within the intensive care differs between countries and therefore our results may be not generalizable to other countries.
5. Conclusions
Our survey indicates that in the Netherlands, use of prophylactic airway care interventions for heated humidification and nebulization in all invasively ventilated patients is common despite evidence of no benefit. Manual hyperinflation is frequently used, while only a minority of ICUs report using MI-E. Substantial heterogeneity exists with regard to the combination of airway care interventions and their intensity of use. The current lack of evidence and guidelines in airway care may be a reason for the heterogeneous practices we report. There is an urgent need for evidence of the benefit of these interventions, particularly when used as a routine prophylactic intervention, to inform evidence based guidelines.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10153381/s1, Table S1: Proportions and their differences, Table S2: Basics of the proportions, Table S3: Models and predictors.
Author Contributions
Conceptualization, W.S., S.M.v.d.H., F.P., L.R., M.J.S., W.J.M.S.o.R.; methodology, W.S., S.M.v.d.H., F.P., L.R., M.J.S., W.J.M.S.o.R.; software, W.S., S.M.v.d.H.; formal analysis, W.S., S.M.v.d.H., F.P.; writing—original draft preparation, W.S. and S.M.v.d.H.; writing—review and editing, F.P., L.R., M.J.S., W.J.M.S.o.R.; visualization, W.S.; supervision, L.R. and F.P.; project administration, W.S.; funding acquisition, W.S., F.P., M.J.S. All authors have read and agreed to the published version of the manuscript.
Funding
This work was funded by a personal (PhD fellowship) grant (WS) from NWO Netherlands Organisation for Scientific Research, number 023.011.016.
Institutional Review Board Statement
The Institutional Review Board of the Amsterdam University Medical Centers, confirmed that the Medical Research Involving Humans Subjects Acts (WMO) did not apply, waiving the need for official approval (W18_024#18.035).
Informed Consent Statement
Survey participation was voluntary and consent was implied through return of survey.
Data Availability Statement
The survey is in Dutch. Data are available on request with the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Fahy, J.V.; Dickey, B.F. Airway Mucus Function and Dysfunction. N. Engl. J. Med. 2010, 363, 2233–2247. [Google Scholar] [CrossRef] [Green Version]
- Konrad, F.; Schreiber, T.; Brecht-Kraus, D.; Georgieff, M. Mucociliary Transport in ICU Patients. Chest 1994, 105, 237–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Restrepo, R.D.; Walsh, B.K.; American Association for Respiratory Care. Humidification during invasive and noninvasive mechanical ventilation. Respir. Care 2012, 57, 782–788. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Konrad, F.; Schoenberg, M.H.; Wiedmann, H.; Kilian, J.; Georgieff, M. The application of n-acetylcysteine as an antioxidant and mucolytic in mechanical ventilation in intensive care patients. A prospective, randomized, placebo-controlled, double-blind study. Der. Anaesthesist 1995, 44, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Ehrmann, S.; Roche-Campo, F.; Papa, G.F.S.; Isabey, D.; Brochard, L.; Apiou-Sbirlea, G.; For the REVA Research Network. Aerosol therapy during mechanical ventilation: An international survey. Intensiv. Care Med. 2013, 39, 1048–1056. [Google Scholar] [CrossRef]
- Grivans, C.; Lindgren, S.; Aneman, A.; Stenqvist, O.; Lundin, S. A Scandinavian survey of drug administration through inhalation, suctioning and recruitment maneuvers in mechanically ventilated patients. Acta Anaesthesiol. Scand. 2009, 53, 710–716. [Google Scholar] [CrossRef]
- Zhang, Z.; Xu, P.; Fang, Q.; Ma, P.; Lin, H.; Fink, J.B.; Liang, Z.; Chen, R.; Ge, H.; China Union of Respiratory Care (CURC). Practice pattern of aerosol therapy among patients undergoing mechanical ventilation in mainland China: A web-based survey involving 447 hospitals. PLoS ONE 2019, 14, e0221577. [Google Scholar] [CrossRef] [Green Version]
- Ntoumenopoulos, G.; Hammond, N.; Watts, N.R.; Thompson, K.; Hanlon, G.; Paratz, J.D.; Thomas, P. Secretion clearance strategies in Australian and New Zealand Intensive Care Units. Aust. Crit. Care 2018, 31, 191–196. [Google Scholar] [CrossRef]
- Paulus, F.; Binnekade, J.M.; Middelhoek, P.; Schuitz, M.J.; Vroom, M.B. Manual hyperinflation of intubated and mechanically ventilated patients in Dutch intensive care units—A survey into current practice and knowledge. Intensiv. Crit. Care Nurs. 2009, 25, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Paulus, F.; Binnekade, J.M.; Vroom, M.B.; Schultz, M.J. Benefits and risks of manual hyperinflation in intubated and mechanically ventilated intensive care unit patients: A systematic review. Crit. Care 2012, 16, R145. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bach, J.R. Mechanical insufflation-exsufflation: Comparison of peak expiratory flows with manually assisted and unassisted coughing techniques. Chest 1993, 104, 1553–1562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rose, L.; Adhikari, N.K.; Leasa, D.; A Fergusson, D.; McKim, D. Cough augmentation techniques for extubation and weaning critically ill patients from mechanical ventilation. Cochrane Database Syst. Rev. 2015, 1:CD011833. [Google Scholar] [CrossRef]
- Gillies, D.; A Todd, D.; Foster, J.P.; Batuwitage, B.T. Heat and moisture exchangers versus heated humidifiers for mechanically ventilated adults and children. Cochrane Database Syst. Rev. 2017, 2017, CD004711. [Google Scholar] [CrossRef] [PubMed]
- van Meenen, D.M.P.; van der Hoeven, S.M.; Binnekade, J.M. Effect of On-Demand vs Routine Nebulization of Acetylcysteine With Salbutamol on Ventilator-Free Days in Intensive Care Unit Patients Receiving Invasive Ventilation: A Randomized Clinical Trial. JAMA 2018, 319, 993–1001. [Google Scholar] [CrossRef] [Green Version]
- American Association for Respiratory Care. AARC Clinical Practice Guidelines. Endotracheal suctioning of mechanically ventilated patients with artificial airways. Respir Care 2010, 55, 758–764. [Google Scholar]
- Strickland, S.L.; Rubin, B.K.; Drescher, G.S.; Haas, C.F.; O’Malley, C.A.; Volsko, T.A.; Branson, R.D.; Hess, D.R. AARC Clinical Practice Guideline: Effectiveness of Nonpharmacologic Airway Clearance Therapies in Hospitalized Patients. Respir. Care 2013, 58, 2187–2193. [Google Scholar] [CrossRef] [Green Version]
- Rose, L.; Adhikari, N.K.; Poon., J.; Leasa, D.; McKim, D.A.; Group, C.A. Cough Augmentation Techniques in the Critically Ill: A Canadian National Survey. Respir Care 2016, 61, 1360–1368. [Google Scholar] [CrossRef] [PubMed]
- SurveyMonkey Audience hnsc. Momentive Inc. Location: San Mateo, California, USA. Available online: www.surveymonkey.com/mp/audience (accessed on 26 May 2021).
- Burns, K.E.; Duffett, M.; Kho, M.; Meade, M.O.; Adhikari, N.K.; Sinuff, T.; Cook, D.J.; for the ACCADEMY Group. A guide for the design and conduct of self-administered surveys of clinicians. Can. Med Assoc. J. 2008, 179, 245–252. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Engle, S.; Whalen, S.; Joshi, A.; Pollard, K.S. Unboxing cluster heatmaps. BMC Bioinform. 2017, 18, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- RC Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017; Available online: https://www.R-project.org/ (accessed on 26 May 2021).
- Cook, D.; Ricard, J.-D.; Reeve, B.; Randall, J.; Wigg, M.; Brochard, L.; Dreyfuss, D. Ventilator circuit and secretion management strategies: A Franco-Canadian survey. Crit. Care Med. 2000, 28, 3547–3554. [Google Scholar] [CrossRef] [PubMed]
- Menegueti, M.G.; Auxiliadora-Martins, M.; Nunes, A.A. Cost-Effectiveness Analysis of Heat and Moisture Exchangers in Mechanically Ventilated Critically Ill Patients. Anesthesiol. Pain Med. 2016, 6, ee32602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vargas, M.; Chiumello, D.; Sutherasan, Y.; Ball, L.; Esquinas, A.M.; Pelosi, P.; Servillo, G. Heat and moisture exchangers (HMEs) and heated humidifiers (HHs) in adult critically ill patients: A systematic review, meta-analysis and meta-regression of randomized controlled trials. Crit. Care 2017, 21, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tucci, M.R.; Nakamura, M.A.; Carvalho, N.C.; Volpe, M.S. Manual Hyperinflation: Is It Effective? (editorial). Respir Care 2019, 64, 870–873. [Google Scholar] [CrossRef] [PubMed]
- Paulus, F.; Binnekade, J.M.; Middelhoek, P.; Vroom, M.B.; Schultz, M.J. Performance of manual hyperinflation: A skills lab study among trained intensive care unit nurses. Med Sci. Monit. 2009, 15, CR418–CR422. [Google Scholar] [PubMed]
- Swingwood, E.; Tume, L.; Cramp, F. A survey examining the use of mechanical insufflation-exsufflation on adult intensive care units across the UK. J. Intensiv. Care Soc. 2020, 21, 283–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).