The Effects of Propofol or Dexmedetomidine Sedation on Postoperative Recovery in Elderly Patients Receiving Lower Limb Surgery under Spinal Anesthesia: A Retrospective Propensity Score-Matched Analysis
Abstract
1. Introduction
2. Materials and Methods
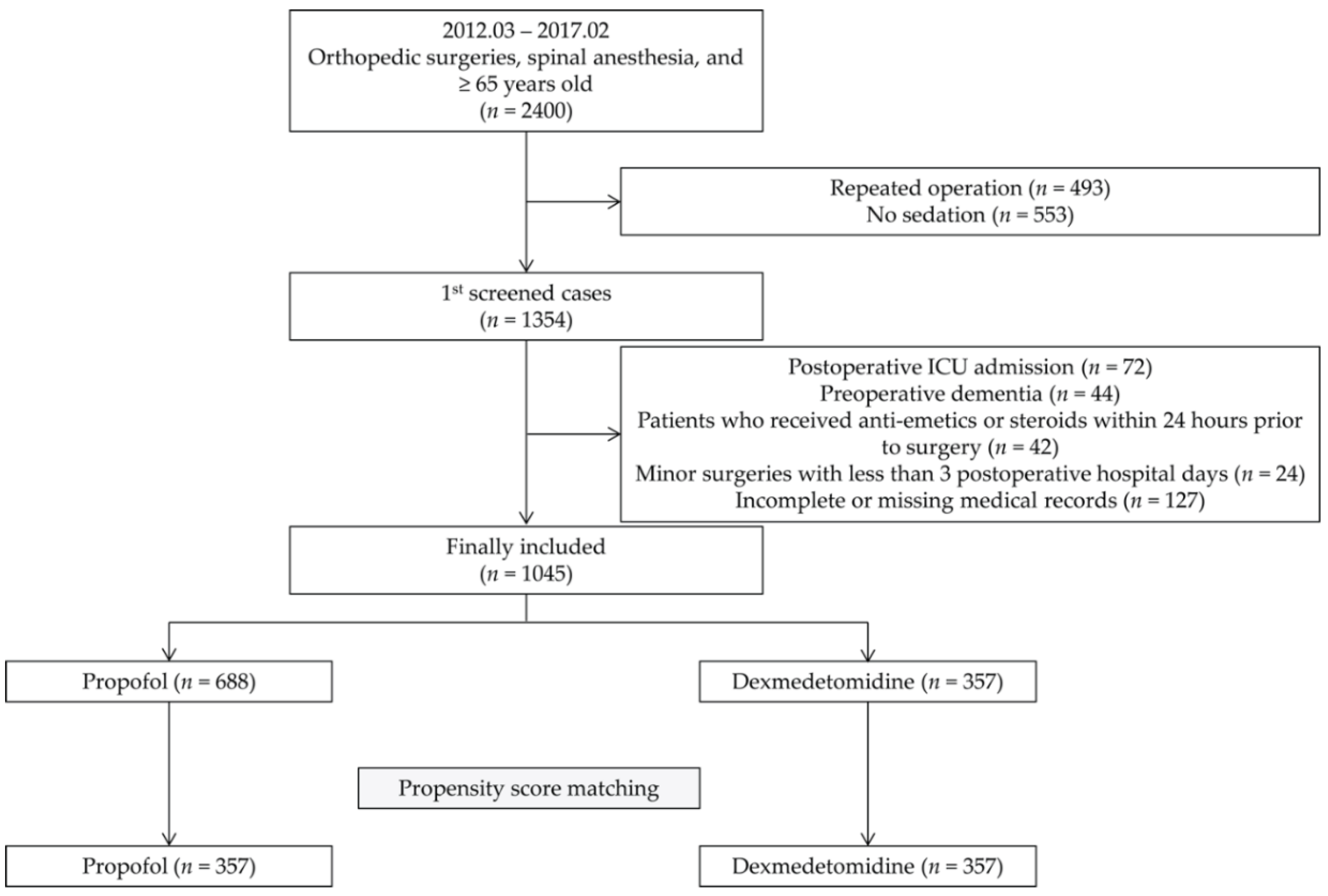
2.1. Study Population
2.2. Spinal Anesthesia and Intraoperative Sedation
2.3. Study Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Athanassoglou, V.; Wallis, A.; Galitzine, S. Audiovisual distraction as a useful adjunct to epidural anesthesia and sedation for prolonged lower limb microvascular orthoplastic surgery. J. Clin. Anesth. 2015, 27, 606–611. [Google Scholar] [CrossRef] [PubMed]
- Höhener, D.; Blumenthal, S.; Borgeat, A. Sedation and regional anaesthesia in the adult patient. Br. J. Anaesth. 2008, 100, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Barakat, A.R.; Sutcliffe, N.; Schwab, M. Effect site concentration during propofol TCI sedation: A comparison of sedation score with two pharmacokinetic models. Anaesthesia 2007, 62, 661–666. [Google Scholar] [CrossRef]
- Maze, M.; Angst, M.S. Dexmedetomidine and Opioid Interactions: Defining the Role of Dexmedetomidine for Intensive Care Unit Sedation. Anesthesiology 2004, 101, 1059–1061. [Google Scholar] [CrossRef]
- Djaiani, G.; Silverton, N.; Fedorko, L.; Carroll, J.; Styra, R.; Rao, V.; Katznelson, R. Dexmedetomidine versus Propofol Sedation Reduces Delirium after Cardiac Surgery: A Randomized Controlled Trial. Anesthesiology 2016, 124, 362–368. [Google Scholar] [CrossRef] [PubMed]
- Park, J.B.; Bang, S.H.; Chee, H.K.; Kim, J.S.; Lee, S.A.; Shin, J.K. Efficacy and Safety of Dexmedetomidine for Postoperative Delirium in Adult Cardiac Surgery on Cardiopulmonary Bypass. Korean J. Thorac. Cardiovasc. Surg. 2014, 47, 249–254. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.J.; Do, S.H.; Lee, J.S.; Kim, T.K.; Na, H.S. Comparison of Intraoperative Sedation with Dexmedetomidine Versus Propofol on Acute Postoperative Pain in Total Knee Arthroplasty Under Spinal Anesthesia: A Randomized Trial. Anesth. Analg. 2018, 129, 1512–1518. [Google Scholar] [CrossRef]
- Jin, S.; Liang, D.D.; Chen, C.; Zhang, M.; Wang, J. Dexmedetomidine prevent postoperative nausea and vomiting on patients during general anesthesia: A PRISMA-compliant meta analysis of randomized controlled trials. Medicine 2017, 96, e5770. [Google Scholar] [CrossRef]
- Bellon, M.; Le Bot, A.; Michelet, D.; Hilly, J.; Maesani, M.; Brasher, C.; Dahmani, S. Efficacy of Intraoperative Dexmedetomidine Compared with Placebo for Postoperative Pain Management: A Meta-Analysis of Published Studies. Pain Ther. 2016, 5, 63–80. [Google Scholar] [CrossRef]
- Deiner, S.; Luo, X.; Lin, H.M.; Sessler, D.I.; Saager, L.; Sieber, F.E.; Lee, H.B.; Sano, M.; Jankowski, C.; Bergese, S.D.; et al. Intraoperative Infusion of Dexmedetomidine for Pre-vention of Postoperative Delirium and Cognitive Dysfunction in Elderly Patients Undergoing Major Elective Noncardiac Surgery: A Randomized Clinical Trial. JAMA Surg. 2017, 152, e171505. [Google Scholar] [CrossRef]
- Park, J.-K.; Cheong, S.H.; Lee, K.M.; Lim, S.H.; Lee, J.H.; Cho, K.; Kim, M.-H.; Kim, H.-T. Does dexmedetomidine reduce postoperative pain after laparoscopic cholecystectomy with multimodal analgesia? Korean J. Anesthesiol. 2012, 63, 436–440. [Google Scholar] [CrossRef] [PubMed]
- Bajwa, S.J.S.; Bajwa, S.K.; Kaur, J.; Singh, G.; Arora, V.; Gupta, S.; Kulshrestha, A.; Singh, A.; Parmar, S.S.; Singh, A.; et al. Dexmedetomidine and clonidine in epidural anaesthesia: A comparative evaluation. Indian J. Anaesth. 2011, 55, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Tramèr, M.; Moore, A.; McQuay, H. Propofol anaesthesia and postoperative nausea and vomiting: Quantitative systematic review of randomized controlled studies. Br. J. Anaesth. 1997, 78, 247–255. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Ginsberg, B.; Grant, A.P.; Glass, P.S.A. Double-blind, Randomized Comparison of Ondansetron and Intraoperative Propofol to Prevent Postoperative Nausea and Vomiting. Anesthesiology 1996, 85, 1036–1042. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.; Yoo, Y.C.; Lee, S.K.; Kim, H.; Ju, H.M.; Min, K.T. Comparison of the efficacy and safety of sedation between dexme-detomidine-remifentanil and propofol-remifentanil during endoscopic submucosal dissection. World J. Gastroenterol. 2015, 21, 3671–3678. [Google Scholar] [CrossRef]
- Mitasova, A.; Kostalova, M.; Bednarik, J.; Michalcakova, R.; Kasparek, T.; Balabanova, P. Poststroke delirium incidence and outcomes: Validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit. Care Med. 2012, 40, 484–490. [Google Scholar] [CrossRef]
- Oh, T.K.; Park, H.Y.; Shin, H.J.; Jeon, Y.T.; Do, S.H.; Hwang, J.W. The Role of Perioperative Statin Use in the Prevention of De-lirium After Total Knee Replacement Under Spinal Anesthesia. J. Arthroplast. 2018, 33, 3666. [Google Scholar] [CrossRef]
- Robinson, T.N.; Raeburn, C.D.; Tran, Z.V.; Angles, E.M.; Brenner, L.A.; Moss, M. Postoperative delirium in the elderly: Risk factors and outcomes. Ann. Surg. 2009, 249, 173–178. [Google Scholar] [CrossRef]
- Rudolph, J.L.; Marcantonio, E.R. Review articles: Postoperative delirium: Acute change with long-term implications. Anesth. Analg. 2011, 112, 1202–1211. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Flacker, J.M.; Michaels, M.; Resnick, N.M. Delirium Is Independently Associated with Poor Functional Recovery After Hip Fracture. J. Am. Geriatr. Soc. 2000, 48, 618–624. [Google Scholar] [CrossRef]
- Liu, Y.; Ma, L.; Gao, M.; Guo, W.; Ma, Y. Dexmedetomidine reduces postoperative delirium after joint replacement in elderly patients with mild cognitive impairment. Aging Clin. Exp. Res. 2016, 28, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R.; Wysong, A.; van der Starre, P.J.; Block, T.; Miller, C.; Reitz, B.A. Dexmedetomidine and the reduction of postoperative delirium after cardiac surgery. Psychosomatics 2009, 50, 206–217. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.J.; Koo, B.W.; Bang, S.U.; Kim, J.H.; Hwang, J.W.; Do, S.H.; Na, H.S. Intraoperative dexmedetomidine sedation reduces the postoperative agitated behavior in elderly patients undergoing orthopedic surgery compared to the propofol sedation. Minerva Anestesiol. 2017, 83, 1042–1050. [Google Scholar] [PubMed]
- Wang, C.-G.; Qin, Y.-F.; Wan, X.; Song, L.-C.; Li, Z.-J.; Li, H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J. Orthop. Surg. Res. 2018, 13, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Pinho, C.; Cruz, S.; Santos, A.; Abelha, F. Postoperative delirium: Age and low functional reserve as independent risk factors. J. Clin. Anesth. 2016, 33, 507–513. [Google Scholar] [CrossRef]
- Kalisvaart, K.J.; Vreeswijk, R.; de Jonghe, J.F.; van der Ploeg, T.; van Gool, W.A.; Eikelenboom, P. Risk factors and prediction of postoperative delirium in elderly hip-surgery patients: Implementation and validation of a medical risk factor model. J. Am. Geriatr. Soc. 2006, 54, 817–822. [Google Scholar] [CrossRef]
- Raats, J.; Jelle, W.; Van Eijsden, W.; Wilbert, A.; Crolla, R.; Steyerberg, E.; Van Der Laan, L. Risk Factors and Outcomes for Postoperative Delirium after Major Surgery in Elderly Patients. PLoS ONE 2015, 10, e0136071. [Google Scholar] [CrossRef]
- Zaal, I.J.; Devlin, J.W.; Hazelbag, M.; Klouwenberg, P.M.C.K.; Van Der Kooi, A.W.; Ong, D.S.Y.; Cremer, O.L.; Groenwold, R.H.; Slooter, A.J.C. Benzodiazepine-associated delirium in critically ill adults. Intensiv. Care Med. 2015, 41, 2130–2137. [Google Scholar] [CrossRef]
- Alagiakrishnan, K.; Wiens, C.A. An approach to drug induced delirium in the elderly. Postgrad. Med. J. 2004, 80, 388–393. [Google Scholar] [CrossRef]
- Arain, S.R.; Ebert, T.J. The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth. Analg. 2002, 95, 461–466. [Google Scholar]
- Cheng, S.S.; Yeh, J.; Flood, P. Anesthesia Matters: Patients Anesthetized with Propofol Have Less Postoperative Pain than Those Anesthetized with Isoflurane. Anesth. Analg. 2008, 106, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Tan, T.; Bhinder, R.; Carey, M.; Briggs, L. Day-Surgery Patients Anesthetized with Propofol Have Less Postoperative Pain than Those Anesthetized with Sevoflurane. Anesth. Analg. 2010, 111, 83–85. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.; Zhou, M.; Feng, J.J.; Wu, L.; Fang, S.P.; Ge, X.Y.; Sun, H.J.; Ren, P.C.; Lv, X. Efficacy of dexmedetomidine on postoperative nausea and vomiting: A meta-analysis of randomized controlled trials. Int. J. Clin. Exp. Med. 2015, 8, 8450–8571. [Google Scholar] [PubMed]
- Visser, K.; Hassink, E.A.; Bonsel, G.J.; Moen, J.; Kalkman, C.J. Randomized controlled trial of total intravenous anesthesia with propofol versus inhalation anesthesia with isoflurane-nitrous oxide: Postoperative nausea with vomiting and economic analysis. Anesthesiology 2001, 95, 616–626. [Google Scholar] [CrossRef] [PubMed]
| Unmatched Cohort (n = 1045) | Matched Cohort (n = 714) | |||||||
|---|---|---|---|---|---|---|---|---|
| Propofol n = 688 | DMED n = 357 | SMD | p | Propofol n = 357 | DMED n = 357 | SMD | p | |
| Age, year | 74.0 (70.0–79.0) | 74.0 (70.0–79.0) | 0.004 | 0.870 | 74.0 (70.0–78.0) | 74.0 (70.0–79.0) | 0.018 | 0.954 |
| Sex | ||||||||
| Male | 123 (17.9) | 68 (19.0) | 0.030 | 0.643 | 68 (19.0) | 68 (19.0) | < 0.001 | > 0.999 |
| Female | 565 (82.1) | 289 (81.0) | 289 (81.0) | 289 (81.0) | ||||
| BMI, kg m–2 | 25.6 (23.2–28.0) | 25.6 (23.3–28.2) | 0.088 | 0.580 | 25.7 (23.4–28.1) | 25.6 (23.3–28.2) | 0.047 | 0.951 |
| ASA status (I/II) | ||||||||
| I | 85 (12.4) | 44 (12.3) | 0.019 | 0.958 | 40 (11.2) | 44 (12.3) | 0.038 | 0.879 |
| II | 545 (79.2) | 281 (78.7) | 283 (79.3) | 281 (78.7) | ||||
| III | 58 (8.4) | 32 (9.0) | 34 (9.5) | 32 (9.0) | ||||
| Hypertension | 384 (55.8) | 205 (57.4) | 0.032 | 0.619 | 203 (56.9) | 205 (57.4) | 0.011 | 0.880 |
| Diabetes mellitus | 163 (23.7) | 84 (23.5) | 0.004 | 0.953 | 76 (21.3) | 84 (23.5) | 0.054 | 0.473 |
| Ischemic heart disease | 58 (8.4) | 26 (7.3) | 0.043 | 0.518 | 24 (6.7) | 26 (7.3) | 0.022 | 0.769 |
| Cerebrovascular disease | 47 (6.8) | 31 (8.7) | 0.069 | 0.280 | 30 (8.4) | 31 (8.7) | 0.010 | 0.893 |
| CCI | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.003 | 0.804 | 0.0 (0.0–1.0) | 0.0 (0.0–1.0) | 0.018 | 0.574 |
| Anemia (Hb < 10 g dL–1) | 44 (6.4) | 16 (4.5) | 0.084 | 0.207 | 13 (3.6) | 16 (4.5) | 0.043 | 0.570 |
| Albumin, g dL–1 | 4.2 (4.0–4.4) | 4.3 (4.0–4.4) | 0.055 | 0.555 | 4.3 (4.1–4.4) | 4.3 (4.0–4.4) | 0.075 | 0.462 |
| Type of surgery | ||||||||
| CRIF | ||||||||
| Femur | 18 (2.6) | 2 (0.6) | 0.233 | 0.081 | 2 (0.6) | 2 (0.6) | 0.055 | 0.881 |
| Tibia, fibula, and foot | 2 (0.3) | 1 (0.3) | 2 (0.6) | 1 (0.3) | ||||
| ORIF | ||||||||
| Femur | 56 (8.1) | 21 (5.9) | 23 (6.4) | 21 (5.9) | ||||
| Tibia, fibula, and foot | 28 (4.1) | 7 (2.0) | 8 (2.2) | 7 (2.0) | ||||
| Replacement | ||||||||
| Hip | 124 (18.0) | 72 (20.2) | 73 (20.4) | 72 (20.2) | ||||
| Knee | 426 (61.9) | 237 (66.4) | 240 (67.2) | 237 (66.4) | ||||
| Ankle | 4 (0.6) | 3 (0.8) | 1 (0.3) | 3 (0.8) | ||||
| Others | 30 (4.4) | 14 (3.9) | 8 (2.2) | 14 (3.9) | ||||
| Operative characteristics | ||||||||
| Operation time (min) | 135.0 (115.0–150.0) | 135.0 (120.0–150.0) | 0.062 | 0.304 | 135.0 (120.0–150.0) | 135.0 (120.0–150.0) | 0.021 | 0.922 |
| Estimated blood loss (mL) | 100.0 (50.0–200.0) | 100.0 (50.0–200.0) | 0.014 | 0.195 | 100.0 (50.0–200.0) | 100.0 (50.0–200.0) | < 0.001 | 0.980 |
| MBP, mmHg | 72.9 (68.5–78.3) | 73.7 (68.7–78.9) | 0.019 | 0.333 | 73.0 (68.3–78.3) | 73.7 (68.7–78.9) | 0.023 | 0.415 |
| RBC transfusion | 135 (19.6) | 64 (17.9) | 0.043 | 0.508 | 67 (18.8) | 64 (17.9) | 0.022 | 0.772 |
| Admission period | 7.5 (5.4–12.5) | 7.4 (5.4–12.4) | 0.041 | 0.622 | 7.4 (5.4–12.4) | 7.4 (5.4–12.4) | 0.065 | 0.566 |
| Years at surgery | ||||||||
| 2012–2013 | 187 (27.2) | 96 (26.9) | 0.058 | 0.347 | 92 (25.8) | 96 (26.9) | 0.042 | 0.316 |
| 2014–2015 | 315 (45.8) | 150 (42.0) | 169 (47.3) | 150 (42.0) | ||||
| 2016–2017 | 186 (27.0) | 111 (31.1) | 96 (26.9) | 111 (31.1) | ||||
| Premedication | ||||||||
| Midazolam (mg) | 3.0 (1.0–3.0) | 3.0 (1.0–3.0) | 0.035 | 0.571 | 3.0 (1.0–3.0) | 3.0 (1.0–3.0) | 0.041 | 0.684 |
| Propofol | DMED | Odds Ratio (95% CI) | p | |
|---|---|---|---|---|
| Before matching | ||||
| POD | 38/688 (5.5) | 7/357 (2.0) | 0.19 (0.07–0.55) | 0.007 |
| Neuropsychiatry consultation | 51/688 (7.4) | 12/357 (3.4) | 0.43 (0.23–0.83) | 0.009 |
| MEC, mg | 126.0 (69.9–207.3) | 123.0 (57.0–195.0) | 0.071 | |
| NRA | 1.0 (0.0–2.0) | 1.0 (0.0–3.0) | 0.527 | |
| After matching | ||||
| POD | 20/357 (5.6) | 7/357 (2.0) | 0.19 (0.07–0.56) | 0.011 |
| Neuropsychiatry consultation | 26/357 (7.3) | 12/357 (3.4) | 0.44 (0.22–0.90) | 0.020 |
| MEC, mg | 119.0 (70.0–202.0) | 123.0 (57.0–195.0) | 0.156 | |
| NRA | 1.0 (0.0–2.0) | 1.0 (0.0–3.0) | 0.245 |
| Odds Ratio (95% CI) | p | |
|---|---|---|
| Sedative | ||
| Propofol | 1 | |
| DMED | 0.34 (0.15–0.77) | 0.010 |
| Age | 1.15 (1.10–1.20) | <0.001 |
| Sex | ||
| Male | 1 | |
| Female | 0.77 (0.38–1.59) | 0.485 |
| BMI | 0.86 (0.80–0.93) | <0.001 |
| ASA | ||
| I | 1 | |
| II | 5.89 (0.80–43.31) | 0.082 |
| III | 12.59 (1.55–102.49) | 0.018 |
| Hypertension | 1.06 (0.58–1.94) | 0.845 |
| Diabetes mellitus | 1.18 (0.60–2.33) | 0.625 |
| Ischemic heart disease | 1.46 (0.56–3.80) | 0.441 |
| Cerebrovascular disease | 0.82 (0.29– 2.35) | 0.711 |
| CCI | 1.28 (1.05–1.56) | 0.016 |
| Anemia | 4.65 (2.13–10.18) | <0.001 |
| Albumin | 0.33 (0.19–0.57) | <0.001 |
| Hip surgery | 4.60 (2.49–8.49) | <0.001 |
| Operation time | 0.99 (0.98–1.00) | 0.006 |
| Estimated blood loss | 1.00 (1.00–1.00) | 0.381 |
| MBP | 1.01 (0.98–1.05) | 0.442 |
| RBC transfusion | 3.02 (1.63–5.60) | <0.001 |
| Years at surgery | ||
| 2012-2013 | 1 | |
| 2014-2015 | 0.95 (0.48–1.90) | 0.894 |
| 2016-2017 | 0.60 (0.26–1.41) | 0.242 |
| Midazolam | 0.67 (0.51–0.87) | 0.003 |
| MEC | 1.00 (1.00–1.00) | 0.577 |
| NRA | 1.17 (0.99–1.39) | 0.063 |
| Odds Ratio (95% CI) | p | |
|---|---|---|
| Sedative | ||
| Propofol | 1 | |
| DMED | 0.33 (0.14–0.77) | 0.011 |
| Age | 1.10 (1.05–1.15) | <0.001 |
| BMI | 0.99 (0.90–1.08) | 0.769 |
| ASA | ||
| I | 1 | |
| II | 5.43 (0.72–40.70) | 0.100 |
| III | 6.32 (0.74–54.10) | 0.093 |
| CCI | 1.07 (0.84–1.37) | 0.597 |
| Anemia | 2.22 (0.94–5.24) | 0.070 |
| Albumin | 0.43 (0.23–0.98) | 0.046 |
| Hip surgery | 2.86 (1.45–5.65) | 0.002 |
| Operation time | 1.00 (0.99–1.01) | 0.691 |
| RBC transfusion | 1.17 (0.53–2.56) | 0.698 |
| Midazolam | 1.04 (0.76–1.41) | 0.818 |
| NRA | 1.02 (0.80–1.31) | 0.856 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, J.-W.; Kim, E.-K.; Lee, H.-T.; Park, S.; Do, S.-H. The Effects of Propofol or Dexmedetomidine Sedation on Postoperative Recovery in Elderly Patients Receiving Lower Limb Surgery under Spinal Anesthesia: A Retrospective Propensity Score-Matched Analysis. J. Clin. Med. 2021, 10, 135. https://doi.org/10.3390/jcm10010135
Park J-W, Kim E-K, Lee H-T, Park S, Do S-H. The Effects of Propofol or Dexmedetomidine Sedation on Postoperative Recovery in Elderly Patients Receiving Lower Limb Surgery under Spinal Anesthesia: A Retrospective Propensity Score-Matched Analysis. Journal of Clinical Medicine. 2021; 10(1):135. https://doi.org/10.3390/jcm10010135
Chicago/Turabian StylePark, Jin-Woo, Eun-Kyoung Kim, Hun-Taek Lee, Seongjoo Park, and Sang-Hwan Do. 2021. "The Effects of Propofol or Dexmedetomidine Sedation on Postoperative Recovery in Elderly Patients Receiving Lower Limb Surgery under Spinal Anesthesia: A Retrospective Propensity Score-Matched Analysis" Journal of Clinical Medicine 10, no. 1: 135. https://doi.org/10.3390/jcm10010135
APA StylePark, J.-W., Kim, E.-K., Lee, H.-T., Park, S., & Do, S.-H. (2021). The Effects of Propofol or Dexmedetomidine Sedation on Postoperative Recovery in Elderly Patients Receiving Lower Limb Surgery under Spinal Anesthesia: A Retrospective Propensity Score-Matched Analysis. Journal of Clinical Medicine, 10(1), 135. https://doi.org/10.3390/jcm10010135





