The Effectiveness of Different Concepts of Bracing in Adolescent Idiopathic Scoliosis (AIS): A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
- What is the most effective brace concept?
- What is the most effective brace type (Boston brace, Providence brace, etc.)?
- What is the effect of skeletal maturity on the effectiveness of different concepts of brace treatment?
2. Materials and Methods
2.1. Protocol
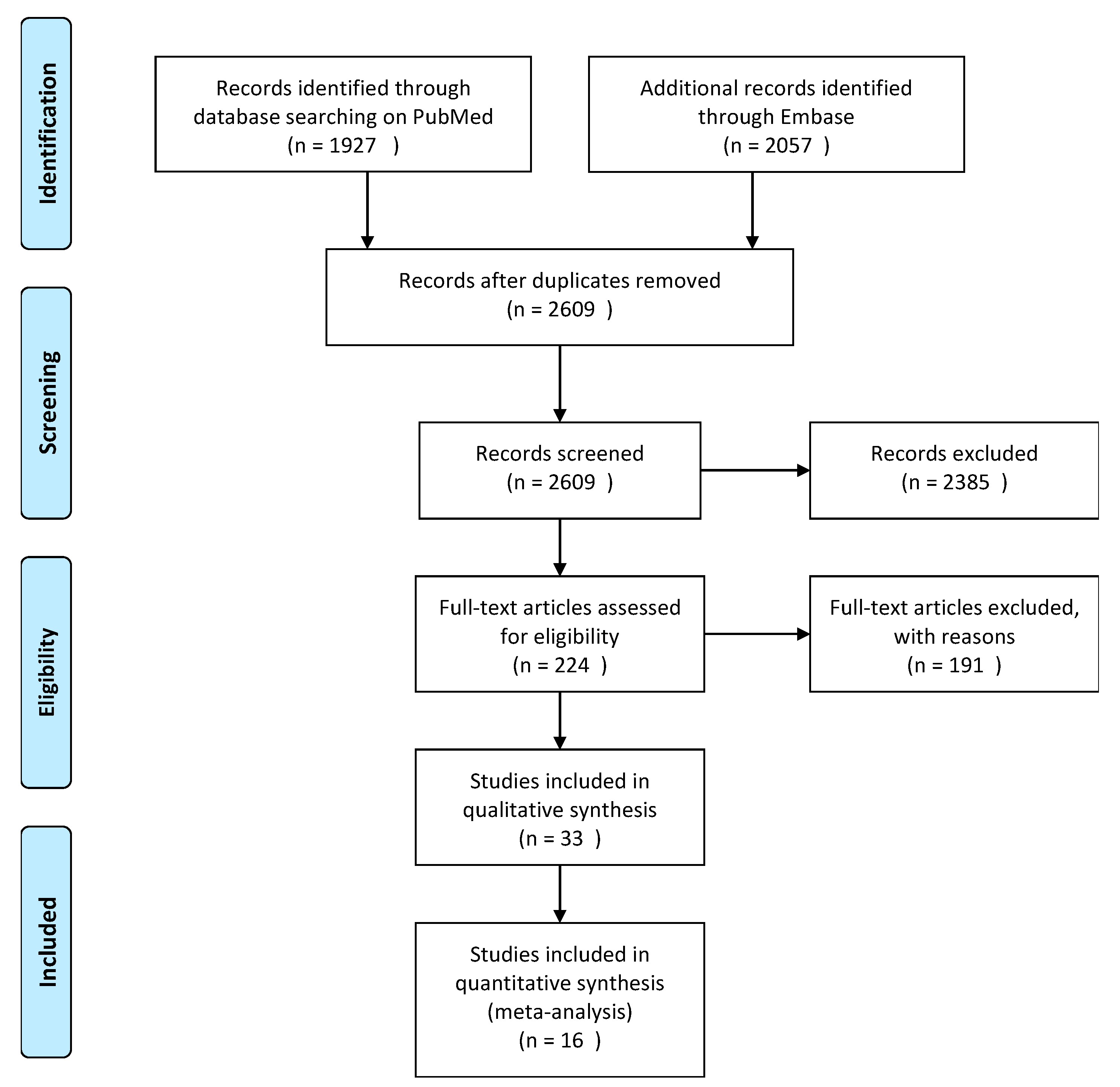
2.2. Search Methods and Study Selections
2.3. Appraisal
2.4. Synthesis
3. Results
3.1. Search
3.2. Study Characteristic
- Rigid full-time braces (15 studies): 30% 20–40°, 30% 25–40°, 8% 25–45°, 8% ≥ 40°, 8% > 25°, 8% 0–45°.
- Night-time braces (8 studies): 63% 25–40°, 13% 20–45°, 13% 25–49°, 13% < 25°.
- Soft full-time braces (2 studies): 50% 25–40°, 50% 15–40°.
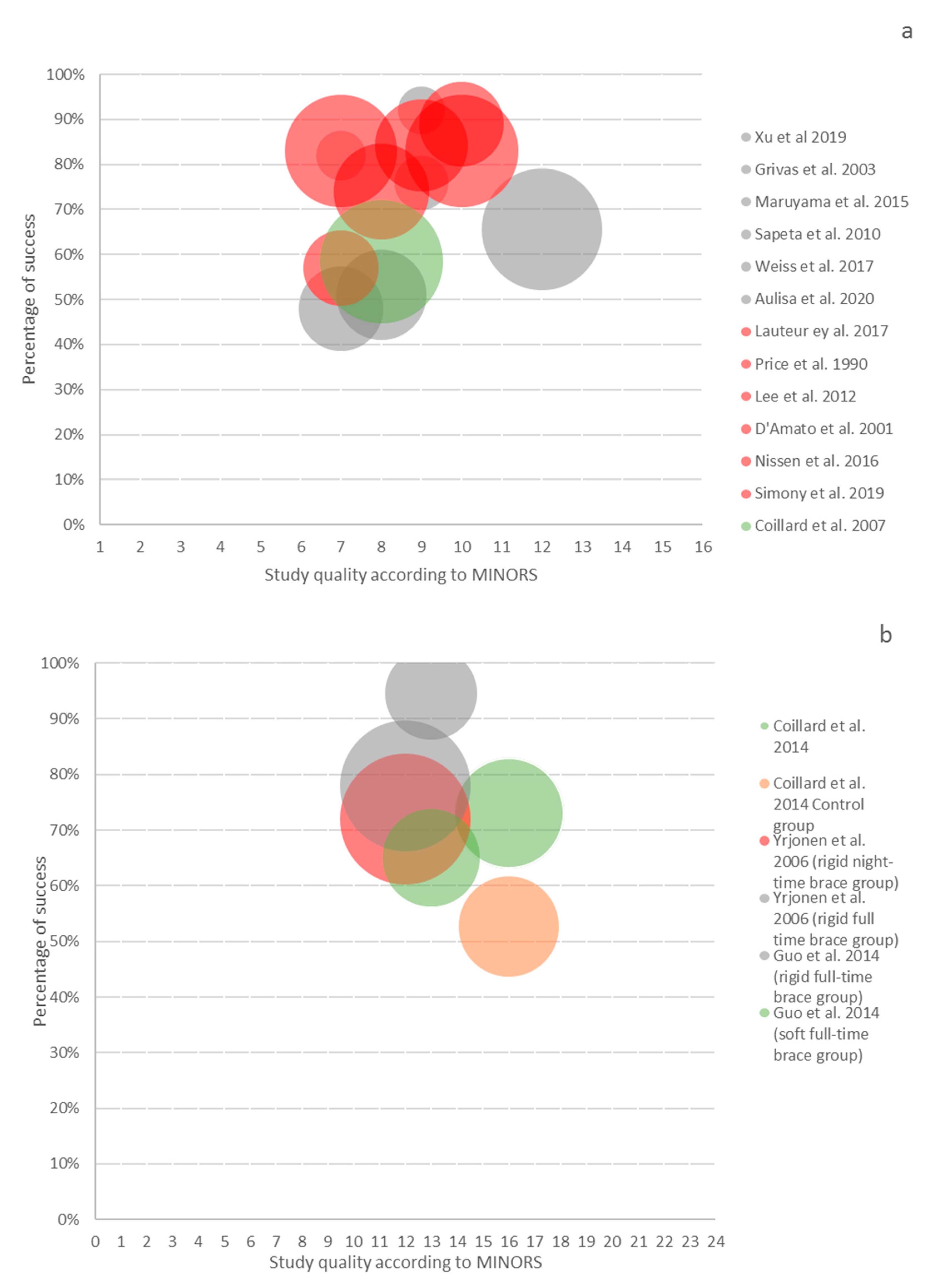
3.3. Study Quality
3.4. Qualitative Analysis
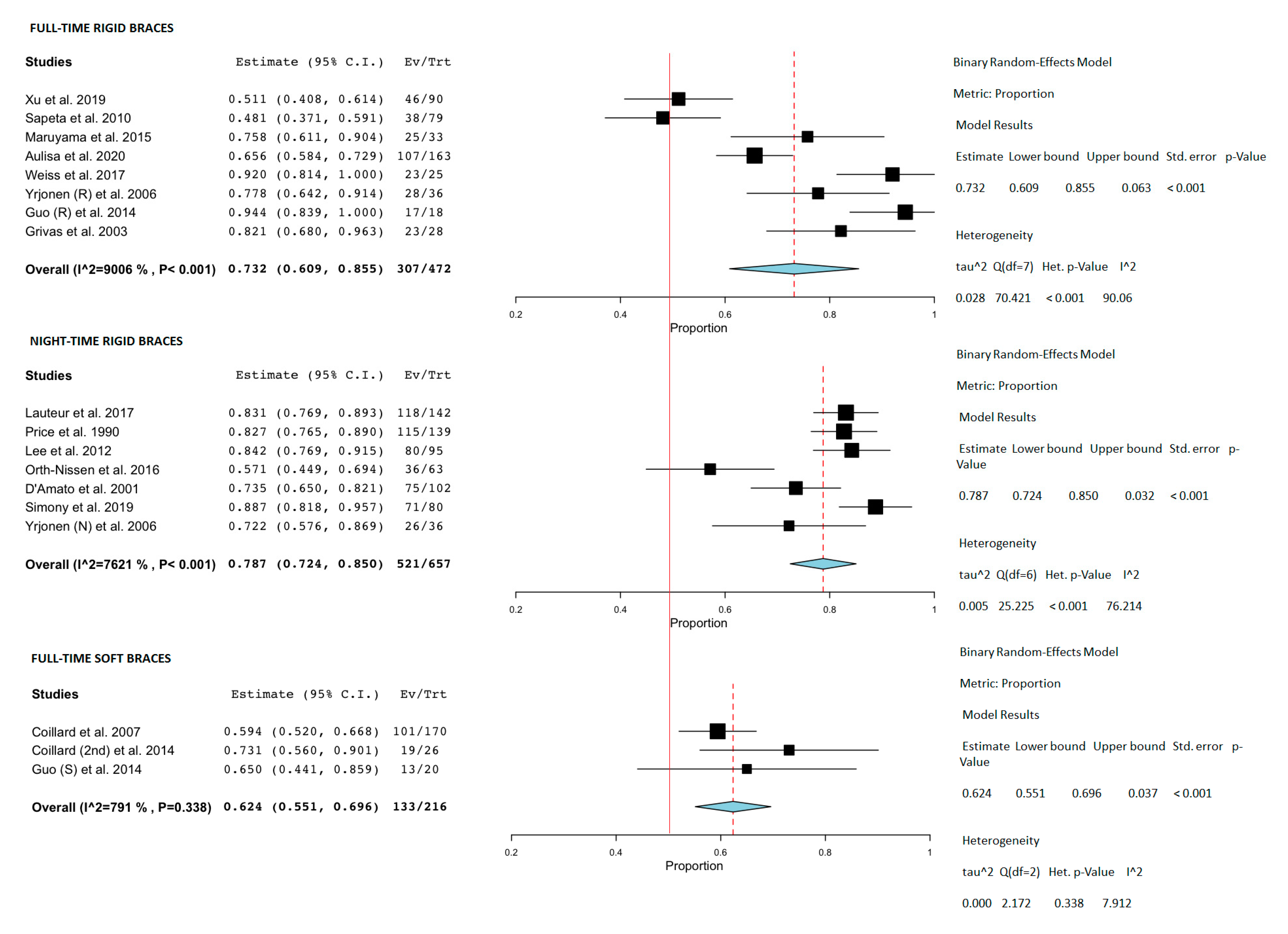
- Full-time, rigid braces
- Part-time, rigid braces
- Night-time, rigid braces
- Full-time soft braces
- Comparative studies
3.5. Meta-Analysis
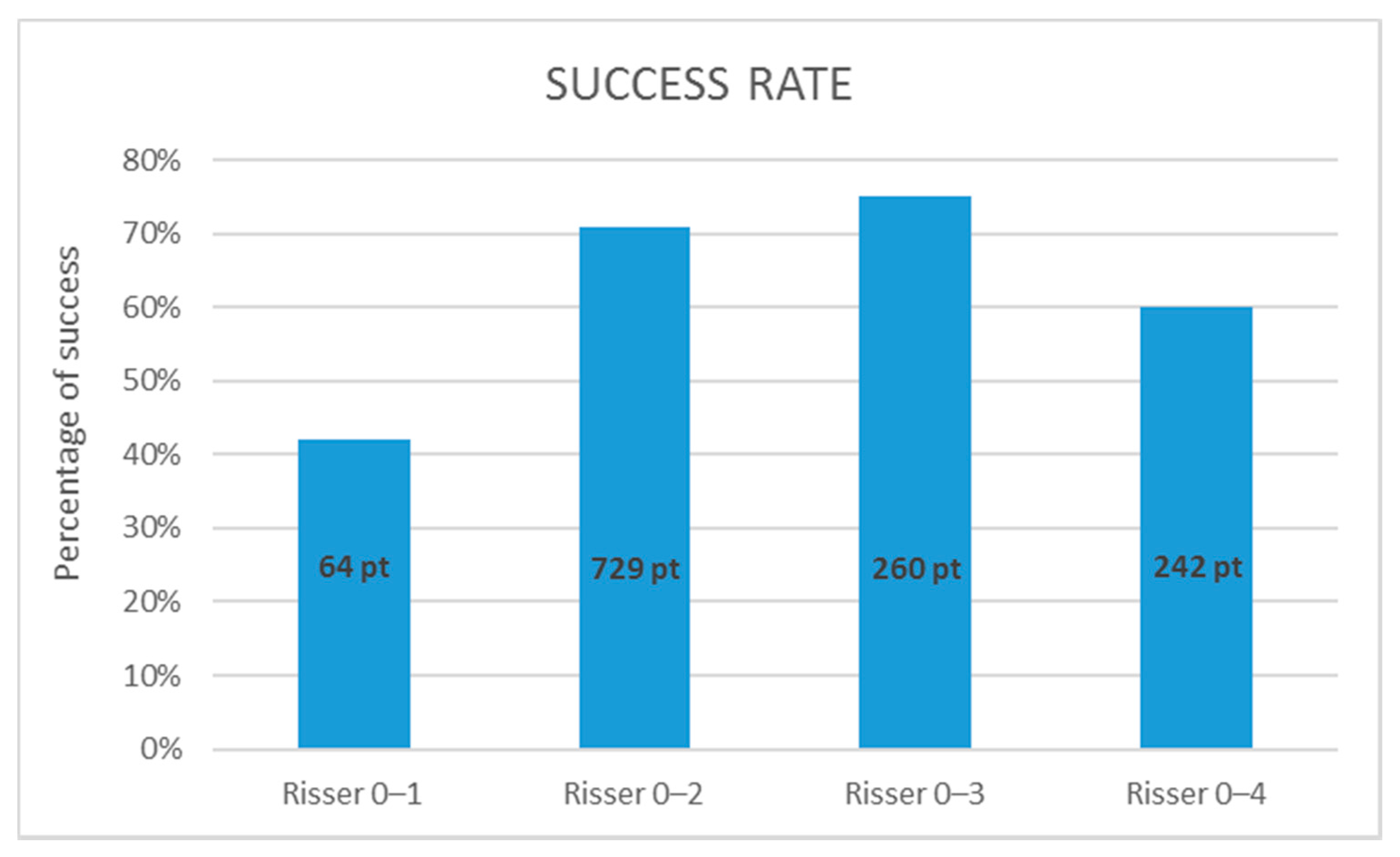
3.6. The Role of Skeletal Maturity
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Konieczny, M.R.; Senyurt, H.; Krauspe, R. Epidemiology of adolescent idiopathic scoliosis. J. Child. Orthop. 2013, 7, 3–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lonstein, J.E. Scoliosis: Surgical versus nonsurgical treatment. Clin. Orthop. Relat. Res. 2006, 87, 248–259. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, S.L.; Dolan, L.A.; Cheng, J.C.; Danielsson, A.; Morcuende, J.A. Adolescent idiopathic scoliosis. Lancet 2008, 371, 1527–1537. [Google Scholar] [CrossRef] [Green Version]
- Yrjönen, T.; Ylikoski, M.; Schlenzka, D.; Kinnunen, R.; Poussa, M. Effectiveness of the Providence nighttime bracing in adolescent idiopathic scoliosis: A comparative study of 36 female patients. Eur. Spine J. 2006, 15, 1139–1143. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- D’Amato, C.R.; Griggs, S.; McCoy, B. Nighttime bracing with the Providence brace in adolescent girls with idiopathic scoliosis. Spine 2001, 26, 2006–2012. [Google Scholar] [CrossRef]
- Weinstein, S.L.; Dolan, L.; Wright, J.G.; Dobbs, M.B. Effect of bracing adolescent idiopathic scoliosis. New Engl. J. Med. 2014, 369, 1512–1521. [Google Scholar] [CrossRef] [Green Version]
- Lenssinck, M.L.B.; Frijlink, A.C.; Berger, M.Y.; Bierma-Zeinstra, S.M.; Verkerk, K.; Verhagen, A.P. Effect of bracing and other conservative Interventions in the Treatment of Idiopathic Scoliosis in Adolescents: A Systematic Review of clinical trials. Phys. Ther. 2005, 85, 1329–1339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; De Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 1–48. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; Debeer, H.; et al. GRADE guidelines: 1. Introduction – GRADE evidence profiles and summary of findings tables. Washington (DC): National Academies P. BMJ 2011, 16, 1–13. [Google Scholar] [CrossRef]
- McKee, M.; Britton, A.; Black, N.; McPherson, K.; Sanderson, C.; Bain, C. Methods in health services research: Interpreting the evidence: Choosing between randomised and non-randomised studies. Br. Med. J. 1999, 319, 312–315. [Google Scholar] [CrossRef] [PubMed]
- Houwert, R.; Verhofstad, M.; Hietbrink, F.; Kruyt, M. De conventionele RCT voor trauma- en orthopedisch chirurgen: Geen heilige graal. Ned. Tijdschr. Voor Traumachirurgie 2016, 24, 2–5. [Google Scholar] [CrossRef] [Green Version]
- Abraham, N.S.; Byrne, C.J.; Young, J.M.; Solomon, M.J. Meta-analysis of well-designed nonrandomized comparative studies of surgical procedures is as good as randomized controlled trials. J. Clin. Epidemiol. 2010, 63, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, W.C.; Kruyt, M.C.; Verbout, A.J.; Oner, F.C. Spine surgery research: On and beyond current strategies. Spine J. 2012, 12, 706–713. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, W.C.; Kruyt, M.C.; Moojen, W.A.; Verbout, A.J.; Öner, F. C No evidence for intervention-dependent influence of methodological features on treatment effect. J. Clin. Epidemiol. 2013, 66, 1347–1355.e3. [Google Scholar] [CrossRef] [PubMed]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (Minors): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.; Jennifer, T. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, 50931. [Google Scholar] [CrossRef] [PubMed]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negrini, S.; Minozzi, S.; Bettany-Saltikov, J.; Chockalingam, N.; Grivas, T.B.; Kotwicki, T.; Maruyama, T.; Romano, M.; Zaina, F. Braces for idiopathic scoliosis in adolescents (Review) summary of findings for the main comparison. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [Green Version]
- Wallace, B.C.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the Gap between Methodologists and End-Users: R as a Computational Back-End. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef] [Green Version]
- Picault, C.; Demauroy, J.C.; Mouilleseaux, B.; Diana, G. Natural history of idiopathic scoliosis in girls and boys. Spine 1986, 11, 777–778. [Google Scholar] [CrossRef]
- Nachemson, A.L.; Peterson, L. E Effectiveness of tretment with a brace in girls who have adolescent idiopathic scoliosis. J. Bone Joint Surg. Am. 1995, 77, 815–822. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Yang, X.; Wang, Y.; Wu, Z.; Xia, C.; Qiu, Y.; Zhu, Z. Brace Treatment in Adolescent Idiopathic Scoliosis Patients with Curve Between 40° and 45°: Effectiveness and Related Factors. World Neurosurg. 2019, 126, e901–e906. [Google Scholar] [CrossRef]
- Yrjönen, T.; Ylikoski, M.; Schlenzka, D.; Poussa, M. Results of brace treatment of adolescent idiopathic scoliosis in boys compared with girls: A retrospective study of 102 patients treated with the Boston brace. Eur. Spine J. 2007, 16, 393–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grivas, T.B.; Vasiliadis, E.; Chatziargiropoulos, T.; Polyzois, V.D.; Gatos, K. The effect of a modified Boston brace with anti-rotatory blades on the progression of curves in idiopathic scoliosis: Aetiologic implications. Pediatr. Rehabil. 2003, 6, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Pasquini, G.; Cecchi, F.; Bini, C.; Molino-Lova, R.; Vannetti, F.; Castagnoli, C.; Paperini, A.; Boni, R.; Macchi, C.; Crusco, B.; et al. The outcome of a modified version of the Cheneau brace in adolescent idiopathic scoliosis (AIS) based on SRS and SOSORT criteria: A retrospective study. Eur J Phys Rehabil Med 2016, 52, 618–629. [Google Scholar] [PubMed]
- Fang, M.-Q.; Wang, C.; Xiang, G.-H.; Lou, C.; Tian, N.-F.; Xu, H.-Z. Long-term effects of the Chêneau brace on coronal and sagittal alignment in adolescent idiopathic scoliosis. J. Neurosurg. Spine 2015, 23, 505–509. [Google Scholar] [CrossRef] [Green Version]
- Pham, V.-M.; Herbaux, B.; Schill, A.; Thevenon, A. Evaluation of the Chêneau brace in adolescent idiopathic scoliosis. Évaluation du résultat du corset Chêneau dans la scoliose idiopathique l’adolescent 2007, 50, 125–133. [Google Scholar]
- Zabrowska-Sapeta, K.; Kowalski, I.M.; Protasiewicz-Fałdowska, H.; Wolska, O. Evaluation of the effectiveness of Chêneau brace treatment for idiopathic scoliosis—Own observations. Pol. Ann. Med. 2010, 17, 44–53. [Google Scholar] [CrossRef]
- Aulisa, A.G.; Guzzanti, V.; Galli, M.; Perisano, C.; Falciglia, F.; Maggi, G.; Aulisa, L. Treatment of lumbar curves in adolescent females affected by idiopathic scoliosis with a progressive action short brace (PASB): Assessment of results according to the SRS committee on bracing and nonoperative management standardization criteria. J. Orthop. Traumatol. 2009, 12, S38. [Google Scholar] [CrossRef] [Green Version]
- Aulisa, A.G.; Guzzanti, V.; Falciglia, F.; Giordano, M.; Marzetti, E.; Aulisa, L. Lyon bracing in adolescent females with thoracic idiopathic scoliosis: A prospective study based on SRS and SOSORT criteria Orthopedics and biomechanics. BMC Musculoskelet. Disord. 2015, 16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, H.-R.; Tournavitis, N.; Seibel, S.; Kleban, A. A Prospective Cohort Study of AIS Patients with 40° and More Treated with a Gensingen Brace (GBW): Preliminary Results. Open Orthop. J. 2017, 11, 1558–1567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuroki, H.; Inomata, N.; Hamanaka, H.; Higa, K.; Chosa, E.; Tajima, N. Predictive factors of Osaka Medical College (OMC) brace treatment in patients with adolescent idiopathic scoliosis. Scoliosis 2015, 10, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, Y.; Lou, E.; Lam, T.P.; Cheng, J.C.-Y.; Sin, S.W.; Kwok, W.K.; Wong, M.S. The Intelligent Automated Pressure-Adjustable Orthosis for Patients With Adolescent Idiopathic Scoliosis: A Bi-Center Randomized Controlled Trial. Spine 2020, 45, 1395–1402. [Google Scholar] [CrossRef] [PubMed]
- Price, C.T.; Scott, D.S.; Reed, F.E.; Riddick, M.F. Nighttime bracing for adolescent idiopathic scoliosis with the Charleston bending brace. Preliminary report. Spine 1990, 15, 1294–1299. [Google Scholar] [CrossRef]
- Lee, C.S.; Hwang, C.J.; Kim, D.-J.; Kim, J.H.; Kim, Y.-T.; Lee, M.Y.; Yoon, S.J.; Lee, D.-H. Effectiveness of the Charleston night-time bending brace in the treatment of adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2012, 32, 368–372. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.; Murphy, J.S.; Shaw, K.A.; Cash, K.; Devito, D.P.; Schmitz, M.L. Nighttime bracing with the Providence thoracolumbosacral orthosis for treatment of adolescent idiopathic scoliosis: A retrospective consecutive clinical series. Prosthet. Orthot. Int. 2019, 43, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Ohrt-Nissen, S.; Hallager, D.W.; Gehrchen, M.; Dahl, B. Flexibility Predicts Curve Progression in Providence Nighttime Bracing of Patients With Adolescent Idiopathic Scoliosis. Spine 2016, 41, 1724–1730. [Google Scholar] [CrossRef]
- Bohl, D.D.; Telles, C.J.; Golinvaux, N.S.; Basques, B.A.; DeLuca, P.A.; Grauer, J.N. Effectiveness of Providence nighttime bracing in patients with adolescent idiopathic scoliosis. Orthopedics 2014, 37, e1085-90. [Google Scholar] [CrossRef] [Green Version]
- Simony, A.; Beuschau, I.; Quisth, L.; Jespersen, S.M.; Carreon, L.Y.; Andersen, M.O. Providence nighttime bracing is effective in treatment for adolescent idiopathic scoliosis even in curves larger than 35°. Eur. Spine J. 2019, 28, 2020–2024. [Google Scholar] [CrossRef]
- Coillard, C.; Vachon, V.; Circo, A.B.; Beauséjour, M.; Rivard, C.H. Effectiveness of the SpineCor brace based on the new standardized criteria proposed by the scoliosis research society for adolescent idiopathic scoliosis. J. Pediatr. Orthop. 2007, 27, 375–379. [Google Scholar] [CrossRef] [Green Version]
- Coillard, C.; Circo, A.B.; Rivard, C.H. A prospective randomized controlled trial of the natural history of idiopathic scoliosis versus treatment with the SpineCor brace. Sosort Award 2011 winner. Eur. J. Phys. Rehabil. Med. 2014, 50, 479–487. [Google Scholar]
- Hanks, G.A.; Zimmer, B.; Nogi, J. TLSO treatment of idiopathic scoliosis. An analysis of the Wilmington jacket. Spine 1988, 13, 626–629. [Google Scholar] [CrossRef]
- Katz, D.E.; Herring, J.A.; Browne, R.H.; Kelly, D.M.; Birch, J.G. Brace wear control of curve progression in adolescent idiopathic scoliosis. J. Bone Joint Surg. Am. 2010, 92, 1343–1352. [Google Scholar] [CrossRef] [PubMed]
- Maruyama, T.; Kobayashi, Y.; Miura, M.; Nakao, Y. Effectiveness of brace treatment for adolescent idiopathic scoliosis. Scoliosis 2015, 10, S12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aulisa, A.G.; Giordano, M.; Toniolo, R.M.; Aulisa, L. Long term results after brace treatment with PASB in adolescent idipathic scoliosis. Minerva Anestesiol. 2020. [Google Scholar] [CrossRef]
- Lateur, G.; Grobost, P.; Gerbelot, J.; Eid, A.; Griffet, J.; Courvoisier, A. Efficacy of nighttime brace in preventing progression of idiopathic scoliosis of less than 25°. Orthop. Traumatol. Surg. Res. 2017, 103, 275–278. [Google Scholar] [CrossRef]
- Minsk, M.K.; Venuti, K.D.; Daumit, G.L.; Sponseller, P.D. Effectiveness of the Rigo Chêneau versus Boston-style orthoses for adolescent idiopathic scoliosis: A retrospective study. Scoliosis Spin. Disord. 2017, 12, 1–6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janicki, J.A.; Poe-Kochert, C.; Armstrong, D.G.; Thompson, G.H. A comparison of the thoracolumbosacral orthoses and providence orthosis in the treatment of adolescent idiopathic scoliosis: Results using the new SRS inclusion and assessment criteria for bracing studies. J. Pediatr. Orthop. 2007, 27, 369–374. [Google Scholar] [CrossRef] [Green Version]
- Ohrt-Nissen, S.; Lastikka, M.; Andersen, T.B.; Helenius, I.; Gehrchen, M. Conservative treatment of main thoracic adolescent idiopathic scoliosis: Full-time or nighttime bracing? J. Orthop. Surg. 2019, 27, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Weiss, H.-R.; Weiss, G.M. Brace treatment during pubertal growth spurt in girls with idiopathic scoliosis (IS): A prospective trial comparing two different concepts. Pediatr. Rehabil. 2005, 8, 199–206. [Google Scholar] [CrossRef]
- Guo, J.; Lam, T.P.; Wong, M.S.; Ng, B.K.W.; Lee, K.M.; Liu, K.L.; Hung, L.H.; Lau, A.H.Y.; Sin, S.W.; Kwok, W.K.; et al. A prospective randomized controlled study on the treatment outcome of SpineCor brace versus rigid brace for adolescent idiopathic scoliosis with follow-up according to the SRS standardized criteria. Eur. Spine J. 2014, 23, 2650–2657. [Google Scholar] [CrossRef]
- Emans, M.J.B.; Hresko, M.D.M.T.; Hall, M.D.J.E.; Hedequist, C.D.; Karlin, M.D.L.; Miller, M.D.J.; Miller, R.R.; Magin, C.P.O.M.; McCarthy, R.N.C.; Cassella, R.M.; et al. Reference Manual for the Boston Scoliosis Brace; 2003; Available online: https://www.bostonoandp.com/Customer-Content/www/CMS/files/BostonBraceManual.pdf (accessed on 12 January 2021).
- Fayssoux, R.S.; Cho, R.H.; Herman, M.J. A history of bracing for idiopathic scoliosis in north America. Clin. Orthop. Relat. Res. 2010, 468, 654–664. [Google Scholar] [CrossRef] [Green Version]
- Donzelli, S.; Zaina, F.; Minnella, S.; Lusini, M.; Negrini, S. Consistent and regular daily wearing improve bracing results: A case-control study. Scoliosis spinal Disord. 2018, 13, 16. [Google Scholar] [CrossRef]
- Misteroska, E.; Glowacki, J.; Głowacki, M.; Okręt, A. Long-term effects of conservative treatment of Milwaukee brace on body image and mental health of patients with idiopathic scoliosis. PLoS ONE 2018, 13. [Google Scholar] [CrossRef] [Green Version]
- Aulisa, A.G.; Guzzanti, V.; Falciglia, F.; Galli, M.; Pizzeti, P.; Aulisa, L. Curve progression after long-term brace treatment in adolescent idiopathic scoliosis: Comparative results between over and under 30 Cobb degrees—SOSORT 2017 award winner. Scoliosis Spin. Disord. 2017, 12. [Google Scholar] [CrossRef] [Green Version]
- Bunge, E.M.; De Koning, H.J. Bracing patients with idiopathic scoliosis: Design of the Dutch randomized controlled treatment trial. BMC Musculoskelet. Disord. 2008, 9, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kunz, R.; Oxman, A.D. The unpredictability paradox: Review of empirical comparisons of randomised and non-randomised clinical trials. BMJ 1998, 317, 1185–1190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandenbroucke, J.P. Why do the results of randomised and observational studies differ? Statistical theory conflicts with empirical findings in several areas of research. BMJ 2011, 343, 1128. [Google Scholar] [CrossRef]
- Ioannidis, J.P.; Lau, J. Completeness of Safety Reporting in Randomized Trials. JAMA 2001, 285, 437. [Google Scholar] [CrossRef] [PubMed]
- Concato, J. Randomized controlled trial, observational studies and the hierarchy of research designs. Int. J. Biol. Markers 2000, 15, 79–83. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Richards, B.S.; Bernstein, R.M.; D’Amato, C.R.; Thompson, G.H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine 2005, 30, 2068–2075. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, S.S.; Nelson, I.W.; Ho, E.K.; Hsu, L.C.; Leong, J.C. New Prognostic Factors to Predict the Final Outcome of Brace Treatment in Adolescent Idiopathic Scoliosis. Spine 1995. [Google Scholar] [CrossRef] [PubMed]
| PubMed | (((scoliosis [MeSH Terms] OR scolio * [Title/Abstract] OR spinal curvature [Title/Abstract] OR AIS [Title/Abstract]))) AND ((((brace [MeSH Terms] OR brace [Title/Abstract] OR bracing [Title/Abstract]))) AND ((time [Title/Abstract] OR parttime [Title/Abstract] OR nighttime [Title/Abstract] OR compliance [MeSH Terms] OR compliance [Title/Abstract] OR compliant [Title/Abstract] OR effect [Title/Abstract] OR treatment * [Title/Abstract] OR result [Title/Abstract] OR results [Title/Abstract] OR therap [Title/Abstract] OR mental disorder [Title/Abstract] OR hypersensitive [Title/Abstract] OR peer problem [Title/Abstract] OR depress [Title/Abstract]) OR psychologic [Title/Abstract] OR quality of life [Title/Abstract] OR quality of life [MeSH] OR life quality [Title/Abstract])))). |
| Medscape | (‘scoliosis’: exp OR ‘scolio *’: ti, ab, kw OR ‘spinal curvature *’: ti, ab, kw OR ‘AIS’: ti, ab, kw) AND (‘brace’: exp OR ‘brace *’: ti, ab, kw OR ‘braci *’: ti, ab, kw) AND (‘time’: ti, ab, kw OR ‘parttime’: ti, ab, kw OR ‘nighttime’: ti, ab, kw OR ‘compliance’: exp OR ‘compliance’: ti, ab, kw OR ‘compliant’: ti, ab, kw OR ‘effect *’: ti, ab, kw OR ‘treatment *’: ti, ab, kw OR ‘result’: ti, ab, kw OR ‘results’: ti, ab, kw OR ‘therap *’: ti, ab, kw OR ‘mental disorder *’: ti, ab, kw OR ‘hypersensitiv *’: ti, ab, kw OR ‘peer problem *’: ti, ab, kw OR ‘depress *’: ti, ab, kw OR ‘psychologic *’: ti, ab, kw OR ‘quality of life’: ti, ab, kw OR ‘quality of life’: exp OR ‘life quality’: ti, ab, kw) |
| 1 | Design | Longitudinal studies with at least one-year follow-up from brace initiation |
| 2 | Population | Patients with adolescent idiopathic scoliosis |
| 3 | Intervention | Specification of the concept(s) of brace (prescribed wearing time(s) and brace type(s)) used |
| 4 | Outcome | A definition of success rate (all definitions of success rate were accepted in the qualitative synthesis in this review) |
| 1 | A clearly stated aim | The question address should be precise and relevant. |
| 2 | Inclusions of consecutive patients | All patients potentially fit for inclusion had been included in the study. |
| 3 | Prospective collection data | Data were collected according to a protocol established before the beginning of the study. |
| 4 | Endpoints appropriate to the aim of the study | Unambiguous explanation of the criteria used to evaluate the main outcome. |
| 5 | Unbiased assessment of the study endpoint | Blind evaluation of objective end-points and double blind-evaluation of subjective endpoints. Other explanation of the reasons for not blinding. |
| 6 | Follow-up period appropriate to the aim of the study | The follow-up should be should be sufficiently long to allow the assessment of the main end-points. |
| 7 | Loss to follow-up less than 5% | All patients should be included in the follow-up. Otherwise, the proportion lost should not exceed the proportion experiencing the major end-points. |
| 8 | Prospective calculation of the study size | Information of the size of detectable difference of interest with a calculation of 95% confidence interval. |
| 9 | An adequate control group | Having a gold standard diagnostic test or therapeutic intervention recognized as the optimal intervention according to the available published data. |
| 10 | Contemporary groups | Control and studied group should be managed during the same time period. |
| 11 | Baseline equivalence of groups | The groups should be similar regarding criteria and studied end-point. |
| 12 | Adequate statistical analysis | Whether the statistics were in accordance with the type of study with calculation of confidence interval or relative risk. |
| Brace Type | Rigidity | Prescribed Wearing Time |
|---|---|---|
| Boston [22,23,24] | Rigid brace | Full-time/part-time |
| Cheneau brace [25,26,27,28] | Rigid brace | Full-time/part-time |
| PASB (Progressive Action Short Brace) [29] | Rigid brace | Full-time |
| Lyon brace [30] | Rigid brace | Full-time |
| Gensingen Brace [31] | Rigid brace | Full-time |
| OMC (Osaka Medical College) brace [32] | Rigid brace | Full-time |
| Pressure-adjustable orthosis [33] | Rigid brace | Full-time |
| Charleston brace [34,35] | Rigid brace | Night-time |
| Providence brace [5,36,37,38,39] | Rigid brace | Night-time |
| SpineCor [40,41] | Soft brace | Full-time |
| First Author | Year | Risk of Bias | Sample Size | Cobb Angle | Skeletal Maturity | Type of Brace | Brace | Timing | Follow-Up | Definition of Success Rate | Success Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Weinstein [6] | 2014 | 14/24 | 146 | 20–40 | Risser 0–2 | Rigid | TLSO | Full-time | 7 years | >50° | 72% |
| 96 | Control group | 42% | |||||||||
| Xu [22] | 2019 | 8/16 | 90 | 40–45 | Risser 0–3 (divided in subgroups) | Rigid | Boston brace | Full-time | 2 years | ≤5° | 51.1% |
| Yrjonen [23] | 2007 | 10/24 | 51 | >25° | Risser 0–3 | Rigid | Boston brace | Full-time | > 1 year | ≤5° | Girls 78.4% |
| 51 | Boys 62.7% | ||||||||||
| Grivas [24] | 2003 | 7/16 | 28 | 20–40 | Pre or < 1 year post-menarche and Risser | Rigid | modified Boston brace | Full-time | mean of 2.3 years | ≤5° | 82% |
| Pasquini [25] | 2016 | 5/16 | 843 | 20–40 | Risser 0–2 | Rigid | modified Cheneau brace | Full-time | ≥2 years | ≤5° | 81% |
| Fang [26] | 2015 | 10/16 | 32 | 25–40 | Risser 0–2 | Rigid | Cheneau brace | Full-time | 2 years | no curve progression ≥ 50° | 81% |
| Pham [27] | 2007 | 7/16 | 63 | 20–45 | Risser 0–2 | Rigid | Cheneau brace | Full-time | 2 years after discontinuing brace therapy | <10° | 85.7% |
| Zabrowska Sapeta [28] | 2010 | 7/16 | 79 | 20–45 | Risser 0–4 | Rigid | Cheneau brace + exercises | Full-time | 1–5 years | ≤5° | 48% |
| Maruyama [44] | 2015 | 9/16 | 33 | 25–40 | Risser 0–2 and pre or 1 year post-menarche | Rigid | Rigo- Cheneau brace | Full-time | Mean 2.8 years | ≤5° | 76% |
| Aulisa [29] | 2009 | 6/16 | 50 | 25–40 | Risser 0–2 | Rigid | PASB | Full-time | > 2 years | ≤5° | 100% |
| Aulisa [45] | 2020 | 12/16 | 163 | 20–60 mean 28 | Risser 0–4 | Rigid | PASB | 10y after termination | ≤5° | 65.6% | |
| Aulisa [30] | 2015 | 4/16 | 69 | 25–40 | Risser 0–2 | Rigid | Lyon brace | Full-time | 2 years | ≤5° | 98.5% |
| Weiss [31] | 2017 | 9/16 | 25 | ≥40 | Risser 0–2 | Rigid | Gensingen Brace | Full-time | ≥ 1.5 years | ≤5° | 92% |
| Kuroki [32] | 2015 | 10/16 | 31 | 20–40 | Risser 0–2 | Rigid | OMC brace | Full-time | 2 years after discontinuing brace therapy | no curve progression ≥ 50° | 67.8% |
| Yangmin Lin [33] | 2020 | 6/16 | 24 | 20–40 | Risser 0–2 | Rigid | Pressure-adjustable orthosis | 1 year | ≤5° | 100% | |
| Lateur [46] | 2017 | 10/16 | 142 | <25 | Risser 0–3 | Rigid | Night-time brace | Night-time | >1 year mean 3.75 y | ≤5° | 83% |
| Price [34] | 1990 | 7/16 | 139 | 25–49 | Risser 0–2 | Rigid | Charleston brace | Night-time | > 1 year | ≤5° | 83% |
| Lee [35] | 2012 | 9/16 | 95 | 25–40 | Risser 0–2 | Rigid | Charleston brace | Night-time | > 2 years after skeletal maturity | ≤5° | 84.2% |
| Davis [36] | 2019 | 6/16 | 56 | 25–40 | Risser 0–2 | Rigid | Providence brace | Night-time | mean 2.21 years | ≤5° | 51.8% |
| Ohrt-Nissen [37] | 2016 | 7/16 | 63 | 25–40 | Risser 0–2 | Rigid | Providence brace | Night-time | 2 years | ≤5° | 57% |
| D’ Amato [5] | 2001 | 8/16 | 102 | 20–42 | Risser 0–2 | Rigid | Providence brace | Night-time | Min 2 y after stop bracing | ≤5° | 74% |
| Bohl [38] | 2014 | 6/16 | 34 | 25–40 | Risser 0–2 | Rigid | Providence brace | Night-time | 2 years after maturity | ≤5° or >45 degrees | 50% >5°, 59% >45° |
| Simony [39] | 2019 | 10/16 | 80 | 20–45 | Pre or < 1 year post-menarche | Rigid | Providence brace | Night-time | Till 1 year after stop bracing | ≤5° | 89% |
| Coillard [40] | 2007 | 8/16 | 170 | 25–40 | Risser 0–2 | Soft | SpineCor | Full-time | 2 years after discontinuing brace therapy | ≤5° | 59.4% |
| Coillard [41] | 2014 | 16/24 | 32 | 15–30 | Risser 0–2 | Soft | SpineCor brace | Full-time | 5 years | ≤5° | 73% |
| 36 | control group | 57% |
| First Author | Year | Risk of Bias | Sample Size | Cobb Angle | Skeletal Maturity | Type of Brace | Brace | Timing | Follow-Up | Definition of Success Rate | Success Rate |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Minsk [47] | 2017 | 11/24 | 13 | 25–40 | Risser 0–2 | Rigid | Rigo- Cheneau | Full-time | >1 year | ≤5°; no need of surgery | Spinal surgery: 0% >6°:31% |
| 93 | Boston | Spinal surgery: 34% | |||||||||
| Hanks [42] | 1988 | 11/24 | 75 | >25 | Risser 0–4 | Rigid | Wilmington Jacket | Full-time | 1 year after discontinuing brace | <10° | Full-time 80% |
| 25 | Part-time | 84% | |||||||||
| Katz [43] | 2010 | 11/24 | 57 | 25–40 | Risser 0–2 | Rigid | Boston brace | Full-time | >1 year | ≤5° | 82% > 12 h |
| 43 | Part-time | 31% > 7 h | |||||||||
| Yrjonen [4] | 2006 | 12/24 | 36 | >25° | Risser sign 0–3 | Rigid | Providence brace | Night-time | mean 1.8 years | ≤5° | 72% |
| 36 | Rigid | Boston brace | Full-time | 78% | |||||||
| Janicki [48] | 2007 | 10/24 | 35 | 25–40 | Risser 0–2 | Rigid | Providence brace | Night-time | >2 years | ≤5° | 31% |
| 48 | Rigid | Custom TLSO | Full-time | 15% | |||||||
| Ohrt-Nissen [49] | 2019 | 13/24 | 40 | 25–40 | Risser 0–2 | Rigid | Providence brace | Night-time | 2 years | ≤5° (primary outcome); curve progression ≥45° | 45% |
| 37 | Rigid | Boston brace | Full-time | 38% | |||||||
| Weiss [50] | 2005 | 8/24 | 12 | 15-30 and >30 for rigid brace | Risser sign 0 (one exeption with 1) Tanner 2 or 3 | Soft | SpineCor | Full-time | mean 3.5 years | ≤5° | 8% |
| 10 | Rigid | Cheneau brace | Full-time | 80% | |||||||
| Guo [51] | 2014 | 13/24 | 20 | 20–30 | Risser 0–2 Pre or < 1 year post-menarche | Soft | SpineCor brace | Full-time | 2 years after discontinuing brace therapy | ≤5° | 65% |
| 18 | Rigid | TLSO | Full-time | 94% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, L.; Schlosser, T.P.C.; Jimale, H.; Homans, J.F.; Kruyt, M.C.; Castelein, R.M. The Effectiveness of Different Concepts of Bracing in Adolescent Idiopathic Scoliosis (AIS): A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 2145. https://doi.org/10.3390/jcm10102145
Costa L, Schlosser TPC, Jimale H, Homans JF, Kruyt MC, Castelein RM. The Effectiveness of Different Concepts of Bracing in Adolescent Idiopathic Scoliosis (AIS): A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(10):2145. https://doi.org/10.3390/jcm10102145
Chicago/Turabian StyleCosta, Lorenzo, Tom P. C. Schlosser, Hanad Jimale, Jelle F. Homans, Moyo C. Kruyt, and René M. Castelein. 2021. "The Effectiveness of Different Concepts of Bracing in Adolescent Idiopathic Scoliosis (AIS): A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 10: 2145. https://doi.org/10.3390/jcm10102145
APA StyleCosta, L., Schlosser, T. P. C., Jimale, H., Homans, J. F., Kruyt, M. C., & Castelein, R. M. (2021). The Effectiveness of Different Concepts of Bracing in Adolescent Idiopathic Scoliosis (AIS): A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 10(10), 2145. https://doi.org/10.3390/jcm10102145







