Ulnar Nerve Dislocation and Subluxation from the Cubital Tunnel Are Common in College Athletes
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
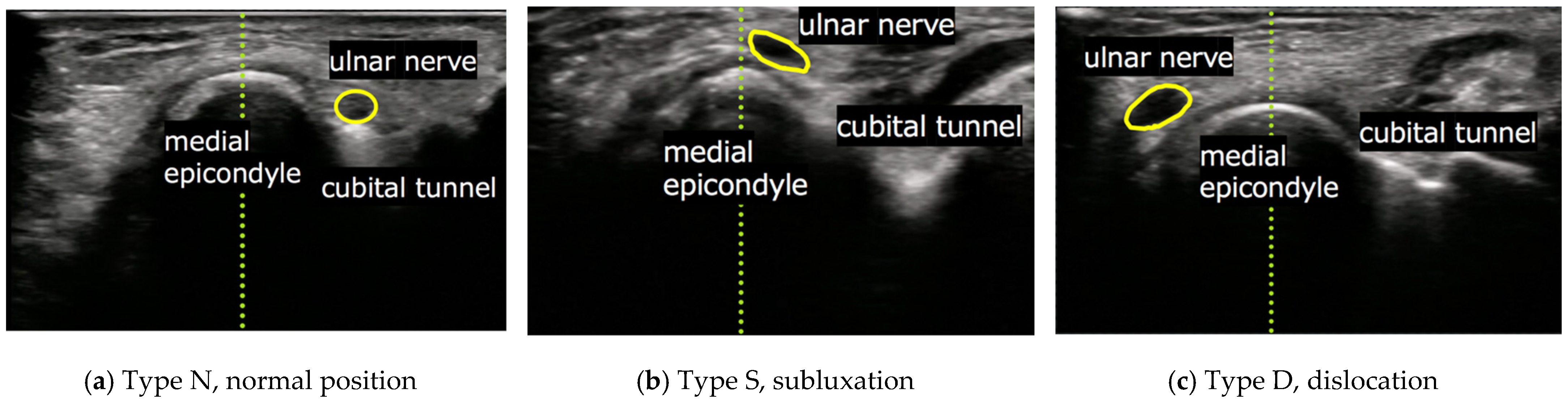
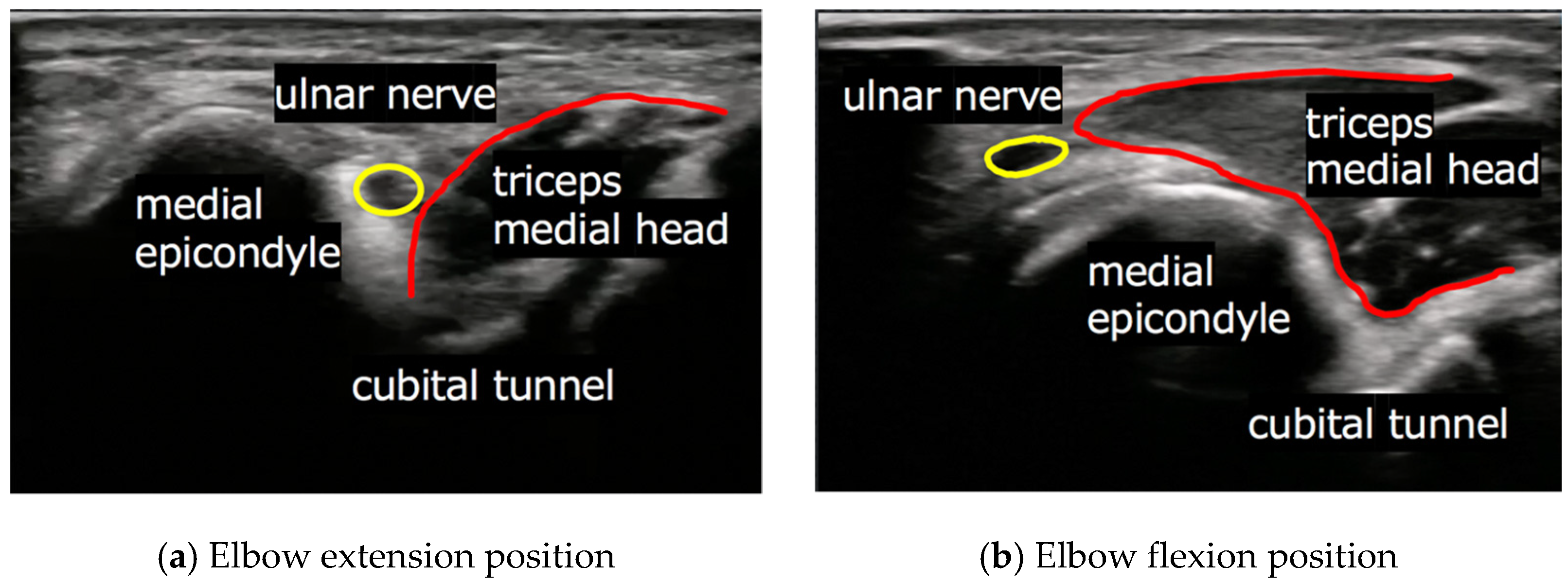
2.2. Evaluation of Ulnar Nerve and Subjective Findings
2.3. Evaluation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Okamoto, M.; Abe, M.; Shirai, H.; Ueda, N. Morphology and dynamics of the ulnar nerve in the cubital tunnel. Observation by ultrasonography. J. Hand Surg. Br. Eur. Vol. 2000, 25, 85–89. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.J.; Date, E.S.; Lee, S.H.; Yoon, J.S.; Hur, S.Y.; Kim, S.J. Distance measure error induced by displacement of the ulnar nerve when the elbow is flexed. Arch. Phys. Med. Rehabil. 2005, 86, 809–812. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, E.; Sonmez, G.; Colak, A.; Sildiroglu, H.O.; Mutlu, H.; Senol, M.G.; Basekim, C.C.; Kizilkaya, E. Sonographic appearances of the normal ulnar nerve in the cubital tunnel. J. Clin. Ultrasound. 2008, 36, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.H.; Joo, B.E.; Kim, K.H.; Park, B.K.; Cha, J.; Kim, D.H. Ultrasonographic and electrophysiological evaluation of ulnar nerve instability and snapping of the triceps medial head in healthy subjects. Am. J. Phys. Med. Rehabil. 2017, 96, e141–e146. [Google Scholar] [CrossRef] [PubMed]
- Cornelson, S.M.; Sclocco, R.; Kettner, N.W. Ulnar nerve instability in the cubital tunnel of asymptomatic volunteers. J. Ultrasound. 2019, 22, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.N.; Yoon, J.S.; Kim, S.J.; Kang, H.J.; Kim, S.H. Movement of the ulnar nerve at the elbow: A sonographic study. J. Ultrasound. Med. 2013, 32, 1747–1752. [Google Scholar] [CrossRef] [PubMed]
- Kleinrensink, G.J.; Stoeckart, R.; Mulder, P.G.; Hoek, G.; Broek, T.; Vleeming, A.; Snijders, C.J. Upper limb tension tests as tools in the diagnosis of nerve and plexus lesions. Anatomical and biomechanical aspects. Clin. Biomech. (Bristol. Avon) 2000, 15, 9–14. [Google Scholar] [CrossRef]
- Husarik, D.B.; Saupe, N.; Pfirrmann, C.W.; Jost, B.; Hodler, J.; Zanetti, M. Elbow nerves: MR findings in 60 asymptomatic subjects—Normal anatomy, variants, and pitfalls. Radiology 2009, 252, 148–156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kawahara, Y.; Yamaguchi, T.; Honda, Y.; Tomita, Y.; Uetani, M. The ulnar nerve at elbow extension and flexion: Assessment of position and signal intensity on MR images. Radiology 2016, 280, 483–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Van Den Berg, P.J.; Pompe, S.M.; Beekman, R.; Visser, L.H. Sonographic incidence of ulnar nerve (sub)luxation and its associated clinical and electrodiagnostic characteristics. Muscle Nerve 2013, 47, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Rolfsen, L. Snapping triceps tendon with ulnar neuritis. Report on a case. Acta Orthop. Scand. 1970, 41, 74–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spinner, R.J.; Goldner, R.D. Snapping of the medial head of the triceps and recurrent dislocation of the ulnar nerve. Anatomical and dynamic factors. J. Bone Jt. Surg. Am. 1998, 80, 239–247. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, J.A.; Jebson, P.J.; Jeffers, A.W.; Fessell, D.P.; Hayes, C.W. Ulnar nerve dislocation and snapping triceps syndrome: Diagnosis with dynamic sonography—Report of three cases. Radiology 2001, 220, 601–605. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yoo, M.J.; Kim, D.D.J.; Oh-Park, M. Exacerbation of habitual dislocation of ulnar nerve by concurrent dislocation of triceps muscle: Complementary role of dynamic ultrasonography to electrodiagnosis. Am. J. Phys. Med. Rehabil. 2007, 86, 1030. [Google Scholar] [CrossRef] [PubMed]
- Mondelli, M.; Filippou, G.; Frediani, B.; Aretini, A. Ultrasonography in ulnar neuropathy at the elbow: Relationships to clinical and electrophysiological findings. Neurophysiol. Clin. 2008, 38, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Beekman, R.; Visser, L.H.; Verhagen, W.I. Ultrasonography in ulnar neuropathy at the elbow: A critical review. Muscle Nerve 2011, 43, 627–635. [Google Scholar] [CrossRef] [PubMed]
- Molnar, S.L.; Lang, P.; Skapinyecz, J.; Shadgan, B. Dislocation of the ulnar nerve at the elbow in an elite wrestler. BMJ Case. Rep. 2011, 7, bcr0220113806. [Google Scholar] [CrossRef] [PubMed]
- Michael, A.E.; Young, P. Is triceps hypertrophy associated with ulnar nerve luxation? Muscle Nerve 2018, 58, 523–527. [Google Scholar] [CrossRef] [PubMed]
| Baseball | Rugby | Soccer | Long-Distance Running | Total | |
|---|---|---|---|---|---|
| n | 60 | 63 | 62 | 61 | 246 |
| Age, mean ± SD | 19.6 ± 1.1 | 19.8 ± 1.2 | 19.7 ± 1.0 | 19.5 ± 1.2 | 19.7 ± 1.1 |
| Male (n) | 60 | 63 | 62 | 61 | 246 |
| Elbows (n) | 120 | 126 | 124 | 122 | 492 |
| Right (n)/Left (n) | 60/60 | 63/63 | 62/62 | 61/61 | 246/246 |
| Type D (n, %) | 29 (48)/33 (55) | 35 (56)/42 (67) | 26 (42)/24 (39) | 17 (28)/20 (33) | 107 (44)/119 (49) |
| Type S (n, %) | 22 (37)/16 (27) | 22 (35)/16 (25) | 19 (31)/15 (24) | 17 (28)/20 (33) | 80 (33)/67 (27) |
| Type N (n, %) | 9 (15)/11 (18) | 6 (9)/5 (8) | 17 (27)/23 (37) | 27 (44)/21 (34) | 59 (23)/60 (24) |
| Types D and S | Type N | p-Value | ||
|---|---|---|---|---|
| Right | Group | <0.001 † | ||
| Group H (n, %) | 108 (88) | 15 (12) | ||
| Baseball (n, %) | 51 (85) | 9 (15) | 0.15 ‡ | |
| Rugby (n, %) | 57 (91) | 6 (9) | ||
| Group L (n, %) | 79 (64) | 44 (36) | ||
| Soccer (n, %) | 45 (73) | 17 (27) | 0.05 ‡ | |
| Long-distance running (n, %) | 34 (56) | 27 (44) | ||
| Left | Group | <0.001 † | ||
| Group H (n, %) | 107 (87) | 16 (13) | ||
| Baseball (n, %) | 49 (82) | 11 (16) | 0.03 ‡ | |
| Rugby (n, %) | 58 (92) | 5 (9) | ||
| Group L (n, %) | 79 (64) | 44 (36) | ||
| Soccer (n, %) | 39 (63) | 23 (37) | 0.75 ‡ | |
| Long-distance running (n, %) | 40 (66) | 21 (34) |
| Baseball | Rugby | Soccer | Long-Distance Running | |
|---|---|---|---|---|
| Types D and S (n) | 53 | 58 | 46 | 41 |
| Bilateral (n, %) | 47 (88) | 57 (98) | 38 (83) | 33 (80) |
| Only dominant (n, %) | 4 (8) | 0 (0) | 7 (15) | 3 (8) |
| Only non-dominant (n, %) | 2 (4) | 1 (2) | 1 (2) | 5 (12) |
| Baseball | Rugby | Soccer | Long-Distance Running | Total | |
|---|---|---|---|---|---|
| Types D and S (n) | 100 | 115 | 84 | 74 | 373 |
| Right/Left (n) | 51/49 | 57/58 | 45/39 | 34/40 | 187/186 |
| Pain (n, %) | 15 (29)/5 (10) | 6 (11)/3 (5) | 3 (7)/2 (5) | 0 (0)/0 (0) | 24 (13)/10 (5) |
| Dysesthesia (n, %) | 4 (8)/1 (2) | 5 (9)/3 (5) | 2 (4)/2 (5) | 0 (0)/0 (0) | 11 (6)/6 (3) |
| Baseball | Rugby | Soccer | Long-Distance Running | Total | |
|---|---|---|---|---|---|
| Types D and S (n) | 100 | 115 | 84 | 74 | 373 |
| Right/Left (n) | 51/49 | 57/58 | 45/39 | 34/40 | 187/186 |
| Tinel sign (n, %) | 3 (6)/1 (2) | 6 (10)/4 (6) | 2 (4)/2 (5) | 2 (6)/2 (6) | 13 (7)/9 (5) |
| NTT (n, %) | 1 (2)/0 (0) | 1 (2)/2 (3) | 1 (2)/0 (2) | 0 (0)/0 (0) | 3 (2)/2 (1) |
| Froment’s sign (n, %) | 0 (0)/0 (0) | 0 (0)/2 (3) | 0 (0)/0 (0) | 0 (0)/0 (0) | 0 (0)/2 (1) |
| Weakness of opponens digiti minimi muscle (n, %) | 2 (4)/3 (6) | 8 (14)/11 (19) | 3 (6)/2 (5) | 0 (0)/0 (0) | 13 (7)/16 (9) |
| Push-Out of the Ulnar Nerve by the Triceps | Others | p-Value | ||
|---|---|---|---|---|
| Right | Group | <0.001 † | ||
| Group H (n, %) | 83 (79) | 25 (21) | ||
| Baseball (n, %) | 38 (75) | 13 (25) | 0.58 ‡ | |
| Rugby (n, %) | 45 (79) | 12 (21) | ||
| Group L (n, %) | 36 (45) | 43 (55) | ||
| Soccer (n, %) | 26 (58) | 19 (43) | 0.01 ‡ | |
| Long-distance running (n, %) | 10 (29) | 24 (71) | ||
| Left | Group | <0.001 † | ||
| Group H (n, %) | 82 (77) | 25 (23) | ||
| Baseball (n, %) | 34 (69) | 15 (31) | 0.10 ‡ | |
| Rugby (n, %) | 48 (82) | 10 (18) | ||
| Group L (n, %) | 34 (41) | 49 (59) | ||
| Soccer (n, %) | 20 (47) | 23 (53) | 0.28 ‡ | |
| Long-distance running (n, %) | 14 (35) | 26 (65) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsukada, K.; Yasui, Y.; Sasahara, J.; Okawa, Y.; Nakagawa, T.; Kawano, H.; Miyamoto, W. Ulnar Nerve Dislocation and Subluxation from the Cubital Tunnel Are Common in College Athletes. J. Clin. Med. 2021, 10, 3131. https://doi.org/10.3390/jcm10143131
Tsukada K, Yasui Y, Sasahara J, Okawa Y, Nakagawa T, Kawano H, Miyamoto W. Ulnar Nerve Dislocation and Subluxation from the Cubital Tunnel Are Common in College Athletes. Journal of Clinical Medicine. 2021; 10(14):3131. https://doi.org/10.3390/jcm10143131
Chicago/Turabian StyleTsukada, Keisuke, Youichi Yasui, Jun Sasahara, Yasuaki Okawa, Takumi Nakagawa, Hirotaka Kawano, and Wataru Miyamoto. 2021. "Ulnar Nerve Dislocation and Subluxation from the Cubital Tunnel Are Common in College Athletes" Journal of Clinical Medicine 10, no. 14: 3131. https://doi.org/10.3390/jcm10143131
APA StyleTsukada, K., Yasui, Y., Sasahara, J., Okawa, Y., Nakagawa, T., Kawano, H., & Miyamoto, W. (2021). Ulnar Nerve Dislocation and Subluxation from the Cubital Tunnel Are Common in College Athletes. Journal of Clinical Medicine, 10(14), 3131. https://doi.org/10.3390/jcm10143131






