Infectious Complications in Autoimmune Hemolytic Anemia
Abstract
1. Introduction
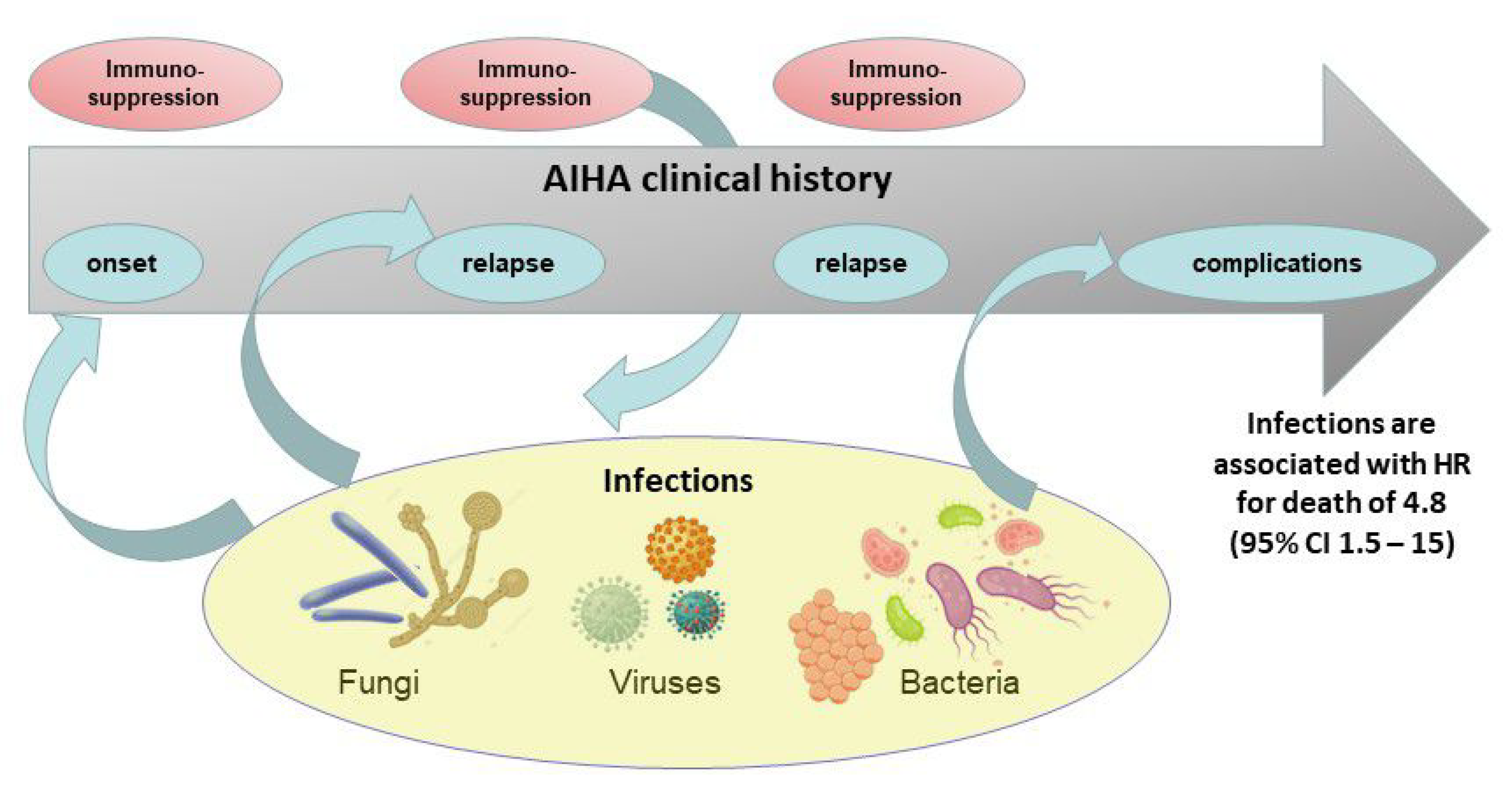
2. Prevalence of Infections in Primary AIHA
3. Infectious Risk Associated with AIHA Therapies
3.1. Steroids
3.2. Rituximab
3.3. Splenectomy
3.4. Immunosuppressive Agents
3.5. New Target Drugs
4. Viral and Mycobacterial Reactivations during AIHA Treatments
4.1. Hepatotropic Viruses
4.2. Herpesviruses
4.3. Tuberculosis
5. Prevention Strategies
5.1. HBV and HCV
5.2. Tuberculosis
5.3. Pneumocystis jirovecii
5.4. Herpesvirus Reactivations
5.5. Vaccinations
6. Infections in AIHA Secondary to Other Diseases
7. AIHA Secondary to Infections
8. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jäger, U.; Barcellini, W.; Broome, C.M.; Gertz, M.A.; Hill, A.; Hil, Q.A.; Jilma, B.; Kuter, D.J.; Michel, M.; Montillo, M.; et al. Diagnosis and treatment of autoimmune hemolytic anemia in adults: Recommendations from the First International Consensus Meeting. Blood Rev. 2020, 41, 100648. [Google Scholar] [CrossRef]
- Berentsen, S. How I manage patients with cold agglutinin disease. Br. J. Haematol. 2018, 181, 320–330. [Google Scholar] [CrossRef]
- Barcellini, W.; Fattizzo, B.; Zaninoni, A.; Radice, T.; Nichele, I.; Di Bona, E.; Lunghi, M.; Tassinari, C.; Alfinito, F.; Ferrari, A.; et al. Clinical heterogeneity and predictors of outcome in primary autoimmune hemolytic anemia: A GIMEMA study of 308 patients. Blood 2014, 124, 2930–2936. [Google Scholar] [CrossRef] [PubMed]
- Barcellini, W.; Zaninoni, A.; Fattizzo, B.; Giannotta, J.A.; Lunghi, M.; Ferrari, A.; Leporace, A.P.; Maschio, N.; Scaramucci, L.; Cantoni, S.; et al. Predictors of refractoriness to therapy and healthcare resource utilization in 378 patients with primary autoimmune hemolytic anemia from eight Italian reference centers. Am. J. Hematol. 2018, 93, E243–E246. [Google Scholar] [CrossRef]
- Prabhu, R.; Bhaskaran, R.; Shenoy, V.; Sidharthan, N. Clinical characteristics and treatment outcomes of primary autoimmune hemolytic anemia: A single center study from South India. Blood Res. 2016, 51, 88–94. [Google Scholar] [CrossRef]
- Giannotta, J.A.; Fattizzo, B.; Zaninoni, A.; Barcellini, W. Infectious Complications in a Cohort of Autoommune Haemolytic Anaemia Patients; Abstract, n. PB2401; EHA Learning Centre: Frankfurt, Germany, 2020. [Google Scholar]
- Genty, I.; Michel, M.; Hermine, O.; Schaeffer, A.; Godeau, B.; Rochant, H. Characteristics of autoimmune hemolytic anemia in adults: Retrospective analysis of 83 cases. Rev. Med. Interne 2002, 23, 901–909. [Google Scholar] [CrossRef]
- Roumier, M.; Loustau, V.; Guillaud, C.; Languille, L.; Mahevas, M.; Khellaf, M.; Limal, N.; Noizat-Pirenne, F.; Godeau, B.; Michel, M. Characteristics and outcome of warm autoimmune hemolytic anemia in adults: New insights based on a single-center experience with 60 patients. Am. J. Hematol. 2014, 89, E150–E155. [Google Scholar] [CrossRef]
- Rattarittamrong, E.; Eiamprapai, P.; Tantiworawit, A.; Rattanathammethee, T.; Hantrakool, S.; Chai-Adisaksopha, C.; Norasetthada, L. Clinical characteristics and long-term outcomes of warm-type autoimmune hemolytic anemia. Hematology 2016, 21, 368–374. [Google Scholar] [CrossRef]
- Fardet, L.; Petersen, I.; Nazareth, I. Common Infections in Patients Prescribed Systemic Glucocorticoids in Primary Care: A Population-Based Cohort Study. PLoS Med. 2016, 13, e1002024. [Google Scholar] [CrossRef]
- Dixon, W.G.; Suissa, S.; Hudson, M. The association between systemic glucocorticoid therapy and the risk of infection in patients with rheumatoid arthritis: Systematic review and meta-analyses. Arthritis Res. Ther. 2011, 13, R139. [Google Scholar] [CrossRef]
- Yang, Y.; Sang, J.; Pan, W.; Du, L.; Liao, W.; Chen, J.; Zhu, Y. Cryptococcal meningitis in patients with autoimmune hemolytic anemia. Mycopathologia 2014, 178, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Fattizzo, B.; Zaninoni, A.; Pettine, L.; Cavallaro, F.; Di Bona, E.; Barcellini, W. Low-dose rituximab in autoimmune hemolytic anemia: 10 years after. Blood 2019, 133, 996–998. [Google Scholar] [CrossRef] [PubMed]
- Bohra, C.; Sokol, L.; Dalia, S. Progressive Multifocal Leukoencephalopathy and Monoclonal Antibodies: A Review. Cancer Control 2017, 24, 1073274817729901. [Google Scholar] [CrossRef] [PubMed]
- MacIsaac, J.; Siddiqui, R.; Jamula, E.; Li, N.; Baker, S.; Webert, K.E.; Evanovitch, D.; Heddle, N.M.; Arnold, D.M. Systematic review of rituximab for autoimmune diseases: A potential alternative to intravenous immune globulin. Transfusion 2018, 58, 2729–2735. [Google Scholar] [CrossRef] [PubMed]
- Reynaud, Q.; Durieu, I.; Dutertre, M.; Ledochowski, S.; Durupt, S.; Michallet, A.-S.; Vital-Durand, D.; Lega, J.-C. Efficacy and safety of rituximab in auto-immune hemolytic anemia: A meta-analysis of 21 studies. Autoimmun. Rev. 2015, 14, 304–313. [Google Scholar] [CrossRef] [PubMed]
- Loomba, R.; Liang, T.J. Hepatitis B reactivation associated with immune suppressive and biological modifier therapies: Current concepts, management strategies, and future directions. Gastroenterology 2017, 152, 1297–1309. [Google Scholar] [CrossRef]
- Sinwar, P.D. Overwhelming post splenectomy infection syndrome—Review study. Int. J. Surg. 2014, 12, 1314–1316. [Google Scholar] [CrossRef]
- Ho, G.; Brunson, A.; Keegan, T.H.M.; Wun, T. Splenectomy and the incidence of venous thromboembolism and sepsis in patients with autoimmune hemolytic anemia. Blood Cells Mol. Dis. 2020, 81, 102388. [Google Scholar] [CrossRef]
- Singh, J.A.; Hossain, A.; Kotb, A.; Wells, G. Risk of serious infections with immunosuppressive drugs and glucocorticoids for lupus nephritis: A systematic review and network meta-analysis. BMC Med. 2016, 14, 137. [Google Scholar] [CrossRef]
- Colombo, D.; Chimenti, S.; Grossi, P.; Marchesoni, A.; Di Nuzzo, S.; Griseta, V.; Gargiulo, A.; Parodi, A.; Simoni, L.; Bellia, G. Prevalence of past and reactivated viral infections and efficacy of cyclosporine A as monotherapy or in combination in patients with psoriatic arthritis-synergy study: A longitudinal observational study. BioMed Res. Int. 2014, 2014, 941767. [Google Scholar] [CrossRef]
- Salama, A. Treatment Options for Primary Autoimmune Hemolytic Anemia: A Short Comprehensive Review. Transfus. Med. Hemother. 2015, 42, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Berentsen, S.; Hill, A.; Hill, Q.A.; Tvedt, T.H.A.; Michel, M. Novel insights into the treatment of complement-mediated hemolytic anemias. Ther. Adv. Hematol. 2019, 10, 2040620719873321. [Google Scholar] [CrossRef] [PubMed]
- Socié, G.; Caby-Tosi, M.P.; Marantz, J.L.; Cole, A.; Bedrosian, C.L.; Gasteyger, C.; Mujeebuddin, A.; Hillmen, P.; Vande Walle, J.; Haller, H. Eculizumab in paroxysmal nocturnal haemoglobinuria and atypical haemolytic uraemic syndrome: 10-year pharmacovigilance analysis. Br. J. Haematol. 2019, 185, 297–310. [Google Scholar] [CrossRef]
- Zinzani, P.L.; Rambaldi, A.; Gaidano, G.; Girmenia, C.; Marchetti, M.; Pane, F.; Tura, S.; Barosi, G. Infection control in patients treated for chronic lymphocytic leukemia with ibrutinib or idelalisib: Recommendations from Italian society of hematology. Leuk. Res. 2019, 81, 88–94. [Google Scholar] [CrossRef]
- Kunwar, S.; Devkota, A.R.; Ghimire, D.K. Fostamatinib, an oral spleen tyrosine kinase inhibitor, in the treatment of rheumatoid arthritis: A meta-analysis of randomized controlled trials. Rheumatol. Int. 2016, 36, 1077–1087. [Google Scholar] [CrossRef] [PubMed]
- Ratnasingam, S.; Walker, P.A.; Tran, H.; Kaplan, Z.S.; McFadyen, J.D.; Tran, H.; The, T.C.; Fleming, S.; Catalano, J.V.; Chunilal, S.D.; et al. Bortezomib-based antibody depletion for refractory autoimmune hematological diseases. Blood Adv. 2016, 1, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.; Gramegna, D.; Paoloni, F.; Fattizzo, B.; Binda, F.; D’Adda, M.; Farina, M.; Lucchini, E.; Mauro, F.R.; Salvi, F.; et al. Short course of bortezomib in anemic patients with relapsed cold agglutinin disease: A phase 2 prospective GIMEMA study. Blood 2018, 132, 547–550. [Google Scholar] [CrossRef] [PubMed]
- Newland, A.C.; Sánchez-González, B.; Rejtő, L.; Egyed, M.; Romanyuk, N.; Godar, M.; Verschueren, K.; Gandini, D.; Ulrichts, P.; Beauchamp, J.; et al. Phase 2 study of efgartigimod, a novel FcRn antagonist, in adult patients with primary immune thrombocytopenia. Am. J. Hematol. 2020, 95, 178–187. [Google Scholar] [CrossRef]
- Robak, T.; Kaźmierczak, M.; Jarque, I.; Musteata, V.; Treliński, J.; Cooper, N.; Kiessling, P.; Massow, U.; Woltering, F.; Snipes, R.; et al. Phase 2 multiple-dose study of an FcRn inhibitor, rozanolixizumab, in patients with primary immune thrombocytopenia. Blood Adv. 2020, 4, 4136–4146. [Google Scholar] [CrossRef]
- Chew, L.-C.; Maceda-Galang, L.M.; Tan, Y.K.; Chakraborty, B.; Thumboo, J. Pneumocystis jirovecii pneumonia in patients with autoimmune disease on high-dose glucocorticoid. J. Clin. Rheumatol. 2015, 21, 72–75. [Google Scholar] [CrossRef]
- Malpica, L.; van Duin, D.; Moll, S. Preventing infectious complications when treating non-malignant immune-mediated hematologic disorders. Am. J. Hematol. 2019, 94, 1396–1412. [Google Scholar] [CrossRef] [PubMed]
- Youssef, J.; Novosad, S.A.; Winthrop, K.L. Infection Risk and Safety of Corticosteroid Use. Rheum. Dis. Clin. N. Am. 2016, 42, 157–176. [Google Scholar] [CrossRef] [PubMed]
- Danza, A.; Ruiz-Irastorza, G. Infection risk in systemic lupus erythematosus patients: Susceptibility factors and preventive strategies. Lupus 2013, 22, 1286–1294. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.; Trivedi, K.; Rudrappa, M. Disseminated Cryptococcal Disease with Diffuse Pulmonary Infiltrates in a Non-HIV Host. J. La. State Med. Soc. 2017, 169, 57. [Google Scholar] [PubMed]
- Gea-Banacloche, J.C. Rituximab-associated infections. Semin. Hematol. 2010, 47, 187–198. [Google Scholar] [CrossRef] [PubMed]
- Vidal, L.; Gafter-Gvili, A.; Leibovici, L.; Shpilberg, O. Rituximab as maintenance therapy for patients with follicular lymphoma. Cochrane Database Syst. Rev. 2009, CD006552. [Google Scholar] [CrossRef]
- Berger, J.R.; Malik, V.; Lacey, S.; Brunetta, P.; Lehane, P.B. Progressive multifocal leukoencephalopathy in rituximab-treated rheumatic diseases: A rare event. J. Neurovirol. 2018, 24, 323–331. [Google Scholar] [CrossRef]
- Cohen, S.B.; Emery, P.; Greenwald, M.W.; Dougados, M.; Furie, R.A.; Genovese, M.C.; Keystone, E.C.; Loveless, J.E.; Burmester, G.R.; Cravets, M.W.; et al. Rituximab for rheumatoid arthritis refractory to anti-tumor necrosis factor therapy: Results of a multicenter, randomized, double-blind, placebo-controlled, phase III trial evaluating primary efficacy and safety at twenty-four weeks. Arthritis Rheum. 2006, 54, 2793–2806. [Google Scholar] [CrossRef]
- Serris, A.; Amoura, Z.; Canouï-Poitrine, F.; Terrier, B.; Hachulla, E.; Costedoat-Chalumeau, N.; Papo, T.; Lambotte, O.; Saadoun, D.; Hié, M.; et al. Efficacy and safety of rituximab for systemic lupus erythematosus-associated immune cytopenias: A multicenter retrospective cohort study of 71 adults. Am. J. Hematol. 2018, 93, 424–429. [Google Scholar] [CrossRef]
- Berentsen, S.; Ulvestad, E.; Gjertsen, B.T.; Hjorth-Hansen, H.; Langholm, R.; Knutsen, H.; Ghanima, W.; Shammas, F.V.; Tjønnfjord, G.E. Rituximab for primary chronic cold agglutinin disease: A prospective study of 37 courses of therapy in 27 patients. Blood 2004, 103, 2925–2928. [Google Scholar] [CrossRef]
- Laribi, K.; Bolle, D.; Ghnaya, H.; Sandu, A.; Besançon, A.; Denizon, N.; Truong, C.; Pineau-Vincent, F.; de Materre, A.B. Rituximab is an effective and safe treatment of relapse in elderly patients with resistant warm AIHA. Ann. Hematol. 2016, 95, 765–769. [Google Scholar] [CrossRef]
- Barcellini, W.; Zaja, W.; Zaninoni, A.; Imperiali, F.G.; Battista, M.L.; Di Bona, E.; Fattizzo, B.; Consonni, D.; Cortelezzi, A.; Fanin, R.; et al. Low-dose rituximab in adult patients with idiopathic autoimmune hemolytic anemia: Clinical efficacy and biologic studies. Blood 2012, 119, 3691–3697. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Yan, S.; Liu, H.; Li, L.; Song, J.; Wang, G.; Wang, H.; Wu, Y.; Shao, Z.; Fu, R. Infection risk in autoimmune hematological disorders with low-dose rituximab treatment. J. Clin. Lab. Anal. 2020, 34, e23455. [Google Scholar] [CrossRef] [PubMed]
- Berentsen, S.; Randen, U.; Oksman, M.; Birgens, H.; Tvedt, T.H.A.; Dalgaard, J.; Galteland, E.; Haukås, E.; Brudevold, R.; Sørbø, J.H.; et al. Bendamustine plus rituximab for chronic cold agglutinin disease: Results of a Nordic prospective multicenter trial. Blood 2017, 130, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Berentsen, S.; Randen, U.; Vågan, A.M.; Hjorth-Hansen, H.; Vik, A.; Dalgaard, J.; Jacobsen, E.M.; Thoresen, A.S.; Beiske, K.; Tjønnfjord, G.E. High response rate and durable remissions following fludarabine and rituximab combination therapy for chronic cold agglutinin disease. Blood 2010, 116, 3180–3184. [Google Scholar] [CrossRef]
- Bisharat, N.; Omari, H.; Lavi, I.; Raz, R. Risk of infection and death among post-splenectomy patients. J. Infect. 2001, 43, 182–186. [Google Scholar] [CrossRef]
- Thomsen, R.W.; Schoonen, W.M.; Farkas, D.K.; Riis, A.; Jacobsen, J.; Fryzek, J.P.; Sørensen, H.T. Risk for hospital contact with infection in patients with splenectomy. Ann. Intern. Med. 2009, 151, 546–555. [Google Scholar] [CrossRef]
- Vianelli, N.; Palandri, F.; Polverelli, N.; Stasi, R.; Joelsson, J.; Johansson, E.; Ruggeri, M.; Zaja, F.; Cantoni, S.; Catucci, A.E.; et al. Splenectomy as a curative treatment for immune thrombocytopenia: A retrospective analysis of 233 patients with a minimum follow up of 10 years. Haematologica 2013, 98, 875–880. [Google Scholar] [CrossRef]
- Waghorn, D.J. Overwhelming infection in asplenic patients: Current best practice preventive measures are not being followed. J. Clin. Pathol. 2001, 54, 214–218. [Google Scholar] [CrossRef]
- Davidson, R.N.; Wall, R.A. Prevention and management of infections in patients without a spleen. Clin. Microbiol. Infect. 2001, 7, 657–660. [Google Scholar] [CrossRef]
- Giudice, V.; Rosamilio, R.; Ferrara, I.; Seneca, E.; Serio, B.; Selleri, C. Efficacy and safety of splenectomy in adult autoimmune hemolytic anemia. Open Med. 2016, 11, 374–380. [Google Scholar] [CrossRef]
- Balagué, C.; Targarona, E.M.; Cerdán, G.; Novell, J.; Montero, O.; Bendahan, G.; García, A.; Pey, A.; Vela, S.; Diaz, M.; et al. Long-term outcome after laparoscopic splenectomy related to hematologic diagnosis. Surg. Endosc. 2004, 18, 1283–1287. [Google Scholar] [CrossRef] [PubMed]
- Cortazar, F.B.; Muhsin, S.A.; Pendergraft, W.F., III; Wallace, Z.S.; Dunbar, C.; Laliberte, K.; Niles, J.L. Combination therapy with rituximab and cyclophosphamide for remission induction in ANCA vasculitis. Kidney Int. Rep. 2017, 3, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Teh, C.L.; Kong, K.O.; Chong, A.P.; Badsha, H. Mycobacterium haemophilum infection in a SLE patient on mycophenolate mofetil. Lupus 2002, 11, 249–252. [Google Scholar] [CrossRef] [PubMed]
- Del Pozo, J.L.; de la Garza, R.G.; de Rada, P.D.; Ornilla, E.; Yuste, J.R. Listeria monocytogenes septic arthritis in a patient treated with mycophenolate mofetil for polyarteritis nodosa: A case report and review of the literature. Int. J. Infect. Dis. 2013, 17, e132–e133. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Gibson, R.H.; Evans, R.J.; Hotham, R.; Bojarczuk, A.; Lewis, A.; Bielska, E.; May, R.C.; Elks, P.M.; Renshaw, S.A.; Johnston, S.A. Mycophenolate mofetil increases susceptibility to opportunistic fungal infection independent of lymphocytes. BioRxiv 2017, 131540. [Google Scholar] [CrossRef]
- Bernardo, D.R.; Chahin, N. Toxoplasmic encephalitis during mycophenolate mofetil immunotherapy of neuromuscular disease. Neurol. Neuroimmunol. Neuroinflamm. 2015, 2, e63. [Google Scholar] [CrossRef]
- Emilia, G.; Messora, C.; Longo, G.; Bertesi, M. Long-term salvage treatment by cyclosporin in refractory autoimmune haematological disorders. Br. J. Haematol. 1996, 93, 341–344. [Google Scholar] [CrossRef]
- Howard, J.; Hoffbrand, A.V.; Prentice, H.G.; Mehta, A. Mycophenolate mofetil for the treatment of refractory auto-immune haemolytic anaemia and auto-immune thrombocytopenia purpura. Br. J. Haematol. 2002, 117, 712–715. [Google Scholar] [CrossRef]
- Newman, K.; Owlia, M.B.; El-Hemaidi, I.; Akhtari, M. Management of immune cytopenias in patients with systemic lupus erythematosus—Old and new. Autoimmun. Rev. 2013, 12, 784–791. [Google Scholar] [CrossRef]
- Langereis, J.D.; van den Broek, B.; Franssen, S.; Joosten, I.; Blijlevens, N.M.A.; de Jonge, M.I.; Langemeijer, S. Eculizumab impairs Neisseria meningitidis serogroup B killing in whole blood despite 4CMenB vaccination of PNH patients. Blood Adv. 2020, 4, 3615–3620. [Google Scholar] [CrossRef] [PubMed]
- Al-Ani, F.; Chin-Yee, I.; Lazo-Langner, A. Eculizumab in the management of paroxysmal nocturnal hemoglobinuria: Patient selection and special considerations. Ther. Clin. Risk Manag. 2016, 12, 1161–1170. [Google Scholar] [PubMed]
- Jäger, U.; D’Sa, S.; Schörgenhofer, C.; Bartko, J.; Derhaschnig, U.; Sillaber, C.; Jilma-Stohlawetz, P.; Fillitz, M.; Schenk, T.; Patou, G.; et al. Inhibition of complement C1s improves severe hemolytic anemia in cold agglutinin disease: A first-in-human trial. Blood 2019, 133, 893–901. [Google Scholar] [CrossRef] [PubMed]
- Manda, S.; Dunbar, N.; Marx-Wood, C.R.; Danilov, A.V. Ibrutinib is an effective treatment of autoimmune haemolytic anaemia in chronic lymphocytic leukaemia. Br. J. Haematol. 2015, 170, 734–736. [Google Scholar] [CrossRef]
- Molica, S.; Levato, L.; Mirabelli, R. Chronic lymphocytic leukemia, autoimmune hemolytic anemia and ibrutinib: A case report and review of the literature. Leuk. Lymphoma. 2016, 57, 735–737. [Google Scholar] [CrossRef]
- Rogers, K.A.; Mousa, L.; Zhao, Q.; Bhat, S.A.; Byrd, J.C.; El Boghdadly, Z.; Guerrero, T.; Levine, L.B.; Lucas, F.; Shindiapina, P.; et al. Incidence of opportunistic infections during ibrutinib treatment for B-cell malignancies. Leukemia 2019, 33, 2527–2530. [Google Scholar] [CrossRef]
- Forero-Torres, A.; Ramchandren, R.; Yacoub, A.; Wertheim, M.S.; Edenfield, W.J.; Caimi, P.; Gutierrez, M.; Akard, L.; Escobar, C.; Call, J.; et al. Parsaclisib, a potent and highly selective PI3Kδ inhibitor, in patients with relapsed or refractory B-cell malignancies. Blood 2019, 133, 1742–1752. [Google Scholar] [CrossRef]
- Bussel, J.B.; Arnold, D.M.; Boxer, M.A.; Cooper, N.; Mayer, J.; Zayed, H.; Tong, S.; Duliege, A.M. Long-term fostamatinib treatment of adults with immune thrombocytopenia during the phase 3 clinical trial program. Am. J. Hematol. 2019, 94, 546–553. [Google Scholar] [CrossRef]
- Scott, K.; Hayden, P.J.; Will, A.; Wheatley, K.; Coyne, I. Bortezomib for the treatment of multiple myeloma. Cochrane Database Syst. Rev. 2016, 4, CD010816. [Google Scholar] [CrossRef]
- Ditto, M.C.; Parisi, S.; Varisco, V.; Talotta, R.; Batticciotto, A.; Antivalle, M.; Gerardi, M.C.; Agosti, M.; Borrelli, R.; Fusaro, E.; et al. Prevalence of hepatitis B virus infection and risk of reactivation in rheumatic population undergoing biological therapy. Clin. Exp. Rheumatol. 2020, in press. [Google Scholar]
- Yeo, W.; Johnson, P.J. Diagnosis, prevention and management of hepatitis B virus reactivation during anticancer therapy. Hepatology 2006, 43, 209–220. [Google Scholar] [CrossRef] [PubMed]
- Evens, A.M.; Jovanovic, B.D.; Su, Y.C.; Raisch, D.W.; Ganger, D.; Belknap, S.M.; Dai, M.S.; Chiu, B.C.; Fintel, B.; Cheng, Y.; et al. Rituximab-associated hepatitis B virus (HBV) reactivation in lymphoproliferative diseases: Meta-analysis and examination of FDA safety reports. Ann. Oncol. 2011, 22, 1170–1180. [Google Scholar] [CrossRef] [PubMed]
- Torres, H.A.; Davila, M. Reactivation of hepatitis B virus and hepatitis C virus in patients with cancer. Nat. Rev. Clin. Oncol. 2012, 9, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Ennishi, D.; Maeda, Y.; Niitsu, N.; Kojima, M.; Izutsu, K.; Takizawa, J.; Kusumoto, S.; Okamoto, M.; Yokoyama, M.; Takamatsu, Y.; et al. Hepatic toxicity and prognosis in hepatitis C virus-infected patients with diffuse large B-cell lymphoma treated with rituximab-containing chemotherapy regimens: A Japanese multicenter analysis. Blood 2010, 116, 5119–5125. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Haggag, R.M.; Abu-Taleb, F.; Khaled, H.M. Rituximab-induced hepatitis C virus reactivation in HCV-positive patients with diffuse large Bcell lymphoma. J. Clin. Oncol. 2016, 34, e19039. [Google Scholar] [CrossRef]
- Foran, J.M. Hepatitis C in the rituximab era. Blood 2010, 116, 5081–5082. [Google Scholar] [CrossRef]
- de Melo Silva, J.; Pinheiro-Silva, R.; Dhyani, A.; Pontes, G.S. Cytomegalovirus and Epstein-Barr infections: Prevalence and impact on patients with hematological diseases. BioMed Res. Int. 2020, 2020, 1627824. [Google Scholar] [CrossRef]
- Elter, T.; Gercheva-Kyuchukova, L.; Pylylpenko, H.; Robak, T.; Jaksic, B.; Rekhtman, G.; Kyrcz-Krzemień, S.; Vatutin, M.; Wu, J.; Sirard, C.; et al. Fludarabine plus alemtuzumab versus fludarabine alone in patients with previously treated chronic lymphocytic leukaemia: A randomised phase 3 trial. Lancet Oncol. 2011, 12, 1204–1213. [Google Scholar] [CrossRef]
- Park, S.S.; Cho, S.Y.; Han, E.; Min, G.J.; Park, S.; Yoon, J.H.; Lee, S.E.; Cho, B.S.; Eom, K.S.; Kim, Y.J.; et al. Reactivation and dynamics of cytomegalovirus and Epstein-Barr virus after rabbit antithymocyte globulin and cyclosporine for aplastic anemia. Eur. J. Haematol. 2019, 103, 433–441. [Google Scholar] [CrossRef]
- Scheinberg, P.; Fischer, S.H.; Li, L.; Nunez, O.; Wu, C.O.; Sloand, E.M.; Cohen, J.I.; Young, N.S.; John Barrett, A. Distinct EBV and CMV reactivation patterns following antibody-based immunosuppressive regimens in patients with severe aplastic anemia. Blood 2007, 109, 3219–3224. [Google Scholar] [CrossRef]
- Marchesi, F.; Pimpinelli, F.; Ensoli, F.; Mengarelli, A. Cytomegalovirus infection in hematologic malignancy settings other than the allogeneic transplant. Hematol. Oncol. 2018, 36, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Angarone, M. Epidemiology and prevention of viral infections in patients with hematologic malignancies. Infect. Disord. Drug Targets 2011, 11, 27–33. [Google Scholar] [CrossRef]
- Akiyama, M.; Yoshifuji, K.; Fukuda, T.; Tohda, S.; Miki, T.; Miura, O.; Yamamoto, M. Fulminant visceral disseminated varicella-zoster virus infection without skin involvement in a patient with autoimmune hemolytic anemia on prednisolone therapy. Rinsho Ketsueki 2016, 57, 467–471. [Google Scholar] [PubMed]
- Orvain, C.; Ducancelle, A.; Eymerit-Morin, C.; Rousselet, M.-C.; Oberti, F.; Hunault-Berger, M.; Tanguy-Schmidt, A. Severe viral hepatitis in a patient with chronic lymphocytic leukemia (CLL) complicated with autoimmune hemolytic anemia (AIHA), treated with steroids. J. Clin. Virol. 2015, 62, 66–68. [Google Scholar] [CrossRef] [PubMed]
- Arai, A.; Imadome, K.-I.; Fujiwara, S.; Miura, O. Autoimmune hemolytic anemia accompanied by reactivation of an Epstein-Barr virus infection with suppressed CTL response to EBV-infected cells in an elderly man. Intern. Med. 2010, 49, 325–329. [Google Scholar] [CrossRef]
- Troselj-Vukic, B.; Milotic, I.; Milotic, F.; Crnic-Martinovic, M.; Grahovac, B. Cytomegalovirus reactivation after low-dose steroid treatment for hemolytic anemia in a patient with primary Epstein-Barr virus infection. Wien. Klin. Wochenschr. 2007, 119, 435–437. [Google Scholar] [CrossRef] [PubMed]
- Evangelatos, G.; Koulouri, V.; Iliopoulos, A.; Fragoulis, G.E. Tuberculosis and targeted synthetic or biologic DMARDs, beyond tumor necrosis factor inhibitors. Ther. Adv. Musculoskelet. Dis. 2020, 12, 1759720X20930116. [Google Scholar] [CrossRef]
- Godfrey, M.S.; Friedman, L.N. Tuberculosis and Biologic Therapies: Anti-Tumor Necrosis Factor-α and Beyond. Clin. Chest Med. 2019, 40, 721–739. [Google Scholar] [CrossRef] [PubMed]
- Jick, S.S.; Lieberman, E.S.; Rahman, M.U.; Choi, H.K. Glucocorticoid use, other associated factors, and the risk of tuberculosis. Arthritis Rheum. 2006, 55, 19–26. [Google Scholar] [CrossRef]
- Tam, L.-S.; Li, E.K.; Wong, S.-M.; Szeto, C.-C. Risk factors and clinical features for tuberculosis among patients with systemic lupus erythematosus in Hong Kong. Scand. J. Rheumatol. 2002, 31, 296–300. [Google Scholar] [CrossRef]
- De Martino, M.; Lodi, L.; Galli, L.; Chiappini, E. Immune response to mycobacterium tuberculosis: A narrative review. Front. Pediatr. 2019, 7, 350. [Google Scholar] [CrossRef] [PubMed]
- European Association for the Study of the Liver. EASL 2017. Clinical Practice Guidelines on the management of hepatitis B virus infection. J. Hepatol. 2017, 67, 370–398. [Google Scholar] [CrossRef] [PubMed]
- Reddy, K.R.; Beavers, K.L.; Hammond, S.P.; Lim, J.K.; Falck-Ytter, Y.T.; American Gastroenterological Association Institute. American Gastroenterological Association Institute guideline on the prevention and treatment of hepatitis B virus reactivation during immunosuppressive drug therapy. Gastroenterology 2015, 148, 215–219. [Google Scholar] [CrossRef] [PubMed]
- Karadağ, Ö.; Kaşifoğlu, T.; Özer, B.; Kaymakoğlu, S.; Kuş, Y.; İnanç, M.; Keser, G.; Kiraz, S. Viral hepatitis screening guideline before biological drug use in rheumatic patients. Eur. J. Rheumatol. 2016, 3, 25–28. [Google Scholar] [CrossRef] [PubMed]
- Cohn, D.L.; O’Brien, R.J.; Geiter, L.J.; Gordin, F.; Hershfield, E.; Horsburgh, C. Targeted Tuberculin Testing and Treatment of Latent Tuberculosis Infection. American Thoracic Society. MMWR Morb. Mortal. Wkly. Rep. 2000, 49, 1–51. [Google Scholar]
- Maertens, J.; Cesaro, S.; Maschmeyer, G.; Einsele, H.; Donnelly, J.P.; Alanio, A.; Hauser, P.M.; Lagrou, K.; Melchers, W.J.G.; Helweg-Larsen, J.; et al. 5th European Conference on Infections in Leukaemia (ECIL-5), a joint venture of the European Group for Blood and Marrow Transplantation (EBMT), the European Organisation for Research and Treatment of Cancer (EORTC), the Immunocompromised Host Society (ICHS) and the European LeukemiaNet (ELN). ECIL guidelines for preventing Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J. Antimicrob. Chemother. 2016, 71, 2397–2404. [Google Scholar]
- Katsuyama, T.; Saito, K.; Kubo, S.; Nawata, M.; Tanaka, Y. Prophylaxis for pneumocystis pneumonia in patients with rheumatoid arthritis treated with biologics, based on risk factors found in a retrospective study. Arthritis Res. Ther. 2014, 16, R43. [Google Scholar] [CrossRef]
- Rubin, L.G.; Schaffner, W.; Solomon, C.G. Care of the asplenic patient. N. Engl. J. Med. 2014, 371, 349–356. [Google Scholar] [CrossRef]
- Bonanni, P.; Grazzini, M.; Niccolai, G.; Paolini, D.; Varone, O.; Bartoloni, A.; Bartalesi, F.; Santini, M.G.; Baretti, S.; Bonito, C.; et al. Recommended vaccinations for asplenic and hyposplenic adult patients. Hum. Vaccines Immunother. 2017, 13, 359–368. [Google Scholar] [CrossRef]
- Kanhutu, K.; Jones, P.; Cheng, A.C.; Grannell, L.; Best, E.; Spelman, D. Spleen Australia guidelines for the prevention of sepsis in patients with asplenia and hyposplenism in Australia and New Zealand. Intern. Med. J. 2017, 47, 848–855. [Google Scholar] [CrossRef]
- Lee, G.; Malpica Castillo, L.E.; Walter, J.E. Infection Risk, Immunization Recommendations, and Antimicrobial Prophylaxis Needs When Treating Non-Malignant Hematologic Disorders—Wash Your Hands and What Else? Education Program. In Proceedings of the 62nd ASH Annual Meeting and Exposition, San Diego, CA, USA, 5–8 December 2020. [Google Scholar]
- Weinbaum, C.M.; Williams, I.; Mast, E.E.; Wang, S.A.; Finelli, L.; Wasley, A.; Neitzel, S.M.; Ward, J.W.; Centers for Disease Control and Prevention (CDC). Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm. Rep. 2008, 57, 1–20. [Google Scholar] [CrossRef] [PubMed]
- Ramsay, I.; Gorton, R.L.; Patel, M.; Workman, S.; Symes, A.; Haque, T.; Irish, D.; Seneviratne, S.L.; Burns, S.O.; Wey, E.; et al. Transmission of hepatitis B core antibody and galactomannan enzyme immunoassay positivity via immunoglobulin products: A comprehensive analysis. Clin. Infect. Dis. 2016, 63, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Viganò, M.; Serra, G.; Casella, G.; Grossi, G.; Lampertico, P. Reactivation of hepatitis B virus during targeted therapies for cancer and immunemediated disorders. Expert Opin. Biol. Ther. 2016, 16, 917–926. [Google Scholar] [CrossRef] [PubMed]
- Pisaturo, M.; Di Caprio, G.; Calò, F.; Portunato, F.; Martini, S.; Coppola, N. Management of HBV reactivation in non-oncological patients. Expert Rev. Anti-Infect. Ther. 2018, 16, 611–624. [Google Scholar] [CrossRef]
- Keane, J.; Bresnihan, B. Tuberculosis reactivation during immunosuppressive therapy in rheumatic diseases: Diagnostic and therapeutic strategies. Curr. Opin. Rheumatol. 2008, 20, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Mecoli, C.A.; Saylor, D.; Gelber, A.C.; Christopher-Stine, L. Pneumocystis jiroveci pneumonia in rheumatic disease: A 20-year single-centre experience. Clin. Exp. Rheumatol. 2017, 35, 671–673. [Google Scholar]
- Braga, B.P.; Prieto-González, S.; Hernández-Rodríguez, J. Pneumocystis jirovecii pneumonia prophylaxis in immunocompromised patients with systemic autoimmune diseases. Med. Clin. 2019, 152, 502–507. [Google Scholar] [CrossRef] [PubMed]
- Yahav, D.; Gafter-Gvili, A.; Muchtar, E.; Skalsky, K.; Kariv, G.; Yeshurun, M.; Leibovici, L.; Paul, M. Antiviral prophylaxis in haematological patients: Systematic review and meta-analysis. Eur. J. Cancer 2009, 45, 3131–3148. [Google Scholar] [CrossRef]
- Kawamura, K.; Hayakawa, J.; Akahoshi, Y.; Harada, N.; Nakano, H.; Kameda, K.; Ugai, T.; Wada, H.; Yamasaki, R.; Ishihara, Y.; et al. Low-dose acyclovir prophylaxis for the prevention of herpes simplex virus and varicella zoster virus diseases after autologous hematopoietic stem cell transplantation. Int. J. Hematol. 2015, 102, 230–237. [Google Scholar] [CrossRef]
- Sandherr, M.; Hentrich, M.; von Lilienfeld-Toal, M.; Massenkeil, G.; Neumann, S.; Penack, O.; Biehl, L.; Cornely, O.A. Antiviral prophylaxis in patients with solid tumours and haematological malignancies—Update of the Guidelines of the Infectious Diseases Working Party (AGIHO) of the German Society for Hematology and Medical Oncology (DGHO). Ann. Hematol. 2015, 94, 1441–1450. [Google Scholar] [CrossRef]
- Ljungman, P.; de la Camara, R.; Robin, C.; Crocchiolo, R.; Einsele, H.; Hill, J.A.; Hubacek, P.; Navarro, D.; Cordonnier, C.; Ward, K.N.; et al. Guidelines for the management of cytomegalovirus infection in patients with haematological malignancies and after stem cell transplantation from the 2017 European Conference on Infections in Leukaemia (ECIL 7). Lancet Infect. Dis. 2019, 19, e260–e272. [Google Scholar] [CrossRef]
- Moulis, G.; Lapeyre-Mestre, M.; Mahévas, M.; Montastruc, J.-L.; Sailler, L. Need for an improved vaccination rate in primary immune thrombocytopenia patients exposed to rituximab or splenectomy. A nationwide population-based study in France. Am. J. Hematol. 2015, 90, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Davies, J.M.; Barnes, R.; Milligan, D.; British Committee for Standards in Haematology. Working Party of the Haematology/Oncology Task Force. Update of guidelines for the prevention and treatment of infection in patients with an absent or dysfunctional spleen. Clin. Med. 2002, 2, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Gaston, M.H.; Verter, J.I.; Woods, G.; Pegelow, C.; Kelleher, J.; Presbury, G.; Zarkowsky, H.; Vichinsky, E.; Iyer, R.; Lobel, J.S.; et al. Prophylaxis with oral penicillin in children with sickle cell anemia. A randomized trial. N. Engl. J. Med. 1986, 314, 1593. [Google Scholar] [CrossRef]
- Salamah, M.M. Oral penicillin prophylaxis in children with sickle cell anaemia in Saudi Arabia. N. Engl. J. Med. 1987, 316, 274. [Google Scholar]
- Cohn, A.C.; MacNeil, J.R.; Clark, T.A.; Ortega-Sanchez, I.R.; Briere, E.Z.; Meissner, H.C.; Baker, C.J.; Messonnier, N.E.; Centers for Disease Control and Prevention (CDC). Prevention and control of meningococcal disease: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm. Rep. 2013, 62, 1–28. [Google Scholar]
- McNamara, L.A.; Topaz, N.; Wang, X.; Hariri, S.; Fox, L.; MacNeil, J.R. High risk for invasive Meningococcal disease among patients receivingEculizumab (Soliris) despite receipt of Meningococcal vaccine. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 734–737. [Google Scholar] [CrossRef]
- Furer, V.; Rondaan, C.; Heijstek, M.W.; Agmon-Levin, N.; van Assen, S.; Bijl, M.; Breedveld, F.C.; D’Amelio, R.; Dougados, M.; Kapetanovic, M.C.; et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann. Rheum. Dis. 2020, 79, 39–52. [Google Scholar] [CrossRef]
- Oliveira, J.B. The expanding spectrum of the autoimmune lymphoproliferative syndromes. Curr. Opin. Pediatr. 2013, 25, 722–729. [Google Scholar] [CrossRef]
- Odineal, D.D.; Gershwin, M.E. The Epidemiology and Clinical Manifestations of Autoimmunity in Selective IgA Deficiency. Clin. Rev. Allergy Immunol. 2020, 58, 107–133. [Google Scholar] [CrossRef]
- Feuille, E.J.; Anooshiravani, N.; Sullivan, K.E.; Fuleihan, R.L.; Cunningham-Rundles, C. Autoimmune Cytopenias and Associated Conditions in CVID: A Report From the USIDNET Registry. J. Clin. Immunol. 2018, 38, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Gormezano, N.W.; Kern, D.; Pereira, O.L.; Esteves, G.C.; Sallum, A.M.; Aikawa, N.E.; Pereira, R.M.; Silva, C.A.; Bonfá, E. Autoimmune hemolytic anemia in systemic lupus erythematosus at diagnosis: Differences between pediatric and adult patients. Lupus 2017, 26, 426–430. [Google Scholar] [CrossRef] [PubMed]
- Wen, W.; Liu, Y.; Zhao, C.; Sun, X.; Zhang, C.; Li, Z. Clinical and serologic features of primary Sjögren’s syndrome concomitant with autoimmune hemolytic anemia: A large-scale cross-sectional study. Clin. Rheumatol. 2015, 34, 1877–1884. [Google Scholar] [CrossRef] [PubMed]
- Uzzan, M.; Galicier, L.; Gornet, J.M.; Oksenhendler, E.; Fieschi, C.; Allez, M.; Bouhnik, Y.; Kirchgesner, J.; Boutboul, D.; Treton, X.; et al. Autoimmune cytopenias associated with inflammatory bowel diseases: Insights from a multicenter retrospective cohort. Dig. Liver Dis. 2017, 49, 397–404. [Google Scholar] [CrossRef] [PubMed]
- Sallah, S.; Sigounas, G.; Vos, P.; Wan, J.Y.; Nguyen, N.P. Autoimmune hemolytic anemia in patients with non-Hodgkin’s lymphoma. Ann. Oncol. 2000, 11, 1571–1577. [Google Scholar] [CrossRef]
- Visco, C.; Barcellini, W.; Maura, F.; Neri, A.; Cortelezzi, A.; Rodeghiero, F. Autoimmune cytopenias in chronic lymphocytic leukemia. Am. J. Hematol. 2014, 89, 1055–1062. [Google Scholar] [CrossRef]
- De Keyzer, K.; Peeters, P.; Verhelst, C.; Dendooven, A.; Vonck, A.; Vanholder, R. Autoimmune haemolytic anaemia associated with a thymoma: Case report and review of the literature. Acta Clin. Belg. 2009, 64, 447–451. [Google Scholar] [CrossRef]
- Li, M.; Goldfinger, D.; Yuan, S. Autoimmune hemolytic anemia in pediatric liver or combined liver and small bowel transplant patients: A case series and review of the literature. Transfusion 2012, 52, 48–54. [Google Scholar] [CrossRef]
- González-Vicent, M.; Sanz, J.; Fuster, J.L.; Cid, J.; de Heredia, C.D.; Morillo, D.; Fernández, J.M.; Pascual, A.; Badell, I.; Serrano, D.; et al. Autoimmune hemolytic anemia (AIHA) following allogeneic hematopoietic stem cell transplantation (HSCT): A retrospective analysis and a proposal of treatment on behalf of the Grupo Español De Trasplante de Medula Osea en Niños (GETMON) and the Grupo Español de Trasplante Hematopoyetico (GETH). Transfus. Med. Rev. 2018, 32, 179–185. [Google Scholar]
- Saikia, B.; Gupta, S. Common Variable Immunodeficiency. Indian J. Pediatr. 2016, 83, 338–344. [Google Scholar] [CrossRef]
- Yazdani, R.; Azizi, G.; Abolhassani, H.; Aghamohammadi, A. Selective IgA Deficiency: Epidemiology, Pathogenesis, Clinical Phenotype, Diagnosis, Prognosis and Management. Scand. J. Immunol. 2017, 85, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Hsu, C.Y.; Ko, C.H.; Wang, J.L.; Hsu, T.C.; Lin, C.Y. Comparing the burdens of opportunistic infections among patients with systemic rheumatic diseases: A nationally representative cohort study. Arthritis Res. Ther. 2019, 21, 211. [Google Scholar] [CrossRef] [PubMed]
- Barber, R.M.W.; Clarke, A.E. Systemic lupus erythematosus and risk of infection. Expert Rev. Clin. Immunol. 2020, 16, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Wheat, C.L.; Ko, C.W.; Clark-Snustad, K.; Grembowski, D.; Thornton, T.A.; Devine, B. Inflammatory Bowel Disease (IBD) pharmacotherapy and the risk of serious infection: A systematic review and network meta-analysis. BMC Gastroenterol. 2017, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Zhang, H.; Yang, X.; Li, W.; Li, T.; Liu, S. Laboratory-confirmed bloodstream infection in systemic lupus erythematosus: Risk profiling and short-term mortality. Lupus 2020, 24, 961203320948964. [Google Scholar] [CrossRef] [PubMed]
- Morrison, V.A. Infections in patients with leukemia and lymphoma. Cancer Treat. Res. 2014, 161, 319–349. [Google Scholar]
- Ullmann, A.J.; Schmidt-Hieber, M.; Bertz, H.; Heinz, W.J.; Kiehl, M.; Krüger, W.; Mousset, S.; Neuburger, S.; Neumann, S.; Penack, O.; et al. Infectious Diseases Working Party of the German Society for Hematology and Medical Oncology (AGIHO/DGHO) and the DAG-KBT (German Working Group for Blood and Marrow Transplantation). Infectious diseases in allogeneic haematopoietic stem cell transplantation: Prevention and prophylaxis strategy guidelines 2016. Ann. Hematol. 2016, 95, 1435–1455. [Google Scholar]
- Fishman, J.A. Infection in solid-organ transplant recipients. N. Engl. J. Med. 2007, 357, 2601–2614. [Google Scholar] [CrossRef]
- Gavaldà, J.; Meije, Y.; Fortún, J.; Roilides, E.; Saliba, F.; Lortholary, O.; Muñoz, P.; Grossi, P.; Cuenca-Estrella, M.; ESCMID Study Group for Infections in Compromised Hosts. Invasive fungal infections in solid organ transplant recipients. Clin. Microbiol. Infect. 2014, 20, 27–48. [Google Scholar] [CrossRef]
- Barcellini, W.; Fattizzo, B.; Zaninoni, A. Management of refractory autoimmune hemolytic anemia after allogeneic hematopoietic stem cell transplantation: Current perspectives. J. Blood Med. 2019, 10, 265–278. [Google Scholar] [CrossRef]
- Valent, P.; Lechner, K. Diagnosis and treatment of autoimmune haemolytic anaemias in adults: A clinical review. Wien. Klin. Wochenschr. 2008, 120, 136–151. [Google Scholar] [CrossRef] [PubMed]
- Rose, N.R. Predictors of autoimmune disease: Autoantibodies and beyond. Autoimmunity 2008, 41, 419–428. [Google Scholar] [CrossRef] [PubMed]
- Barcellini, W. New Insights in the Pathogenesis of Autoimmune Hemolytic Anemia. Transfus. Med. Hemother. 2015, 42, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Giovannetti, G.; Pauselli, S.; Barrella, G.; Neri, A.; Antonetti, L.; Gentile, G.; Iacobini, M.; Girelli, G.; Coluzzi, S. Severe warm autoimmune haemolytic anaemia due to anti-Jk(a) autoantibody associated with Parvovirus B19 infection in a child. Blood Transfus. 2013, 11, 634–635. [Google Scholar] [PubMed]
- Ramos-Casals, M.; García-Carrasco, M.; López-Medrano, F.; Trejo, O.; Forns, X.; López-Guillermo, A.; Muñoz, C.; Ingelmo, M.; Font, J. Severe autoimmune cytopenias in treatment-naive hepatitis C virus infection: Clinical description of 35 cases. Medicine 2003, 82, 87–96. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, S.; Abdul Muqtadir, K.; Taj, Y. Warm autoimmune haemolytic anaemia and autoimmune hepatitis in an asymptomatic carrier of hepatitis B virus. J. Pak. Med. Assoc. 2011, 61, 512–515. [Google Scholar]
- Chiao, E.Y.; Engels, E.A.; Kramer, J.R.; Pietz, K.; Henderson, L.; Giordano, T.P.; Landgren, O. Risk of immune thrombocytopenic purpura and autoimmune hemolytic anemia among 120 908 US veterans with hepatitis C virus infection. Arch. Intern. Med. 2009, 169, 357–363. [Google Scholar] [CrossRef]
- Wilkinson, L.S.; Petz, L.D.; Garratty, G. Reappraisal of the role of anti-i in haemolytic anaemia in infectious mononucleosis. Br. J. Haematol. 1973, 25, 715–722. [Google Scholar] [CrossRef]
- Zeller, M.P.; Arnold, D.M.; Al Habsi, K.; Cserti-Gazdewich, C.; Delage, G.; Lebrun, A.; Heddle, N.M. Paroxysmal cold hemoglobinuria: A difficult diagnosis in adult patients. Transfusion 2017, 57, 137–143. [Google Scholar] [CrossRef]
- Atta, M.; Brannigan, E.T.; Bain, B.J. Cold autoimmune hemolytic anemia secondary to atypical pneumonia. Am. J. Hematol. 2017, 92, 109. [Google Scholar] [CrossRef]
- Ramagopalan, S.V.; Goldacre, R.; Skingsley, A.; Conlon, C.; Goldacre, M.J. Associations between selected immune-mediated diseases and tuberculosis: Record-linkage studies. BMC Med. 2013, 11, 97. [Google Scholar] [CrossRef] [PubMed]
- Eskazan, A.E.; Dal, M.S.; Kaya, S.; Dal, T.; Ayyildiz, O.; Soysal, T. Two cases of autoimmune hemolytic anemia secondary to brucellosis: A review of hemolytic disorders in patients with brucellosis. Intern. Med. 2014, 53, 1153–1158. [Google Scholar] [CrossRef] [PubMed]
- Maslov, D.V.; Simenson, V.; Jain, S.; Badari, A. COVID-19 and Cold Agglutinin Hemolytic Anemia. TH Open 2020, 4, e175–e177. [Google Scholar] [CrossRef] [PubMed]
- Lazarian, G.; Quinquenel, A.; Bellal, M.; Siavellis, J.; Jacquy, C.; Re, D.; Merabet, F.; Mekinian, A.; Braun, T.; Damaj, G. Autoimmune haemolytic anaemia associated with COVID-19 infection. Br. J. Haematol. 2020, 190, 29–31. [Google Scholar] [CrossRef]
- Lopez, C.; Kim, J.; Pandey, A.; Huang, T.; DeLoughery, T.G. Simultaneous onset of COVID-19 and autoimmune haemolytic anaemia. Br. J. Haematol. 2020, 190, 31–32. [Google Scholar] [CrossRef]
- Patil, N.R.; Herc, E.S.; Girgis, M. Cold agglutinin disease and autoimmune hemolytic anemia with pulmonary embolism as a presentation of COVID-19 infection. Hematol. Oncol. Stem Cell Ther. 2020. [Google Scholar] [CrossRef]
| Treatment | Main Warnings | References |
|---|---|---|
| Corticosteroids | - Infectious risk is dose-dependent - Also prolonged use of low-dose steroids is associated with atypical and opportunistic infections | [10,11,12] |
| Rituximab | - Safe as single agent - Risk of hepatitis B virus reactivation, if antiviral prophylaxis not instituted - Risk increases in chemotherapy-combined regimens or in the context of severe immunodepression (warning for PML) | [13,14,15,16,17] |
| Splenectomy | - Infections in 6–7% of AIHA patients - Encapsulated bacteria are the main pathogens isolated in OPSI, which can be fatal - Risk decreases with proper patient’s education and vaccinations | [18,19] |
| Classic immunosuppressive agents | - CTX, MMF, and AZA are associated with increased infectious risk by several pathogens - Cyclosporine seems safer than the abovementioned drugs | [20,21,22] |
| Complement inhibitors | - Increased risk of encapsulated bacterial infections | [23,24] |
| BCR pathway antagonists | - PI3Kδ inhibitors are associated to PJP - Fostamatinib (used in RA patients) has an increased infectious risk | [25,26] |
| Proteasome inhibitors | - Apparently safe in AIHA | [27,28] |
| FcRn antagonists | - Reported to be safe in ITP patients | [29,30] |
| Drug | Viral Status | Risk Category |
|---|---|---|
| High-dose steroids * | HBsAg+HBsAg-/antiHBc+ | high moderate |
| Moderate-dose steroids ** | HBsAg+HBsAg-/antiHBc+ | moderate low |
| Short-term low-dose steroids *** | irrelevant | low |
| Rituximab | irrelevant | high |
| Cyclosporine | irrelevant | moderate |
| Methotrexate | irrelevant | low |
| Azathioprine | irrelevant | low |
| Bortezomib | irrelevant | moderate |
| Pathogen | Screening Test | Risk Factors | Prophylaxis | References |
|---|---|---|---|---|
| HBV | HBsAg, antiHBs, antiHBc, antiHBe, HBeAg, HBV-DNA when indicated | Steroids Rituximab Immunosuppressors Bortezomib | - Lamivudine, entecavir, tenofovir or pre-emptive therapy according to EASL or AGA guidelines - HBV vaccination of seronegative patients | [93,94] |
| HCV | Anti-HCV (HCV-RNA if Ab positive) | Long-term steroids Rituximab | - No drugs approved for prophylaxis - Eradication therapy in HCV-RNA+ | [9,95] |
| Mycobacterium tuberculosis | tuberculin skin test or serum interferon gamma release assays +/- chest X-ray | Long-term steroids | Isoniazid (or rifampicin) in latent TB, polichemotherapy in active TB | [96] |
| Pneumocystis jirovecii | No screening tests available | Steroids >10 mg/day + age >65 or pulmonary disease or therapy with rituximab/CTX | TMP-SMX (atovaquone, pentamidine, dapsone if not tolerated/contraindicated) | [9,97,98] |
| Encapsulated bacteria | No screening tests available | Splenectomy Complement inhibitors | - ACWY and B group meningococcal vaccines - 23-valent and 13-valent pneumococcal vaccines - Haemophilus influenzae type B vaccine | [23,99,100,101,102] |
| Risk Category | Preventive Strategy Recommended | |
|---|---|---|
| EASL Guidelines (2017) | AGA Guidelines (2015) | |
| High (>10%) | Entecavir or tenofovir if HBsAg+ Lamivudine if HBsAg-/antiHBc+ | Entecavir or tenofovir |
| Moderate (1–10%) | Pre-emptive therapy | Entecavir or tenofovir |
| Low (<1%) | Pre-emptive therapy | Pre-emptive therapy |
| Condition | Frequency of AIHA | Characteristics of Infections | References |
|---|---|---|---|
| Primary immunodeficiencies | |||
| Autoimmune lymphoproliferative syndrome | 29% | Up to 30% of patients with bacterial infections related to neutropenia and splenectomy | [121] |
| IgA deficiency | 15% | 40–90% of patients experience recurrent respiratory infections, cases of Giardia lamblia infections | [122,133] |
| Common variable immundeficiency | 2–5% | 50% of subjects with upper respiratory tract infections, 50% pneumonia, 40% diarrhea, 10% VZV reactivation | [123,132] |
| Autoimmune diseases | |||
| Systemic lupus erythematosus | 3–14% | 43.1/1000 patients/year incidence of opportunistic infections; Infection is a major cause of death | [124,134,135] |
| Sjogren syndrome | 2–3% | 24.1/1000 patients/year incidence of opportunistic infections; infections are one of the main causes of death | [125,134] |
| Inflammatory bowel diseases | 0.05% | Up to 30% of treated patients experienced infections | [126,136] |
| Neoplasms | |||
| Chronic lymphocytic leukemia | 5–20% | Frequency of drug specific infections: 57% FC; 40% FCR (mainly bacterial/opportunistic); 27% alemtuzumab (mainly CMV and fungi); 12–45% anti-CD20 (HBV, CMV, HSV, VZV, PML); 13–50% with novel drugs (ibrutinib, skin, respiratory tract, UTIs; idelalisib, PJP, CMV; venetoclax, bacterial infections) | [128,138] |
| Transplants | |||
| Hematopoietic stem cell transplant | 10–15% | 7–50% bacteriemia; 11–24% airways, GI tract, skin and soft tissue infection; 4–20% UTIs; 1–5% PJP (without prophylaxis); 23% invasive aspergillosis; 30–50% CMV reactivation | [131,139] |
| Solid organs transplant | 2–3% | Frequent bacterial infections in the first month after transplant; 30–97% CMV reactivation; 2% Candida; 1–2% invasive aspergillosis; 1–2% cryptococcosis | [130,140,141] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giannotta, J.A.; Fattizzo, B.; Cavallaro, F.; Barcellini, W. Infectious Complications in Autoimmune Hemolytic Anemia. J. Clin. Med. 2021, 10, 164. https://doi.org/10.3390/jcm10010164
Giannotta JA, Fattizzo B, Cavallaro F, Barcellini W. Infectious Complications in Autoimmune Hemolytic Anemia. Journal of Clinical Medicine. 2021; 10(1):164. https://doi.org/10.3390/jcm10010164
Chicago/Turabian StyleGiannotta, Juri Alessandro, Bruno Fattizzo, Francesca Cavallaro, and Wilma Barcellini. 2021. "Infectious Complications in Autoimmune Hemolytic Anemia" Journal of Clinical Medicine 10, no. 1: 164. https://doi.org/10.3390/jcm10010164
APA StyleGiannotta, J. A., Fattizzo, B., Cavallaro, F., & Barcellini, W. (2021). Infectious Complications in Autoimmune Hemolytic Anemia. Journal of Clinical Medicine, 10(1), 164. https://doi.org/10.3390/jcm10010164





