Clinical Outcomes and Joint Stability after Lateralized Reverse Total Shoulder Arthroplasty with and without Subscapularis Repair: A Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
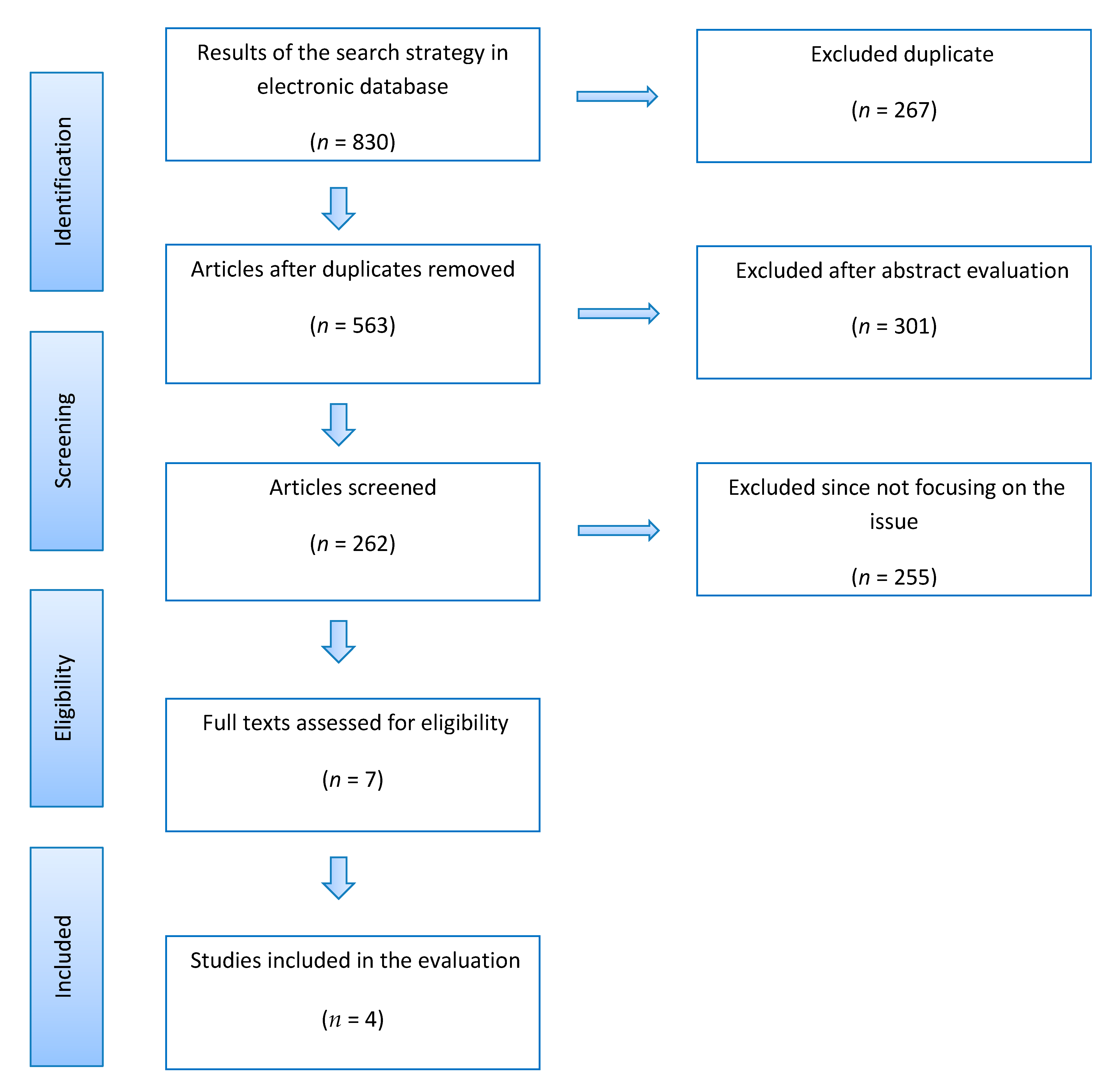
2.1. Search Strategy and Study Selection Process
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Evaluation of the Quality of Studies
3. Statistical Analysis
4. Results
4.1. Search Results
4.2. Patient and Study Characteristics
4.3. Indication for Surgery
4.4. Range of Motion (ROM) Outcomes
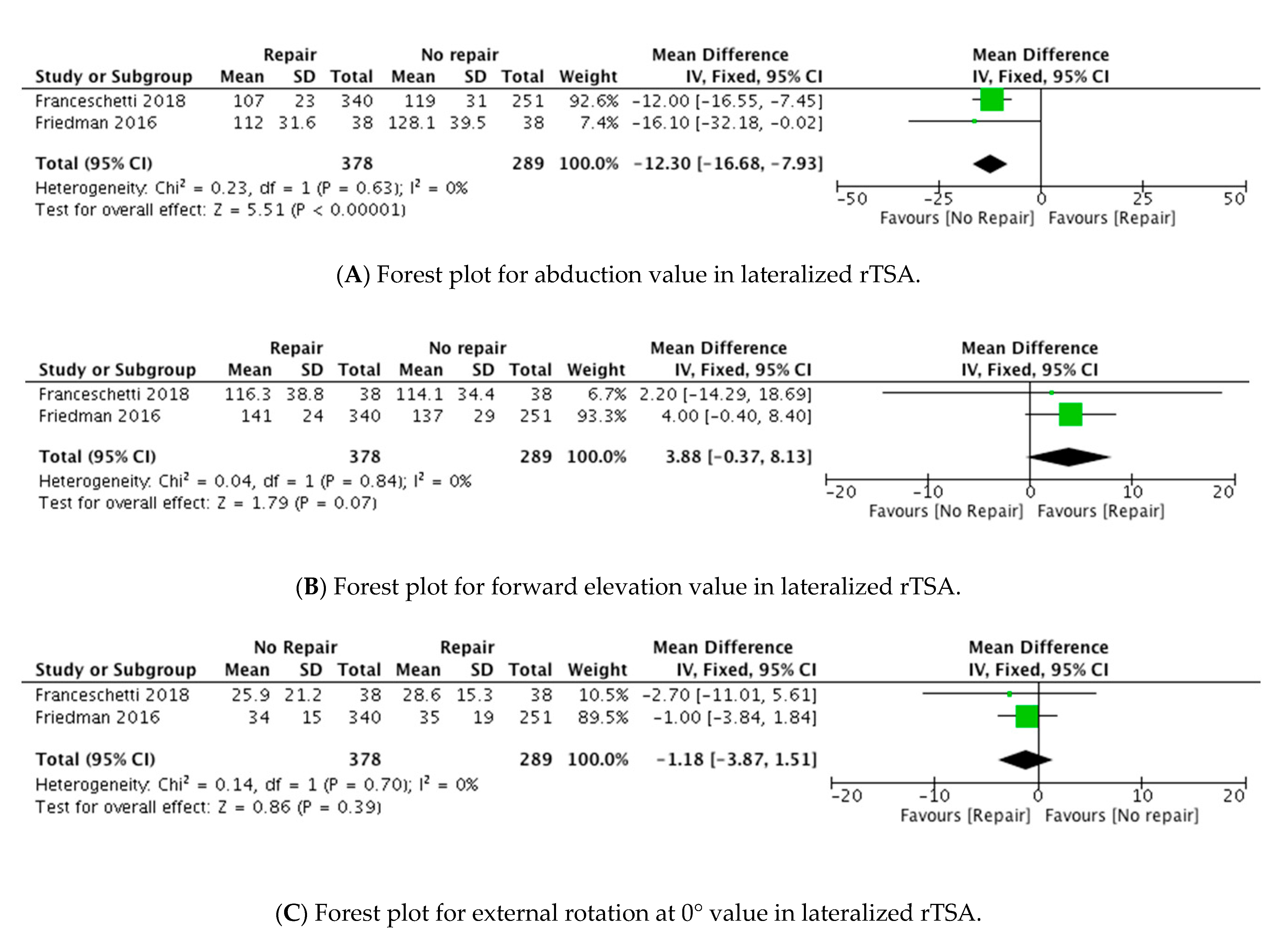
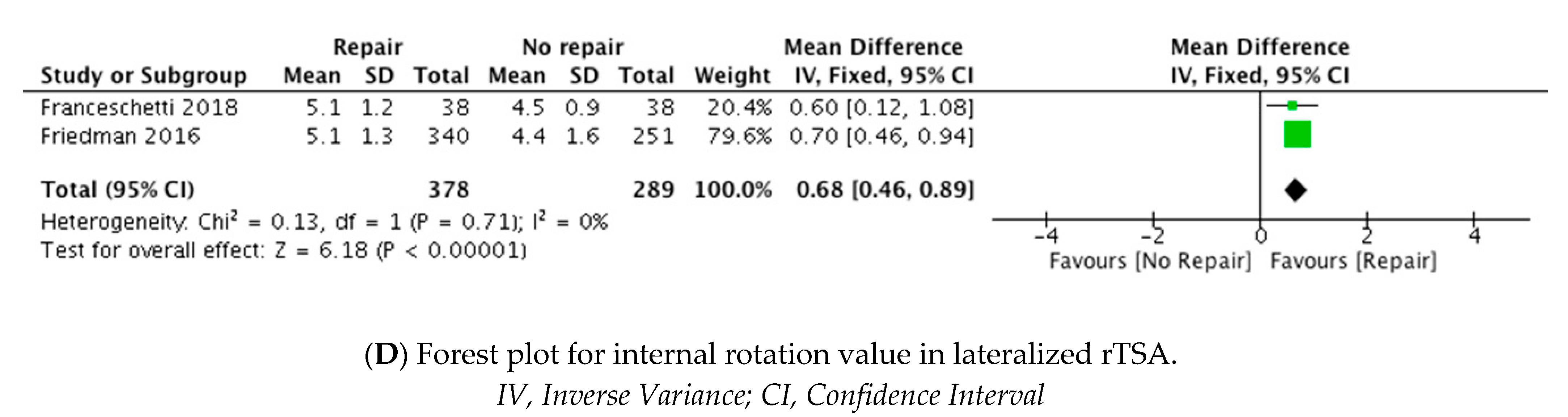
4.5. Clinical Outcomes
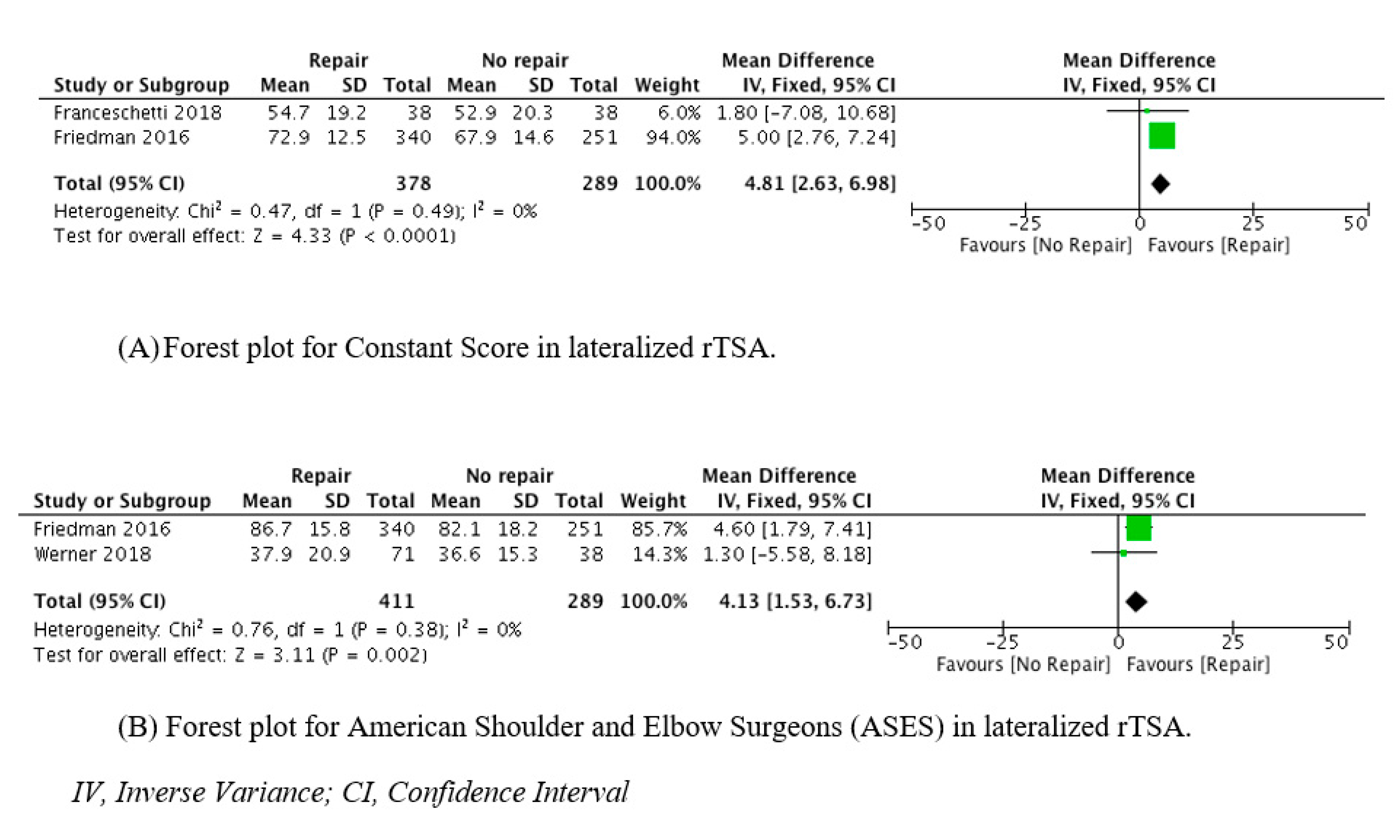
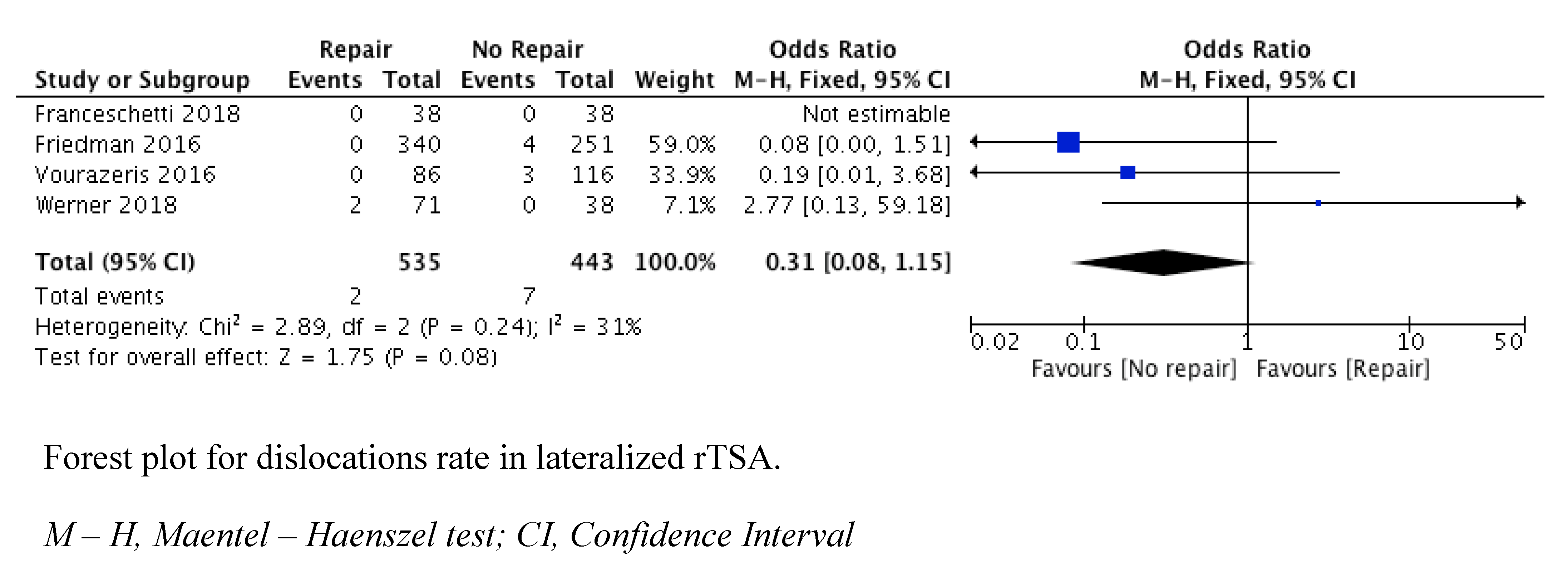
4.6. Dislocation and Complication Rates
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chan, K.; Langohr, G.D.G.; Mahaffy, M.; Johnson, J.A.; Athwal, G.S. Does humeral component lateralization in reverse shoulder arthroplasty affect rotator cuff torque? Evaluation in a cadaver model. Clin. Orthop. Relat. Res. 2017, 475, 2564–2571. [Google Scholar] [CrossRef]
- Costantini, O.; Choi, D.S.; Kontaxis, A.; Gulotta, L.V. The effects of progressive lateralization of the joint center of rotation of reverse total shoulder implants. J. Shoulder Elb. Surg. 2015, 24, 1120–1128. [Google Scholar] [CrossRef]
- Giles, J.W.; Langohr, G.D.; Johnson, J.A.; Athwal, G.S. The rotator cuff muscles are antagonists after reverse total shoulder arthroplasty. J. Shoulder Elb. Surg. 2016, 25, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Henninger, H.B.; Barg, A.; Anderson, A.E.; Bachus, K.N.; Burks, R.T.; Tashjian, R.Z. Effect of lateral offset center of rotation in reverse total shoulder arthroplasty: A biomechanical study. J. Shoulder Elb. Surg. 2012, 21, 1128–1135. [Google Scholar] [CrossRef] [PubMed]
- Langohr, G.D.; Giles, J.W.; Athwal, G.S.; Johnson, J.A. The effects of glenosphere diameter in reverse shoulder arthroplasty on muscle force, joint load, and range of motion. J. Shoulder Elb. Surg. 2015, 24, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Bae, J.H.; Kwon, Y.S.; Kang, H. Clinical outcomes and complications of cementless reverse total shoulder arthroplasty during the early learning curve period. J. Orthop. Surg. 2019, 14, 53. [Google Scholar] [CrossRef]
- Franceschetti, E.; De Sanctis, E.G.; Ranieri, R.; Palumbo, A.; Paciotti, M.; Franceschi, F. The role of the sunscapularis tendon in a lateralized reverse total shoulder arthroplasty: Repair versus nonrepair. Int. Orthop. 2019, 43, 2579–2586. [Google Scholar] [CrossRef]
- Friedman, R.J.; Flurin, P.H.; Wright, T.W.; Zuckerman, J.D.; Roche, C.P. Comparison of reverse total shoulder arthroplasty outcomes with and without subscapularis repair. J. Shoulder Elb. Surg. 2017, 26, 662–668. [Google Scholar] [CrossRef]
- Vourazeris, J.D.; Wright, T.W.; Struk, A.M.; King, J.J.; Farmer, K.W. Primary reverse total shoulder arthroplasty outcomes in patients with subscapularis repair versus tenotomy. J. Shoulder Elb. Surg. 2017, 26, 450–457. [Google Scholar] [CrossRef]
- Wernel, B.C.; Wong, A.C.; Mahony, G.T.; Craig, E.V.; Dines, D.M.; Warren, R.F.; Gulotta, L.V. Clinical outcomes after reverse shoulder arthroplasty with and without subscapularis repair: The importance of considering glenosphere lateralization. J. Am. Acad. Orthop. Surg. 2018, 26, e114–e119. [Google Scholar] [CrossRef]
- Wright, T.; Samitier, G.; Alentorn-Geli, E.; Torrens, C. Reverse shoulder arthroplasty. Part 1: Systematic review of clinical and functional outcomes. Int. J. Shoulder Surg. 2015, 9, 24. [Google Scholar] [CrossRef] [Green Version]
- Werthel, J.D.; Walch, G.; Vegehan, E.; Deransart, P.; Sanchez-Sotelo, J.; Valenti, P. Lateralization in reverse shoulder arthroplasty: A descriptive analysis of different implants in current practice. Int. Orthop. 2019, 43, 2349–2360. [Google Scholar] [CrossRef]
- Giles, J.W.; Langohr, G.D.G.; Johnson, J.A.; Athwal, G.S. Implant design variations in reverse total shoulder arthroplasty influence the required deltoid force and resultant joint load. Clin. Orthop. Relat. Res. 2015, 473, 3615–3626. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greiner, S.; Schmidt, C.; König, C.; Perka, C.; Herrmann, S. Lateralized reverse shoulder arthroplasty maintains rotational function of the remaining rotator cuff. Clin. Orthop. Relat. Res. 2013, 471, 940–946. [Google Scholar] [CrossRef] [Green Version]
- Routman, H.D. The role of subscapularis repair in reverse total shoulder arthroplasty. Bull. Hosp. Jt. Dis. 2013, 71 (Suppl. S2), 108–112. [Google Scholar]
- Greiner, S.; Schmidt, C.; Herrmann, S.; Pauly, S.; Perka, C. Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: A prospective randomized study. J. Shoulder Elb. Surg. 2015, 24, 1397–1404. [Google Scholar] [CrossRef]
- Rotman, H.D.; Flurin, P.H.; Wright, T.W.; Zuckerman, J.D.; Hamilton, M.A.; Roche, C.P. Reverse shoulder arthroplasty prosthesis design classification system. Bull. Hosp. Jt. Dis. 2013, 73 (Suppl. 1), S5. [Google Scholar]
- Matthewson, G.; Kooner, S.; Kwapisz, A.; Leiter, J.; Old, J.; MacDonald, P. The effect of subscapularis repair on dislocation rates in reverse shoulder arthroplasty: A meta-analysis and systematic review. J. Shoulder Elb. Surg. 2019, 28, 989–997. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- OCEBM Levels of Evidence Working Group. The Oxford Levels of Evidence 2. Oxford Centre for Evidence-Based Medicine. Available online: http://www.cebm.net/ocebm-level-of-evidence/ (accessed on 12 December 2020).
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Edwards, T.B.; Williams, M.D.; Labriola, J.E.; Elkousy, H.A.; Gartsman, G.M.; O’Connor, D.P. Subscapularis insufficiency and the risk of shoulder dislocation after reverse shoulder arthroplasty. J. Shoulder Elb. Surg. 2009, 18, 892–896. [Google Scholar] [CrossRef] [PubMed]
- Romano, A.M.; Oliva, F.; Nastrucci, G.; Casillo, P.; Di Giunta, A.; Susanna, M.; Ascione, F. Reverse shoulder arthroplasty patients personalized rehabilitation protocol. Preliminary results according to prognostic groups. Muscles Ligaments Tendons J. 2017, 7, 263–270. [Google Scholar] [CrossRef] [PubMed]
| Vourazeris, 2017 | Friedman, 2017 | Werner, 2018 | Franceschetti, 2019 | |
|---|---|---|---|---|
| Clearly stated aims | 2 | 2 | 2 | 2 |
| Consecutive patients | 2 | 1 | 2 | 2 |
| Prospective data collection | 0 | 0 | 0 | 2 |
| Appropriate endpoints | 2 | 2 | 2 | 2 |
| Unbiased assessment | 2 | 2 | 2 | 2 |
| Appropriate follow-up | 2 | 2 | 2 | 2 |
| <5% lost to follow-up | 0 | 2 | 2 | 2 |
| Prospective study size calculation | 0 | 0 | 0 | 0 |
| Adequate control group | 2 | 2 | 2 | 2 |
| Contemporary groups | 2 | 2 | 2 | 2 |
| Baseline comparability | 2 | 1 | 2 | 2 |
| Adequate statistic | 2 | 2 | 2 | 2 |
| Total | 18 | 18 | 20 | 22 |
| Author | Journal | Group | Number | M/F | Age Mean (SD) | FU Mean (SD) | Prosthetic Design | Indications for Surgery |
|---|---|---|---|---|---|---|---|---|
| Vourazeris, 2016 | JSES | SR NR | 86 116 | - | 71.6 71.1 | 39.6 37.2 | MGLH+ * | Cuff tear arthropathy RCT with OA Rheumatoid arthritis Avascular necrosis of the humeral head with RCT |
| Friedman, 2016 | JSES | SR NR | 340 251 | 119/221 146/105 | 72.9 71.9 | 37.3 35.7 | MGLH+ * | Cuff tear arthropathy RCT with OA Rheumatoid arthritis |
| Werner, 2018 | JAAOS | SR NR | 71 38 | 28/43 15/23 | 71.1 (10.7) 70.7 (8.6) | 24 (18) 25.2 (18) | LGLH+ ** | Cuff tear arthropathy RCT with OA |
| Franceschetti, 2018 | Int Ort | SR NR | 38 38 | 10/34 11/29 | 70.1 (10.6) 69.7 (6.1) | 15.9 (1.2) 16.9 (1.9) | MGLH+ ** | Cuff tear arthropathy |
| Vourazeris, 2016 | Friedman, 2016 | Franceschetti, 2018 | Werner, 2018 | |||||
|---|---|---|---|---|---|---|---|---|
| SR | NR | SR | NR | SR | NR | SR | NR | |
| Range of motion | ||||||||
| Abduction (°) mean (SD) | 109 | 122 | 107 (23) | 119 (31) | 112.2 (31.6) | 128.1 (39.5) | ||
| Forward flexion (°) mean (SD) | 141 (24) | 137(29) | 116.3 (38.8) | 114.1 (34.4) | ||||
| External rotation at 0° (°) mean (SD) | 24 | 26 | 34 (15) | 35 (19) | 25.9 (21.2) | 28.6 (15.3) | ||
| Internal rotation (°) mean (SD) | 5.1 (1.3) | 4.4 (1.6) | 5.1 (1.28) | 4.5 (0.9) | ||||
| Clinical outcomes | ||||||||
| Constant mean (SD) | 72.6 | 72.7 | 72.9 (12.5) | 67.9 (14.6) | 54.7 (19.2) | 52.9 (20.3) | ||
| ASES mean (SD) | 77.7 | 79.3 | 86.7 (15.8) | 82.1 (18.2) | 37.9 (20.9) | 36.6 (15.3) | ||
| Vourazeris, 2016 | Friedman, 2016 | Franceschetti, 2018 | Werner, 2018 | |||||
|---|---|---|---|---|---|---|---|---|
| SR | NR | SR | NR | SR | NR | SR | NR | |
| Range of motion | ||||||||
| Abduction (°) mean (SD) | 109 | 122 | 107 (23) | 119 (31) | 112.2 (31.6) | 128.1 (39.5) | ||
| Forward flexion (°) mean (SD) | 141 (24) | 137(29) | 116.3 (38.8) | 114.1 (34.4) | ||||
| External rotation at 0° (°) mean (SD) | 24 | 26 | 34 (15) | 35 (19) | 25.9 (21.2) | 28.6 (15.3) | ||
| Internal rotation (°) mean (SD) | 5.1 (1.3) | 4.4 (1.6) | 5.1 (1.28) | 4.5 (0.9) | ||||
| Clinical outcomes | ||||||||
| Constant mean (SD) | 72.6 | 72.7 | 72.9 (12.5) | 67.9 (14.6) | 54.7 (19.2) | 52.9 (20.3) | ||
| ASES mean (SD) | 77.7 | 79.3 | 86.7 (15.8) | 82.1 (18.2) | 37.9 (20.9) | 36.6 (15.3) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Corona, K.; Cerciello, S.; Ciolli, G.; Proietti, L.; D'Ambrosi, R.; Braile, A.; Toro, G.; Romano, A.M.; Ascione, F. Clinical Outcomes and Joint Stability after Lateralized Reverse Total Shoulder Arthroplasty with and without Subscapularis Repair: A Meta-Analysis. J. Clin. Med. 2021, 10, 3014. https://doi.org/10.3390/jcm10143014
Corona K, Cerciello S, Ciolli G, Proietti L, D'Ambrosi R, Braile A, Toro G, Romano AM, Ascione F. Clinical Outcomes and Joint Stability after Lateralized Reverse Total Shoulder Arthroplasty with and without Subscapularis Repair: A Meta-Analysis. Journal of Clinical Medicine. 2021; 10(14):3014. https://doi.org/10.3390/jcm10143014
Chicago/Turabian StyleCorona, Katia, Simone Cerciello, Gianluca Ciolli, Lorenzo Proietti, Riccardo D'Ambrosi, Adriano Braile, Giuseppe Toro, Alfonso Maria Romano, and Francesco Ascione. 2021. "Clinical Outcomes and Joint Stability after Lateralized Reverse Total Shoulder Arthroplasty with and without Subscapularis Repair: A Meta-Analysis" Journal of Clinical Medicine 10, no. 14: 3014. https://doi.org/10.3390/jcm10143014
APA StyleCorona, K., Cerciello, S., Ciolli, G., Proietti, L., D'Ambrosi, R., Braile, A., Toro, G., Romano, A. M., & Ascione, F. (2021). Clinical Outcomes and Joint Stability after Lateralized Reverse Total Shoulder Arthroplasty with and without Subscapularis Repair: A Meta-Analysis. Journal of Clinical Medicine, 10(14), 3014. https://doi.org/10.3390/jcm10143014






