High Accommodative Convergence/Accommodation Ratio Consecutive Esotropia Following Surgery for Intermittent Exotropia: Clinical Feature, Diagnosis, and Treatment
Abstract
:1. Introduction
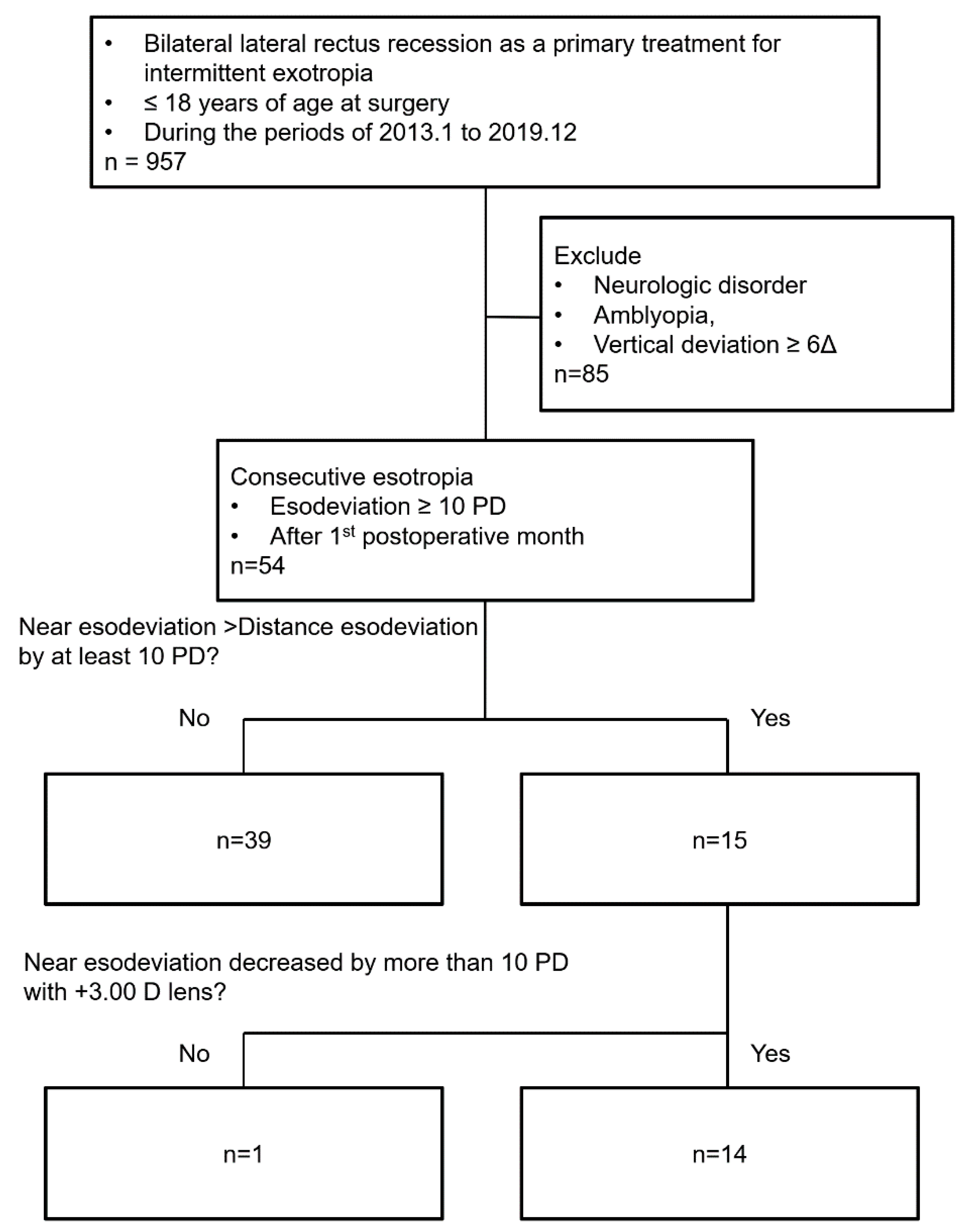
2. Methods
2.1. Subjects
2.2. Preoperative-Assessment Data
2.3. Surgical Procedures
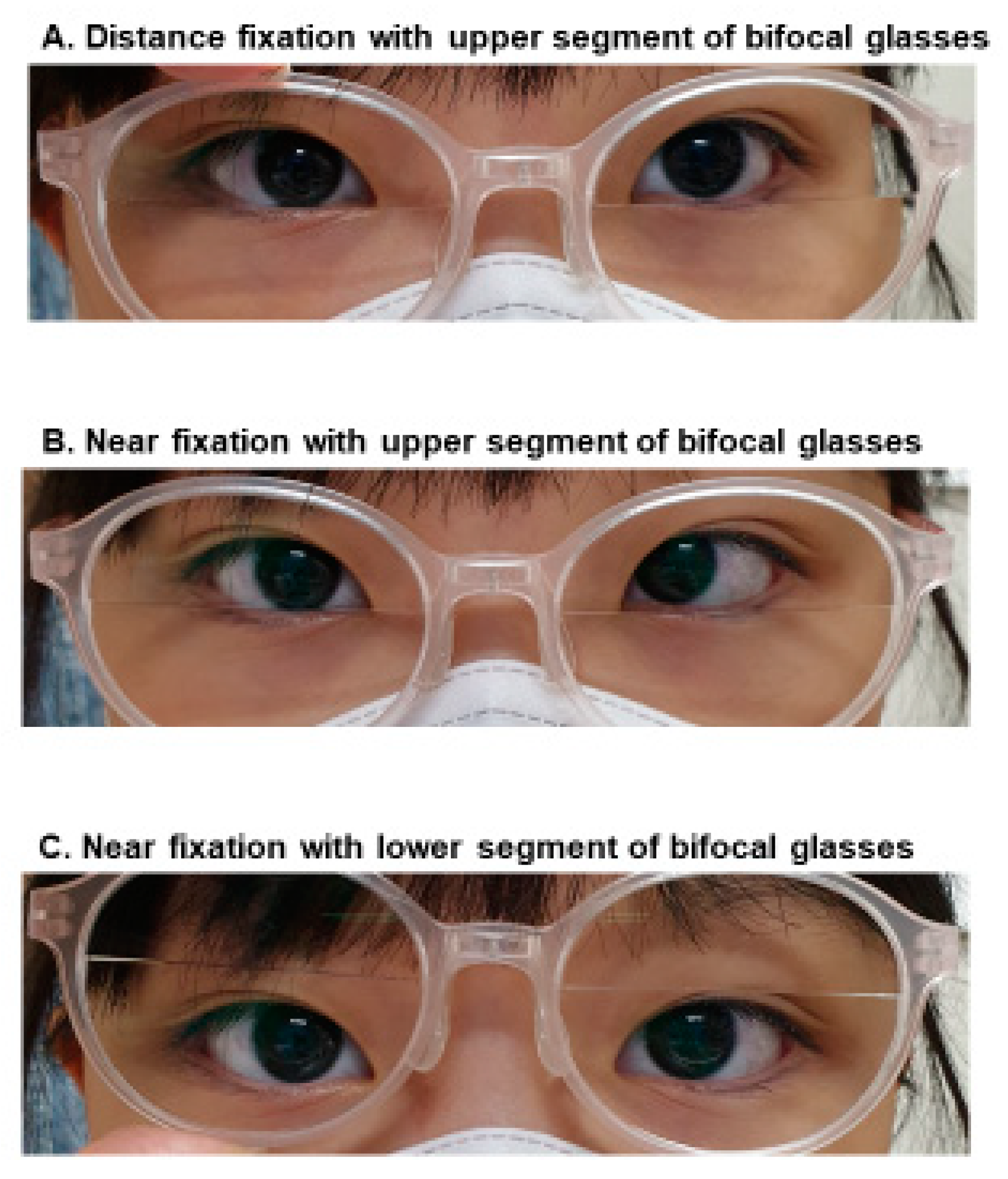
2.4. Postoperative-Assessment Data
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kushner, B.J.; Morton, G.V. Distance/Near Differences in Intermittent Exotropia. Arch. Ophthalmol. 1998, 116, 478–486. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Burian, H.M. Exodeviations: Their Classification, Diagnosis and Treatment. Am. J. Ophthalmol. 1966, 62, 1161–1166. [Google Scholar] [CrossRef]
- Cooper, J.; Ciuffreda, K.J.; Kruger, P.B. Stimulus and response AC/A ratios in intermittent exotropia of the divergence-excess type. Br. J. Ophthalmol. 1982, 66, 398–404. [Google Scholar] [CrossRef] [PubMed]
- Brodsky, M.C.; Fray, K.J. Surgical management of intermittent exotropia with high AC/A ratio. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 1998, 2, 330–332. [Google Scholar] [CrossRef]
- Kushner, B.J. Exotropic Deviations: A Functional Classification and Approach to Treatment. Am. Orthopt. J. 1988, 38, 81–93. [Google Scholar] [CrossRef]
- Jeon, H.; Choi, H. Postoperative Esotropia: Initial Overcorrection or Consecutive Esotropia? Eur. J. Ophthalmol. 2017, 27, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.W.; Kim, J.H.; Hwang, J.-M. Long-Term Outcome of Patients with Large Overcorrection following Surgery for Exotropia. Ophthalmologica 2005, 219, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Buck, D.; Powell, C.J.; Sloper, J.J.; Taylor, R.; Tiffin, P.; Clarke, M.P. Surgical intervention in childhood intermittent exotropia: Current practice and clinical outcomes from an observational cohort study. Br. J. Ophthalmol. 2012, 96, 1291–1295. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, D.H.; Ahn, H.; Lim, H.T. Proposing a new scoring system in intermittent exotropia: Towards a better assessment of control. Can. J. Ophthalmol. 2017, 52, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.K.; Hwang, J.-M. Prismatic Correction of Consecutive Esotropia in Children after a Unilateral Recession and Resection Procedure. Ophthalmologica 2013, 120, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.H.; Park, J.M.; Lee, S.J. Factors predisposing to consecutive esotropia after surgery to correct intermittent exotropia. Graefe’s Arch. Clin. Exp. Ophthalmol. 2012, 250, 1485–1490. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.J.; Choi, D.G. Consecutive esotropia after surgery for intermittent exotropia: The clinical course and factors associated with the onset. Br. J. Ophthalmol. 2014, 98, 871–875. [Google Scholar] [CrossRef] [PubMed]
- Ing, M.R.; Nishimura, J.; Okino, L. Outcome study of bilateral lateral rectus recession for intermittent exotropia in children. Ophthalmic Surg. Lasers 1999, 30, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Kushner, B.J. Diagnosis and treatment of exotropia with a high accommodation convergence-accommodation ratio. Arch. Ophthalmol. 1999, 117, 221–224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arnoldi, K.A.; Reynolds, J.D. Diagnosis of Pseudo-Divergence Excess Exotropia Secondary to High Accommodative Convergence to Accommodation Ratio. Am. Orthopt. J. 2006, 56, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Lucas, E.; Bentley, C.R.; Aclimandos, W. The effect of surgery on the AC/A ratio. Eye 1994, 8, 109–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, H.Y.; Jung, J.H. Bilateral lateral rectus muscle recession with medial rectus pulley fixation for divergence excess intermittent exotropia with high AC/A ratio. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2013, 17, 266–268. [Google Scholar] [CrossRef] [PubMed]
- Parks, M.M. Abnormal Accommodative Convergence in Squint. Arch. Ophthalmol. 1958, 59, 364–380. [Google Scholar] [CrossRef] [PubMed]
- Whitman, M.C.; MacNeill, K.; Hunter, D.G. Bifocals Fail to Improve Stereopsis Outcomes in High AC/A Accommodative Esotropia. Ophthalmologica 2016, 123, 690–696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tejedor, J.; Gutiérrez-Carmona, F.J. Amblyopia in High Accommodative Convergence/Accommodation Ratio Accommodative Esotropia. Influence of Bifocals on Treatment Outcome. Am. J. Ophthalmol. 2018, 191, 124–128. [Google Scholar] [CrossRef] [PubMed]
| High AC/A Ratio Group (n = 14) | Normal AC/A Ratio Group (n = 40) | p Value | |
|---|---|---|---|
| Mean age at presentation (years) | 3.9 ± 2.1 | 4.1 ± 3.0 | 0.89 † |
| Mean age at surgery (years) | 4.9 ± 1.9 | 5.6 ± 2.7 | 0.42 † |
| Postoperative F/U duration (months) | 37.4 ± 16.4 | 28.8 ± 16.6 | 0.30 † |
| Onset of consecutive ET after surgery (months) | 4.1 ± 5.0 | 5.0 ± 8.1 | 0.86 † |
| Male gender | 6 (42.9%) | 12 (30%) | 0.29 ‡ |
| Type of exotropia | |||
| Basic type | 14 | 40 | 0.71 ‡ |
| Divergence excess type | 0 | 0 | |
| Convergence insufficiency type | 0 | 0 | |
| Preoperative control score (LACTOSE) at distance | |||
| 0–2 | 1 (8.3%) | 1 (3.2%) | 0.50 ‡ |
| 3–4 | 11 (91.6%) | 30 (96.8%) | |
| NA | 2 | 10 | |
| Preoperative control score (LACTOSE) at near | |||
| 0–2 | 10 (83.3%) | 14 (46.7%) | 0.03 ‡ |
| 3–4 | 2 (16.6%) | 8 (53.4%) | |
| NA | 2 | 10 | |
| Preoperative SE, OD (D) | −0.6 ± 2.1 | −0.4 ± 1.4 | 0.96 † |
| Preoperative SE, OS (D) | −0.5 ± 1.8 | −0.3 ± 1.4 | 0.99 † |
| Preoperative stereoacuity (seconds of arc) | |||
| ≤100 | 8 | 21 | 0.36 ‡ |
| >100 | 4 | 6 | |
| NA | 2 | 13 | |
| Mean | 111.7 | 101.9 | 0.46 |
| Preoperative angle of exodeviation | |||
| Distance (PD) | 27.3 ± 7.5 | 28.3 ± 6.5 | 0.34 † |
| Near (PD) | 29.4 ± 7.0 | 29.7 ± 6.4 | 0.50 † |
| Absolute value of distance-near angle (PD) | 2.1 ± 2.3 | 2.8 ± 3.9 | 0.82 † |
| Postoperative angle of esodeviation (1st postoperative month) | |||
| Distance (PD) | −7.4 ± 8.1 | −9.8 ± 6.5 | 0.13 † |
| Near (PD) | −7.4 ± 8.1 | −9.6 ± 6.6 | 0.18 † |
| Surgical correction for consecutive ET | |||
| Yes | 3 (21.4%) | 11 (27.5%) | 0.45 ‡ |
| No | 11 (78.6%) | 29 (72.5%) | |
| Final angle of deviation | |||
| Distance (PD) | −0.9 ± 2.4 | −13.0 ± 5.0 | <0.001 † |
| Near (PD) | −0.4 ± 1.6 | −12.4 ± 5.7 | <0.001 † |
| Final stereoacuity (seconds of arc) | |||
| ≤100 | 13 (92.9%) | 17 (46.0%) | 0.11 ‡ |
| >100 | 1 (7.1%) | 33 (54.0%) | |
| Mean | 67.9 | 670.0 | 0.04 † |
| Patient No | Sex | Age at Surgery for XT (year) | Preop Angle of XT (Δ) | Preop SE (D) | Preop SA (SecArc) | Surgery | Onset of Consecutive ET (mo) | Max. Angle of Consecutive ET (Δ) | AC/A Ratio | Time from Surgery to Start of Bifocals (mo) | Duration of Wearing Bifocals (mo) | After Wearing Bifocal Glasses | Response to Bifocals | Clinical Course | Postoperative FU Period (mo) | Final Alignment | Final SA (SecArc) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 4 | Dcc 25 Ncc 30 | R + 1.50 L + 2.00 | 140 | BLRc 6.50 | 2 | Dcc ortho Ncc 30 | 8.3 | 4 | 51 | Dcc ortho Ncc 30 Ncc+3 ortho | Good response to bifocals | Successfully weaned from bifocals | 74 | Dcc ortho Ncc ortho | 100 |
| 2 | F | 2 | Dcc 50 Ncc 50 | R − 0.50 L − 0.50 | NA | BLRc 9.00 | 6 | Dcc 5 Ncc 20 | 6.7 | 19 | 10 | Dcc ortho Ncc 16 Ncc+3 ortho | Good response to bifocals | Successfully weaned from bifocals | 50 | Dcc ortho Ncc 5 ET | 80 |
| 3 | M | 3 | Dcc 30 Ncc 30 | R + 1.00 L + 1.00 | NA | BLRc 7.25 | 1 | Dcc 20 Ncc 30 | 4.7 | 5 | 54 | Dcc ortho Ncc 10 Ncc+3 ortho | Good response to bifocals | Successfully weaned from bifocals | 59 | Dcc ortho Ncc ortho | 80 |
| 4 | M | 8 | Dcc 20 Ncc 23 | R − 2.25 L − 2.25 | 40 | BLRc 6.50 | 2 | Dcc 10 Ncc 25 | 6.7 | 4 | 25 | Dcc ortho Ncc 10 Ncc+3 ortho | Good response to bifocals | Successfully weaned from bifocals | 29 | Dcc ortho Ncc ortho | 40 |
| 5 | M | 7 | Dcc 20 Ncc 25 | R + 0.50 L + 0.50 | 80 | BLRc 6.25 | 1 | Dcc 10 Ncc 25 | 5.0 | 2 | 18 | Dcc ortho Ncc 14 ET Ncc+3 ortho | Good response to bifocals | Successfully weaned from bifocals | 32 | Dcc ortho Ncc ortho | 80 |
| 6 | F | 4 | Dcc 30 Ncc 35 | R + 0.50 L + 0.50 | 40 | BLRc 7.50 | 4 | Dcc 10 Ncc 30 | 5.0 | 5 | 25 | Dcc ortho Ncc 20 ET Ncc+3 ortho | Good response to bifocals | Need to continue wearing bifocals | 30 | Dcc ortho Ncc 20 ET Ncc+3 ortho | 80 |
| 7 | F | 4 | Dcc 25 Ncc 30 | R + 2.00 L + 2.00 | 60 | BLRc 7.25 | 1 | Dcc 10 Ncc 25 | 6.7 | 12 | 8 | Dcc 10 Ncc 25 Ncc+3 ortho | Good response to bifocals | Need to continue wearing bifocals | 20 | Dcc 5 ET Ncc 20 ET Ncc+3 ortho | 40 |
| 8 | F | 6 | Dcc 25 Ncc 25 | R 0.00 L + 1.00 | 60 | BLRc 7.00 | 6 | Dcc 6 Ncc 30 | 8.0 | 9 | 6 | Dcc ortho Ncc 20 ET Ncc+3 ortho | Good response to bifocals | Need to continue wearing bifocals | 21 | Dcc ortho Ncc 16 ET Ncc+3 ortho | 40 |
| 9 | M | 5 | Dcc 25 Ncc 25 | R − 0.75 L − 0.75 | 100 | BLRc 6.75 | 1 | Dcc 5 Ncc 20 | 5.0 | 5 | 7 | Dcc 2 ET Ncc 20 ET Ncc+3 ortho | Good response to bifocals | Need to continue wearing bifocals | 12 | Dcc ortho Ncc 14 ET Ncc+3 ortho | 60 |
| 10 | F | 5 | Dcc 25 Ncc 30 | R + 1.50 L + 1.75 | 40 | BLRc 7.25 | 1 | Dcc 12 ET Ncc 30 ET | 6.0 | 19 | 16 | Dcc ortho Ncc 20 Ncc+3 ortho | Good response to bifocals | Need to continue wearing bifocals | 35 | Dcc ortho Ncc 14 Ncc+3 ortho | 40 |
| 11 | F | 5 | Dcc 25 Ncc 25 | R − 0.50 L − 0.25 | 60 | BLRc 6.75 | 6 | Dcc 20 Ncc 35 | 5.7 | 12 | 15 | Dcc 2 ET Ncc 20 Ncc+3 2 ET | Good response to bifocals, later decompensated to basic ET | Underwent BMRc 5.00 | 43 | Dcc ortho Ncc ortho | 40 |
| 12 | M | 4 | Dcc 40 Ncc 40 | R − 6.86 L−5.63 | 140 | BLRc 8.25 | 16 | Dcc 10 Ncc 50 | 13.3 | 18 | 20 | Dcc 20 ET Ncc 50 ET Ncc+3 20 ET | Partially corrected by bifocals | Underwent BMRc 5.00 | 45 | Dcc ortho Ncc ortho | 140 |
| 13 | F | 7 | Dcc 20 Ncc 25 | R − 0.75 L − 0.75 | 100 | BLRc 6.25 | 1 | Dcc 20 Ncc 35 | 4.0 | 27 | 2 | Dcc 16 Ncc 30 Ncc+3 10 | Partially corrected by bifocals | Underwent BMRc 5.25 | 31 | Dcc ortho Ncc ortho | 80 |
| 14 | M | 4 | Dcc 25 Ncc 30 | R + 0.25 L − 0.25 | 400 | BLRc 7.25 | 4 | Dcc 25 Ncc 35 | 5.7 | 39 | 4 | Dcc 10 ET Ncc 25 ET Ncc+3 10 ET | Partially corrected by bifocals | Need to continue wearing bifocals | 43 | Dcc 8 ET Ncc 20 ET Ncc+3 6 ET | 50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, B.J.; Lim, H.T. High Accommodative Convergence/Accommodation Ratio Consecutive Esotropia Following Surgery for Intermittent Exotropia: Clinical Feature, Diagnosis, and Treatment. J. Clin. Med. 2021, 10, 2135. https://doi.org/10.3390/jcm10102135
Lee BJ, Lim HT. High Accommodative Convergence/Accommodation Ratio Consecutive Esotropia Following Surgery for Intermittent Exotropia: Clinical Feature, Diagnosis, and Treatment. Journal of Clinical Medicine. 2021; 10(10):2135. https://doi.org/10.3390/jcm10102135
Chicago/Turabian StyleLee, Byung Joo, and Hyun Taek Lim. 2021. "High Accommodative Convergence/Accommodation Ratio Consecutive Esotropia Following Surgery for Intermittent Exotropia: Clinical Feature, Diagnosis, and Treatment" Journal of Clinical Medicine 10, no. 10: 2135. https://doi.org/10.3390/jcm10102135
APA StyleLee, B. J., & Lim, H. T. (2021). High Accommodative Convergence/Accommodation Ratio Consecutive Esotropia Following Surgery for Intermittent Exotropia: Clinical Feature, Diagnosis, and Treatment. Journal of Clinical Medicine, 10(10), 2135. https://doi.org/10.3390/jcm10102135






