Symptoms and Quality of Life Changes after Hysteroscopic Treatment in Patients with Symptomatic Isthmocele—Preliminary Results
Abstract
:1. Introduction
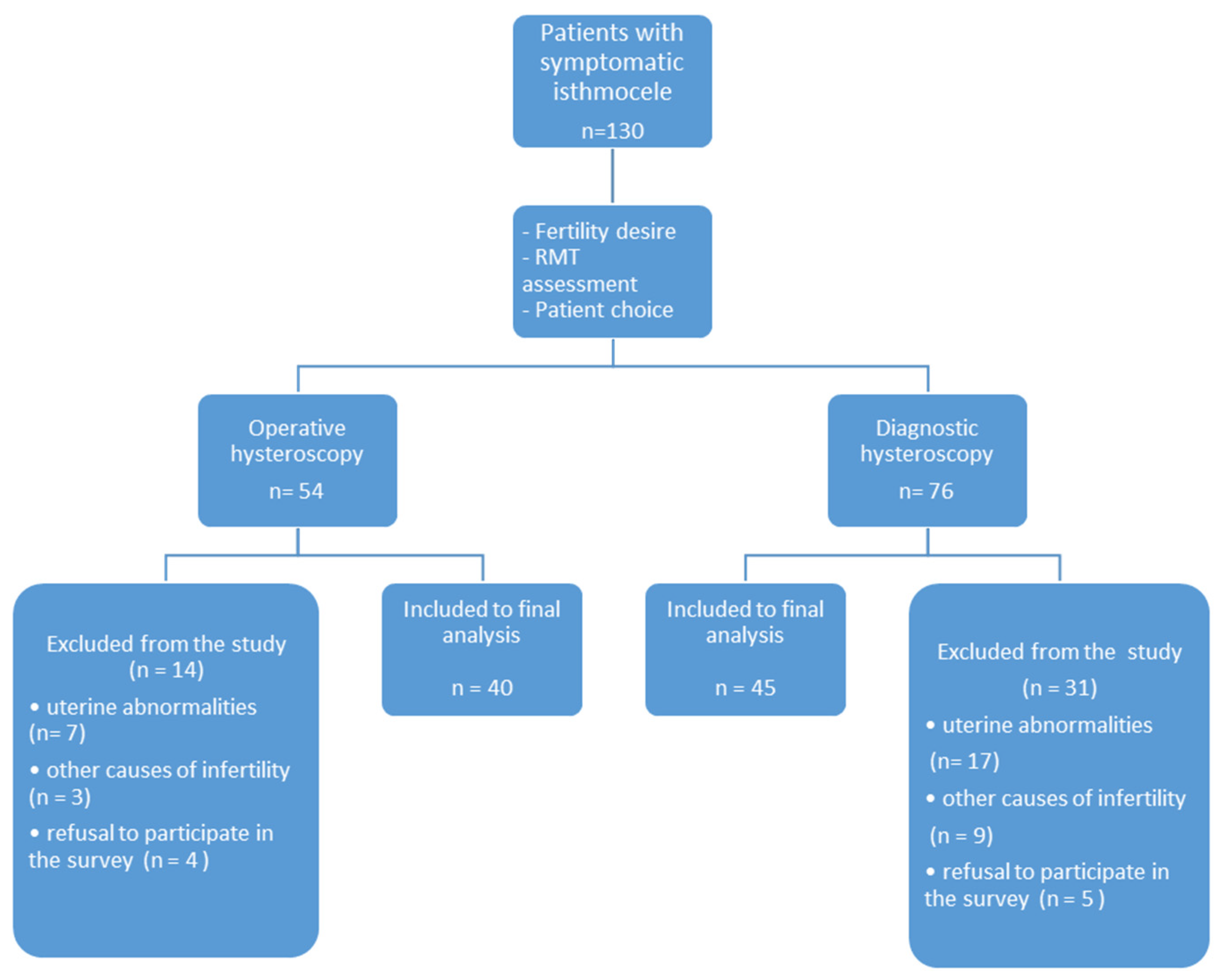
2. Materials and Methods
Statistical Analysis
3. Results
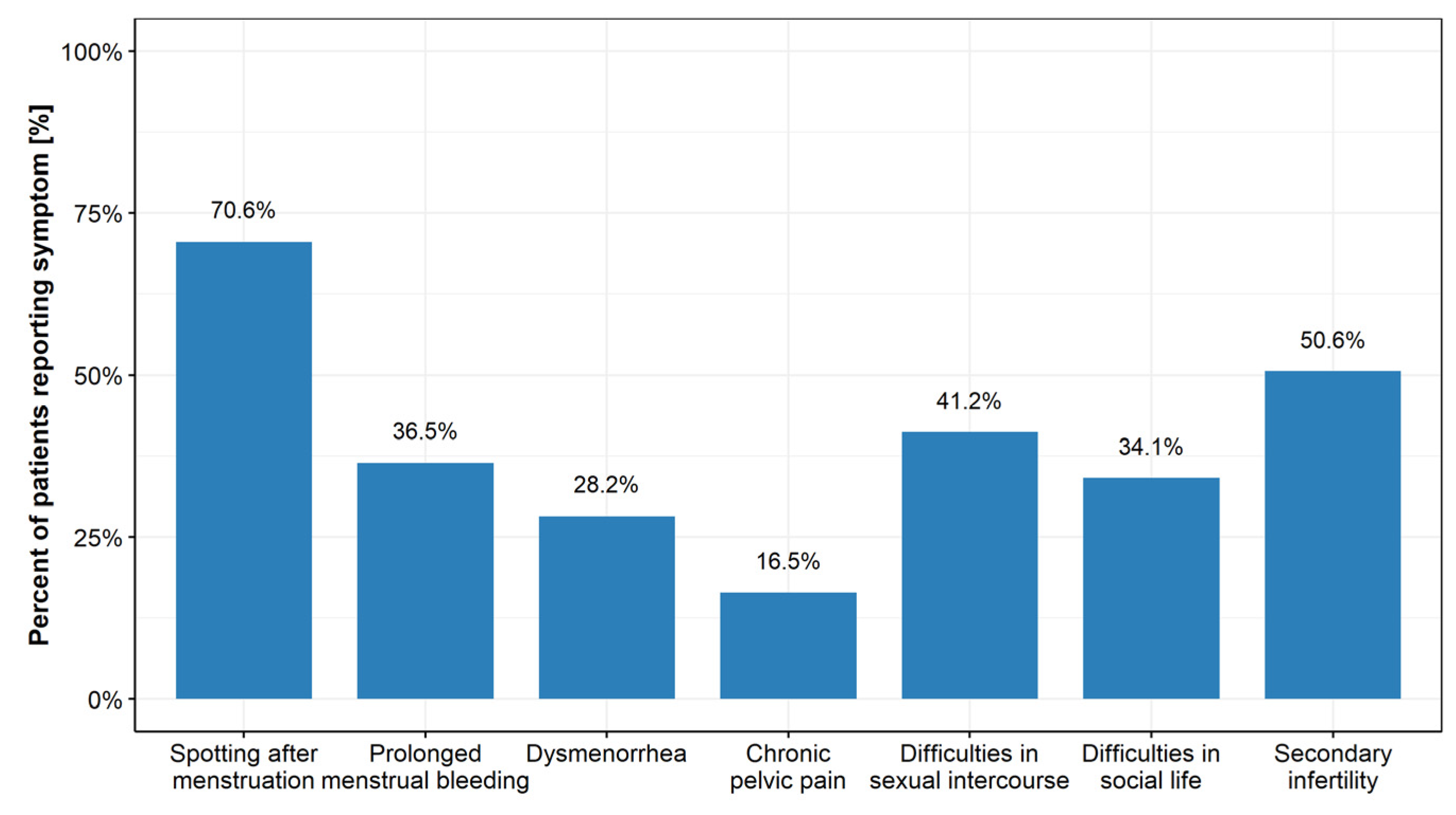
3.1. Characteristics of the Study Population
3.1.1. Physical Health
3.1.2. Subfertility
3.1.3. Psychological and Environmental Aspect
3.1.4. Social Health
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stegwee, S.I.; Beij, A.; de Leeuw, R.A.; Mokkink, L.B.; van der Voet, L.F.; Huirne, J.A.F. Niche-related outcomes after caesarean section and quality of life: A focus group study and review of literature. Qual. Life Res. 2020, 29, 1013–1025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Baranowski, W.; Doniec, J.; Szafarowska, M. Isthmocele—Treat or not to treat? AJBSR Am. J. Biomed. Sci. Res. 2020, 7, 472–474. [Google Scholar]
- Vitale, S.G.; Ludwin, A.; Vilos, G.A.; Török, P.; Tesarik, J.; Vitagliano, A.; Lasmar, R.B.; Chiofalo, B. From hysteroscopy to laparoendoscopic surgery: What is the best surgical approach for symptomatic isthmocele? A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2020, 301, 33–52. [Google Scholar] [CrossRef] [PubMed]
- Jordans, I.P.M.; de Leeuw, R.A.; Stegwee, S.I.; Amso, N.N.; Barri-Soldevila, P.N.; van den Bosch, T.; Bourne, T.; Brölmann, H.A.M.; Donnez, O.; Dueholm, M.; et al. Sonographic examination of uterine niche in non-pregnant women: A modified Delphi procedure. Ultrasound Obstet. Gynecol. 2019, 53, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Bettocchi, S. New Era of Office Hysteroscopy. J. Am. Assoc. Gynecol. Laparosc. 1996, 3, S4. [Google Scholar] [CrossRef]
- Betran, A.P.; Ye, J.; Moller, A.B.; Zhang, J.; Gulmezoglu, A.M.; Torloni, M.R. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE 2016, 5, e0148343. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wielgos, M.; Bomba-Opon, D.; Breborowicz, G.H.; Czajkowski, K.; Debski, R.; Leszczynska-Gorzelak, B.; Oszukowski, P.; Radowicki, S.; Zimmer, M. Recommendations of the Polish Society of Gynecologists and Obstetricians regarding caesarean sections. Ginekol. Pol. 2018, 89, 644–657. [Google Scholar] [CrossRef] [PubMed]
- Donnez, J. An update on uterine cervix pathologies related to infertility. Fertil. Steril. 2020, 113, 683–684. [Google Scholar] [CrossRef] [PubMed]
- Muzii, L.; Domenici, L.; Lecce, F.; Di Feliciantonio, M.; Frantellizzi, R.; Marchetti, C.; Monti, M.; Benedetti Panici, P. Clinical outcomes after resectoscopic treatment of cesarean-induced isthmocele: A prospective case-control study. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 3341–3346. [Google Scholar] [PubMed]
- Mashiach, R.; Burke, Y.Z. Optimal Isthmocele Management: Hysteroscopic, Laparoscopic, or Combination. J. Minim. Invasive Gynecol. 2021, 28, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Kremer, T.G.; Ghiorzi, I.B.; Dibi, R.P. Isthmocele: An overview of diagnosis and treatment. Rev. Assoc. Med. Bras. 2019, 65, 714–721. [Google Scholar] [CrossRef] [PubMed]
- Tan, D.A.; Haththotuwa, R.; Fraser, I.S. Cultural aspects and mythologies surrounding menstruation and abnormal uterine bleeding. Best Pract. Res. Clin. Obstet. Gynaecol. 2017, 40, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Guo, Y.; Liu, Y.; Cheng, J.; Zhang, W. Hysteroscopic and laparoscopic management of uterine defects on previous cesarean delivery scars. J. Peérinat. Med. 2014, 42, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Tsuji, S.; Kimura, F.; Yamanaka, A.; Hanada, T.; Hirata, K.; Takebayashi, A.; Takashi, M.; Seko-Nitta, A.; Murakami, T. Impact of hysteroscopic surgery for isthmocele associated with cesarean scar syndrome. J. Obstet. Gynaecol. Res. 2018, 44, 43–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tanimura, S.; Funamoto, H.; Hosono, T.; Shitano, Y.; Nakashima, M.; Ametani, Y.; Nakano, T. New diagnostic criteria and operative strategy for cesarean scar syndrome: Endoscopic repair for secondary infertility caused by cesarean scar defect. J. Obstet. Gynaecol. Res. 2015, 41, 1363–1369. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vissers, J.; Hehenkamp, W.; Lambalk, C.B.; Huirne, J.A. Post-Caesarean section niche-related impaired fertility: Hypothetical mechanisms. Hum. Reprod. 2020, 35, 1484–1494. [Google Scholar] [CrossRef] [PubMed]
- Vissers, J.; Sluckin, T.C.; van Driel-Delprat, C.C.R.; Schats, R.; Groot, C.J.M.; Lambalk, C.B.; Twisk, J.W.R.; Huirne, J.A.F. Reduced pregnancy and live birth rates after in vitro fertilization in women with previous Caesarean section: A retrospective cohort study. Hum. Reprod. 2020, 35, 595–604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Donnez, O. Cesarean scar defects: Management of an iatrogenic pathology whose prevalence has dramatically increased. Fertil. Steril. 2020, 113, 704–716. [Google Scholar] [CrossRef] [PubMed]
| Hysteroscopy | |||||
|---|---|---|---|---|---|
| Characteristic | N | Overall, N = 85 1 | Diagnostic Hysteroscopy, N = 45 1 | Operative Hysteroscopy, N = 40 1 | p-Value 2 |
| Prolonged menses | 31 | 0.697 | |||
| improvement after hysteroscopy | 21 (67.7%) | 12 (63.2%) | 9 (75.0%) | ||
| unsuccessful treatment | 10 (32.3%) | 7 (36.8%) | 3 (25.0%) | ||
| Postmenstrual spotting | 59 | 0.018 | |||
| improvement after hysteroscopy | 38 (64.4%) | 16 (51.6%) | 22 (78.6%) | ||
| unsuccessful treatment | 21 (35.6%) | 15 (48.4%) | 6 (21.4%) | ||
| Dysmenorrhoea | 24 | >0.999 | |||
| improvement after hysteroscopy | 12 (50.0%) | 6 (46.2%) | 6 (54.5%) | ||
| unsuccessful treatment | 12 (50.0%) | 7 (53.8%) | 5 (45.5%) | ||
| Pelvic pain | 13 | >0.999 | |||
| improvement after hysteroscopy | 9 (69.2%) | 5 (71.4%) | 4 (66.7%) | ||
| unsuccessful treatment | 4 (30.8%) | 2 (28.6%) | 2 (33.3%) | ||
| Characteristic | N = 44 1 | Diagnostic Hysteroscopy | Operative Hysteroscooy | p-Value 2 |
|---|---|---|---|---|
| Pregnancy after hysteroscopy | 0.159 | |||
| YES | 18 (40.9%) | 5 (26.3%) | 13 (52.0%) | |
| NO | 26 (59.1%) | 14 (73.7%) | 12 (48.0%) |
| Characteristic | N | Overall 1 | Diagnostic Hysteroscopy 1 | Operative Hysteroscopy 1 | p-Value 2 |
|---|---|---|---|---|---|
| Avoiding participation in leisure activities | 14 | 0.266 | |||
| improvement after hysteroscopy | 9 (64.3%) | 3 (42.9%) | 6 (85.7%) | ||
| unsuccessful treatment | 5 (35.7%) | 4 (57.1%) | 1 (14.3%) | ||
| Necessity to have a toilet nearby | 9 | 0.083 | |||
| improvement after hysteroscopy | 3 (33.3%) | 1 (14.3%) | 2 (100.0%) | ||
| unsuccessful treatment | 6 (66.7%) | 6 (85.7%) | 0 (0.0%) | ||
| Limited working capacity | 4 | ||||
| improvement after hysteroscopy | 3 (75.0%) | 3 (75.0%) | 0 (NA%) | NS | |
| unsuccessful treatment | 1 (25.0%) | 1 (25.0%) | 0 (NA%) | ||
| Low self esteem | 3 | >0.999 | |||
| improvement after hysteroscopy | 2 (66.7%) | 1 (50.0%) | 1 (100.0%) | ||
| unsuccessful treatment | 1 (33.3%) | 1 (50.0%) | 0 (0.0%) | ||
| Loneliness or depression | 11 | 0.061 | |||
| improvement after hysteroscopy | 5 (45.5%) | 0 (0.0%) | 5 (71.4%) | ||
| unsuccessful treatment | 6 (54.5%) | 4 (100.0%) | 2 (28.6%) |
| Characteristic | N | Overall, N = 11 1 | Diagnostic Hysteroscopy, N = 7 1 | Operative hysteroscopy, N = 4 1 | p-Value 2 |
|---|---|---|---|---|---|
| Dyspareunia | 10 | >0.999 | |||
| improvement after hysteroscopy | 7 (70.0%) | 5 (71.4%) | 2 (66.7%) | ||
| unsuccessful treatment | 3 (30.0%) | 2 (28.6%) | 1 (33.3%) | ||
| Spotting after intercourse | 27 | 0.014 | |||
| improvement after hysteroscopy | 17 (63.0%) | 6 (40.0%) | 11 (91.7%) | ||
| unsuccessful treatment | 10 (37.0%) | 9 (60.0%) | 1 (8.3%) | ||
| Unpleasant odor | 8 | >0.999 | |||
| improvement after hysteroscopy | 4 (50.0%) | 2 (40.0%) | 2 (66.7%) | ||
| unsuccessful treatment | 4 (50.0%) | 3 (60.0%) | 1 (33.3%) | ||
| Reduced lubrication | 3 | >0.999 | |||
| improvement after hysteroscopy | 1 (33.3%) | 0 (0.0%) | 1 (50.0%) | ||
| unsuccessful treatment | 2 (66.7%) | 1 (100.0%) | 1 (50.0%) | ||
| Reduced libido | 3 | NS | |||
| improvement after hysteroscopy | 2 (66.7%) | 0 (NA%) | 2 (66.7%) | ||
| unsuccessful treatment | 1 (33.3%) | 0 (NA%) | 1 (33.3%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szafarowska, M.; Biela, M.; Wichowska, J.; Sobociński, K.; Segiet-Święcicka, A.; Doniec, J.; Kamiński, P. Symptoms and Quality of Life Changes after Hysteroscopic Treatment in Patients with Symptomatic Isthmocele—Preliminary Results. J. Clin. Med. 2021, 10, 2928. https://doi.org/10.3390/jcm10132928
Szafarowska M, Biela M, Wichowska J, Sobociński K, Segiet-Święcicka A, Doniec J, Kamiński P. Symptoms and Quality of Life Changes after Hysteroscopic Treatment in Patients with Symptomatic Isthmocele—Preliminary Results. Journal of Clinical Medicine. 2021; 10(13):2928. https://doi.org/10.3390/jcm10132928
Chicago/Turabian StyleSzafarowska, Monika, Magdalena Biela, Joanna Wichowska, Kamil Sobociński, Agnieszka Segiet-Święcicka, Jacek Doniec, and Paweł Kamiński. 2021. "Symptoms and Quality of Life Changes after Hysteroscopic Treatment in Patients with Symptomatic Isthmocele—Preliminary Results" Journal of Clinical Medicine 10, no. 13: 2928. https://doi.org/10.3390/jcm10132928
APA StyleSzafarowska, M., Biela, M., Wichowska, J., Sobociński, K., Segiet-Święcicka, A., Doniec, J., & Kamiński, P. (2021). Symptoms and Quality of Life Changes after Hysteroscopic Treatment in Patients with Symptomatic Isthmocele—Preliminary Results. Journal of Clinical Medicine, 10(13), 2928. https://doi.org/10.3390/jcm10132928






