Abstract
The current gold-standard treatment for COVID-19-related hypoxemic respiratory failure is invasive mechanical ventilation. However, do not intubate orders (DNI), prevent the use of this treatment in some cases. The aim of this study was to evaluate if non-invasive ventilatory supports can provide a good therapeutic alternative to invasive ventilation in patients with severe COVID-19 infection and a DNI. Data were collected from four centres in three European countries. Patients with severe COVID-19 infection were included. We emulated a hypothetical target trial in which outcomes were compared in patients with a DNI order treated exclusively by non-invasive respiratory support with patients who could be intubated if necessary. We set up a propensity score and an inverse probability of treatment weighting to remove confounding by indication. Four-hundred patients were included: 270 were eligible for intubation and 130 had a DNI order. The adjusted risk ratio for death among patients eligible for intubation was 0.81 (95% CI 0.46 to 1.42). The median length of stay in acute care for survivors was similar between groups (18 (10–31) vs. (19 (13–23.5); p = 0.76). The use of non-invasive respiratory support is a good compromise for patients with severe COVID-19 and a do not intubate order.
1. Introduction
Hospitals around the world have had to reorganise their services and increase their capacity due to the influx of hundreds of thousands of patients with severe COVID-19 infection. Furthermore, the severe acute respiratory failure and hypoxia induced by the disease has led to a widespread need for mechanical ventilation by orotracheal intubation [1,2,3]. Although invasive mechanical ventilation is the current gold-standard treatment for these conditions [4], it has some potential harmful effects on the pulmonary system. Prolonged mechanical ventilation has been associated with severe muscle weakness in all patients [5,6], and a high mortality rate for older patients and those with a low PaO2/FiO2 ratio [2,7]. Another issue with mechanical ventilation is that the massive influx of patients caused a shortage of equipment and induced an ethical challenge leading to a need for alternative methods of oxygenation [8,9].
In the context of limited resources, older patients and those with comorbidities, who represent a considerable proportion of patients with severe COVID-19 infection admitted to hospital, are often considered ineligible for invasive ventilation and are issued with a do not intubate (DNI) order. Therefore, during this pandemic, the use of non-invasive respiratory supports has increased throughout the world. High flow nasal cannula (HFNC) is the first line treatment to increase FiO2 and avoid intubation in patients with hypoxia [10]. Continuous Positive Airway Pressure (CPAP) can be used as a first or second line treatment, if HFNC therapy is insufficient, and its use in intensive care units (ICU) [11,12,13] as well as on conventional wards [14,15] has greatly expanded. Several treatment algorithms have been developed to guide clinicians in the non-invasive management of patients with severe COVID-19 infection [16,17]. Although the use of CPAP in the management of patients with COVID-19 is highly feasible, the results are uncertain. Several studies have reported a high rate of failure (40 to 66%) of this treatment [18,19,20], and a high rate of mortality in patients ineligible for intubation [13,21]. However, existing data are purely descriptive, and no definitive conclusions can be drawn regarding the efficacy of HFNC and CPAP in patients with a DNI order due to the lack of a comparison with a gold standard. The aim of this study is to determine if non-invasive ventilatory supports is a sufficient therapeutic alternative in patients with severe COVID-19 infection and a DNI.
2. Method
We conducted a multicentre retrospective study of data from patients admitted to 4 hospitals (Le Havre Hospital, Rouen University Hospital, Erasme Hospital, Réseau Hospitalier Neuchâtelois (RHNE) Pourtlaès Hospital) situated in three different European countries (France, Belgium and Switzerland) between the 1 October 2020 and 15 December 2020. All participating hospitals obtained ethical approval according to their country’s legislation.
Consecutive patients with severe COVID-19 infection (confirmed by PCR) who fulfilled the following criteria were included: age > 18 years, hospitalised in ICU or an intermediate care unit (IU), with high oxygen dependency (High Flow Nasal Cannula (HFNC) or PaO2/FiO2 < 300 or SpO2 < 94% with a non-rebreather mask and an O2 flow of at least at 10 L/min).
Exclusion criteria were as follows: Patient already using home HFNC for another reason, patient intubated by emergency services out of hospital or in the emergency department, use of CPAP or Bi-level non-invasive ventilation (NIV) for a reason another than acute respiratory failure due to COVID-19 infection, patient refusal of ventilatory support.
2.1. Procedure
In the four participating centres, all patients with severe COVID-19 infection and hypoxia were hospitalised in ICU or IU depending on bed availability and whether they were eligible or not for intubation. Details of the procedures in each centre are provided in the Supplementary file. The decision not to intubate was collegial and was based on age, comorbidities and bed availability in ICU. Depending on the patient’s respiratory status and equipment availability, each hospital used either HFNC (set at 50 L/min with FiO2 titrated for SpO2 > 92%) and/or CPAP (set between 8 and 12 cmH20 with FiO2 titrated for SpO2 > 92%). Respiratory support was primarily provided to treat acute respiratory failure due to hypoxemia, however if an increase in the partial pressure of carbon dioxide occurred, some patients were treated with Bi-level NIV (NIV). For patients with a Do Not Intubate (DNI) order, CPAP or Bi-level NIV was the ceiling treatment.
Due to the retrospective design of this study, the indications for intubation were not standardized: intubation was performed according to the judgement of the attending clinician. Nonetheless, indications for intubation in our ICU department include hypoxemia associated with marked respiratory failure, an inability to ensure airway protection, shock, and a reduced level of consciousness.
2.2. Main Reasons for Non-Intubation
The reasons for non-intubation were as follows: Patients older than 85 years, patients older than 80 years with a low level of autonomy and/or severe comorbidity (Chronic respiratory disease, chronic heart failure, etc.) and/or living with a mild frailty (Clinical Frailty scale ≥ 5), patients older than 80 years in the case of low ICU capacity (last ICU bed), patients with several comorbidities or living with a severe frailty (Clinical Frailty scale ≥ 7), and patients who refused orotracheal intubation.
2.3. Data Collection
Study personnel at each site collected data by manual chart review and used a standardized case report form to enter data into a secure online database. Data were collected using REDCap, a secure, HIPAA-compliant, web-based application. Potentials errors were all flagged in real time using the REDCap Data Quality module. After collection, all data were again manually reviewed, and values that appeared incongruent or out of range were manually validated by confirming the accuracy of the data with the collaborator who entered it.
Demographic characteristics, body mass index (BMI), comorbidities, date of COVID-19 diagnosis (positive PCR), date of hospital admission, biological examinations on admission to ICU/IU (including PaO2/FiO2 ratio, C-reactive protein, D-dimer and Fibrinogen) and quick-SOFA score on admission to ICU/IU were recorded.
We chose not to use the SOFA score because the patients in IU did not undergo daily blood samples. Therefore, to avoid a large number of missing data, we used the quick-SOFA score [22] which summarises the severity of the patient’s condition using three items: (respiratory rate > 22 c/min; Glasgow Coma Scale score < 15/15; systolic blood pressure < 100 mmHg). This assessment has been evaluated for use in patients with COVID-19 [23]. When it was not possible to collect FiO2 data for a patient, we used the conversion table described by the COVID-ICU group of the REVA network [2].
Finally, use and duration of HFNC, CPAP, Bi-level NIV, invasive mechanical ventilation, medication (antibiotherapy, corticosteroids, hydroxychloroquine and tocilizumab) and clinical outcomes (mortality, ICU/IU length of stay and discharge destination) were collected. We chose not to collect data for interventions after intubation (neuromuscular blockers, prone position, ECMO, and weaning strategy) because we considered that the indications were not different from usual practice. Patients were followed up until death or discharge from ICU or IU.
2.4. Target Trial Framework
We sought to emulate a hypothetical target trial by classifying patients into two groups: Group 1 was composed of patients with severe COVID-19 with a DNI order who were treated with HFNC and/or CPAP as a ceiling treatment, and Group 2 was composed of patients who remained eligible for invasive mechanical ventilation.
2.5. Inverse Probability of Treatment Weighting
Because patients were categorized into one of these two groups using medical criteria, we set up a propensity score for the probability of belonging to Group 1 and an inverse probability of treatment weighting to remove confounding by indication. For the propensity score, a logistic regression model was fitted with (i) the variables that informed the decision to classify patients into Group 1 or Group 2 (age, age-squared and severe comorbidities) or (ii) the variables that are potentially associated with mortality (PaO2/FiO2, BMI, BMI-squared, administration of corticosteroids, quick-SOFA score, hypertension, time from diagnosis to admission, HFNC at admission and CPAP (or bilevel-NIV) at admission). The choice of variables to include was made a priori to the data analysis as they were thought to be potentially associated with a clinician’s decision to classify patients in Group 1 or 2 and with survival.
The overlap of the distributions of the variables between Group 1 and Group 2 was checked. Because no patient aged 85 or older was allocated to the Group 2 which was eligible for intubation, we excluded patients aged 85 or older from the primary analysis.
The model’s predicted probabilities for classification into the Group 1 were used to calculate stabilized inverse probability weights [24], which were then used to weight each individual’s contribution to the logistic regression for death. To account for the inverse probability weighting, we used a robust variance estimator.
2.6. Statistical Analysis
For missing data, we imputed ten data sets with multiple imputations and combined the results using Rubin’s rule [25]. Descriptive statistics were performed on non-imputed data, as recommended.
We evaluated standardized differences across each measured covariate before and after applying the weighting. The balance of prognostic variables pre- and post-inverse probability of treatment weighting was evaluated with Cohen’s d for continuous variables and with odds ratios for binary variables. For continuous outcomes, we performed unweighted and weighted linear regressions, for binary outcomes we used logistic regression, and we calculated the Cohen’s d on unweighted (i.e., before inverse probability of treatment weighting) and weighted results (i.e., after inverse probability of treatment weighting).
We chose to report the overall mortality rate rather than time to death because invasive mechanical ventilation could increase the duration of survival, even in patients with a very low probability of surviving.
3. Results
During the period studied, 517 patients were admitted to ICU or IU due to severe COVID-19 infection. Of these, 86 were sufficiently oxygenated with a low O2 flow rate, and a further 31 did not fulfil the inclusion criteria (See Figure 1). A total of 400 patients was included in the analysis.
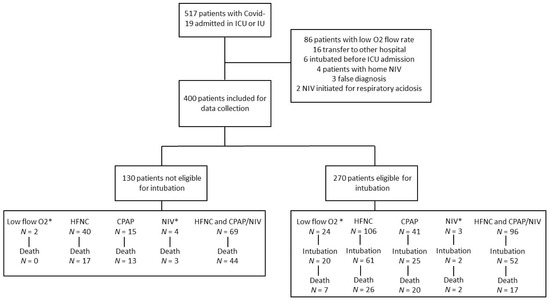
Figure 1.
Flow chart. * Low flow O2 is defined by non-rebreather mask with O2 flow at least at 10 L/min. NIV: Bi-level NIV.
Table 1 describes the patient characteristics and characteristics by centre are shown in Supplementary file (Table S1). Briefly, 130 (32.5%) were issued with a DNI order (Group 1) and 270 patients were classified as eligible for intubation and invasive mechanical ventilation (67.5%) (Group 2). In Group 1, 109 (84%) patients were treated with HFNC and 74 (57%) with CPAP therapy. In Group 2, 202 (75%) received HFNC and 118 (44%) received CPAP therapy. Finally, 161 (60%) had to be intubated. The median time from admission to intubation was 3 (2–6.5) days. Patients in Group 2 were younger (66 (58–73) vs. 79.5 (72–84) years; p < 0.0001) and had fewer comorbidities. There were no significant between group differences for the Quick-SOFA score, PaO2/FiO2 and C-reactive protein at admission. The durations of HFNC and CPAP therapy were significantly longer for patients in Group 1 (respectively., 6 (4–9) vs. 3 (2–5) days; p < 0.0001 and 6 (3–9) vs. 3 (2–7) days; p < 0.001).

Table 1.
Population characteristics.
In Group 2, 72 (27%) patients died compared to 77 (59%) in Group 1: risk ratio 0.49 (0.36–0.67). Once confounding factors were taken into account, the adjusted risk ratio for death among patients eligible for intubation was 0.81 (95% CI 0.46 to 1.42) (Figure 2).
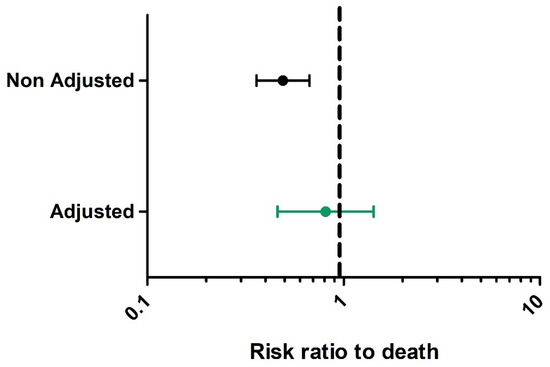
Figure 2.
Black caterpillar plot represents overall risk ratio to death before inverse probability of treatment weighting. Green caterpillar plot represents risk ratio to death after inverse probability of treatment weighting.
Figure 3 shows the characteristics of the patients in both groups, before and after applying inverse probability of treatment weighting. The effect sizes for the differences between the two groups in the important prognostic factors were strongly reduced when the inverse probability of treatment weighting was applied. However, there was still a small difference for age: patients in Group 1 were older.
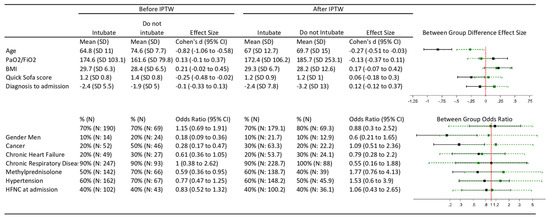
Figure 3.
Characteristics of the patients before and after applying inverse probability of treatment weighting. Black Caterpillar plot represents risk ratio to death before inverse probability of treatment weighting. Green caterpillar plot represents risk ratio to death after inverse probability of treatment weighting. BMI: Body Mass Index; HFNC: High Flow Nasal Cannula; IPTW: Inverse Probability of Treatment Weighting; n: Number of patients; SD: Standardized Deviation.
Factors associated with mortality are presented in Supplementary file (Figure S1). Risk ratio to death were higher for Older age, Chronic Heart Failure, Cancer and Neurological pathology comorbidities (respectively, 1.05 (1.03 to 1.06); 1.59 (1.14 to 2.21); 1.68 (1.09 to 2.6) and 2.34 (1.5 to 3.64)). Use of HFNC at admission and PaO2/FiO2 were associated with lower mortality (respectively, 0.62 (0.45 to 0.86) and 0.90 (0.82 to 0.99)).
The median length of stay in ICU or IU was similar between groups for survivors (19 days (13–23.5) vs. 18 days (10–31); p = 0.76)) (Figure 4).
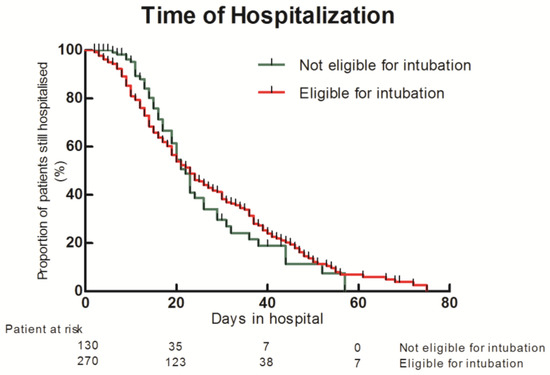
Figure 4.
Kaplan–Meier of hospital length of stay between patient eligible to intubation and patients not eligible to intubation.
In Group 1, 16% of survivors were discharged home compared with 44% in Group 2. The proportion of patients discharged to a rehabilitation centre was similar between the two groups (respectively, 20% and 21%) (See Supplementary file: Figure S2).
4. Discussion
This is the first European-wide study to compare outcomes in patients with severe COVID-19 infection and a do not intubate order treated with non-invasive respiratory support to those patients eligible for treatment with invasive mechanical ventilation. Since a randomised, controlled trial would be unethical to conduct in such a situation, we simulated an intention to treat analysis in which patients received treatment according to the severity of their condition (and its progression), with adjustment by the covariables associated with mortality. The results suggest that (1) there was no significant difference in adjusted mortality rate between the patients with a DNI and those eligible for intubation, and (2) the duration of hospitalization was similar between survivors with a DNI order and those eligible for intubation.
The decision not to intubate patients with severe COVID-19 infection is not straightforward. It depends on the number of available beds and patient-related factors [8,9]. Until now, the high mortality rates among patients with a DNI order who were managed using non-invasive ventilatory supports, created uncertainty as to the benefits of such supports [15,21]: the results of this study provide some clarity regarding this issue. Although the unadjusted rate of mortality was higher for the patients with a DNI order, adjustment for the different mortality-related variables showed that the mortality rate was not statistically different from that of the patients eligible for intubation. These results suggest that for those patients with several comorbidities, invasive mechanical ventilation would not lead to better outcomes.
The gold-standard treatment for respiratory failure in those who are eligible remains invasive mechanical ventilation. This treatment increases the short-term probability of survival and intubation provides a bridge for other rescue treatments, such as protective ventilation with alveolar recruitment, prone position [26] or extra corporeal membrane oxygenation [27]. Nevertheless, the efficacy of mechanical ventilation in patients with COVID-19 and severe ARDS is reduced [2], and long-term mortality is increased [28]. Furthermore, our results do not suggest a large benefit from invasive ventilation for patients with a DNI order. Indeed, a recent meta-analysis reported that the case fatality rate in patients with COVID-19 over the age of 60 years who are intubated is more than 70%, and increases exponentially with age, up to 84.4% in those above the age of 80 years [7]. Furthermore, in fragile and older patients, non-invasive respiratory support has the advantage of not requiring sedation and immobility. As such, transfers to the chair and rehabilitation can begin early, maintaining patient autonomy and reducing the physical and psychological consequences of mechanical ventilation [29,30]. Unfortunately, we were unable to report functional status at discharge from ICU/IU or hospital discharge, however the length of stay in ICU/IU was similar between groups, and the same proportion (20%) of patients were discharged to a rehabilitation centre.
A large proportion (78%) of the patients in this multicentre cohort were treated with HFNC at ICU/IU admission. The use of HFNC as a first line treatment for COVID-19-induced respiratory failure was proposed by Demoule et al. and appears to decrease the need for intubation at day 28 [10]. Despite this, HFNC failed to sufficiently reverse hypoxia in 56% of the patients in that study who were subsequently treated with invasive mechanical ventilation. We propose that in patients with a DNI order, CPAP could be a valid rescue option. Compared to HFNC, CPAP has the advantage of providing a high FiO2 at higher pressures, thus increasing alveolar oxygenation and decreasing respiratory muscle work [31]. However, these devices have also been reported to be potentially dangerous due to the generation of high tidal volumes and excessive transpulmonary pressure swings which can induce volutrauma [32] and the risk of delayed intubation [33]. The results of the present study showed that the rate of CPAP use was lower in patients eligible for intubation, probably due to the rapid use of invasive ventilation after HFNC failure. One of the major problems with CPAP is that it cannot be used continuously for several days because, even when optimally applied, the interface can be uncomfortable. In the present cohort, all types of interfaces were used (helmet, face mask and nasal pillows) depending on the habits of each department, equipment availability and patient toleration.
This study has several limitations. Firstly, it was not a randomized control trial and, even after adjustment, there was still a small difference in age between groups. However, our results are based on real life practices in ICUs and IUs where personalized, not protocolized, respiratory support is provided to patients. Secondly, the sample size was limited by the inclusion of only patients from the second wave of the pandemic in Europe (winter 2020). However, the advantage of this is that, by this time patients were treated with the highest level of evidence-based knowledge of the disease (e.g., 93% were treated with corticosteroids). The health-care teams were also experienced in the management of the disease, thus similar treatment protocols were applied across the four participating hospitals. Thirdly, published studies on that topic focused on CPAP or high flow nasal cannula alone, whereas both supports are very frequently combined in our centres, which is thought to provide better outcomes [34], and the superiority of those devices on one another has not yet been well established.
5. Conclusions
This comparison of the outcomes of treatment with non-invasive respiratory support in patient’s ineligible and eligible for intubation found that the use of non-invasive respiratory support is a good compromise for patients with severe COVID-19 and a do not intubate order. Future research is required to further define the modalities of application of non-invasive ventilatory supports.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/jcm10132783/s1, Supplementary file of Role of non-invasive respiratory supports in COVID-19 acute respiratory failure patients with do not intubate order, Table S1. Population characteristics by centre, Figure S1. Risk ratio of mortality according to unadjusted variable, Figure S2. Orientation after Hospital discharge.
Author Contributions
Conceptualization, C.M., A.G., F.B., J.D., N.C., R.H., O.C.; Methodology, C.M., M.Z., R.H., O.C.; Software, M.Z., R.H.; Validation, All authors; Formal Analysis, M.Z., R.H.; Investigation, All authors; Resources, All authors; Data Curation, All authors; Writing—Original Draft Preparation, C.M., A.G., R.H., O.C.; Writing—Review and Editing, All authors; Visualization, All authors; Supervision, C.M., O.C.; Project Administration, C.M., A.G., F.B., J.D., N.C., O.C.; Funding Acquisition, A.G. All authors have read and agreed to the published version of the manuscript.
Funding
Alexis Gillet received grants by Fonds Erasme pour la Recherche medical.
Institutional Review Board Statement
All participating hospitals obtained ethical approval according to their country’s legislation.
Informed Consent Statement
Institutional Review Boards waived the need to obtain consent to participate due to the retrospective design.
Data Availability Statement
Clément Medrinal had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Data can be obtained from the corresponding author: Clément Medrinal; medrinal.clement.mk@gmail.com.
Acknowledgments
The Authors thanks Johanna Robertson, medical translator.
Conflicts of Interest
No conflicts of interest in regards with the subject of the manuscript.
References
- Grasselli, G.; Zangrillo, A.; Zanella, A.; Antonelli, M.; Cabrini, L.; Castelli, A.; Cereda, D.; Coluccello, A.; Foti, G.; Fumagalli, R.; et al. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA 2020, 323, 1574. [Google Scholar] [CrossRef] [Green Version]
- COVID-ICU Group on Behalf of the REVA Network and the COVID-ICU Investigators. Clinical Characteristics and Day-90 Outcomes of 4244 Critically Ill Adults with COVID-19: A Prospective Cohort Study. Intensive Care Med. 2021, 47, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, Clinical Course, and Outcomes of Critically Ill Adults with COVID-19 in New York City: A Prospective Cohort Study. Lancet 2020, 395, 1763–1770. [Google Scholar] [CrossRef]
- Alhazzani, W.; Evans, L.; Alshamsi, F.; Møller, M.H.; Ostermann, M.; Prescott, H.C.; Arabi, Y.M.; Loeb, M.; Ng Gong, M.; Fan, E.; et al. Surviving Sepsis Campaign Guidelines on the Management of Adults With Coronavirus Disease 2019 (COVID-19) in the ICU: First Update. Crit. Care Med. 2021, 49, e219–e234. [Google Scholar] [CrossRef] [PubMed]
- COVID-19 Consortium; Van Aerde, N.; Van den Berghe, G.; Wilmer, A.; Gosselink, R.; Hermans, G. Intensive Care Unit Acquired Muscle Weakness in COVID-19 Patients. Intensive Care Med. 2020, 46, 2083–2085. [Google Scholar] [CrossRef] [PubMed]
- Medrinal, C.; Prieur, G.; Bonnevie, T.; Gravier, F.-E.; Mayard, D.; Desmalles, E.; Smondack, P.; Lamia, B.; Combret, Y.; Fossat, G. Muscle Weakness, Functional Capacities and Recovery for COVID-19 ICU Survivors. BMC Anesthesiol. 2021, 21, 64. [Google Scholar] [CrossRef] [PubMed]
- Lim, Z.J.; Subramaniam, A.; Ponnapa Reddy, M.; Blecher, G.; Kadam, U.; Afroz, A.; Billah, B.; Ashwin, S.; Kubicki, M.; Bilotta, F.; et al. Case Fatality Rates for Patients with COVID-19 Requiring Invasive Mechanical Ventilation. A Meta-Analysis. Am. J. Respir. Crit. Care Med. 2021, 203, 54–66. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.-L.; Creteur, J. Ethical Aspects of the COVID-19 Crisis: How to Deal with an Overwhelming Shortage of Acute Beds. Eur. Heart J. Acute Cardiovasc. Care 2020, 9, 248–252. [Google Scholar] [CrossRef]
- Truog, R.D.; Mitchell, C.; Daley, G.Q. The Toughest Triage—Allocating Ventilators in a Pandemic. N. Engl. J. Med. 2020, 382, 1973–1975. [Google Scholar] [CrossRef]
- Demoule, A.; Vieillard Baron, A.; Darmon, M.; Beurton, A.; Géri, G.; Voiriot, G.; Dupont, T.; Zafrani, L.; Girodias, L.; Labbé, V.; et al. High-Flow Nasal Cannula in Critically III Patients with Severe COVID-19. Am. J. Respir. Crit. Care Med. 2020, 202, 1039–1042. [Google Scholar] [CrossRef]
- Oranger, M.; Gonzalez-Bermejo, J.; Dacosta-Noble, P.; Llontop, C.; Guerder, A.; Trosini-Desert, V.; Faure, M.; Raux, M.; Decavele, M.; Demoule, A.; et al. Continuous Positive Airway Pressure to Avoid Intubation in SARS-CoV-2 Pneumonia: A Two-Period Retrospective Case-Control Study. Eur. Respir. J. 2020, 56, 2001692. [Google Scholar] [CrossRef]
- Nightingale, R.; Nwosu, N.; Kutubudin, F.; Fletcher, T.; Lewis, J.; Frost, F.; Haigh, K.; Robinson, R.; Kumar, A.; Jones, G.; et al. Is Continuous Positive Airway Pressure (CPAP) a New Standard of Care for Type 1 Respiratory Failure in COVID-19 Patients? A Retrospective Observational Study of a Dedicated COVID-19 CPAP Service. BMJ Open Respir. Res. 2020, 7, e000639. [Google Scholar] [CrossRef]
- Coppadoro, A.; Benini, A.; Fruscio, R.; Verga, L.; Mazzola, P.; Bellelli, G.; Carbone, M.; Mulinacci, G.; Soria, A.; Noè, B.; et al. Helmet CPAP to Treat Hypoxic Pneumonia Outside the ICU: An Observational Study during the COVID-19 Outbreak. Crit. Care 2021, 25, 80. [Google Scholar] [CrossRef]
- Franco, C.; Facciolongo, N.; Tonelli, R.; Dongilli, R.; Vianello, A.; Pisani, L.; Scala, R.; Malerba, M.; Carlucci, A.; Negri, E.A.; et al. Feasibility and Clinical Impact of Out-of-ICU Noninvasive Respiratory Support in Patients with COVID-19-Related Pneumonia. Eur. Respir. J. 2020, 56, 2002130. [Google Scholar] [CrossRef] [PubMed]
- Bellani, G.; Grasselli, G.; Cecconi, M.; Antolini, L.; Borelli, M.; De Giacomi, F.; Bosio, G.; Latronico, N.; Filippini, M.; Gemma, M.; et al. Noninvasive Ventilatory Support of COVID-19 Patients Outside the Intensive Care Units (WARd-COVID). Ann. Am. Thorac. Soc. 2021, 18, 1020–1026. [Google Scholar] [CrossRef]
- Radovanovic, D.; Rizzi, M.; Pini, S.; Saad, M.; Chiumello, D.A.; Santus, P. Helmet CPAP to Treat Acute Hypoxemic Respiratory Failure in Patients with COVID-19: A Management Strategy Proposal. J. Clin. Med. 2020, 9, 1191. [Google Scholar] [CrossRef]
- Pfeifer, M.; Ewig, S.; Voshaar, T.; Randerath, W.J.; Bauer, T.; Geiseler, J.; Dellweg, D.; Westhoff, M.; Windisch, W.; Schönhofer, B.; et al. Position Paper for the State-of-the-Art Application of Respiratory Support in Patients with COVID-19. Respiration 2020, 99, 521–542. [Google Scholar] [CrossRef]
- Aliberti, S.; Radovanovic, D.; Billi, F.; Sotgiu, G.; Costanzo, M.; Pilocane, T.; Saderi, L.; Gramegna, A.; Rovellini, A.; Perotto, L.; et al. Helmet CPAP Treatment in Patients with COVID-19 Pneumonia: A Multicentre Cohort Study. Eur. Respir. J. 2020, 56, 2001935. [Google Scholar] [CrossRef]
- Alviset, S.; Riller, Q.; Aboab, J.; Dilworth, K.; Billy, P.-A.; Lombardi, Y.; Azzi, M.; Ferreira Vargas, L.; Laine, L.; Lermuzeaux, M.; et al. Continuous Positive Airway Pressure (CPAP) Face-Mask Ventilation Is an Easy and Cheap Option to Manage a Massive Influx of Patients Presenting Acute Respiratory Failure during the SARS-CoV-2 Outbreak: A Retrospective Cohort Study. PLoS ONE 2020, 15, e0240645. [Google Scholar] [CrossRef] [PubMed]
- On Behalf of the UCL Critical Care COVID-19 Research Group; Arina, P.; Baso, B.; Moro, V.; Patel, H.; Ambler, G. Discriminating between CPAP Success and Failure in COVID-19 Patients with Severe Respiratory Failure. Intensive Care Med. 2021, 47, 237–239. [Google Scholar] [CrossRef]
- Vaschetto, R.; Barone-Adesi, F.; Racca, F.; Pissaia, C.; Maestrone, C.; Colombo, D.; Olivieri, C.; De Vita, N.; Santangelo, E.; Scotti, L.; et al. Outcomes of COVID-19 Patients Treated with Continuous Positive Airway Pressure Outside the Intensive Care Unit. ERJ Open Res. 2021, 7, 00541–02020. [Google Scholar] [CrossRef] [PubMed]
- Serafim, R.; Gomes, J.A.; Salluh, J.; Póvoa, P. A Comparison of the Quick-SOFA and Systemic Inflammatory Response Syndrome Criteria for the Diagnosis of Sepsis and Prediction of Mortality. Chest 2018, 153, 646–655. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Yao, N.; Qiu, Y.; He, C. Predictive Performance of SOFA and QSOFA for In-Hospital Mortality in Severe Novel Coronavirus Disease. Am. J. Emerg. Med. 2020, 38, 2074–2080. [Google Scholar] [CrossRef] [PubMed]
- Cole, S.R.; Hernán, M.A. Constructing Inverse Probability Weights for Marginal Structural Models. Am. J. Epidemiol. 2008, 168, 656–664. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation for Nonresponse in Surveys; Wiley Series in Probability and Statistics; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 1987; pp. i–xxix. ISBN 978-0-470-31669-6. [Google Scholar]
- Guérin, C.; Reignier, J.; Richard, J.-C.; Beuret, P.; Gacouin, A.; Boulain, T.; Mercier, E.; Badet, M.; Mercat, A.; Baudin, O.; et al. Prone Positioning in Severe Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2013, 368, 2159–2168. [Google Scholar] [CrossRef]
- Combes, A.; Hajage, D.; Capellier, G.; Demoule, A.; Lavoué, S.; Guervilly, C.; Da Silva, D.; Zafrani, L.; Tirot, P.; Veber, B.; et al. Extracorporeal Membrane Oxygenation for Severe Acute Respiratory Distress Syndrome. N. Engl. J. Med. 2018, 378, 1965–1975. [Google Scholar] [CrossRef]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk Factors Associated with Mortality among Patients with COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345. [Google Scholar] [CrossRef]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early Physical and Occupational Therapy in Mechanically Ventilated, Critically Ill Patients: A Randomised Controlled Trial. Lancet (Lond. Engl.) 2009, 373, 1874–1882. [Google Scholar] [CrossRef]
- Hopkins, R.O.; Suchyta, M.R.; Farrer, T.J.; Needham, D. Improving Post–Intensive Care Unit Neuropsychiatric Outcomes: Understanding Cognitive Effects of Physical Activity. Am. J. Respir. Crit. Care Med. 2012, 186, 1220–1228. [Google Scholar] [CrossRef]
- Grieco, D.L.; Menga, L.S.; Raggi, V.; Bongiovanni, F.; Anzellotti, G.M.; Tanzarella, E.S.; Bocci, M.G.; Mercurio, G.; Dell’Anna, A.M.; Eleuteri, D.; et al. Physiological Comparison of High-Flow Nasal Cannula and Helmet Noninvasive Ventilation in Acute Hypoxemic Respiratory Failure. Am. J. Respir. Crit. Care Med. 2020, 201, 303–312. [Google Scholar] [CrossRef]
- Carteaux, G.; Millán-Guilarte, T.; De Prost, N.; Razazi, K.; Abid, S.; Thille, A.W.; Schortgen, F.; Brochard, L.; Brun-Buisson, C.; Mekontso Dessap, A. Failure of Noninvasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume. Crit. Care Med. 2016, 44, 282–290. [Google Scholar] [CrossRef] [PubMed]
- Esteban, A.; Frutos-Vivar, F.; Muriel, A.; Ferguson, N.D.; Peñuelas, O.; Abraira, V.; Raymondos, K.; Rios, F.; Nin, N.; Apezteguía, C.; et al. Evolution of Mortality over Time in Patients Receiving Mechanical Ventilation. Am. J. Respir. Crit. Care Med. 2013, 188, 220–230. [Google Scholar] [CrossRef] [PubMed]
- Thille, A.W.; Muller, G.; Gacouin, A.; Coudroy, R.; Decavèle, M.; Sonneville, R.; Beloncle, F.; Girault, C.; Dangers, L.; Lautrette, A.; et al. Effect of Postextubation High-Flow Nasal Oxygen With Noninvasive Ventilation vs High-Flow Nasal Oxygen Alone on Reintubation Among Patients at High Risk of Extubation Failure: A Randomized Clinical Trial. JAMA 2019, 322, 1465–1475. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).