Uterine Cervical Change at Term Examined Using Ultrasound Elastography: A Longitudinal Study
Abstract
1. Introduction
2. Materials and Methods
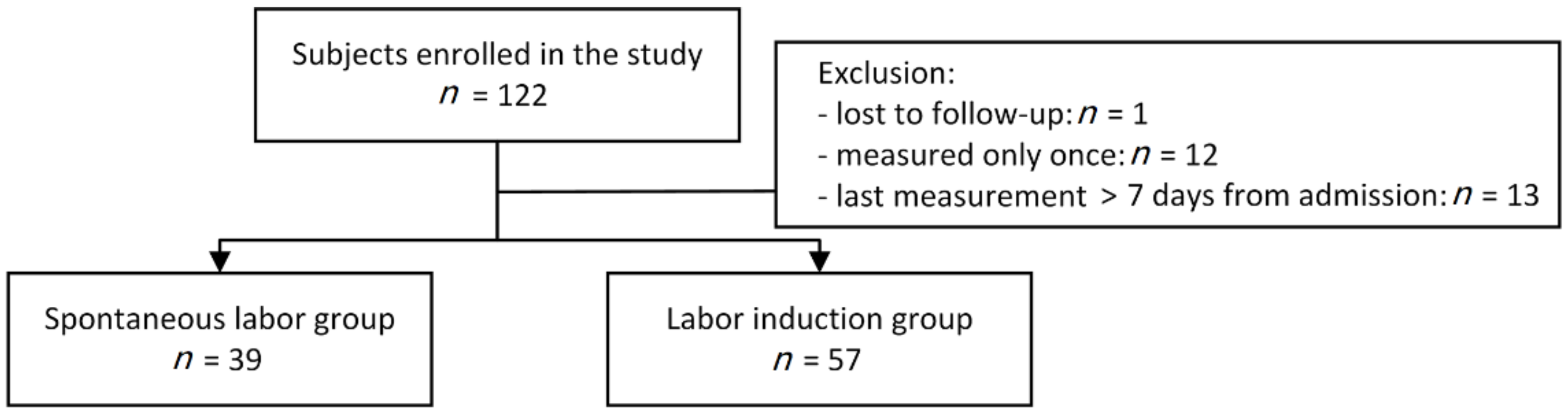
2.1. Subjects
2.2. Cervical Length and Elastographic Measurements
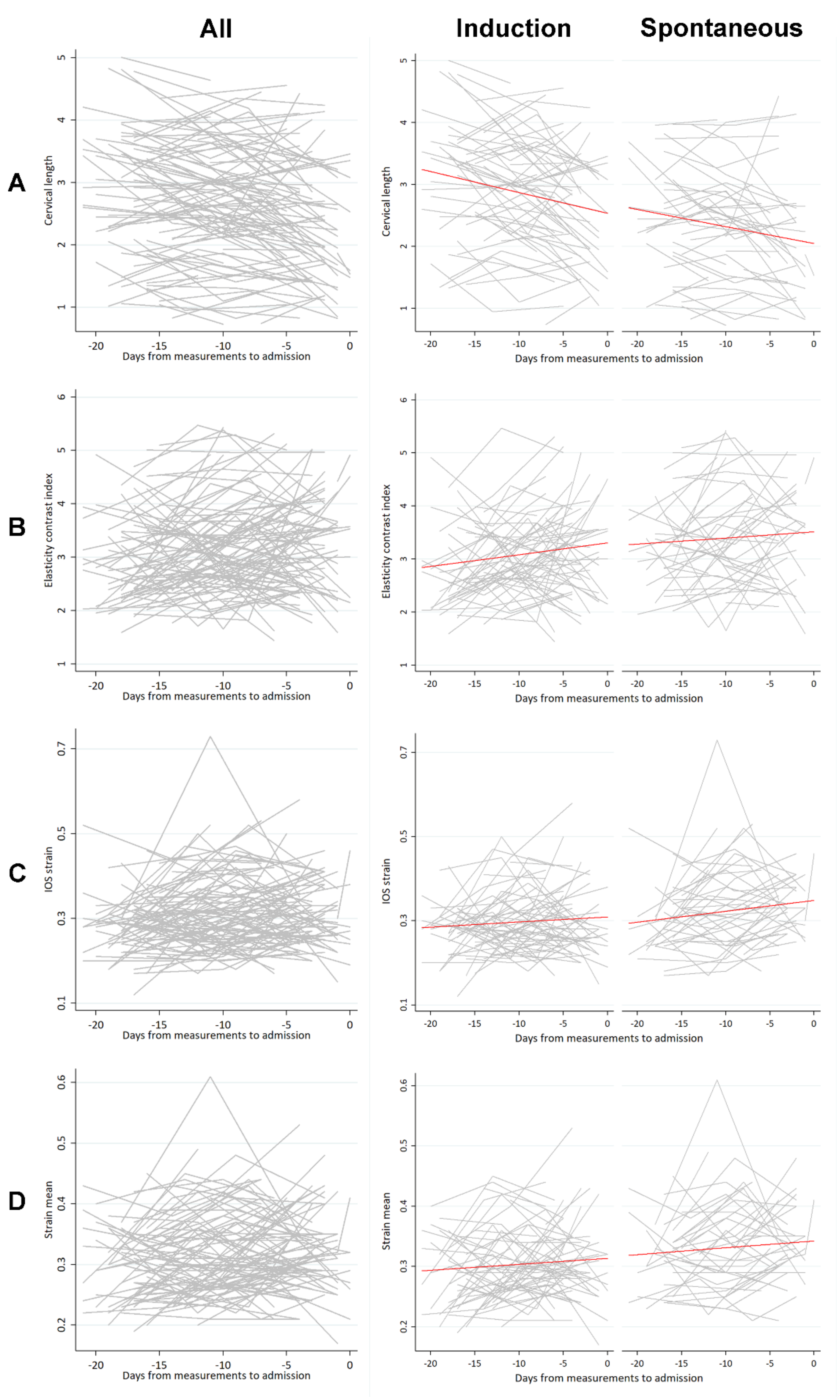
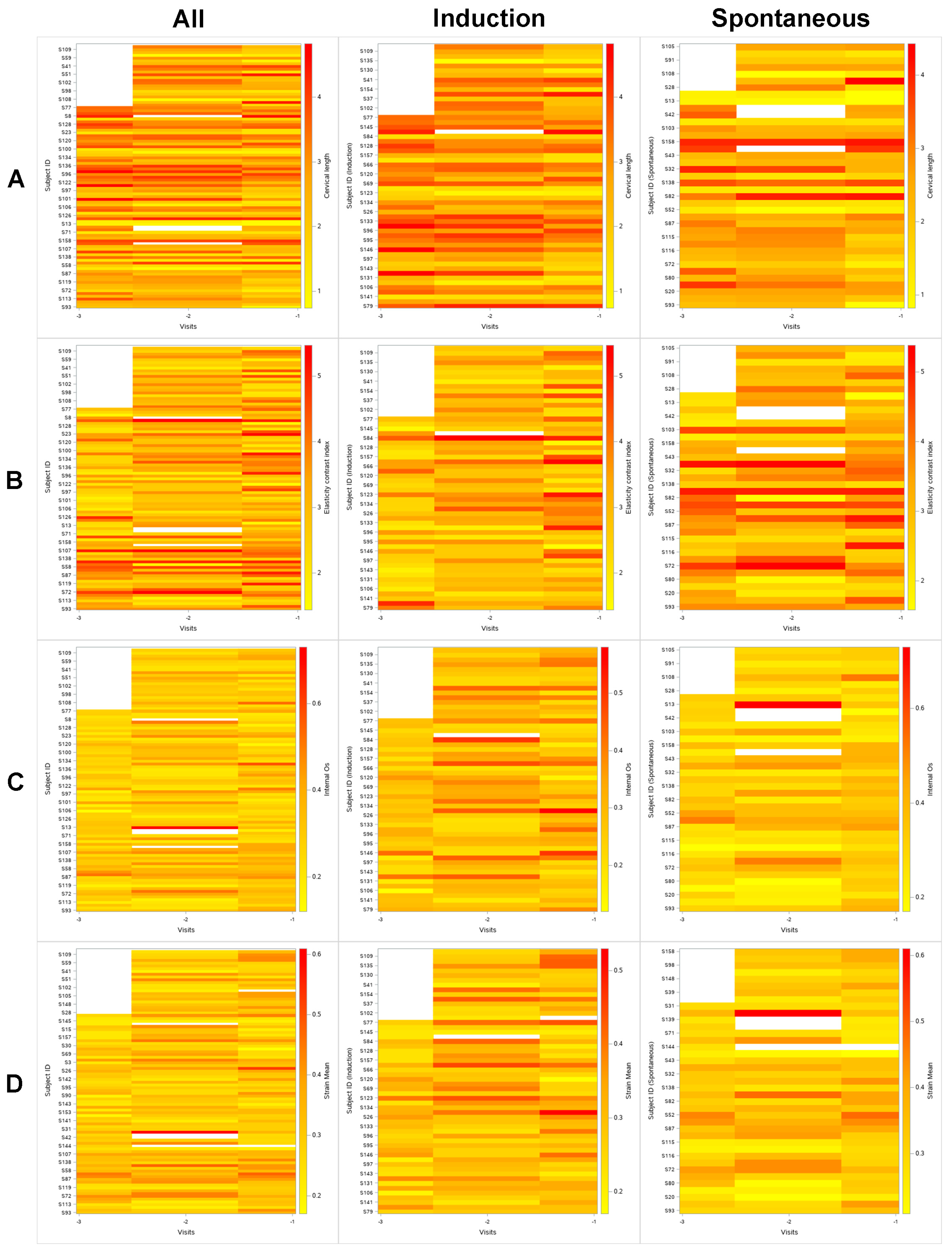
2.3. Plots and Regression Analysis
2.4. Other Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Yellon, S.M. Immunobiology of Cervix Ripening. Front. Immunol. 2019, 10, 3156. [Google Scholar] [CrossRef] [PubMed]
- Word, R.A.; Li, X.H.; Hnat, M.; Carrick, K. Dynamics of cervical remodeling during pregnancy and parturition: Mechanisms and current concepts. Semin. Reprod. Med. 2007, 25, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Iams, J.D.; Goldenberg, R.L.; Meis, P.J.; Mercer, B.M.; Moawad, A.; Das, A.; Thom, E.; McNellis, D.; Copper, R.L.; Johnson, F.; et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N. Engl. J. Med. 1996, 334, 567–572. [Google Scholar] [CrossRef] [PubMed]
- Kuusela, P.; Wennerholm, U.B.; Fadl, H.; Wesstrom, J.; Lindgren, P.; Hagberg, H.; Jacobsson, B.; Valentin, L. Second trimester cervical length measurements with transvaginal ultrasound: A prospective observational agreement and reliability study. Acta Obstet. Gynecol. Scand. 2020, 99, 1476–1485. [Google Scholar] [CrossRef]
- Valentin, L.; Bergelin, I. Intra- and interobserver reproducibility of ultrasound measurements of cervical length and width in the second and third trimesters of pregnancy. Ultrasound Obstet. Gynecol. 2002, 20, 256–262. [Google Scholar] [CrossRef]
- Hernandez-Andrade, E.; Romero, R.; Ahn, H.; Hussein, Y.; Yeo, L.; Korzeniewski, S.J.; Chaiworapongsa, T.; Hassan, S.S. Transabdominal evaluation of uterine cervical length during pregnancy fails to identify a substantial number of women with a short cervix. J. Matern. Fetal Neonatal Med. 2012, 25, 1682–1689. [Google Scholar] [CrossRef]
- Kuwata, T.; Matsubara, S.; Taniguchi, N.; Ohkuchi, A.; Ohkusa, T.; Suzuki, M. A novel method for evaluating uterine cervical consistency using vaginal ultrasound gray-level histogram. J. Perinat. Med. 2010, 38, 491–494. [Google Scholar] [CrossRef]
- Tekesin, I.; Hellmeyer, L.; Heller, G.; Romer, A.; Kuhnert, M.; Schmidt, S. Evaluation of quantitative ultrasound tissue characterization of the cervix and cervical length in the prediction of premature delivery for patients with spontaneous preterm labor. Am. J. Obstet. Gynecol. 2003, 189, 532–539. [Google Scholar] [CrossRef]
- Banos, N.; Perez-Moreno, A.; Julia, C.; Murillo-Bravo, C.; Coronado, D.; Gratacos, E.; Deprest, J.; Palacio, M. Quantitative analysis of cervical texture by ultrasound in mid-pregnancy and association with spontaneous preterm birth. Ultrasound Obstet. Gynecol. 2018, 51, 637–643. [Google Scholar] [CrossRef]
- Sigrist, R.M.S.; Liau, J.; Kaffas, A.E.; Chammas, M.C.; Willmann, J.K. Ultrasound Elastography: Review of Techniques and Clinical Applications. Theranostics 2017, 7, 1303–1329. [Google Scholar] [CrossRef]
- Swiatkowska-Freund, M.; Preis, K. Cervical elastography during pregnancy: Clinical perspectives. Int. J. Womens Health 2017, 9, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Papillon-Smith, J.; Abenhaim, H.A. The role of sonographic cervical length in labor induction at term. J. Clin. Ultrasound 2015, 43, 7–16. [Google Scholar] [CrossRef] [PubMed]
- Glover, A.V.; Manuck, T.A. Screening for spontaneous preterm birth and resultant therapies to reduce neonatal morbidity and mortality: A review. Semin. Fetal Neonatal Med. 2018, 23, 126–132. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Lin, M.F.; Wu, L.H.; Zhang, L.H.; Zheng, Q.; Gu, Y.J.; Xie, H.N. Quantitative elastography of cervical stiffness during the three trimesters of pregnancy with a semiautomatic measurement program: A longitudinal prospective pilot study. J. Obstet. Gynaecol. Res. 2020, 46, 237–248. [Google Scholar] [CrossRef] [PubMed]
- Kwak, D.W.; Kim, M.; Oh, S.Y.; Park, H.S.; Kim, S.J.; Kim, M.Y.; Hwang, H.S. Reliability of strain elastography using in vivo compression in the assessment of the uterine cervix during pregnancy. J. Perinat. Med. 2020, 48, 256–265. [Google Scholar] [CrossRef]
- Park, H.S.; Kwon, H.; Kwak, D.W.; Kim, M.Y.; Seol, H.J.; Hong, J.S.; Shim, J.Y.; Choi, S.K.; Hwang, H.S.; Oh, M.J.; et al. Addition of Cervical Elastography May Increase Preterm Delivery Prediction Performance in Pregnant Women with Short Cervix: A Prospective Study. J. Korean Med. Sci. 2019, 34, e68. [Google Scholar] [CrossRef]
- Seol, H.J.; Sung, J.H.; Seong, W.J.; Kim, H.M.; Park, H.S.; Kwon, H.; Hwang, H.S.; Jung, Y.J.; Kwon, J.Y.; Oh, S.Y. Standardization of measurement of cervical elastography, its reproducibility, and analysis of baseline clinical factors affecting elastographic parameters. Obstet. Gynecol. Sci. 2020, 63, 42–54. [Google Scholar] [CrossRef]
- Swihart, B.J.; Caffo, B.; James, B.D.; Strand, M.; Schwartz, B.S.; Punjabi, N.M. Lasagna plots: A saucy alternative to spaghetti plots. Epidemiology 2010, 21, 621–625. [Google Scholar] [CrossRef]
- Fitzmaurice, G.M.; Laird, N.M.; Ware, J.H. Applied Longitudinal Analysis, 2nd ed.; Wiley: Hoboken, NJ, USA, 2011; pp. 144–145. [Google Scholar]
- Hernandez-Andrade, E.; Garcia, M.; Ahn, H.; Korzeniewski, S.J.; Saker, H.; Yeo, L.; Chaiworapongsa, T.; Hassan, S.S.; Romero, R. Strain at the internal cervical os assessed with quasi-static elastography is associated with the risk of spontaneous preterm delivery at ≤34 weeks of gestation. J. Perinat. Med. 2015, 43, 657–666. [Google Scholar] [CrossRef]
- Wozniak, S.; Czuczwar, P.; Szkodziak, P.; Milart, P.; Wozniakowska, E.; Paszkowski, T. Elastography in predicting preterm delivery in asymptomatic, low-risk women: A prospective observational study. BMC Pregnancy Childbirth 2014, 14, 238. [Google Scholar] [CrossRef]
- Wozniak, S.; Czuczwar, P.; Szkodziak, P.; Wrona, W.; Paszkowski, T. Elastography for predicting preterm delivery in patients with short cervical length at 18–22 weeks of gestation: A prospective observational study. Ginekol. Pol. 2015, 86, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Meath, A.J.; Ramsey, P.S.; Mulholland, T.A.; Rosenquist, R.G.; Lesnick, T.; Ramin, K.D. Comparative longitudinal study of cervical length and induced shortening changes among singleton, twin, and triplet pregnancies. Am. J. Obstet. Gynecol. 2005, 192, 1410–1415. [Google Scholar] [CrossRef] [PubMed]
- Cunningham, F.G. Williams Obstetrics, 25th ed.; McGraw-Hill: New York, NY, USA, 2018; pp. 400–420. [Google Scholar]

| Measurement Parameter | Description |
|---|---|
| ECI | ECI score within the ROI, value range: 0 (homogeneity)–81 (heterogeneity) |
| IOS strain mean level | Standardized strain mean level in 1 cm circle of IOS, value range: 0 (hard)–1 (soft) |
| EOS strain mean level | Standardized strain mean level in 1 cm circle of EOS, value range: 0 (hard)–1 (soft) |
| Ratio (IOS/EOS) | IOS strain level/EOS strain level |
| Strain mean level | Strain mean level within the ROI, value range: 0 (hard)–1 (soft) |
| Hardness ratio | 30-percentile hardness area ratio within the ROI, value range: 0% (soft)–100% (hard) |
| Spontaneous Labor n = 39 | Labor Induction n = 57 | p-Value | |
|---|---|---|---|
| Maternal age | 32.00 (29.00–35.00) | 33.00 (31.00–36.00) | 0.067 |
| History of abortion | 6 (15.38%) | 15 (26.32%) | 0.220 |
| History of CIN | 2 (5.13%) | 2 (3.51%) | 1.000 |
| History of LEEP | 1 (2.56%) | 1 (1.75%) | 1.000 |
| IVF-ET | 7 (17.95%) | 13 (22.81%) | 0.620 |
| pre-pregnancy BMI | 21.77 (20.32–23.50) | 21.30 (19.71–23.44) | 0.480 |
| Smoking | 1 (2.56%) | 2 (3.51%) | 1.000 |
| Hypertensive diseases | 0 (0.00%) | 3 (5.26%) | 0.270 |
| GDM | 6 (15.38%) | 7 (12.28%) | 0.760 |
| Progesterone use | 2 (5.13%) | 1 (1.75%) | 0.560 |
| Maternal weight at delivery | 71.90 (64.70–76.50) | 70.30 (65.00–79.90) | 0.880 |
| GA at admission | 39.57 (39.14–40.29) | 39.71 (39.00–40.29) | 0.960 |
| GA at delivery | 39.57 (39.14–40.43) | 39.86 (39.14–40.43) | 0.630 |
| Cesarean delivery | 3 (7.69%) | 21 (36.84%) | 0.001 |
| Birthweight | 3244 (3000–3404) | 3340 (3110–3498) | 0.120 |
| NICU admission | 2 (5.13%) | 1 (1.79%) | 0.570 |
| Days from the Measurement to Admission (α1) in Equation (1) | SEM | p-Value | Days from the Measurement to Admission (ß1) in Equation (2) | SEM | p-Value | Labor Group (ß2) in Equation (2) | SEM | p-Value | |
|---|---|---|---|---|---|---|---|---|---|
| Cervical length | −0.02459 | 0.00483 | <0.001 | −0.02468 | 0.00483 | <0.001 | −0.4810 | 0.1692 | 0.0055 |
| ECI | 0.0175 | 0.00824 | 0.0363 | 0.01756 | 0.00824 | 0.0357 | 0.2872 | 0.1386 | 0.0442 |
| IOS strain mean level | 0.00159 | 0.00072 | 0.0284 | 0.001605 | 0.00072 | 0.0272 | 0.0318 | 0.0122 | 0.0105 |
| EOS strain mean level | 0.001 | 0.00074 | 0.1788 | 0.001033 | 0.00074 | 0.1673 | 0.03131 | 0.0133 | 0.0209 |
| IOS/EOS ratio | −0.0004 | 0.00279 | 0.8799 | −0.00041 | 0.0028 | 0.8831 | 0.02319 | 0.0418 | 0.5805 |
| Strain mean | 0.00113 | 0.00053 | 0.0353 | 0.001140 | 0.00053 | 0.0323 | 0.03204 | 0.0103 | 0.0025 |
| Hardness ratio | −0.2049 | 0.1142 | 0.0759 | −0.2084 | 0.1137 | 0.0699 | −6.3078 | 2.1683 | 0.0045 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, H.S.; Kwon, H.; Kwon, J.-Y.; Jung, Y.J.; Seol, H.-J.; Seong, W.J.; Kim, H.M.; Hwang, H.-S.; Sung, J.-H.; Oh, S.-y., on behalf of the Korean Consortium for the Study of Cervical Elastography in the Prediction of Preterm Delivery. Uterine Cervical Change at Term Examined Using Ultrasound Elastography: A Longitudinal Study. J. Clin. Med. 2021, 10, 75. https://doi.org/10.3390/jcm10010075
Park HS, Kwon H, Kwon J-Y, Jung YJ, Seol H-J, Seong WJ, Kim HM, Hwang H-S, Sung J-H, Oh S-y on behalf of the Korean Consortium for the Study of Cervical Elastography in the Prediction of Preterm Delivery. Uterine Cervical Change at Term Examined Using Ultrasound Elastography: A Longitudinal Study. Journal of Clinical Medicine. 2021; 10(1):75. https://doi.org/10.3390/jcm10010075
Chicago/Turabian StylePark, Hyun Soo, Hayan Kwon, Ja-Young Kwon, Yun Ji Jung, Hyun-Joo Seol, Won Joon Seong, Hyun Mi Kim, Han-Sung Hwang, Ji-Hee Sung, and Soo-young Oh on behalf of the Korean Consortium for the Study of Cervical Elastography in the Prediction of Preterm Delivery. 2021. "Uterine Cervical Change at Term Examined Using Ultrasound Elastography: A Longitudinal Study" Journal of Clinical Medicine 10, no. 1: 75. https://doi.org/10.3390/jcm10010075
APA StylePark, H. S., Kwon, H., Kwon, J.-Y., Jung, Y. J., Seol, H.-J., Seong, W. J., Kim, H. M., Hwang, H.-S., Sung, J.-H., & Oh, S.-y., on behalf of the Korean Consortium for the Study of Cervical Elastography in the Prediction of Preterm Delivery. (2021). Uterine Cervical Change at Term Examined Using Ultrasound Elastography: A Longitudinal Study. Journal of Clinical Medicine, 10(1), 75. https://doi.org/10.3390/jcm10010075






