Myocardial Injury in COVID-19 Patients: Association with Inflammation, Coagulopathy and In-Hospital Prognosis
Abstract
:1. Introduction
2. Materials and Methods
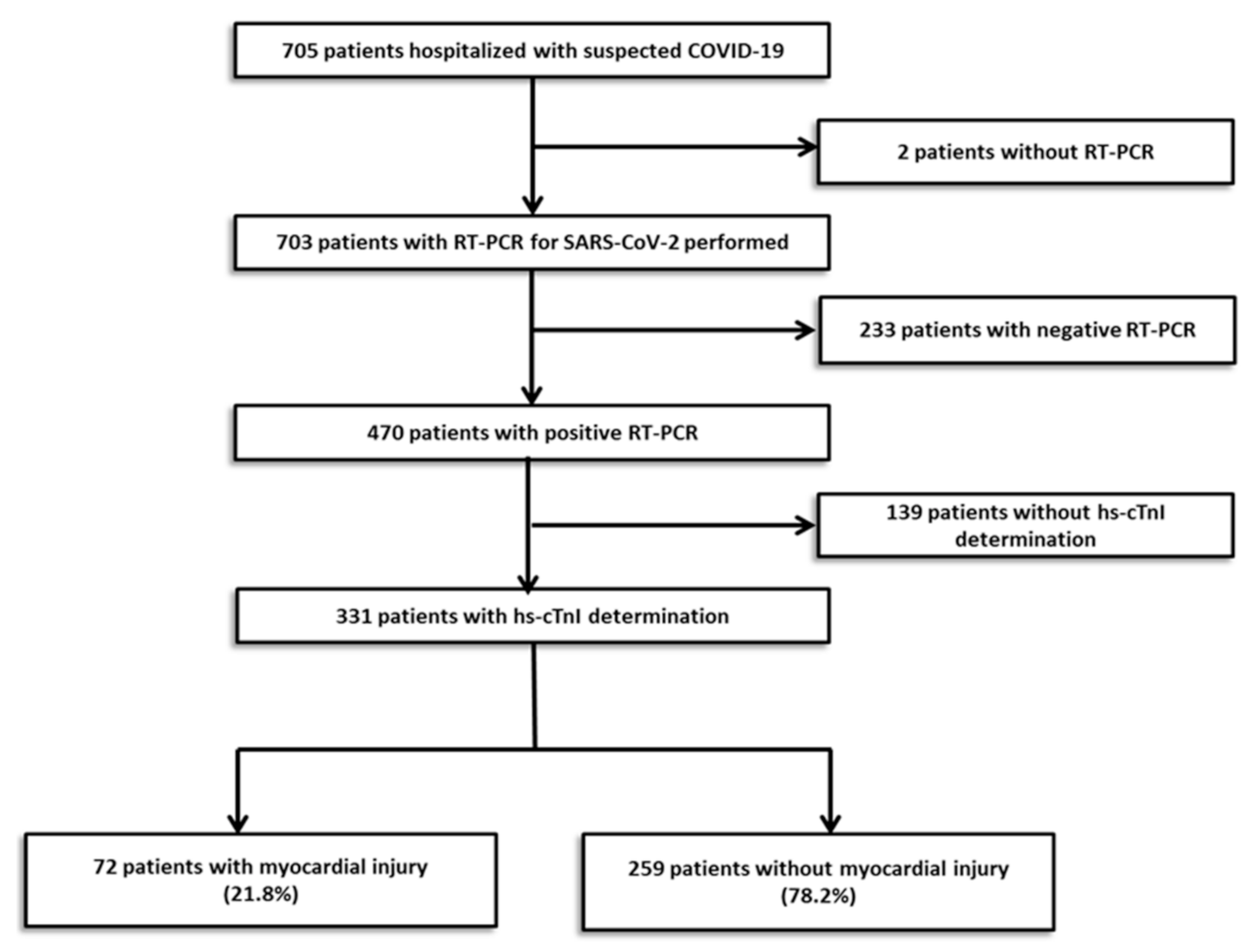
2.1. Study Design and Participants
2.2. Data Collection
2.3. Definitions
- Prolonged PT at least 25%,
- Platelets count lower than 100 × 109/L,
- Fibrinogen lower than 2 g/dL,
- Increased D-dimer more than four times the normal value (500 ng/mL) [10].
2.4. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Inflammation and Coagulopathy
3.3. In-Hospital Outcomes
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, C.L.; Qiu, X.; Zeng, Y.K.; Jiang, M.; Fan, H.R.; Zhang, Z.M. Coronavirus Disease 2019: A Clinical Review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 4585–4596. [Google Scholar] [CrossRef]
- Bourgonje, A.R.; Abdulle, A.E.; Timens, W.; Hillebrands, J.; Bourgonje, A.R.; Abdulle, A.E.; Timens, W.; Hillebrands, J. Angiotensin-converting enzyme 2 (ACE2), SARS-CoV-2 and the pathophysiology of coronavirus disease 2019 (COVID-19). J. Pathol. 2019, 251, 228–248. [Google Scholar] [CrossRef]
- Driggin, E.; Madhavan, M.V.; Bikdeli, B.; Chuich, T.; Laracy, J.; Biondi-Zoccai, G.; Brown, T.S.; Der Nigoghossian, C.; Zidar, D.A.; Haythe, J.; et al. Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems during the COVID-19 Pandemic. J. Am. Coll. Cardiol. 2020, 75, 2352–2371. [Google Scholar] [CrossRef]
- Nie, S.; Yu, M.; Xie, T.; Yang, F.; Wang, H.; Wang, Z.; Li, M.; Gao, X.; Lv, B.; Wang, S.; et al. Cardiac Troponin I Is an Independent Predictor for Mortality in Hospitalized Patients with Coronavirus Disease 2019. Circulation 2020, 142, 608–610. [Google Scholar] [CrossRef]
- Shi, S.; Qin, M.; Shen, B.; Cai, Y.; Liu, T.; Yang, F.; Gong, W.; Liu, X.; Liang, J.; Zhao, Q.; et al. Association of Cardiac Injury with Mortality in Hospitalized Patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020, 5, 802–810. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Toraih, E.A.; Elshazli, R.M.; Hussein, M.H.; Elgaml, A.; Amin, M.N.; El-Mowafy, M.; El-Mesery, M.; Ellythy, A.; Duchesne, J.; Killackey, M.T.; et al. Association of Cardiac Biomarkers and Comorbidities with Increased Mortality, Severity, and Cardiac Injury in COVID-19 Patients: A Meta-regression and Decision Tree Analysis. J. Med. Virol. 2020, 92, 2473–2488. [Google Scholar] [CrossRef] [PubMed]
- Bavishi, C.; Bonow, R.O.; Trivedi, V.; Abbott, J.D.; Messerli, F.H.; Bhatt, D.L. Acute Myocardial Injury in Patients Hospitalized with COVID-19 Infection: A Review. Prog. Cardiovasc. Dis. 2020, 63, 682–689. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Mickley, H.; Crea, F.; Van De Werf, F.; et al. Fourth Universal Definition of Myocardial Infarction (2018). Eur. Heart J. 2019, 40, 237–269. [Google Scholar] [CrossRef] [Green Version]
- Charlson, M.; Szatrowsky, T.P.; Peterson, J.; Gold, J. Validation of a Combined Comorbidity Index. Clin. Epidemiol. 1994, 47, 1245–1251. [Google Scholar] [CrossRef]
- Thachil, J.; Tang, N.; Gando, S.; Levi, M.; Clark, C.; Iba, T.; Falanga, A.; Cattaneo, M. ISTH Interim Guidance on Recognition and Management of Coagulopathy in COVID-19. J. Thromb. Haemost. 2020, 18, 1023–1026. [Google Scholar] [CrossRef]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized Bleeding Definitions for Cardiovascular Clinical Trials: A Consensus Report from the Bleeding Academic Research Consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gebhard, C.; Regitz-zagrosek, V.; Neuhauser, H.K.; Morgan, R.; Klein, S.L. Impact of Sex and Gender on COVID-19 Outcomes in Europe. Biol. Sex Differ. 2020, 11, 1–13. [Google Scholar] [CrossRef]
- Denmark, I. Charlson Comorbidity Index Score and Risk of Severe Outcome and Death in Danish COVID-19 Patients. J. Gen. Intern. Med. 2020, 35, 2801–2803. [Google Scholar] [CrossRef]
- Wan, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China. JAMA Cardiol. 2020, 323, 1061–1069. [Google Scholar] [CrossRef]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical Features of Patients Infected with 2019 Novel Coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef] [Green Version]
- Tang, N.; Bai, H.; Chen, X.; Gong, J.; Li, D.; Sun, Z. Anticoagulant Treatment Is Associated with Decreased Mortality in Severe Coronavirus Disease 2019 Patients with Coagulopathy. J. Thromb. Haemost. 2020, 1094–1099. [Google Scholar] [CrossRef] [PubMed]
- Guo, T.; Fan, Y.; Chen, M.; Wu, X.; Zhang, L.; He, T.; Wang, H.; Wan, J.; Wang, X.; Lu, Z. Cardiovascular Implications of Fatal Outcomes of Patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Chen, L.; Li, X. The ACE2 Expression in Human Heart Indicates New Potential Mechanism of Heart Injury among Patients Infected with SARS-CoV-2. Cardiovasc. Res. 2020, 116, 1097–1100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varga, Z.; Flammer, A.J.; Steiger, P.; Haberecker, M.; Andermatt, R.; Zinkernagel, A.S.; Mehra, M.R.; Schuepbach, R.A.; Ruschitzka, F.; Moch, H. Endothelial Cell Infection and Endotheliitis in COVID-19. Lancet 2020, 395, 1417–1418. [Google Scholar] [CrossRef]
- García, L.F. Immune Response, Inflammation, and the Clinical Spectrum of COVID-19. Front. Immunol. 2020, 11, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Merad, M.; Martin, J.C. Pathological Inflammation in Patients with COVID-19: A Key Role for Monocytes and Macrophages. Nat. Rev. Immunol. 2020, 20, 355–362. [Google Scholar] [CrossRef]
- Franchini, M.; Marano, G.; Cruciani, M.; Mengoli, C.; Pati, I.; Masiello, F.; Veropalumbo, E.; Pupella, S.; Vaglio, S. COVID-19-Associated Coagulopathy. Diagnosis 2020, 50, 54–67. [Google Scholar] [CrossRef]
- Ortega-Paz, L.; Capodanno, D.; Montalescot, G.; Angiolillo, D.J. COVID-19 Associated Thrombosis and Coagulopathy: Review of the Pathophysiology and Implications for Antithrombotic Management. J. Am. Heart Assoc. 2020. [Google Scholar] [CrossRef]
- Becker, R.C. COVID-19 Update: Covid-19—Associated Coagulopathy. J. Thromb. Thrombolysis 2020, 50, 54–67. [Google Scholar] [CrossRef]
- Luan, Y.; Liu, Y.; Liu, X.; Yu, B.; Chen, R.; Peng, M.; Ren, D. Coronavirus Disease 2019 (COVID-19) Associated Coagulopathy and Its Impact on Outcomes in Shenzhen, China: A Retrospective Cohort Study. Thromb. Res. 2020, 195, 62–68. [Google Scholar] [CrossRef] [PubMed]
- Miesbach, W.; Makris, M. COVID-19: Coagulopathy, Risk of Thrombosis, and the Rationale for Anticoagulation. Clin. Appl. Thromb. Hemost. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ayerbe, L.; Risco, C.; Ayis, S. The Association between Treatment with Heparin and Survival in Patients with Covid-19. J. Thromb. Thrombolysis 2020, 50, 298–301. [Google Scholar] [CrossRef]
- Paranjpe, I.; Fuster, V.; Lala, A.; Russak, A.J.; Glicksberg, B.S.; Levin, M.; Charney, A.; Narula, J.; Fayad, Z.A.; Bagiella, E. Association of Treatment Dose In-Hospital Survival Among Hospitalized Patients With COVID-19. J. Am. Coll. Cardiol. 2020, 76, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Lemos, A.C.B.; do Espírito Santo, D.A.; Salvetti, M.C.; Gilio, R.N.; Agra, L.B.; Pazin-Filho, A.; Miranda, C.H. Therapeutic versus Prophylactic Anticoagulation for Severe COVID-19: A Randomized Phase II Clinical Trial (HESACOVID). Thromb. Res. 2020, 196, 359–366. [Google Scholar] [CrossRef] [PubMed]
- Khan, I.H.; Savarimuthu, S.; Leung, M.S.T.; Harky, A. The Need to Manage the Risk of Thromboembolism in COVID-19 Patients. J. Vasc. Surg. 2020, 72, 799–804. [Google Scholar] [CrossRef]
- Atallah, B.; Mallah, S.I.; AlMahmeed, W. Anticoagulation in COVID-19. Eur. Heart J. Cardiovasc. Pharmacother. 2020, 6, 260–261. [Google Scholar] [CrossRef] [PubMed]
| Myocardial Injury | p-Value | ||
|---|---|---|---|
| With (n = 72) | Without (n = 259) | ||
| Characteristic | |||
| Age (years), mean ± SD | 75 ± 11 | 61 ± 17 | 0.001 |
| Male sex, n (%) | 50 (69.4) | 145 (56.0) | 0.043 |
| BMI, median (IQR) | 28.6 (25.8–30.4) | 27.0 (24.2–29.8) | 0.071 |
| Current smoker, n (%) | 2 (2.8) | 7 (2.7) | 1.000 |
| Diabetes, n (%) | 28 (38.9) | 39 (15.1) | 0.001 |
| Hypertension, n (%) | 54 (75.0) | 107 (41.3) | 0.001 |
| Hypercholesterolemia, n (%) | 33 (45.8) | 70 (27.0) | 0.004 |
| Chronic kidney disease, n (%) | 34 (47.2) | 35 (13.5) | 0.001 |
| Hemodialysis, n (%) | 4 (5.6) | 2 (0.8) | 0.022 |
| Atrial fibrillation, n (%) | 7 (9.7) | 13 (5.0) | 0.161 |
| Previous stroke or TIA, n (%) | 10 (13.9) | 6 (2.3) | 0.001 |
| Previous AMI, n (%) | 11 (15.3) | 8 (3.1) | 0.001 |
| Previous PCI, n (%) | 14 (19.4) | 10 (3.9) | 0.001 |
| Previous CABG, n (%) | 4 (5.6) | 2 (0.8) | 0.022 |
| Previous PVD, n (%) | 5 (16.7) | 2 (2.2) | 0.001 |
| Previous COPD or Asthma, n (%) | 11 (15.3) | 32 (12.4) | 0.553 |
| Previous pneumonia, n (%) | 3 (4.2) | 3 (3.5) | 0.732 |
| Previous heart failure, n (%) | 12 (16.7) | 10 (3.9) | 0.001 |
| Previous bleeding | 9 (12.5) | 9 (3.5) | 0.006 |
| LVEF, mean ± SD | 53 ± 9 | 57 ± 8 | 0.106 |
| Previous PE, n (%) | 2 (2.8) | 3 (1.2) | 0.299 |
| Active cancer, n (%) | 10 (13.9) | 12 (4.6) | 0.013 |
| Organ transplant, n (%) | 3 (4.2) | 9 (3.5) | 0.728 |
| Charlson Comorbidity Index, median (IQR) | 5 (4–7) | 2 (1–4) | 0.001 |
| Anticoagulation | |||
| Any anticoagulants, n (%) | 57 (79.2) | 229 (88.4) | 0.051 |
| LMWH | 58 (81.0) | 225 (87.0) | 0.178 |
| DOAC | 0 | 4 (1.5) | 0.580 |
| Prophylactic indication | 46 (80.7) | 203 (88.6) | 0.001 |
| Biomarkers | Myocardial Injury | p-Value | |
|---|---|---|---|
| With (n = 72) | Without (n = 259) | ||
| NT-ProBNP (pg/mL), Median (IQR) a | 3009 (1288–4523) | 409 (156 –1486) | 0.001 |
| Hemoglobin (g/L), Median (IQR) b | 105 (84 –119) | 121 (109 –134) | 0.001 |
| Creatinine (mg/dL), Median (IQR) a | 2.02 (1.32–3.69) | 0.95 (0.77–1.19) | 0.001 |
| Lymphocytes (109/L), Median (IQR) b | 0.3 (0.2–0.5) | 0.65 (0.40–1.0) | 0.001 |
| CRP (mg/dL), Median (IQR) a | 18.3 (9.6–25.9) | 12.0 (5.4–19.4) | 0.001 |
| Creatinine (mg/dL), Median (IQR) a | 2.02 (1.32–3.69) | 0.95 (0.77–1.19) | 0.001 |
| Thrombotic biomarkers | |||
| D-dimer (ng/mL), Median (IQR) a | 4250 (1500–8600) | 1700 (800–4300) | 0.001 |
| PT (segundos), Median (IQR) a | 14.7 (13.4–17.3) | 13.1 (12.3–14.0) | 0.001 |
| Platelets (109/L), Median (IQR) b | 138 (95–189) | 171 (134–215) | 0.001 |
| Fibrinogen (g/L), Median (IQR) b | 3.40 (2.4–6.0) | 4.0 (2.8–5.8) | 0.512 |
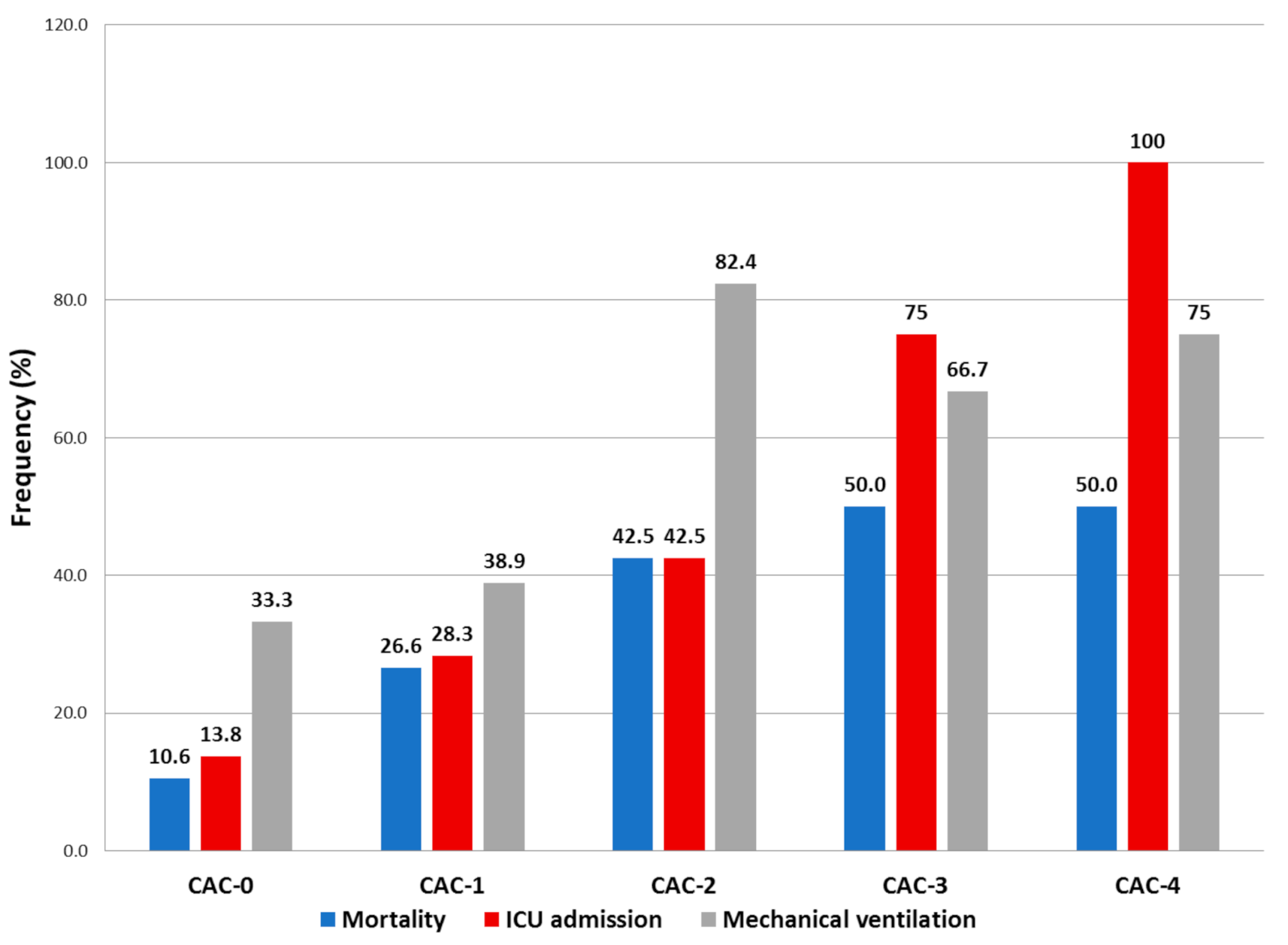
| CAC | |||
| CAC score, median (IQR) | 1 (0–2) | 0 (0–1) | 0.001 |
| CAC 0 feature, n(%) | 20 (27.8) | 131 (50.6) | 0.001 |
| CAC 1 feature, n(%) | 25 (34.7) | 103 (39.8) | |
| CAC 2 feature, n(%) | 19 (26.4) | 21 (8.1) | |
| CAC 3 feature, n(%) | 5 (6.9) | 3 (1.2) | |
| CAC 4 feature, n(%) | 3 (4.2) | 1 (0.4) | |
| Myocardial Injury | p-Value | ||
|---|---|---|---|
| With (n = 72) | Without (n = 259) | ||
| Hospitalization days, mean ± SD | 15.3 ± 12.9 | 15.85 ± 9.0 | 0.751 |
| Need for ICU, n (%) | 25 (34.7) | 58 (22.4) | 0.046 |
| UCI days, mean ± SD | 12.5 ± 9.6 | 7.9 ± 5.3 | 0.032 |
| Invasive mechanical ventilation, n (%) | 21 (29.1) | 21 (8.1) | 0.001 |
| Need for vasoactive drugs, n (%) | 20 (27.8) | 29 (11.2) | 0.001 |
| Need for IMV, n (%) | 4 (5.6) | 5 (1.9) | 0.107 |
| ACS, n (%) | 10 (13.9) | 0 | 0.001 |
| NSTEMI | 8 (11.1) | 0 | |
| STEMI | 2 (2.8) | 0 | |
| Stroke, n (%) | 0 (0) | 1 (0.4) | 1.000 |
| Ischemic | 0 | 1 (0.4) | |
| DVT, n (%) | 2 (2.8) | 2 (0.8) | 0.207 |
| PE, n (%) | 3 (4.2) | 14 (5.4) | 1.000 |
| Bleeding, n (%) | 8 (11.1) | 3 (1.2) | 0.001 |
| Red blood cell transfusion, n (%) * | 18 (25) | 6 (2.3) | 0.001 |
| Cardiac arrhythmias, n (%) ** | 8 (11.1) | 0 (0) | 0.001 |
| All-cause mortality, n (%) | 48 (66.7) | 25 (9.7) | 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arévalos, V.; Ortega-Paz, L.; Rodríguez-Arias, J.J.; Calvo, M.; Castrillo, L.; Salazar, A.; Roque, M.; Dantas, A.P.; Sabaté, M.; Brugaletta, S. Myocardial Injury in COVID-19 Patients: Association with Inflammation, Coagulopathy and In-Hospital Prognosis. J. Clin. Med. 2021, 10, 2096. https://doi.org/10.3390/jcm10102096
Arévalos V, Ortega-Paz L, Rodríguez-Arias JJ, Calvo M, Castrillo L, Salazar A, Roque M, Dantas AP, Sabaté M, Brugaletta S. Myocardial Injury in COVID-19 Patients: Association with Inflammation, Coagulopathy and In-Hospital Prognosis. Journal of Clinical Medicine. 2021; 10(10):2096. https://doi.org/10.3390/jcm10102096
Chicago/Turabian StyleArévalos, Victor, Luis Ortega-Paz, Juan José Rodríguez-Arias, Margarita Calvo, Leticia Castrillo, Anthony Salazar, Merce Roque, Ana Paula Dantas, Manel Sabaté, and Salvatore Brugaletta. 2021. "Myocardial Injury in COVID-19 Patients: Association with Inflammation, Coagulopathy and In-Hospital Prognosis" Journal of Clinical Medicine 10, no. 10: 2096. https://doi.org/10.3390/jcm10102096
APA StyleArévalos, V., Ortega-Paz, L., Rodríguez-Arias, J. J., Calvo, M., Castrillo, L., Salazar, A., Roque, M., Dantas, A. P., Sabaté, M., & Brugaletta, S. (2021). Myocardial Injury in COVID-19 Patients: Association with Inflammation, Coagulopathy and In-Hospital Prognosis. Journal of Clinical Medicine, 10(10), 2096. https://doi.org/10.3390/jcm10102096






