Efficacy of Manual Therapy and Transcutaneous Electrical Nerve Stimulation in Cervical Mobility and Endurance in Subacute and Chronic Neck Pain: A Randomized Clinical Trial
Abstract
1. Introduction
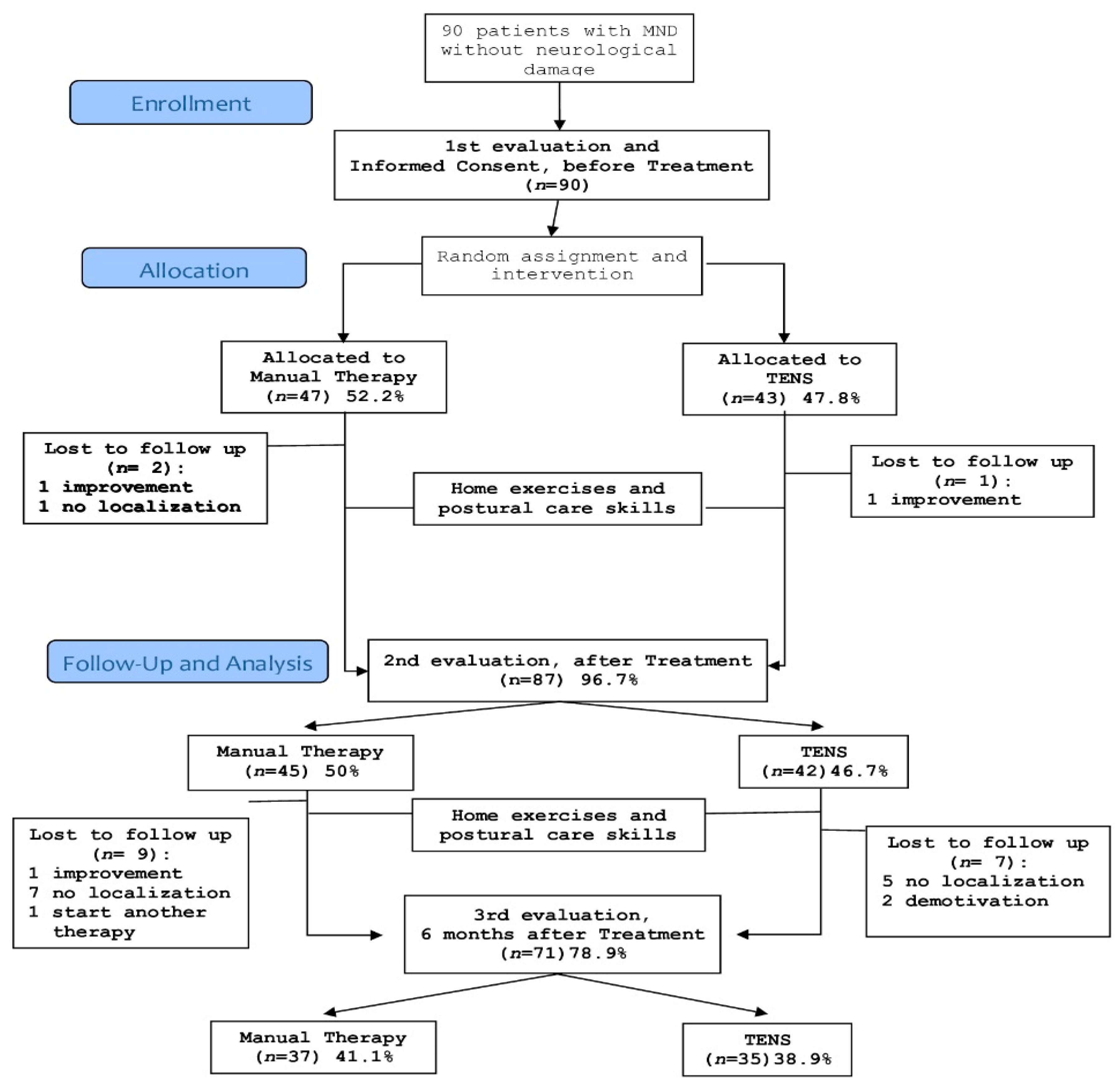
2. Materials and Methods
2.1. Study Design
2.2. Patients
2.3. Sample Size Determination
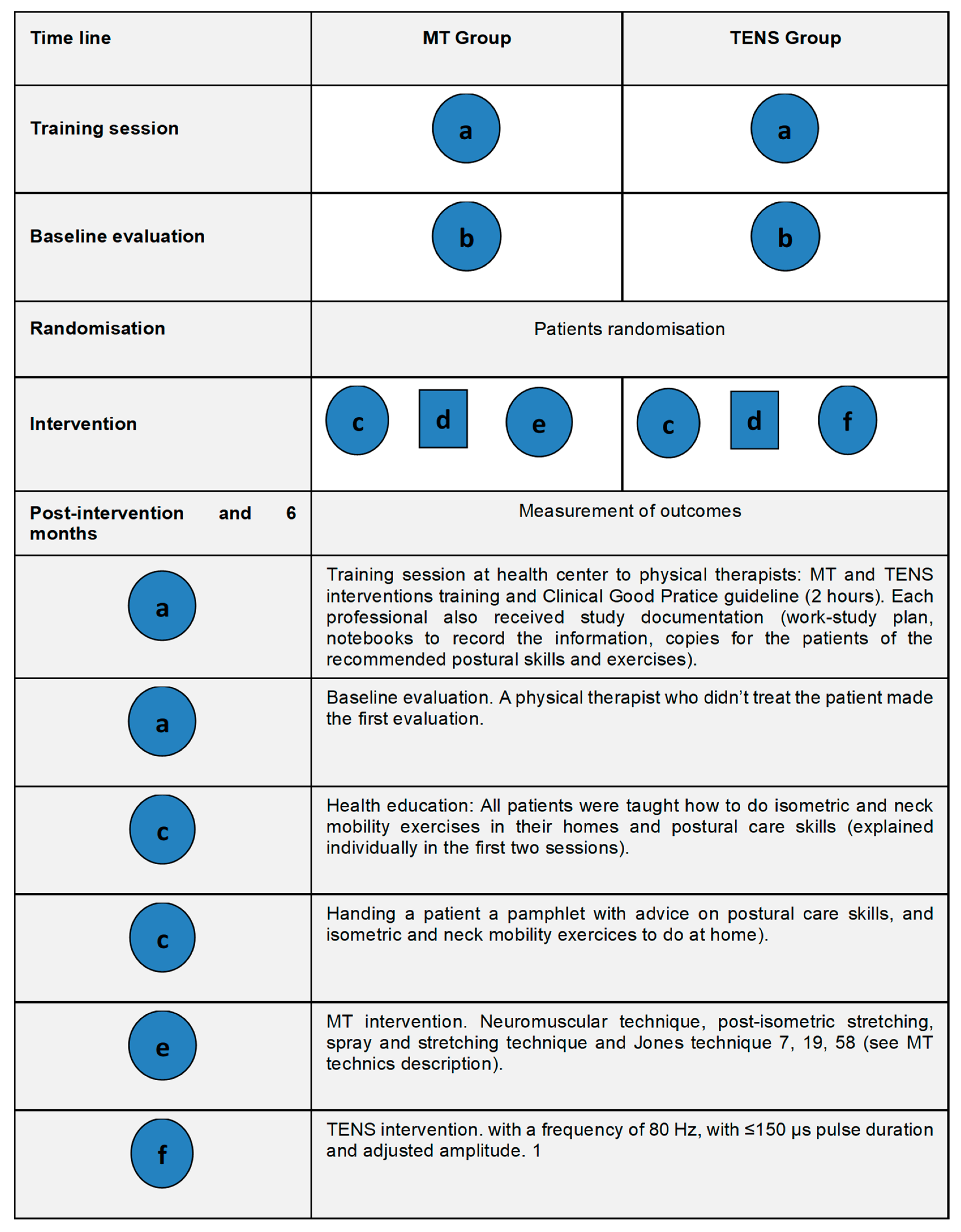
2.4. Interventions
2.5. Outcome Measures
2.6. Subject Follow up
2.7. Data Analysis
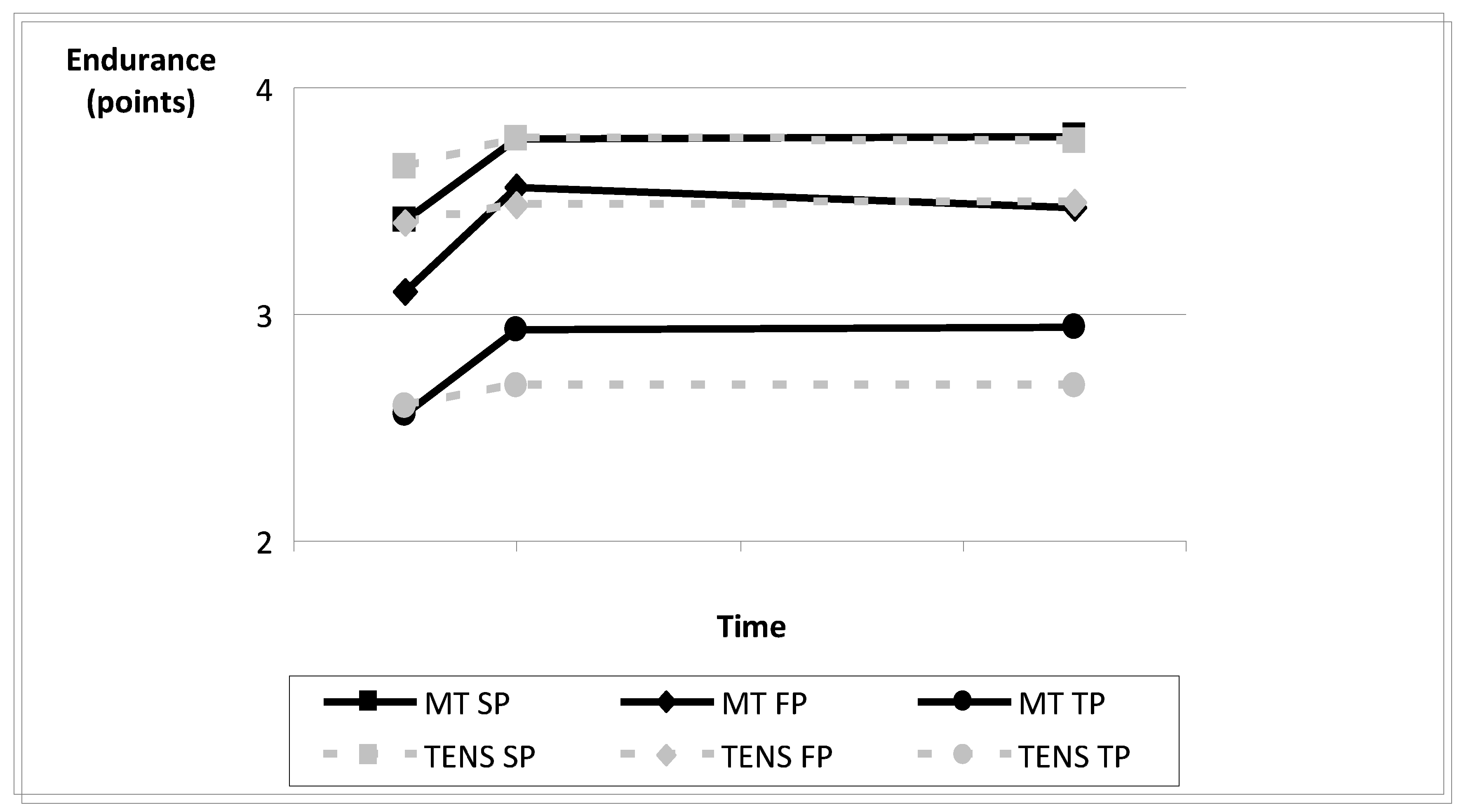
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Aker, P.D.; Gross, A.R.; Goldsmith, C.H.; Peloso, P. Conservative management of mechanical neck pain: Systematic overview and meta-analysis. BMJ 1996, 313, 1291–1296. [Google Scholar] [CrossRef] [PubMed]
- Brosseau, L.; Wells, G.A.; Tugwell, P.; Casimiro, L.; Novikov, M.; Loew, L.; Sredic, D.; Clément, S.; Gravelle, A.; Hua, K.; et al. Ottawa panel evidence-based clinical practice guidelines on therapeutic massage for neck pain. J. Bodyw. Mov. Ther. 2012, 16, 300–325. [Google Scholar] [CrossRef] [PubMed]
- Guzman, J.; Haldeman, S.; Carroll, L.J.; Carragee, E.J.; Hurwitz, E.L.; Peloso, P.; Nordin, M.; Cassidy, J.D.; Holm, L.W.; Côté, P.; et al. Clinical practice implications of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. Eur. Spine J. 2008, 17, 199–213,. [Google Scholar] [CrossRef]
- Bier, J.D.; Scholten-Peeters, W.G.M.; Staal, J.B.; Pool, J.; van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical Practice Guideline for Physical Therapy Assessment and Treatment in Patients With Nonspecific Neck Pain. Phys. Ther. 2018, 98, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Borghouts, J.A.; Koes, B.A.; Vondeling, H.; Bouter, L.M. Cost-of-illness of neck pain in The Netherlands in 1996. Pain 1999, 80, 629–636. [Google Scholar] [CrossRef]
- Gross, A.R.; Kay, T.; Hondras, M.; Goldsmith, C.; Haines, T.; Peloso, P.; Kennedy, C.; Hoving, J. Manual therapy for mechanical neck disorders: A systematic review. Man. Ther. 2002, 7, 131–149. [Google Scholar] [CrossRef]
- Viljanen, M.; Malmivaara, A.; Uitti, J.; Rinne, M.; Palmroos, P.; Laippala, P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: Randomised controlled trial. BMJ 2003, 327, 475–479. [Google Scholar] [CrossRef]
- Gross, A.R.; Hoving, J.L.; Haines, T.A.; Goldsmith, C.H.; Kay, T.; Aker, P.; Bronfort, G.; Cervical Overview Group. Movilización Activa y Pasiva Para Trastornos Mecánicos de Cuello. In Cochrane Library Plus En Español Oxford: Update Software; Wiley: New York, NY, USA, 2003. [Google Scholar]
- Gross, A.R.; Aker, P.D.; Goldsmith, C.H.; Peloso, P. Physical Medicine Modalities for Mechanical Neck Disorders. Cochrane Database Syst. Rev. 2000, CD000961. [Google Scholar] [CrossRef]
- Ezzo, J.; Haraldsson, B.G.; Gross, A.R.; Myers, C.D.; Morien, A.; Goldsmith, C.H.; Bronfort, G.; Peloso, P.M. Massage for mechanical neck disorders: A systematic review. Spine 2007, 32, 353–362. [Google Scholar] [CrossRef]
- Hogg-Johnson, S.; van der Velde, G.; Carroll, L.J.; Holm, L.W.; Cassidy, J.D.; Guzmán, J.; Côté, P.; Haldeman, S.; Ammendolia, C.; Carragee, E.; et al. The Burden and Determinants of Neck Pain in the General Population. Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, 39–51. [Google Scholar] [CrossRef]
- Vernon, H.; Humphreys, B.K. Chronic mechanical neck pain in adults treated by manual therapy: A systematic review of change scores in randomized controlled trials of a single session. J. Manip. Physiol. Ther. 2008, 16, E42–E52. [Google Scholar] [CrossRef] [PubMed]
- Zaproudina, N.; Hänninen, O.O.; Airaksinen, O. Effectiveness of traditional bone setting in chronic neck pain: Randomized clinical trial. J. Manip. Physiol. Ther. 2007, 30, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Bussières, A.E.; Stewart, G.; Al-Zoubi, F.; Decina, P.; Descarreaux, M.; Hayden, J.; Hendrickson, B.; Hincapié, C.; Pagé, I.; Passmore, S.; et al. The Treatment of Neck Pain-Associated Disorders and Whiplash-Associated Disorders: A Clinical Practice Guideline. J. Manip. Physiol. Ther. 2016, 39, 523–564. [Google Scholar] [CrossRef] [PubMed]
- Farì, G.; Santagati, D.; Pignatelli, G.; Scacco, V.; Renna, D.; Cascarano, G.; Vendola, F.; Bianchi, F.P.; Fiore, P.; Ranieri, M.; et al. Collagen Peptides, in Association with Vitamin C, Sodium Hyaluronate, Manganese and Copper, as Part of the Rehabilitation Project in the Treatment of Chronic Low Back Pain. Endocr. Metab. Immune Disord Drug Targets 2021, 21. [Google Scholar] [CrossRef]
- Haldeman, S.; Carroll, L.; Cassidy, J.D.; Schubert, J.; Nygren, A. The Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: Executive summary. Spine 2008, 33, S5–S7. [Google Scholar] [CrossRef]
- Nestares, T.; Salinas, M.; de-Teresa, C.; Diaz-Castro, J.; Moreno-Fernandez, J.; Lopez-Frias, M. Factores de riesgo relacionados con los hábitos de vida en pacientes con patología osteomuscular. Nutr. Hosp. 2017, 34, 444–453. [Google Scholar] [CrossRef]
- Meseguer Henarejos, B.; Medina i Mirapeix, F.; Canovas Gascón, J.J.; Esteban Argente, I.; Torres Vaquero, A.I.; Alcántara, F. Prevalencia, consecuencias y factores de riesgo de la cervicalgia. Fisioterapia 2000, 22, 13–32. [Google Scholar]
- Dalewski, B.; Kaminska, A.; Szydlowski, M.; Kozak, M.; Sobolewska, E. Comparison of Early Effectiveness of Three Different Intervention Methods in Patients with Chronic Orofacial Pain: A Randomized Controlled Clinical Trial. Pain Res. Manag. 2019, 11, 7954291. [Google Scholar] [CrossRef]
- Adel, R.V.; Luykx, R.H.J. Electroterapia de Frecuencia Baja y Media; Enraf Nonius: Madrid, España, 1996. [Google Scholar]
- Escortell-Mayor, E.; Lebrijo-Pérez, G.; Asúnsolo-del-Barco, A.; Sánchez-Sánchez, B. Difficulties in carrying out public projects of investigation in primary care. Atención Primaria 2008, 40, 536–537. [Google Scholar] [CrossRef][Green Version]
- Girardin, M. Terapia Manual de La Disfunción Neuromuscular y Articular; Paidotribo: Barcelona, Spain, 2004; ISBN 9788480193702. [Google Scholar]
- Gross, A.R.; Aker, P.D.; Quartly, C. Manual therapy in the treatment of neck pain. Rheum. Dis. Clin. 1996, 22, 579–598. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Aker, P.D.; Adams, A.H.; Meeker, W.C.; Shekelle, P.G. Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine 1996, 21, 1746–1758. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Turner, J.A.; Romano, J.M.; Fisher, L.D. Comparative reliability and validity of chronic pain intensity measures. Pain 1999, 83, 157–162. [Google Scholar] [CrossRef]
- Ylinen, J.; Takala, E.P.; Nykanen, M.J.; Kautlainen, H.J.; Häkkinen, A.; Airaksinen, O.V.P. Effects of twelve-month strength training subsequent to twelve-month stretching exercise in treatment of chronic neck pain. J. Strength Cond. Res. 2006, 20, 304–308. [Google Scholar] [CrossRef]
- Medina i Mirapeix, F.; Meseguer Henarejos, A.B.; Montilla Herrador, J. Clinical Practice Guideline for the mechanical neck pain physiotherapy treatment [Guía de práctica clínica para el tratamiento y seguimiento fisioterápico de la cervicalgia mecánica]. Fisioterapia 2000, 22, 33–46. [Google Scholar]
- Escortell Mayor, E.; Pérez Muñoz, M.; Martín Castro, B. Guía de Actuación: Procedimientos de Intervención de Fisioterapia en Atención Primaria Área 3; Gerencia de Atención Primaria Área 3 Servicio Madrileño de Salud: Madrid, Spain, 2010. [Google Scholar]
- Fernández Moreno, R. coordinador. Indicadores de actividad. In Procesos Susceptibles de Atención y Técnicas de Tratamiento En Las Unidades de Fisioterapia de Atención Primaria; Servicio Madrileño de Salud: Comunidad de Madrid, Spain, 2014. [Google Scholar]
- Gerencia Asistencial de Atención Primaria, Consejería de Sanidad. Cartera de Servicios Estandarizados de Atención Primaria de Madrid; Gerencia Asistencial de Atención Primaria: Madrid, Spain, 2018. [Google Scholar]
- Binder, A. Neck pain. BMJ 2006, 11, 1103–1124. [Google Scholar]
- Hoving, J.L.; Gross, A.R.; Gasner, D.; Kay, T.; Kennedy, C.; Hondras, M.A.; Haines, T.; Bouter, L.M. A critical appraisal of review articles on the effectiveness of conservative treatment for neck pain. Spine 2001, 26, 196–205. [Google Scholar] [CrossRef]
- Kroeling, P.; Gross, A.R.; Goldsmith, C.H. A Cochrane review of electrotherapy for mechanical neck disorders. Spine 2005, 30, E641–E648. [Google Scholar] [CrossRef] [PubMed]
- Guzman, J.; Haldeman, S.; Carroll, L.J.; Carragee, E.J.; Hurwitz, E.L.; Peloso, P.; Nordin, M.; Cassidy, J.D.; Holm, L.W.; Côté, P.; et al. Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and its associated disorders: From concepts and findings to recommendations. Spine 2008, 33, S199–S213. [Google Scholar] [CrossRef] [PubMed]
- Häkkinen, A.; Salo, P.; Tarvainen, U.; Wirén, K.; Ylinen, J. Effect of manual therapy and stretching on neck muscle strength and mobility in chronic neck pain. J. Rehabil. Med. 2007, 39, 575–579. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, J.; Kautiainen, H.; Wirén, K.; Häkkinen, A. Stretching exercises vs manual therapy in treatment of chronic neck pain: A randomized, controlled cross-over trial. J. Rehabil Med. 2007, 39, 126–132. [Google Scholar] [CrossRef]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K. Neck Pain: Revision 2017. J. Orthop Sports Phys. Ther. 2017, 47, A1–A83. [Google Scholar] [CrossRef] [PubMed]
- De Koning, C.H.; van den Heuvel, S.P.; Staal, J.B.; Smits-Engelsman, B.C.; Hendriks, E.J. Clinimetric evaluation or active range of motion measures in patients with non-specific pain: A systematic review. Eur. Spine J. 2008, 7, 905–921. [Google Scholar] [CrossRef] [PubMed]
- Korthals-de, B.I.; Hoving, J.L.; van Tulder, M.W.; Rutten-van Mölken, M.P.; Ader, H.J.; de Vet, H.C.W.; Koes, B.W.; Vondeling, H.; Bouter, L.M. Cost effectiveness of physiotherapy, manual therapy, and general practitioner care for neck pain: Economic evaluation alongside a randomised controlled trial. BMJ 2003, 326, 911–916. [Google Scholar] [CrossRef]
- Kjellman, G.V.; Skargren, E.I.; Oberg, B.E. A critical analysis of randomised clinical trials on neck pain and treatment efficacy. A review of the literature. Scand. J. Rehabil. Med. 1999, 31, 139–152. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Carragee, E.J.; van der Velde, G.; Carroll, L.J.; Nordin, M.; Guzman, J.; Peloso, P.M.; Holm, L.W.; Côté, P.; Hogg-Johnson, S.; et al. Treatment of neck pain: Noninvasive interventions: Results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008, 33, S123–S152. [Google Scholar] [CrossRef]
- Valera-Garrido, F.; Martínez-Rodríguez, A.; Medina-i-Mirapeix, F.; Meseguer –Henarejos, A.; Millan-Robles, F.; Campillo-Pomata, E. El modelo biopsicosocial en los síndromes de dolor vertebral: Implicaciones para la protocolización. Rev. Iberoam Fisioter Kinesiol. 2001, 4, 81–87. [Google Scholar]
- Jull, G.; Moore, A.; Falla, D.; Lewis, J.; McCarthy, C.; Sterling, M. Grieve’s Modern Musculoskeletal Physiotherapy, 4th ed.; Elsevier: London, UK, 2015; ISBN 9780702051524. [Google Scholar]
- Jull, G.; Falla, D.; Treleaven, J.; O’Leary, S. Management of Neck Pain Disorders E-Book: A Research Informed Approach, 1st ed.; Elsevier Health Sciences: London, UK, 2018; ISBN 9780702074769. [Google Scholar]
- Escortell-Mayor, E.; Riesgo-Fuertes, R.; Garrido-Elustondo, S.; Asúnsolo-del Barco, A.; Díaz-Pulido, B.; Blanco-Díaz, M.; Bejerano-Álvarez, E.; TEMA-TENS Group. Primary care randomized clinical trial: Manual Therapy effectivenes in comparison with TENS in patiens with neck pain. Man. Ther. 2011, 16, 66–73. [Google Scholar] [CrossRef]
- Spitzer, W.O.; Leblanc, F.E.; Dupuis, M. Scientific approach to the assessment and management of activity related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine 1987, 7, 1–59. [Google Scholar]
- Escortell-Mayor, E.; Lebrijo-Pérez, G.; Pérez-Martín, Y.; Asúnsolo-del-Barco, A.; Riesgo-Fuertes, R.; Saa-Requejo, C. Randomized clinical trial for primary care patients with neck pain: Manual therapy versus electrical stimulation. Atención Primaria. 2008, 40, 337–343. [Google Scholar] [CrossRef]
- Stratford, P.W.; Riddle, D.L.; Binkley, J.M.; Spadoni, G.; Westaway, M.D.; Padfield, B. Using the Neck Disability index to make decisions concerning individual patients. Physiother Can. 1999, 51, 107–112. [Google Scholar]
- Ylinen, J.; Savolainen, S.; Airaksinen, O.; Kautiainen, H.; Salo, P.; Häkkinen, A. Decreased strength and mobility in patients after anterior cervical diskectomy compared with healthy subjects. Arch. Phys. Med. Rehabil. 2003, 84, 1043–1047. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, J.D.; Whitman, J.M. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch. Phys. Med. Rehabil. 2008, 89, 69–74. [Google Scholar] [CrossRef]
- Chaitow, L. Técnica Neuromuscular: Tratamiento de Los Tejidos Blandos: Método Diagnóstico y Terapéutico de La Disfunción Tisular; Bellaterra: Barcelona, Spain, 1999; ISBN 84-7290-027-4. [Google Scholar]
- Travell, J.G.; Simons, G.D. Miofascial Pain and Dysfunction. The Trigger Point Manual [Dolor y Disfunción Miofascial. El Manual de Los Puntos Gatillo], 2nd ed.; Medica Panamericana: Madrid, Spain, 2001; ISBN 0683083635. [Google Scholar]
- Lantz, C.A.; Chen, J.; Buch, D. Clinical validity and stability of active and passive cervical range of motion with regard to total and unilateral uniplanar motion. Spine 1999, 24, 1082–1089. [Google Scholar] [CrossRef] [PubMed]
- Magee, D. Ortopedia, 2nd ed.; Interamericana Mc Graw-Hill: Mexico City, Mexico, 1994; ISBN 968252055X. [Google Scholar]
- Boyles, R.E.; Walker, M.J.; Young, B.A.; Strunce, J.B.; Wainner, R.S. The addition of cervical thrust manipulations to a manual physical therapy approach in patients treated for mechanical neck pain: A secondary analysis. J. Orthop. Sports Phys. Ther. 2010, 40, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Edmondston, S.J.; Wallumrod, M.E.; MacLéid, F.; Kvamme, L.S.; Joebges, S.; Brabham, G.C. Reliability or isometric muscle endurance test in subjects with postural neck pain. J. Manipul. Physiol. Ther. 2008, 31, 348–352. [Google Scholar] [CrossRef]
- Medina, F.; Messeguer, A.B.; Montilla, J. Clinical Practice Guideline for the mechanical neck pain physiotherapy diagnosis [Guía de práctica clínica para el diagnóstico fisioterápico de la cervicalgia mecánica]. Fisioterapia 2000, 22, 13–32. [Google Scholar]
- Resende, L.; Merriwether, E.; Rampazo, É.; Dailey, D.; Embree, J.; Deberg, J.; Liebano, R.E.; Sluka, K.A. Meta-analysis of transcutaneous electrical nerve stimulation for relief of spinal pain. Eur. J. Pain 2018, 22, 663–678. [Google Scholar] [CrossRef]
- Paolucci, T.; Agostini, F.; Paoloni, M.; de Sire, A.; Verna, S.; Pesce, M.; Ribecco, L.; Mangone, M.; Bernetti, A.; Saggini, R. Efficacy of TENS in Cervical Pain Syndromes: An Umbrella Review of Systematic Reviews. Appl. Sci. 2021, 11, 3423. [Google Scholar] [CrossRef]
- Tuttle, N.; Barrett, R.; Laakso, L. Relation between changes in posteroanterior stiffness and active range of movement of the cervical spine following manual therapy treatment. Spine 2008, 33, E673–E679. [Google Scholar] [CrossRef]
- Heikki, M.; Hemmilä, M.D. Bone setting for prolongad neck pain: A randomized clinical trial. J. Manip. Physiol. Ther. 2005, 28, 507–515. [Google Scholar] [CrossRef]
- Nordemar, R.; Thörner, C. Treatment of acute cervical pain-a comparative group study. Pain 1981, 10, 93–101. [Google Scholar] [CrossRef]
- Dusunceli, Y.; Ozturk, C.; Atamaz, F.; Hepguler, S.; Durmaz, B. Efficacy of neck stabilization exercises for neck pain: A randomized controlled study. J. Rehabil. Med. 2009, 41, 626–631. [Google Scholar] [CrossRef]
- Chiu, T.T.; Hui-Chan, C.W.; Cheing, G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clin. Rehabil. 2005, 19, 850–860. [Google Scholar] [CrossRef]
- Jordan, A.; Bendix, T.; Nielsen, H.; Hansen, F.R.; Host, D.; Winkel, A. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain. A prospective, single-blinded, randomized clinical trial. Spine 1998, 23, 311–318. [Google Scholar] [CrossRef]
- Levoska, S.; Keinanen-Kiukaannieni, S. Active or passive physiotherapy for occupational cervicobrachial disorders? A comparison of two treatment methods with a 1-year follow- up. Arch. Phys. Med. Rehabil. 1993, 74, 425–430. [Google Scholar] [PubMed]
- Cheville, A.L.; Smith, S.R.; Basford, J.R. Rehabilitation Medicine Approaches to Pain Management. Hematol/Oncol Clin. N. Am. 2018, 32, 469–482. [Google Scholar] [CrossRef]
- Hodges, P.W.; Moseley, G.L. Pain and motor control of the lumbopelvic region: Effect and possible mechanisms. J. Electromyogr. Kinesiol. 2003, 13, 361–370. [Google Scholar] [CrossRef]
- Falla, D.; Bilenkij, G.; Jull, G. Patients with chronic neck pain demonstrate altered patterns of muscle activation during performance of a functional upper limb task. Spine 2004, 29, 1436–1440. [Google Scholar] [CrossRef]
- Al-Obaidi, S.M.; Nelson, R.M.; Al-Awadhi, S.; Al-Shuwaie, N. The role of anticipation and fear of pain in the persistence of avoidance behaviour in patients with chronic low back pain. Spine 2000, 25, 1126–1131. [Google Scholar] [CrossRef] [PubMed]
- Häkkinen, A.; Kautiainen, H.; Hannonen, P.; Ylinen, J. Strentght training and stretching versus stretching only in the treatment of patients with chronic neck pain: A randomized one-year follow-up study. Clin. Rehabil. 2008, 22, 592–600. [Google Scholar] [CrossRef]
- Schabrun, S.M.; Cannan, A.; Mullens, R.; Dunphy, M.; Pearson, T.; Lau, C.; Chipchase, L.S. The effect of interactive neurostimulation therapy on myofascial trigger point associated with mechanical neck pain: A preliminary randomized, sham-controlled trial. J. Altern. Complement. Med. 2012, 18, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Kay, T.M.; Gross, A.; Goldsmith, C.H.; Santaguida, P.L.; Hoving, J.; Bronfort, G.; Santaguida, P.L. Exercise for Mechanical Neck Disorders (Cochrane Review). Cochrane Database Syst. Rev. 2012, 15, CD004250. [Google Scholar] [CrossRef]
- Loudon, K.; Treweek, S.; Sullivan, F.; Donnan, P.; Thorpe, K.E.; Zwarenstein, M. The PRECIS-2 tool: Designing trials that are fit for purpose. BMJ 2015, 8, 350. [Google Scholar] [CrossRef] [PubMed]
- Ylinen, J.; Häkkinen, A.; NyKänen, M.; Kautiainen, H.; Takala, E.P. Neck muscle training in the treatment of chronic neck pain: A three-year follow-up study. Eur. Med. 2007, 43, 161. [Google Scholar]
- Kelly, M.; Cardy, N.; Melvin, E.; Reddin, C.; Ward, C.; Wilson, F. The craniocervical flexion test: An investigation or performance in young asymptomatic subjects. Man. Ther. 2013, 18, 83–86. [Google Scholar] [CrossRef] [PubMed]
- Coulter, I.D.; Crawford, C.; Vernon, H.; Hurwitz, E.L.; Khorsan, R.; Booth, M.S.; Herman, P.M. Manipulation and Mobilization for Treating Chronic Nonspecific Neck Pain: A Systematic Review and Meta-Analysis for an Appropriateness Panel. Pain Phy-Sician 2019, 22, E55–E70. [Google Scholar] [CrossRef]
- Rondon-Ramos, A.; Martinez-Calderon, J.; Diaz-Cerrillo, J.; Rivas-Ruiz, F.; Ariza-Hurtado, G.; Clavero-Cano, S.; Luque-Suarez, A. Pain Neuroscience Education Plus Usual Care Is More Effective than Usual Care Alone to Improve Self-Efficacy Beliefs in People with Chronic Musculoskeletal Pain: A Non-Randomized Controlled Trial. J. Clin. Med. 2020, 9, 2195. [Google Scholar] [CrossRef]
- Pérez-Martín, Y.; Díaz-Pulido, B.; Lebrijo-Pérez, G. Efectividad del tratamiento fisioterápico en pacientes con cervicalgia mecánica. Fisioterapia 2002, 24, 165–174. [Google Scholar] [CrossRef]
- Garrido- Elustondo, S.; Riesgo-Fuertes, R.; Escortell-Mayor, E.; Asúnsolo-del-Barco, A.; Pérez-Martín, Y.; Martín-Castro, B. Satisfaction of patients with mechanical neck disorders attended by Primary Care Physical Therapists. J. Eval. Clin. Pract. 2010, 16, 445–450. [Google Scholar] [CrossRef]

| MT Technic | Description |
|---|---|
| Neuromuscular technique | Longitudinal strokes were performed along the fibers of each muscle to stretch locally the areas of most tension that were previously located. The technique was applied with the physical therapist’s first finger, and using the last four fingers as support. |
| Post-isometric stretching | The patient was placed in a stretching position that was comfortable for the affected muscles, and he/she was asked to do an isometric contraction for 5 to 7 s. After that, a new barrier was searched for, and the sequence was repeated up to three times. |
| Spray and stretching technique | From a comfortable position for the patient, the first cold spray was applied to the target muscle’s MTrPs, in order to start immediately afterward with muscle stretching up to the position the patient allowed. After this, the area was sprayed again, but this time the whole area with pain was covered, in order to perform another stretch. On each area the spray could only be applied three times. |
| Jones technique | Pressure was applied to the painful points and/or the MtrPs, which had previously been located, until pain was generated. Then a position where pain disappeared was searched (maximum comfort position), and it was maintained for 90 s before passively returning to the original position. |
| Manual Therapy (n = 47) | TENS (n = 43) | |
|---|---|---|
| Gender: women (n (%)) | 42 (89.4) | 38 (88.4) |
| Age (decimal ages) (X (SD)) | 40.8 (11.6) | 39.3 (9.7) |
| Previous neck pain episodes (n (%)) | 38 (84.4) | 37 (86.0) |
| History of accident with cervical impaired (n (%)) | 12 (26.1) | 6 (14.3) |
| Disability: NDI (X (SD)) | 31.6 (11.3) | 34.4 (13.9) |
| Pain: VAS (X (SD)) | 54.9 (18.8) | 56.4 (20.2) |
| Cervical current episode duration (days) (X (SD)) | 141 (280.8) | 154.3 (216.2) |
| Baseline | Basal and Post-Intervention | Basal and 6-Months Follow-Up | ||||||
|---|---|---|---|---|---|---|---|---|
| MT Group (CI 95%) (n = 47) | TENS Group x (CI 95%) (n = 43) | MT Group Difference (CI 95%) (n = 45) | TENS Group Difference (CI 95%) (n = 42) | Between Groups p-Value | MT Group Difference (CI 95%) (n = 36) | TENS Group Difference (CI 95%) (n = 35) | Between Groups p-Value | |
| MOBILITY (planes) | ||||||||
| SAGITAL | 111.62 (105.9–117.3) | 112.86 (106.6–119.2) | 8.93 (4.37–13.50) | 3.44 (−1.54–8.42) | 0.372 (*) | 5.68 (0.37–11.0) | −2.38 (−11.37–6.60) | 0.114 (*) |
| FRONTAL | 83.34 (77.5–89.2) | 82.95 (76.8–89.1) | 4.98 (1.28–8.67) | 1.62 (−3.70– 6.93) | 0.583 (*) | −0.46 (−6.66–5.73) | 3.09 (−4.45–10.62) | 0.459 (*) |
| TRANSVERSAL | 122.85 (115.2–130.5) | 124.72 (116.2–133.3) | 7.64 (1.24–14.05) | 4.05 (-2.57– 10.67) | 0.902 (*) | 4.89 (−2.23–12.02) | 8.79 (−0.39–17.97) | 0.494 (*) |
| ENDURANCE (planes) | ||||||||
| SAGITAL | 3.44 (3.2–3.6) | 3.67 (3.5–3.8) | 0.33 (0.15–0.49) | 0.12 (−0.01–0.25) | 0.140 (†) | 0.3 (0.11–0.49) | 0.11 (−0.04–0.28) | 0.505 (†) |
| FRONTAL | 3.11 (2.9–3.3) | 3.42 (3.2–3.6) | 0.43 (0.24–0.62) | 0.08 (−0.13– 0.29) | 0.114 (†) | 0.3 (0.10–0.50) | 0.07 (−0.19–0.34) | 0.234 (†) |
| TRANSVERSAL | 2.57 (2.3–2.7) | 2.59 (2.3–2.7) | 0.33 (0.12–0.55) | 0.11 (−0.13–0.35) | 0.117 (†) | 0.32 (0.07–0.57) | 0.04 (−0.24–0.33) | 0.114 (†) |
| Models | Intervention | Disability (NDI) | Episode Duration | Postural Compliance | Previous Episode | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rc | p | β | p | β | p | β | p | β | p | β | p | ||
| Post-intervention | |||||||||||||
| MOBILITY (planes) | SAGITAL | 0.16 | 0.00 | −6.58 | 0.03 | −0.02 | 0.02 | 6.75 | 0.03 | −9.63 | 0.04 | ||
| FRONTAL | 0.04 | 0.07 | −3.18 | 0.32 | 6.54 | 0.04 | |||||||
| TRANSVERSAL | 0.06 | 0.03 | −5.26 | 0.24 | 0.46 | 0.01 | |||||||
| ENDURANCE (planes) | SAGITAL | 0.09 | 0.02 | 0.84 | 0.01 | −0.03 | 0.04 | ||||||
| FRONTAL | 0.15 | 0.00 | 0.29 | 0.07 | |||||||||
| TRANSVERSAL | 0.06 | 0.02 | 0.25 | 0.11 | |||||||||
| Six months after intervention | |||||||||||||
| MOBILITY (planes) | SAGITAL | 0.10 | 0.01 | −10.08 | 0.04 | 0.56 | 0.01 | ||||||
| FRONTAL | 0.08 | 0.04 | 3.58 | 0.44 | 0.42 | 0.04 | −0.02 | 0.07 | |||||
| TRANSVERSAL | 0.17 | 0.00 | 0.73 | 0.89 | 0.88 | 0.00 | |||||||
| ENDURANCE (planes) | SAGITAL | 0.17 | 0.01 | 0.56 | 0.00 | −0.81 | 0.04 | 0.31 | 0.10 | ||||
| FRONTAL | 0.26 | 0.00 | 0.06 | 0.73 | 0.02 | 0.00 | |||||||
| TRANSVERSAL | 0.16 | 0.00 | 0.20 | 0.26 | 0.00 | 0.00 | |||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Díaz-Pulido, B.; Pérez-Martín, Y.; Pecos-Martín, D.; Rodríguez-Costa, I.; Pérez-Muñoz, M.; Calvo-Fuente, V.; Ortiz-Jiménez, M.F.; Asúnsolo-del Barco, Á. Efficacy of Manual Therapy and Transcutaneous Electrical Nerve Stimulation in Cervical Mobility and Endurance in Subacute and Chronic Neck Pain: A Randomized Clinical Trial. J. Clin. Med. 2021, 10, 3245. https://doi.org/10.3390/jcm10153245
Díaz-Pulido B, Pérez-Martín Y, Pecos-Martín D, Rodríguez-Costa I, Pérez-Muñoz M, Calvo-Fuente V, Ortiz-Jiménez MF, Asúnsolo-del Barco Á. Efficacy of Manual Therapy and Transcutaneous Electrical Nerve Stimulation in Cervical Mobility and Endurance in Subacute and Chronic Neck Pain: A Randomized Clinical Trial. Journal of Clinical Medicine. 2021; 10(15):3245. https://doi.org/10.3390/jcm10153245
Chicago/Turabian StyleDíaz-Pulido, Belén, Yolanda Pérez-Martín, Daniel Pecos-Martín, Isabel Rodríguez-Costa, Milagros Pérez-Muñoz, Victoria Calvo-Fuente, María Félix Ortiz-Jiménez, and Ángel Asúnsolo-del Barco. 2021. "Efficacy of Manual Therapy and Transcutaneous Electrical Nerve Stimulation in Cervical Mobility and Endurance in Subacute and Chronic Neck Pain: A Randomized Clinical Trial" Journal of Clinical Medicine 10, no. 15: 3245. https://doi.org/10.3390/jcm10153245
APA StyleDíaz-Pulido, B., Pérez-Martín, Y., Pecos-Martín, D., Rodríguez-Costa, I., Pérez-Muñoz, M., Calvo-Fuente, V., Ortiz-Jiménez, M. F., & Asúnsolo-del Barco, Á. (2021). Efficacy of Manual Therapy and Transcutaneous Electrical Nerve Stimulation in Cervical Mobility and Endurance in Subacute and Chronic Neck Pain: A Randomized Clinical Trial. Journal of Clinical Medicine, 10(15), 3245. https://doi.org/10.3390/jcm10153245








