Forward Left Ventricular Ejection Fraction as a Predictor of Postoperative Left Ventricular Dysfunction in Patients with Degenerative Mitral Regurgitation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Echocardiographic Data
2.3. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- d‘Arcy, J.L.; Coffey, S.; Loudon, M.A.; Kennedy, A.; Pearson-Stuttard, J.; Birks, J.; Frangou, E.; Farmer, A.J.; Mant, D.; Wilson, J.; et al. Large-scale community echocardiographic screening reveals a major burden of undiagnosed valvular heart disease in older people: The OxVALVE Population Cohort Study. Eur. Heart J. 2016, 37, 3515–3522. [Google Scholar] [CrossRef]
- Nishimura, R.A.; Otto, C.M.; Bonow, R.O.; Carabello, B.A.; Erwin, J.P.; Fleisher, L.A.; Jneid, H.; Mack, M.J.; McLeod, C.J.; O’Gara, P.T.; et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation 2017, 135, e1159–e1195. [Google Scholar] [CrossRef]
- Crawford, M.H.; Souchek, J.; Oprian, C.A.; Miller, D.C.; Rahimtoola, S.; Giacomini, J.C.; Sethi, G.; Hammermeister, K.E. Determinants of survival and left ventricular performance after mitral valve replacement. Department of Veterans Affairs Cooperative Study on Valvular Heart Disease. Circulation 1990, 81, 1173–1181. [Google Scholar] [CrossRef] [PubMed]
- Enriquez-Sarano, M.; Tajik, A.J.; Schaff, H.; Orszulak, T.A.; Bailey, K.R.; Frye, R.L. Echocardiographic prediction of survival after surgical correction of organic mitral regurgitation. Circulation 1994, 90, 830–837. [Google Scholar] [CrossRef] [PubMed]
- Dujardin, K.S.; Seward, J.B.; Orszulak, T.A.; Schaff, H.; Bailey, K.R.; Tajik, A.J.; Enriquez-Sarano, M. Outcome after surgery for mitral regurgitation. Determinants of postoperative morbidity and mortality. J. Heart Valve Dis. 1997, 6, 17–21. [Google Scholar]
- Suri, R.M.; Vanoverscheide, J.-L.; Grigioni, F.; Schaff, H.V.; Tribouilloy, C.; Avierinos, J.-F.; Barbieri, A.; Pasquet, A.; Huebner, M.; Rusinaru, D.; et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. Surv. Anesthesiol. 2014, 58, 271–272. [Google Scholar] [CrossRef]
- Quintana, E.; Suri, R.M.; Thalji, N.M.; Daly, R.C.; Dearani, J.A.; Burkhart, H.M.; Li, Z.; Enriquez-Sarano, M.; Schaff, H.V. Left ventricular dysfunction after mitral valve repair—The fallacy of ”normal” preoperative myocardial function. J. Thorac. Cardiovasc. Surg. 2014, 148, 2752–2760. [Google Scholar] [CrossRef]
- Tribouilloy, C.; Rusinaru, D.; Szymanski, C.; Mezghani, S.; Fournier, A.; Lévy, F.; Peltier, M.; Ben Ammar, A.; Carmi, D.; Remadi, J.-P.; et al. Predicting left ventricular dysfunction after valve repair for mitral regurgitation due to leaflet prolapse: Additive value of left ventricular end-systolic dimension to ejection fraction. Eur. J. Echocardiogr. 2011, 12, 702–710. [Google Scholar] [CrossRef]
- Enriquez-Sarano, M.; Tajik, A.; Schaff, H.; Orszulak, T.A.; McGoon, M.D.; Bailey, K.R.; Frye, R.L. Echocardiographic prediction of left ventricular function after correction of mitral regurgitation: Results and clinical implications. J. Am. Coll. Cardiol. 1994, 24, 1536–1543. [Google Scholar] [CrossRef]
- Matsumura, T.; Ohtaki, E.; Tanaka, K. Echocardiographic prediction of left ventricular dysfunction after mitral valve repair for mitral regurgitation as an indicator to decide the optimal timing of repair. J. Am. Coll. Cardiol. 2004, 13, 28. [Google Scholar] [CrossRef]
- Pandis, D.; Sengupta, P.P.; Castillo, J.G.; Caracciolo, G.; Fischer, G.W.; Narula, J.; Anyanwu, A.; Adams, D.H. Assessment of longitudinal myocardial mechanics in patients with degenerative mitral valve regurgitation predicts postoperative worsening of left ventricular systolic function. J. Am. Soc. Echocardiogr. 2014, 27, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Witkowski, T.; Thomas, J.D.; Debonnaire, P.J.; Delgado, V.; Hoke, U.; Ewe, S.H.; Versteegh, M.I.; Holman, E.R.; Schalij, M.J.; Bax, J.J.; et al. Global longitudinal strain predicts left ventricular dysfunction after mitral valve repair. Eur. Heart. J. Cardiovasc. Imaging. 2013, 14, 69–76. [Google Scholar] [CrossRef]
- Suri, R.M.; Schaff, H.; Dearani, J.A.; Sundt, T.M.; Daly, R.C.; Mullany, C.J.; Sarano, M.E.; Orszulak, T.A. Determinants of early decline in ejection fraction after surgical correction of mitral regurgitation. J. Thorac. Cardiovasc. Surg. 2008, 136, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, M.; Mahjoub, H.; Clavel, M.-A.; Côté, N.; Toubal, O.; Tastet, L.; Dumesnil, J.G.; O’Connor, K.; Dahou, A.; Thébault, C.; et al. Forward left ventricular ejection fraction: A simple risk marker in patients with primary mitral regurgitation. J. Am. Heart. Assoc. 2017, 6. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, C.; Rahko, P.S.; Blauwet, L.A.; Canaday, B.; Finstuen, J.A.; Foster, M.C.; Horton, K.; Ogunyankin, K.O.; Palma, R.A.; Velazquez, E.J. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: Recommendations from the american society of echocardiography. J. Am. Soc. Echocardiogr. 2019, 32, 1–64. [Google Scholar] [CrossRef] [PubMed]
- Zoghbi, W.A.; Adams, D.; Bonow, R.O.; Enriquez-Sarano, M.; Foster, E.; Grayburn, P.A.; Hahn, R.T.; Han, Y.; Hung, J.; Lang, R.M.; et al. Recommendations for noninvasive evaluation of native valvular regurgitation: A report from the American society of echocardiography developed in collaboration with the society for cardiovascular magnetic resonance. J. Am. Soc. Echocardiogr. 2020, 4, 58. [Google Scholar] [CrossRef]
- Shimizu, G.; Hirota, Y.; Kita, Y.; Kawamura, K.; Saito, T.; Gaasch, W.H. Left ventricular midwall mechanics in systemic arterial hypertension. Myocardial function is depressed in pressure-overload hypertrophy. Circulation 1991, 83, 1676–1684. [Google Scholar] [CrossRef] [PubMed]
- Gaasch, W.H.; Zile, M.; Hoshino, P.K.; Apstein, C.S.; Blaustein, A.S.; Gaasch, W.H.; Zile, M.; Hoshino, P.K.; Apstein, C.S.; Blaustein, A.S. Stress-shortening relations and myocardial blood flow in compensated and failing canine hearts with pressure-overload hypertrophy. Circulation 1989, 79, 872–883. [Google Scholar] [CrossRef]
- de Simone, G.; Devereux, R.B.; Roman, M.J.; Ganau, A.; Saba, P.S.; Alderman, M.H.; Laragh, J.H. Assessment of left ventricular function by the midwall fractional shortening/end-systolic stress relation in human hypertension. J. Am. Coll. Cardiol. 1994, 23, 1444–1451. [Google Scholar] [CrossRef]
- Kitkungvan, D.; Nabi, F.; Kim, R.J.; Bonow, R.O.; Khan, A.; Xu, J.; Little, S.H.; Quinones, M.A.; Lawrie, G.M.; Zoghbi, W.A.; et al. Myocardial fibrosis in patients with primary mitral regurgitation with and without prolapse. J. Am. Coll. Cardiol. 2018, 72, 823–834. [Google Scholar] [CrossRef] [PubMed]
- Edwards, N.C.; Moody, W.E.; Yuan, M.; Weale, P.; Neal, D.; Townend, J.; Steeds, R. Quantification of left ventricular interstitial fibrosis in asymptomatic chronic primary degenerative mitral regurgitation. Circ. Cardiovasc. Imaging 2014, 7, 946–953. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, M.I.; Gladden, J.D.; Litovsky, S.H.; Lloyd, S.G.; Gupta, H.; Inusah, S.; Denney, T.; Powell, P.; McGiffin, D.C.; Dell’Italia, L.J. Increased oxidative stress and cardiomyocyte myofibrillar degeneration in patients with chronic isolated mitral regurgitation and ejection fraction > 60%. J. Am. Coll. Cardiol. 2010, 55, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Van De Heyning, C.M.; Magne, J.; Pierard, L.A.; Bruyère, P.J.; Davin, L.; De Maeyer, C.; Paelinck, B.P.; Vrints, C.J.; Lancellotti, P. Late gadolinium enhancement CMR in primary mitral regurgitation. Eur. J. Clin. Investig. 2014, 44, 840–847. [Google Scholar] [CrossRef] [PubMed]
- Marciniak, A.; Claus, P.; Sutherland, G.R.; Marciniak, M.; Karu, T.; Baltabaeva, A.; Merli, E.; Bijnens, B.; Jahangiri, M. Changes in systolic left ventricular function in isolated mitral regurgitation. A strain rate imaging study. Eur. Heart J. 2007, 28, 2627–2636. [Google Scholar] [CrossRef][Green Version]
- Gelfand, E.V.; Haffajee, J.A.; Hauser, T.H.; Yeon, S.B.; Goepfert, L.; Kissinger, K.V.; Delatorre, R.; Manning, W.J. Predictors of preserved left ventricular systolic function after surgery for chronic organic mitral regurgitation: A prospective study. J. Heart Valve Dis. 2010, 19, 43–50. [Google Scholar]
- Trevethan, R. Sensitivity, specificity, and predictive values: Foundations, pliabilities, and pitfalls in research and practice. Front. Public Health 2017, 5, 307. [Google Scholar] [CrossRef]
- Abhayaratna, W.; Seward, J.B.; Appleton, C.P.; Douglas, P.S.; Oh, J.K.; Tajik, A.J.; Tsang, T.S. Left atrial size: Physiologic determinants and clinical applications. J. Am. Coll. Cardiol. 2006, 47, 2357–2363. [Google Scholar] [CrossRef]
- Beaufils, A.C.F.; Huttin, O.; Jobbe-Duval, A.; Senage, T.S.; Filippetti, L.; Piriou, N.; Cueff, C.; Venner, C.; Mandry, D.; Sellal, J.M.; et al. Replacement myocardial fibrosis in patients with mitral valve prolapse: Relation to mitral regurgitation, ventricular remodeling, and arrhythmia. Circulation 2021, 143, 1763–1774. [Google Scholar] [CrossRef] [PubMed]
- Moreo, A.; Ambrosio, G.; De Chiara, B.; Pu, M.; Tran, T.; Mauri, F.; Raman, S.V. Influence of myocardial fibrosis on left ventricular diastolic function: Noninvasive assessment by cardiac magnetic resonance and echo. Circ. Cardiovasc. Imaging 2009, 2, 437–443. [Google Scholar] [CrossRef]
- Kebed, K.; Sun, D.; Addetia, K.; Mor-Avi, V.; Markuzon, N.; Lang, R.M. Measurement errors in serial echocardiographic assessments of aortic valve stenosis severity. Int. J. Cardiovasc. Imaging 2020, 36, 471–479. [Google Scholar] [CrossRef]

| Total | LVD | Non-LVD | p | |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 51.8 ± 11.8 | 52.2 ± 10.8 | 51.7 ± 12.1 | 0.781 |
| Male | 165 (70.5) | 37 (71.2) | 127 (69.8) | 1.0 |
| BMI (kg/m2) | 24.7 (22.5–26.5) | 24.3 (21.6–25.9) | 24.7 (22.7–26.7) | 0.113 |
| Comorbidities | ||||
| DM | 41 (17.5) | 12 (23.1) | 29 (15.9) | 0.3 |
| HTN | 93 (39.7) | 20 (38.5) | 73 (40.1) | 0.873 |
| CVA | 5 (2.1) | 0 (0) | 5 (2.7) | 0.589 |
| PVD | 2 (0.9) | 0 (0) | 2 (1.1) | 1.0 |
| COPD | 7 (3.0) | 0 (0) | 7 (3.8) | 0.353 |
| CKD | 6 (2.6) | 3 (5.8) | 3 (1.6) | 0.005 |
| A-fib | 26 (11.1) | 11 (21.2) | 15 (8.2) | 0.021 |
| Euroscore Ⅱ | 0.7 (0.5–1.0) | 0.7 (0.6–1.0) | 0.7(0.5–1.0) | 0.445 |
| Preoperative Medication | ||||
| ACEI/ARB | 112 (47.9) | 26(50.0) | 86 (47.3) | 0.755 |
| β-blocker | 68 (29.1) | 16 (30.8) | 52 (28.6) | 0.733 |
| CCB | 52 (22.2) | 13 (25.0) | 39 (21.4) | 0.575 |
| Digoxin | 15 (6.4) | 3 (5.8) | 12 (6.6) | 1.0 |
| Diuretics | 107 (45.7) | 25 (48.1) | 82 (45.1) | 0.753 |
| Intraoperative Data | ||||
| Op time (mins) | 275.0 (237.0–323.3) | 256.5 (233.3–305.0) | 280.0 (237.0–325.0) | 0.187 |
| CPB time (mins) | 140.0 (115.8–170.0) | 144.5 (113.0–167.5) | 138.0 (115.8–170.5) | 0.679 |
| ACC time (mins) | 77.5 (64.0–99.0) | 84.0 (71.3–107.0) | 77.0 (63.0–96.0) | 0.093 |
| Colloid (L) | 0.5 (0.3–0.5) | 0.5 (0.4–0.5) | 0.5 (0.3–0.5) | 0.095 |
| Crystalloid (L) | 1.5 (1.2–1.8) | 1.5 (1.0–1.6) | 1.5 (1.2–1.8) | 0.073 |
| Total | LVD | Non-LVD | p | |
|---|---|---|---|---|
| LVEF | 68.0 (65.0–71.0) | 66.5 (64.0–69.0) | 68.0 (65.0–72.0) | 0.020 |
| LVESD | 36.7 ± 5.2 | 40.3 ± 4.9 | 35.6 ± 4.8 | <0.001 |
| LVEDD | 59.6 ± 5.5 | 63.8 ± 4.5 | 58.4 ± 5.1 | <0.001 |
| LVESV | 56.0 (43.0–68.0) | 70.5 (58.0–80.0) | 51.5 (41.0–62.3) | <0.001 |
| LVEDV | 172.0 (141.8–209.3) | 210.5 (184.3–238.5) | 163.0 (137.0–197.0) | <0.001 |
| RWT | 0.32 (0.29–0.35) | 0.30 (0.27–0.32) | 0.33 (0.29–0.36) | <0.001 |
| LVMI | 129.3 (112.3–151.6) | 149.6 (133.3–168.5) | 123.5 (108.5–141.9) | <0.001 |
| LAD | 47.0 (43.0–53.0) | 49.5 (46.3–55.8) | 46.0 (43.0–52.0) | <0.001 |
| PGTR | 29.0 (23.0–36.0) | 29.0 (27.0–38.0) | 27.0 (23.0–36.0) | 0.104 |
| E/A | 2.0 (1.5–2.5) | 2.2 (1.7–2.5) | 1.9 (1.4–2.6) | 0.303 |
| S′ | 7.9 (7.0–8.7) | 7.9 (7.1–8.9) | 7.9 (7.0–8.7) | 0.568 |
| E′ | 8.0 (6.4–9.9) | 8.3 (6.3–9.6) | 8.0 (6.5–10.0) | 0.897 |
| A′ | 7.5 (6.2–8.9) | 7.1 ± 1.7 | 7.6 ± 1.9 | 0.098 |
| E/E′ | 14.0 (11.0–19.0) | 15.5 (11.3–19.8) | 14.0 (11.0–19.0) | 0.234 |
| cESS | 135.8 (113.2–161.3) | 154.0 (129.8–170.5) | 131.9 (112.2–157.9) | 0.006 |
| mFS | 20.3 (18.6–21.9) | 20.2 (18.7–21.9) | 20.3 (18.5–21.9) | 0.843 |
| sc-mFS | 118.9 (109.5–130.4) | 123.7 (111.9–131.3) | 118.2 (108.3–130.4) | 0.114 |
| Forward SV | 53.1 (45.0–60.6) | 50.1 (43.3–59.2) | 54.0 (46.0–61.8) | 0.074 |
| Forward LVEF | 31.4 (24.9–37.4) | 24.0 (18.9–29.5) | 33.2 (26.8–39.4) | <0.001 |
| EROA | 0.8 (0.6–1.1) | 1.0 (0.8–1.3) | 0.8 (0.6–1.1) | <0.001 |
| RVol | 64.5 (44.0–86.4) | 85.7 (69.6–110.8) | 57.5 (39.3–78.0) | <0.001 |
| RF | 54.0 (45.4–62.7) | 62.7 (54.4–70.1) | 51.8 (41.5–60.0) | <0.001 |
| LVD | Non-LVD | |||||||
|---|---|---|---|---|---|---|---|---|
| Pre | Post | p * | Pre | Post | p * | p † | p‡ | |
| LVEDV (preload) | 210.5 (184.3–238.5) | 141.5 (119.3–187.3) | <0.001 | 163.0 (137.0–197.0) | 114.0 (95.8–137.0) | <0.001 | <0.001 | <0.001 |
| cESS (afterload) | 154.0 (129.8–170.5) | 151.3 (133.4–186.7) | 0.122 | 131.9 (112.2–157.9) | 120.8 (101.9–138.5) | <0.001 | 0.006 | <0.001 |
| LVEF | 66.5 (64.0–69.0) | 45.0 (41.0–48.8) | <0.001 | 68.0 (65.0–72.0) | 58.0 (55.0–62.0) | <0.001 | 0.020 | <0.001 |
| S′ | 7.9 (7.1–8.9) | 5.5 (4.8–6.3) | <0.001 | 7.9 (7.0–8.7) | 6.8 (5.9–7.9) | <0.001 | 0.568 | <0.001 |
| mFS | 20.2 (18.7–21.9) | 13.4 (12.1–15.3) | <0.001 | 20.3 (18.5–21.9) | 16.0 (14.4–17.5) | <0.001 | 0.843 | <0.001 |
| sc-mFS | 123.7 (111.9–131.3) | 82.5 (72.3–92.0) | <0.001 | 118.2 (108.3–130.4) | 91.9 (84.9–100.2) | <0.001 | 0.114 | <0.001 |
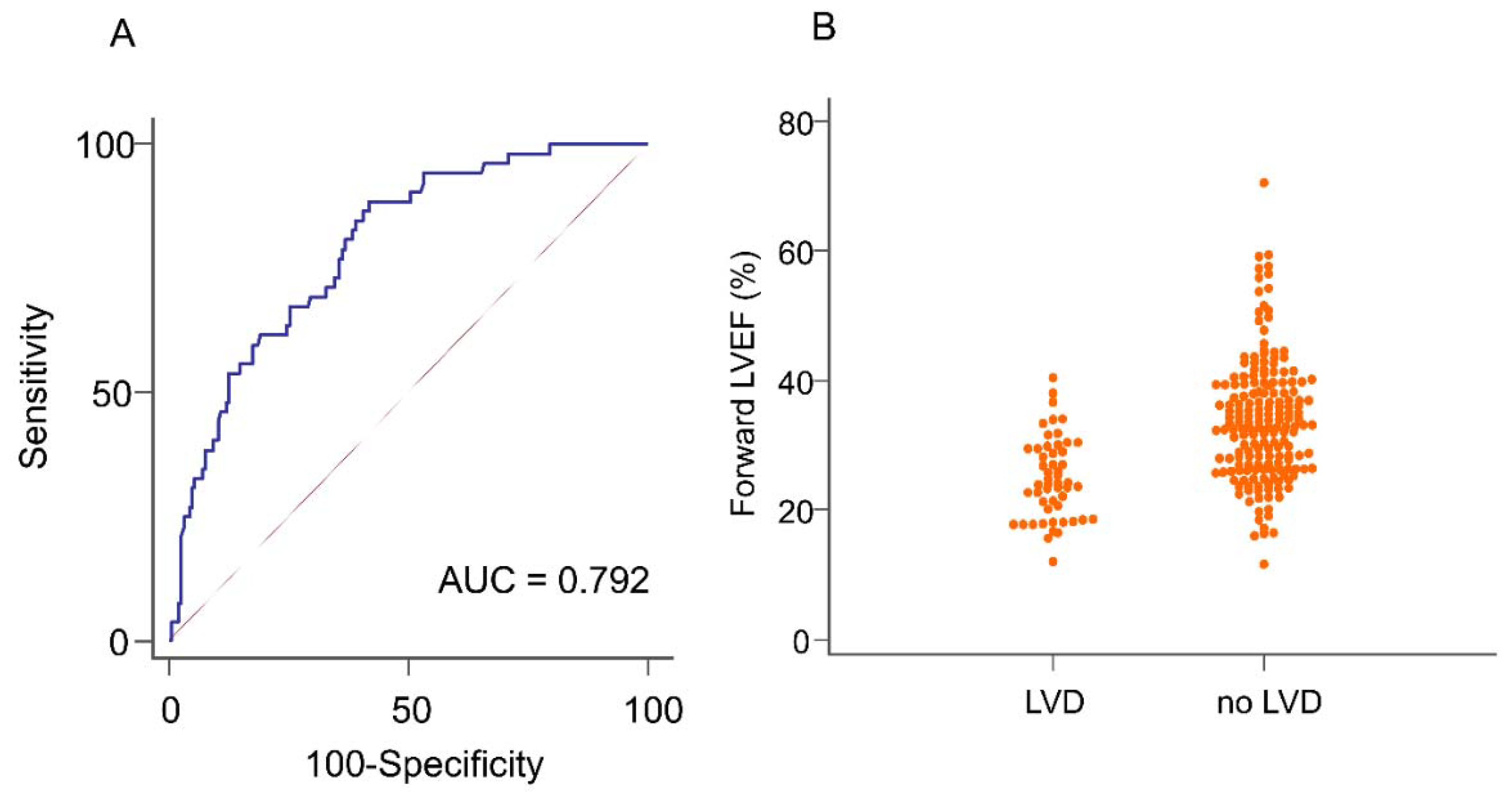
| AUC (95% CI) | Cut-off | Sen (%) | Spe (%) | PPV (%) | NPV (%) | |
|---|---|---|---|---|---|---|
| LVESD (mm) | 0.75(0.67–0.83) | 38.0 | 65.4 | 74.2 | 42.0 | 88.2 |
| Forward LVEF (%) | 0.79 (0.73–0.86) | 31.8 | 88.5 | 58.2 | 37.7 | 94.6 |
| RVol (mL) | 0.78 (0.71–0.84) | 73.5 | 73.1 | 70.3 | 41.3 | 90.1 |
| RF (%) | 0.77(0.70–0.84) | 60.6 | 65.4 | 78.6 | 46.6 | 88.8 |
| LVEDV (mL) | 0.77 (0.70–0.84) | 196.0 | 71.2 | 74.2 | 43.0 | 89.8 |
| LVESV (mL) | 0.78 (0.72–0.85) | 55.0 | 86.5 | 58.8 | 36.0 | 93.6 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Nam, J.-S.; Kim, Y.; Chin, J.-H.; Choi, I.-C. Forward Left Ventricular Ejection Fraction as a Predictor of Postoperative Left Ventricular Dysfunction in Patients with Degenerative Mitral Regurgitation. J. Clin. Med. 2021, 10, 3013. https://doi.org/10.3390/jcm10143013
Kim J, Nam J-S, Kim Y, Chin J-H, Choi I-C. Forward Left Ventricular Ejection Fraction as a Predictor of Postoperative Left Ventricular Dysfunction in Patients with Degenerative Mitral Regurgitation. Journal of Clinical Medicine. 2021; 10(14):3013. https://doi.org/10.3390/jcm10143013
Chicago/Turabian StyleKim, Juyoun, Jae-Sik Nam, Youngdo Kim, Ji-Hyun Chin, and In-Cheol Choi. 2021. "Forward Left Ventricular Ejection Fraction as a Predictor of Postoperative Left Ventricular Dysfunction in Patients with Degenerative Mitral Regurgitation" Journal of Clinical Medicine 10, no. 14: 3013. https://doi.org/10.3390/jcm10143013
APA StyleKim, J., Nam, J.-S., Kim, Y., Chin, J.-H., & Choi, I.-C. (2021). Forward Left Ventricular Ejection Fraction as a Predictor of Postoperative Left Ventricular Dysfunction in Patients with Degenerative Mitral Regurgitation. Journal of Clinical Medicine, 10(14), 3013. https://doi.org/10.3390/jcm10143013






