Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population and Setting
2.3. Sample Size and Sampling Procedure
2.4. Data Collection Tool
2.5. Ethical Approval
2.6. Data Analysis
3. Results
3.1. Descriptive Statistics Analyses
3.2. Bivariate Analysis
3.3. Multilevel Logistic Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data. Available online: https://covid19.who.int/region/afro/country/ke (accessed on 8 August 2021).
- Barasa, E.; Mothupi, M.C.; Guleid, F.; Nwosu, C.; Kabia, E.; Araba, D.; Orangi, S.; Muraya, K.; Gitaka, J.; Marsh, K. Health and Socio-Economic Impacts of Physical Distancing for COVID-19 in Africa; Center for Global Development: Washington, DC, USA, 2020. [Google Scholar]
- Barasa, E.; Kazungu, J.; Orangi, S.; Kabia, E.; Ogero, M.; Kasera, K. Assessing the Indirect Health Effects of the COVID-19 Pandemic in Kenya; CGD Work. Pap. 570; Center for Global Development: Washington, DC, USA, 2021. [Google Scholar]
- World Health Organization. A Coordinated Global Research RoadMap: 2019 Novel Coronavirus; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- World Health Organization. Draft Landscape and Tracker of COVID-19 Candidate Vaccines. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 18 February 2021).
- Anyiam-Osigwe, T. COVID-19 Vaccines Are Now Approved in Some Countries. What Will It Take to Approve Them for the Rest of the World? Available online: https://www.gavi.org/vaccineswork/covid-19-vaccines-are-now-approved-some-countries-what-will-it-take-approve-them (accessed on 25 April 2021).
- Kyobutungi, C. The Ins and Outs of Kenya’s COVID-19 Vaccine Rollout Plan. Available online: https://theconversation.com/the-ins-and-outs-of-kenyas-covid-19-vaccine-rollout-plan-156310 (accessed on 26 April 2021).
- Dyer, O. Covid-19: Delta infections threaten herd immunity vaccine strategy. BMJ 2021, 374, n1933. [Google Scholar] [CrossRef] [PubMed]
- Aschwanden, C. Five reasons why COVID herd immunity is probably impossible. Nat. Cell Biol. 2021, 591, 520–522. [Google Scholar] [CrossRef]
- World Health Organization. SAGE Working Group on Vaccine Hesitancy Report of the SAGE Working Group on Vaccine Hesitancy; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Afolabi, A.A.; Ilesanmi, O.S. Dealing with vaccine hesitancy in Africa: The prospective COVID-19 vaccine context. Pan Afr. Med J. 2021, 38, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Nachega, J.B.; Sam-Agudu, N.A.; Masekela, R.; van der Zalm, M.M.; Nsanzimana, S.; Condo, J.; Ntoumi, F.; Rabie, H.; Kruger, M.; Wiysonge, C.S.; et al. Addressing challenges to rolling out COVID-19 vaccines in African countries. Lancet Glob. Health 2021, 9, e746–e748. [Google Scholar] [CrossRef]
- Dinga, J.; Sinda, L.; Titanji, V. Assessment of Vaccine Hesitancy to a COVID-19 Vaccine in Cameroonian Adults and Its Global Implication. Vaccines 2021, 9, 175. [Google Scholar] [CrossRef] [PubMed]
- Ditekemena, J.; Nkamba, D.; Mavoko, A.; Fodjo, J.S.; Luhata, C.; Obimpeh, M.; Van Hees, S.; Nachega, J.; Colebunders, R. COVID-19 Vaccine Acceptance in the Democratic Republic of Congo: A Cross-Sectional Survey. Vaccines 2021, 9, 153. [Google Scholar] [CrossRef] [PubMed]
- Gallup. Wellcome Global Monitor-First Wave Findings; Wellcome: London, UK, 2019. [Google Scholar]
- Abuya, T.; Austrian, K.; Isaac, A.; Kangwana, B.; Mbushi, F.; Muluve, E.; Mwanga, D.; Ngo, T.; Nzioki, M.; Ochako, R.; et al. Experiences among Adults and Adolescents During COVID-19 Pandemic from Four Locations across Kenya-Study Description; Population Council: New York, NY, USA, 2020. [Google Scholar]
- Muthengi, E.; Austrian, K. Cluster randomized evaluation of the Nia Project: Study protocol. Reprod. Health 2018, 15, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Austrian, K.; Muthengi, E.; Mumah, J.; Soler-Hampejsek, E.; Kabiru, C.W.; Abuya, B.; Maluccio, J.A. The Adolescent Girls Initiative-Kenya (AGI-K): Study protocol. BMC Public Health 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Austrian, K. Evaluation of the NISITU Program: A Study to Determine the Effect of a Gender Attitudes and Gender Based Violence Program for Adolescents in Nairobi, Kenya. Available online: https://www.isrctn.com/ISRCTN67829143 (accessed on 25 April 2021).
- Larson, H.J.; Jarrett, C.; Schulz, W.S.; Chaudhuri, M.; Zhou, Y.; Dubé, E.; Schuster, M.; MacDonald, N.E.; Wilson, R. Measuring vaccine hesitancy: The development of a survey tool. Vaccine 2015, 33, 4165–4175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Al-Mohaithef, M.; Padhi, B.K. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A web-based national survey. J. Multidiscip. Health 2020, 13, 1657–1663. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2020, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Dzinamarira, T.; Nachipo, B.; Phiri, B.; Musuka, G. COVID-19 Vaccine Roll-Out in South Africa and Zimbabwe: Urgent Need to Address Community Preparedness, Fears and Hesitancy. Vaccines 2021, 9, 250. [Google Scholar] [CrossRef]
- IOL 52% of South Africans Don’t Want Covid Vaccine, Despite SA Securing Initial Batch. Available online: https://www.iol.co.za/personal-finance/insurance/52-of-south-africans-dont-want-covid-vaccine-despite-sa-securing-initial-batch-f45373f0-6199-46ab-8207-fb632706b8e5 (accessed on 30 April 2021).
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Arce, J.S.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef]
- Edwards, B.; Biddle, N.; Gray, M.; Sollis, K. COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE 2021, 16, e0248892. [Google Scholar] [CrossRef]
- Almaghaslah, D.; Alsayari, A.; Kandasamy, G.; Vasudevan, R. COVID-19 Vaccine hesitancy among young adults in Saudi Arabia: A cross-sectional web-based study. Vaccines 2021, 9, 330. [Google Scholar] [CrossRef]
- World Health Organization. Behavioural Considerations for Acceptance and Uptake of COVID-19 Vaccines; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Lawes-Wickwar, S.; Ghio, D.; Tang, M.; Keyworth, C.; Stanescu, S.; Westbrook, J.; Jenkinson, E.; Kassianos, A.; Scanlan, D.; Garnett, N.; et al. A rapid systematic review of public responses to health messages encouraging vaccination against infectious diseases in a pandemic or epidemic. Vaccines 2021, 9, 72. [Google Scholar] [CrossRef] [PubMed]
| County | Location | Underlying Population Council Cohort | Sample Size |
|---|---|---|---|
| Kilifi | 3 sub-counties (Ganze, Kaloleni, Magarini) |
| n = 1096 (657 females) |
| Kisumu | 1 informal settlement (Nyalenda) 1 peri-urban area (Kolwa East) |
| n = 704 (593 females) |
| Nairobi | 5 Informal Settlements (Kibera, Huruma, Dandora, Kariobangi, Mathare) |
| n = 1117 (697 females) |
| Wajir | 79 villages in 3 sub-counties (Wajir East, Wajir West, Wajir South) |
| n = 1218 (833 females) |
| Socio-Demographic Characteristics | Total Sample | Kilifi County | Kisumu County | Nairobi County | Wajir County |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| All respondents across all counties | 4136 (100%) | - | - | - | - |
| County: | |||||
| Urban county (Nairobi/Kisumu) | 1822 (44.0%) | - | 704 (100%) | 1118 (100%) | - |
| Rural county (Kilifi/Wajir) | 2314 (56.0%) | 1096 (100%) | - | - | 1218 (100%) |
| Sex: | |||||
| Female | 2780 (67.2%) | 657 (60.0%) | 593(84.2%) | 697 (62.4%) | 833 (68.4%) |
| Male | 1355 (32.8%) | 439 (40.0%) | 111 (15.8%) | 420 (37.6%) | 385 (31.6%) |
| Age group (years): | |||||
| 18–35 | 1348 (33.3%) | 258 (24.4%) | 350 (50.5%) | 471 (42.4%) | 269 (22.7%) |
| 36–57 | 2358 (58.3%) | 689 (65.1%) | 311 (44.9%) | 596 (53.7%) | 762 (64.4%) |
| 58+ | 338 (8.4%) | 111 (10.5%) | 32 (4.6%) | 43 (3.9%) | 152 (12.9%) |
| Marital status: | |||||
| Single | 1, 128(27.3%) | 245 (22.4%) | 297 (42.2%) | 455 (40.7%) | 131 (10.8%) |
| Married | 3008 (72.7%) | 851 (77.6%) | 407 (57.8%) | 663 (59.3%) | 1087 (89.2%) |
| Highest level of education: | |||||
| No schooling/Pre-primary | 1476 (35.7%) | 253 (23.1%) | 18 (2.6%) | 40 (3.6%) | 1165 (95.7%) |
| Primary school | 1450 (35.0%) | 625 (57.0%) | 323 (45.9%) | 470 (42.0%) | 32 (2.6%) |
| Secondary school | 904 (21.9%) | 165 (15.1%) | 268 (38.1%) | 462 (41.3%) | 9 (0.7%) |
| Tertiary school | 306 (7.4%) | 53 (4.8%) | 95 (13.5%) | 146 (13.1%) | 12 (1.0%) |
| Socio-economic status: | |||||
| Tertile 1 (Poorest) | 1516 (36.7%) | 364 (33.2%) | 301 (42.9%) | 299 (26.8%) | 552 (45.3%) |
| Tertile 2 | 1120 (27.1%) | 382 (34.9%) | 179 (25.5%) | 536 (48.0%) | 23 (1.9%) |
| Tertile 3 (Wealthiest) | 1496 (36.2%) | 350 (31.9%) | 222 (31.6%) | 281 (25.2%) | 643 (52.8%) |
| Average household size: Mean (sd) | |||||
| Urban county | 5.8 (3.2) | - | 6.4 (3.9) | 5.4 (2.6) | - |
| Rural county | 8.9 (4.8) | 8.8 (4.8) | - | - | 9.0 (4.8) |
| Socio-Demographic Factors | Overall | Kilifi County | Kisumu County | Nairobi County | Wajir County | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Vaccine | p-Value | Vaccine | p-Value | Vaccine | p-Value | Vaccine | p-Value | Vaccine | p-Value | |
| Hesitant n (%) | Hesitant n (%) | Hesitant n (%) | Hesitant n (%) | Hesitant n (%) | ||||||
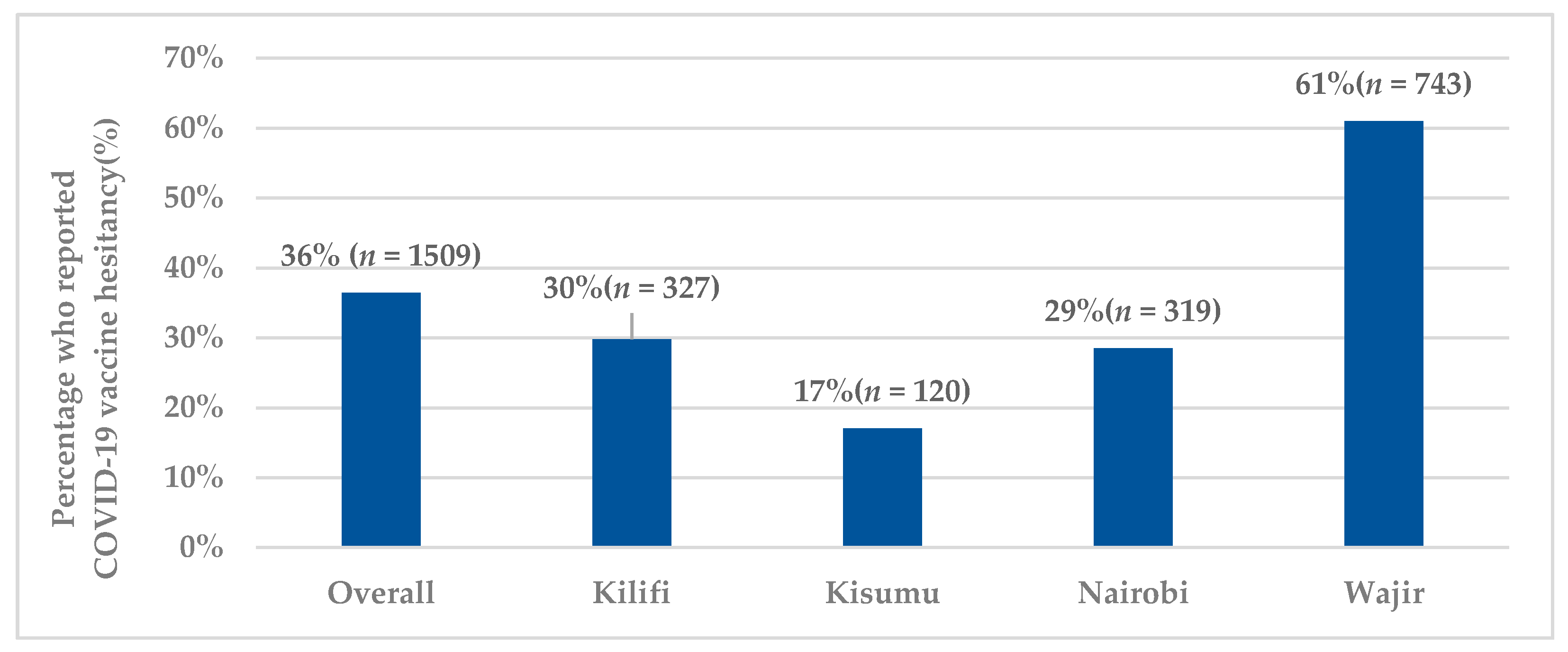
| All respondents | 1509 (36.5%) | - | 327 (29.8%) | - | 120 (17.1%) | 319 (28.5%) | 743 (61.0%) | |||
| County: | ||||||||||
| Urban county (Nairobi/Kisumu) | 439 (24.1%) | 0.000 * | ||||||||
| Rural county (Kilifi/Wajir) | 1070 (46.2%) | |||||||||
| Sex: | ||||||||||
| Female | 1023 (36.8%) | 0.559 | 214 (32.6%) | 0.015 * | 104 (17.5%) | 0.422 | 203 (29.1%) | 0.589 | 502 (60.3%) | 0.438 |
| Male | 486 (35.9%) | 113 (25.7%) | 16 (14.4%) | 116 (27.6%) | 241 (62.6%) | |||||
| Age group (years): | ||||||||||
| 18–35 | 453 (33.6%) | 0.003 * | 87 (33.7%) | 0.344 | 65 (18.6%) | 0.083 | 140 (29.7%) | 0.748 | 161 (59.9%) | 0.189 |
| 36–57 | 878 (37.2%) | 201 (29.2%) | 52 (16.7%) | 167 (28.0%) | 458 (60.1%) | |||||
| 58+ | 146 (43.2%) | 31 (27.9%) | 1 (3.1%) | 11(25.6%) | 103 (67.8%) | |||||
| Marital status: | ||||||||||
| Single | 358 (31.7%) | 0.000 * | 84 (34.3%) | 0.084 | 54 (18.2%) | 0.493 | 114 (31.7%) | 0.056 | 76 (58.0%) | 0.458 |
| Married | 1151 (38.3%) | 243 (28.6%) | 66 (16.2%) | 175 (26.4%) | 667 (61.4%) | |||||
| Highest level of education: | ||||||||||
| No schooling/Pre-primary | 795 (53.9%) | 0.000 * | 75 (29.6%) | 0.51 | 2 (11.1%) | 0.000 * | 6 (15.0%) | 0.097 | 712 (61.1%) | 0.09 |
| Primary school | 363 (25.0%) | 178 (28.5%) | 37 (11.5%) | 125 (26.6%) | 23 (71.9%) | |||||
| Secondary school | 254 (28.1%) | 56 (33.9%) | 53 (19.8%) | 141 (30.5%) | 4 (44.4%) | |||||
| Tertiary school | 97 (31.7%) | 18 (34.0%) | 28 (29.5%) | 47 (32.2%) | 4 (33.3%) | |||||
| Socio-economic status: | ||||||||||
| Tertile 1 (Poorest) | 594 (39.2%) | 0.000 * | 115 (31.6%) | 0.611 | 47 (15.6%) | 0.525 | 97 (32.4%) | 0.206 | 335 (60.7%) | 0.693 |
| Tertile 2 | 297 (26.5%) | 108 (28.3%) | 30 (16.8%) | 143 (26.7%) | 16 (69.6%) | |||||
| Tertile 3 (Wealthiest) | 618 (41.3%) | 104 (29.7%) | 43 (19.4%) | 79 (28.1%) | 392 (60.96%) | |||||
| Predictor Variables | aOR (95% CI) | p-Value |
|---|---|---|
| Socio-Demographic Factors | ||
| County: | ||
| Urban county (Nairobi/Kisumu) | Ref | |
| Rural county (Kilifi/Wajir) | 2.46 (1.02–5.94) | 0.046 * |
| Sex | ||
| Female | Ref | |
| Male | 0.91 (0.77–1.08) | 0.301 |
| Age group (years): | ||
| 18–35 | Ref | |
| 36–57 | 0.96 (0.81–1.14) | 0.645 |
| 58+ | 1.03 (0.76–1.39) | 0.835 |
| Marital status: | ||
| Single | Ref | |
| Married | 0.92 (0.76–1.10) | 0.367 |
| Education: | ||
| No schooling/Pre-primary | Ref | |
| Primary school | 0.92 (0.69–1.24) | 0.59 |
| Secondary school | 1.21 (0.87–1.69) | 0.25 |
| Tertiary school | 1.30 (0.87–1.92) | 0.2 |
| Socio-economic status: | ||
| Tertile 1 (Poorest) | Ref | |
| Tertile 2 | 0.90 (0.74–1.11) | 0.325 |
| Tertile 3 (Wealthiest) | 0.93 (0.78–1.10) | 0.386 |
| Individual influences, risks, and perceptions | ||
| Perceived COVID infection risk: | ||
| Some risk | Ref | |
| No risk | 1.80 (1.54–2.10) | 0.000 * |
| Perceived ability to adhere to government regulations | ||
| regarding COVID-19 prevention: | ||
| Easy to adhere | Ref | |
| Difficult to adhere | 1.96 (1.65–2.33) | 0.000 * |
| Wearing of masks (now compared to when COVID began): | ||
| Wear masks more or the same | Ref | |
| Wear masks less | 1.09 (0.93–1.27) | 0.282 |
| Socio-economic impact of COVID measures: | ||
| Socio-economically affected by measures | Ref | |
| Not socio-economically affected by measures | 1.10 (0.88–1.37) | 0.407 |
| Context | ||
| Healthcare providers as a trusted source of information: | ||
| No | Ref | |
| Yes | 0.98 (0.84–1.14) | 0.768 |
| Vaccine specific issues | ||
| Vaccine side effects concerns: | ||
| No | Ref | |
| Yes | 3.38 (2.81–4.07) | 0.000 * |
| Don’t think the vaccine is effective: | ||
| No | Ref | |
| Yes | 1.89 (1.58–2.27) | 0.000 * |
| Hard to access vaccination sites: | ||
| No | Ref | |
| Yes | 0.72 (0.58–0.90) | 0.004 * |
| Scared of needles: | ||
| No | Ref | |
| Yes | 0.82 (0.64–1.04) | 0.105 |
| Religious and cultural reasons: | ||
| No | Ref | |
| Yes | 1.42 (1.01–1.98) | 0.040 * |
| Too busy to get vaccinated: | ||
| No | Ref | |
| Yes | 1.10 (0.81–1.50) | 0.527 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Orangi, S.; Pinchoff, J.; Mwanga, D.; Abuya, T.; Hamaluba, M.; Warimwe, G.; Austrian, K.; Barasa, E. Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya. Vaccines 2021, 9, 936. https://doi.org/10.3390/vaccines9080936
Orangi S, Pinchoff J, Mwanga D, Abuya T, Hamaluba M, Warimwe G, Austrian K, Barasa E. Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya. Vaccines. 2021; 9(8):936. https://doi.org/10.3390/vaccines9080936
Chicago/Turabian StyleOrangi, Stacey, Jessie Pinchoff, Daniel Mwanga, Timothy Abuya, Mainga Hamaluba, George Warimwe, Karen Austrian, and Edwine Barasa. 2021. "Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya" Vaccines 9, no. 8: 936. https://doi.org/10.3390/vaccines9080936
APA StyleOrangi, S., Pinchoff, J., Mwanga, D., Abuya, T., Hamaluba, M., Warimwe, G., Austrian, K., & Barasa, E. (2021). Assessing the Level and Determinants of COVID-19 Vaccine Confidence in Kenya. Vaccines, 9(8), 936. https://doi.org/10.3390/vaccines9080936






