Kawasaki Disease and Vaccination: Prospective Case-Control and Case-Crossover Studies among Infants in Japan
Abstract
1. Introduction
2. Materials and Methods
2.1. Case-Control Study
2.1.1. Study Design and Subjects
2.1.2. Questionnaires
2.1.3. Statistical Analyses
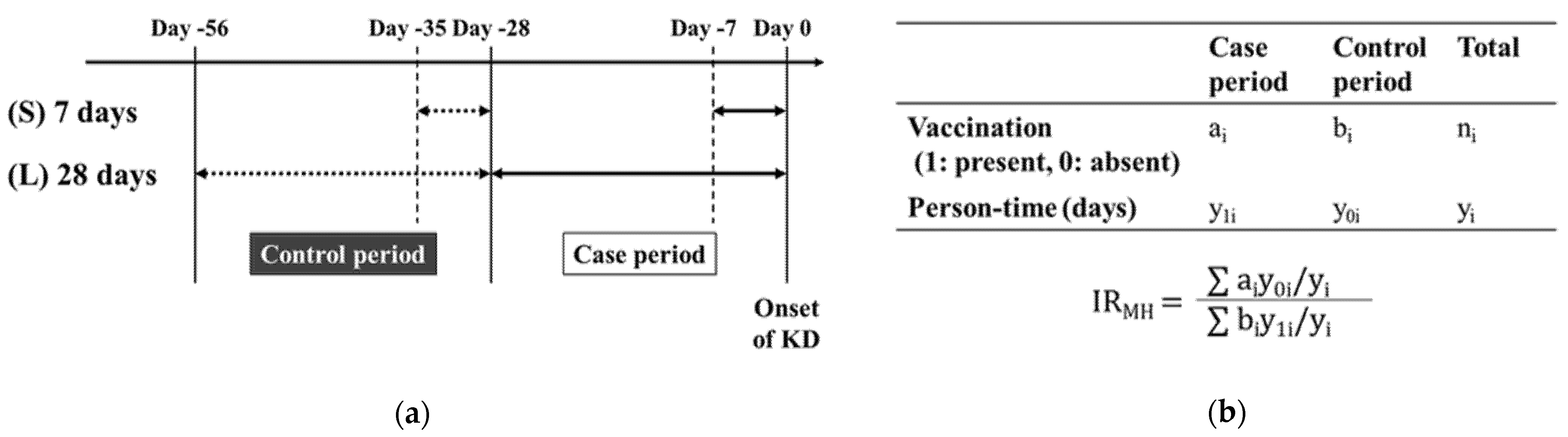
2.2. Case-Crossover Study
2.3. The Analysis of Data from the Nationwide Survey of KD in Japan
3. Results
3.1. Case-Control Study
3.1.1. Patient Characteristics
3.1.2. Comparison of Vaccination Status
3.2. Case-Crossover Study
3.3. The Analysis of Data from the Nationwide Survey of KD in Japan
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kawasaki, T.; Kosaki, F.; Okawa, S.; Shigematsu, I.; Yanagawa, H. A new infantile acute febrile mucocutaneous lymph node syndrome (MLNS) prevailing in Japan. Pediatrics 1974, 54, 271–276. [Google Scholar]
- Fukazawa, R.; Kobayashi, J.; Ayusawa, M.; Hamada, H.; Miura, M.; Mitani, Y.; Tsuda, E.; Nakajima, H.; Matsuura, H.; Ikeda, K.; et al. JCS/JSCS 2020 Guideline on Diagnosis and Management of Cardiovascular Sequelae in Kawasaki Disease. Circ. J. 2020, 84, 1348–1407. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, N.; Singh-Grewal, D. Kawasaki Disease: A Clinician’s Update. Int. J. Pediatrics 2013, 2013, 645391. [Google Scholar] [CrossRef] [PubMed]
- Hara, T.; Nakashima, Y.; Sakai, Y.; Nishio, H.; Motomura, Y.; Yamasaki, S. Kawasaki disease: a matter of innate immunity. Clin Exp Immunol 2016. [Google Scholar] [CrossRef] [PubMed]
- Rowley, A.H.; Baker, S.C.; Orenstein, J.M.; Shulman, S.T. Searching for the cause of Kawasaki disease--cytoplasmic inclusion bodies provide new insight. Nat. Rev. Microbiol. 2008, 6, 394–401. [Google Scholar] [CrossRef]
- Matsuno, S.; Utagawa, E.; Sugiura, A. Association of rotavirus infection with Kawasaki syndrome. J. Infect. Dis. 1983, 148, 177. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.Y.; Lu, C.Y.; Shao, P.L.; Lee, P.I.; Lin, M.T.; Fan, T.Y.; Cheng, A.L.; Lee, W.L.; Hu, J.J.; Yeh, S.J.; et al. Viral infections associated with Kawasaki disease. J. Med. Assoc. 2014, 113, 148–154. [Google Scholar] [CrossRef]
- Chang, A.; Islam, S. Kawasaki disease and vasculitis associated with immunization. Pediatr. Int. 2018, 60, 613–617. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. Package Insert-RotaTeq. Available online: https://www.fda.gov/vaccines-blood-biologics/vaccines/rotateq (accessed on 13 October 2020).
- Rypdal, M.; Rypdal, V.; Burney, J.A.; Cayan, D.; Bainto, E.; Skochko, S.; Tremoulet, A.H.; Creamean, J.; Shimizu, C.; Kim, J.; et al. Clustering and climate associations of Kawasaki Disease in San Diego County suggest environmental triggers. Sci. Rep. 2018, 8, 16140. [Google Scholar] [CrossRef]
- Ayusawa, M.; Sonobe, T.; Uemura, S.; Ogawa, S.; Nakamura, Y.; Kiyosawa, N.; Ishii, M.; Harada, K. Revision of diagnostic guidelines for Kawasaki disease (the 5th revised edition). Pediatr. Int. 2005, 47, 232–234. [Google Scholar] [CrossRef]
- Kobayashi, T.; Ayusawa, M.; Suzuki, H.; Abe, J.; Ito, S.; Kato, T.; Kamada, M.; Shiono, J.; Suda, K.; Tsuchiya, K.; et al. Revision of diagnostic guidelines for Kawasaki disease (6th revised edition). Pediatr. Int. 2020, 62, 1135–1138. [Google Scholar] [CrossRef]
- Ministry of Internal Affairs and Communications of Japan. Japan Standard Occupational Classification (Rev. 4th, December 1997), Classification Structure and Explanatory Notes. Available online: https://www.soumu.go.jp/english/dgpp_ss/seido/shokgyou/5soc.htm (accessed on 19 March 2021).
- Fukushima, W.; Ozasa, K.; Okumura, A.; Mori, M.; Hosoya, M.; Nakano, T.; Tanabe, T.; Yamaguchi, N.; Suzuki, H.; Mori, M.; et al. Oseltamivir use and severe abnormal behavior in Japanese children and adolescents with influenza: Is a self-controlled case series study applicable? Vaccine 2017, 35, 4817–4824. [Google Scholar] [CrossRef]
- Ki, M.; Park, T.; Yi, S.G.; Oh, J.K.; Choi, B. Risk analysis of aseptic meningitis after measles-mumps-rubella vaccination in Korean children by using a case-crossover design. Am. J. Epidemiol. 2003, 157, 158–165. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fujita, Y.; Nakamura, Y.; Sakata, K.; Hara, N.; Kobayashi, M.; Nagai, M.; Yanagawa, H.; Kawasaki, T. Kawasaki disease in families. Pediatrics 1989, 84, 666–669. [Google Scholar]
- Yanagawa, H.; Nakamura, Y.; Yashiro, M.; Fujita, Y.; Nagai, M.; Kawasaki, T.; Aso, S.; Imada, Y.; Shigematsu, I. A Nationwide Incidence Survey of Kawasaki Disease in 1985–1986 in Japan. J. Infect. Dis. 1988, 158, 1296–1301. [Google Scholar] [CrossRef]
- Banday, A.Z.; Bhattacharya, D.; Pandiarajan, V.; Singh, S. Kawasaki disease in siblings in close temporal proximity to each other-what are the implications? Clin. Rheumatol. 2021, 40, 849–855. [Google Scholar] [CrossRef]
- Nakamura, Y.; Yashiro, M.; Uehara, R.; Sadakane, A.; Chihara, I.; Aoyama, Y.; Kotani, K.; Yanagawa, H. Epidemiologic features of Kawasaki disease in Japan: results of the 2007–2008 nationwide survey. J. Epidemiol./Jpn. Epidemiol. Assoc. 2010, 20, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Yashiro, M.; Uehara, R.; Sadakane, A.; Tsuboi, S.; Aoyama, Y.; Kotani, K.; Tsogzolbaatar, E.O.; Yanagawa, H. Epidemiologic features of Kawasaki disease in Japan: results of the 2009–2010 nationwide survey. J. Epidemiol./Jpn. Epidemiol. Assoc. 2012, 22, 216–221. [Google Scholar] [CrossRef]
- Makino, N.; Nakamura, Y.; Yashiro, M.; Ae, R.; Tsuboi, S.; Aoyama, Y.; Kojo, T.; Uehara, R.; Kotani, K.; Yanagawa, H. Descriptive epidemiology of Kawasaki disease in Japan, 2011–2012: from the results of the 22nd nationwide survey. J. Epidemiol./Jpn. Epidemiol. Assoc. 2015, 25, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Makino, N.; Nakamura, Y.; Yashiro, M.; Sano, T.; Ae, R.; Kosami, K.; Kojo, T.; Aoyama, Y.; Kotani, K.; Yanagawa, H. Epidemiological observations of Kawasaki disease in Japan, 2013–2014. Pediatr. Int. 2018, 60, 581–587. [Google Scholar] [CrossRef] [PubMed]
- Makino, N.; Nakamura, Y.; Yashiro, M.; Kosami, K.; Matsubara, Y.; Ae, R.; Aoyama, Y.; Yanagawa, H. Nationwide epidemiologic survey of Kawasaki disease in Japan, 2015–2016. Pediatr. Int. 2019, 61, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Ae, R.; Makino, N.; Kosami, K.; Kuwabara, M.; Matsubara, Y.; Nakamura, Y. Epidemiology, Treatments, and Cardiac Complications in Patients with Kawasaki Disease: The Nationwide Survey in Japan, 2017–2018. J. Pediatr. 2020, 225, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Bonaldo, G.; Noseda, R.; Ceschi, A.; Vaccheri, A.; Motola, D. Evaluation of the safety profile of rotavirus vaccines: a pharmacovigilance analysis on American and European data. Sci. Rep. 2020, 10, 13601. [Google Scholar] [CrossRef] [PubMed]
- Layton, J.B.; Butler, A.M.; Panozzo, C.A.; Brookhart, M.A. Rotavirus vaccination and short-term risk of adverse events in US infants. Paediatr. Perinat. Epidemiol. 2018, 32, 448–457. [Google Scholar] [CrossRef] [PubMed]
- Mellone, N.G.; Silva, M.T.; Paglia, M.D.G.; Lopes, L.C.; Barberato-Filho, S.; Del Fiol, F.S.; Bergamaschi, C.C. Kawasaki Disease and the Use of the Rotavirus Vaccine in Children: A Systematic Review and Meta-Analysis. Front. Pharm. 2019, 10, 1075. [Google Scholar] [CrossRef]
- Yung, C.F.; Ma, X.; Cheung, Y.B.; Oh, B.K.; Soh, S.; Thoon, K.C. Kawasaki Disease following administration of 13-valent pneumococcal conjugate vaccine in young children. Sci. Rep. 2019, 9, 14705. [Google Scholar] [CrossRef]
- Baker, M.A.; Baer, B.; Kulldorff, M.; Zichittella, L.; Reindel, R.; DeLuccia, S.; Lipowicz, H.; Freitas, K.; Jin, R.; Yih, W.K. Kawasaki disease and 13-valent pneumococcal conjugate vaccination among young children: A self-controlled risk interval and cohort study with null results. PLoS Med. 2019, 16, e1002844. [Google Scholar] [CrossRef]
- O’Ryan, M.; Stoddard, J.; Toneatto, D.; Wassil, J.; Dull, P.M. A Multi-Component Meningococcal Serogroup B Vaccine (4CMenB): The Clinical Development Program. Drugs 2014, 74, 15–30. [Google Scholar] [CrossRef] [PubMed]
- Phuong, L.K.; Bonetto, C.; Buttery, J.; Pernus, Y.B.; Chandler, R.; Felicetti, P.; Goldenthal, K.L.; Kucuku, M.; Monaco, G.; Pahud, B.; et al. Kawasaki disease and immunisation: A systematic review. Vaccine 2017, 35, 1770–1779. [Google Scholar] [CrossRef] [PubMed]
- Abrams, J.Y.; Weintraub, E.S.; Baggs, J.M.; McCarthy, N.L.; Schonberger, L.B.; Lee, G.M.; Klein, N.P.; Belongia, E.A.; Jackson, M.L.; Naleway, A.L.; et al. Childhood vaccines and Kawasaki disease, Vaccine Safety Datalink, 1996–2006. Vaccine 2015, 33, 382–387. [Google Scholar] [CrossRef]
- Stowe, J.; Andrews, N.J.; Turner, P.J.; Miller, E. The risk of Kawasaki disease after pneumococcal conjugate & meningococcal B vaccine in England: A self-controlled case-series analysis. Vaccine 2020, 38, 4935–4939. [Google Scholar] [CrossRef] [PubMed]
- Abe, J.; Jibiki, T.; Noma, S.; Nakajima, T.; Saito, H.; Terai, M. Gene expression profiling of the effect of high-dose intravenous Ig in patients with Kawasaki disease. J. Immunol. 2005, 174, 5837–5845. [Google Scholar] [CrossRef]
- Foell, D.; Ichida, F.; Vogl, T.; Yu, X.; Chen, R.; Miyawaki, T.; Sorg, C.; Roth, J. S100A12 (EN-RAGE) in monitoring Kawasaki disease. Lancet 2003, 361, 1270–1272. [Google Scholar] [CrossRef]
- Hoshina, T.; Kusuhara, K.; Ikeda, K.; Mizuno, Y.; Saito, M.; Hara, T. High mobility group box 1 (HMGB1) and macrophage migration inhibitory factor (MIF) in Kawasaki disease. Scand. J. Rheumatol. 2008, 37, 445–449. [Google Scholar] [CrossRef]
- Jia, C.; Zhang, J.; Chen, H.; Zhuge, Y.; Chen, H.; Qian, F.; Zhou, K.; Niu, C.; Wang, F.; Qiu, H.; et al. Endothelial cell pyroptosis plays an important role in Kawasaki disease via HMGB1/RAGE/cathespin B signaling pathway and NLRP3 inflammasome activation. Cell Death Dis. 2019, 10, 778. [Google Scholar] [CrossRef]
- Nakashima, Y.; Sakai, Y.; Mizuno, Y.; Furuno, K.; Hirono, K.; Takatsuki, S.; Suzuki, H.; Onouchi, Y.; Kobayashi, T.; Tanabe, K.; et al. Lipidomics links oxidized phosphatidylcholines and coronary arteritis in Kawasaki disease. Cardiovasc. Res. 2021, 117, 96–108. [Google Scholar] [CrossRef] [PubMed]
- Takeshita, S.; Kawase, H.; Yamamoto, M.; Fujisawa, T.; Sekine, I.; Yoshioka, S. Increased expression of human 63-kD heat shock protein gene in Kawasaki disease determined by quantitative reverse transcription-polymerase chain reaction. Pediatr. Res. 1994, 35, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Truong, D.; Minich, L.; Lin, E.; Williams, R.V.; Schlaberg, R.; Lambert, L.M.; Yang, Y.; Areinamo, I.; Ampofo, K.; Tristani-Firouzi, M. Next Generation Sequencing in Kawasaki Disease: A Pilot Study. Circulation 2019, 140, A15274. [Google Scholar]
- Horinouchi, T.; Nozu, K.; Hamahira, K.; Inaguma, Y.; Abe, J.; Nakajima, H.; Kugo, M.; Iijima, K. Yersinia pseudotuberculosis infection in Kawasaki disease and its clinical characteristics. BMC Pediatrics 2015, 15, 177. [Google Scholar] [CrossRef]
- Chen, M.R.; Kuo, H.C.; Lee, Y.J.; Chi, H.; Li, S.C.; Lee, H.C.; Yang, K.D. Phenotype, Susceptibility, Autoimmunity, and Im-munotherapy Between Kawasaki Disease and Coronavirus Disease-19 Associated Multisystem Inflammatory Syndrome in Children. Front. Immunol. 2021, 12, 632890. [Google Scholar] [CrossRef]
- Jorgensen, I.; Miao, E.A. Pyroptotic cell death defends against intracellular pathogens. Immunol. Rev. 2015, 265, 130–142. [Google Scholar] [CrossRef]
- Evans, P.C.; Rainger, G.E.; Mason, J.C.; Guzik, T.J.; Osto, E.; Stamataki, Z.; Neil, D.; Hoefer, I.E.; Fragiadaki, M.; Waltenberger, J.; et al. Endothelial dysfunction in COVID-19: a position paper of the ESC Working Group for Atherosclerosis and Vascular Biology, and the ESC Council of Basic Cardiovascular Science. Cardiovasc. Res. 2020, 116, 2177–2184. [Google Scholar] [CrossRef] [PubMed]
- Barnett, K.C.; Kagan, J.C. Lipids that directly regulate innate immune signal transduction. Innate. Immun. 2020, 26, 4–14. [Google Scholar] [CrossRef]
- He, Y.E.; Qiu, H.X.; Wu, R.Z.; Rong, X.; Xu, H.T.; Xiang, R.L.; Chu, M.P. Oxidised Low-Density Lipoprotein and Its Receptor-Mediated Endothelial Dysfunction Are Associated with Coronary Artery Lesions in Kawasaki Disease. J. Cardiovasc. Transl. Res. 2020, 13, 204–214. [Google Scholar] [CrossRef]
- Zeng, C.; Wang, R.; Tan, H. Role of Pyroptosis in Cardiovascular Diseases and its Therapeutic Implications. Int. J. Biol. Sci. 2019, 15, 1345–1357. [Google Scholar] [CrossRef]
- Tang, J.; Zhang, Y.; Zhang, X.; Liao, Y.; Wang, Y.; Ouyang, S.; Che, Y.; Xu, M.; Pu, J.; Shen, Q.; et al. RNA gene profile variation in peripheral blood mononuclear cells from rhesus macaques immunized with Hib conjugate vaccine, Hib capsular polysaccharide and TT carrier protein. BMC Immunol. 2018, 19, 4. [Google Scholar] [CrossRef] [PubMed]
- Antas, P.R.Z.; Ponte, C.G.G.; Almeida, M.R.; Albuquerque, L.H.P.; Sousa-Vasconcelos, P.S.; Pedro, T.; Gomes, N.L.S.; Moreira, O.C.; Silva, F.C.; Castello-Branco, L.R.R.; et al. The in vitro Mycobacterium bovis BCG Moreau infection of human monocytes that induces Caspase-1 expression, release and dependent cell death is mostly reliant upon cell integrity. J. Inflamm. (Lond) 2019, 16, 18. [Google Scholar] [CrossRef]
- Ponte, C.; Hacker, M.; Moraes, M.; Castello-Branco, L.; Silva, F.; Antas, P. The patterns of in vitro cell-death and inflammatory cytokines induced by distinct BCG vaccine strains are differentially induced in human mononuclear cells. Hum. Vaccines Immunother. 2018, 14, 28–35. [Google Scholar] [CrossRef] [PubMed]
- HogenEsch, H.; O’Hagan, D.T.; Fox, C.B. Optimizing the utilization of aluminum adjuvants in vaccines: you might just get what you want. NPJ Vaccines 2018, 3, 51. [Google Scholar] [CrossRef]
- Hara, T.; Yamamura, K.; Sakai, Y. The up-to-date pathophysiology of Kawasaki disease. Clin. Transl. Immunol. 2021, 10, e1284. [Google Scholar] [CrossRef]
| Characteristics | KD | (n) | Control | (n) | p |
|---|---|---|---|---|---|
| Age (months) 1 | 6 (2–9) | (102) | 5 (1–9) | (139) | 0.017 2 |
| Sex (male) | 64 (62.7%) | (102) | 77 (55.4%) | (139) | 0.29 3 |
| Breast feeding | 94 (93.1%) | (101) | 120 (87.6%) | (137) | 0.20 3 |
| Baby food | 44 (43.6%) | (101) | 37 (27.0%) | (137) | 0.0088 3 |
| History of allergic disease | 5 (5.0%) | (100) | 18 (13.0%) | (138) | 0.046 3 |
| Food allergy | 2 (2.0%) | (100) | 9 (6.5%) | (138) | 0.13 3 |
| Atopic dermatitis | 3 (3.0%) | (100) | 10 (7.3%) | (138) | 0.25 3 |
| Asthma | 0 (0%) | (100) | 5 (3.6%) | (138) | 0.076 3 |
| Symptoms of infection within 2 months before hospitalization | 29 (29.0%) | (100) | 44 (32.1%) | (137) | 0.70 3 |
| Antibiotic use within 2 months before hospitalization | 16 (15.7%) | (102) | 21 (15.1%) | (139) | 1.00 3 |
| Number of family member living together 1 | 4 (3–11) | (102) | 4 (1–10) | (138) | 0.28 2 |
| Sibling(s) | 57 (55.9%) | (102) | 84 (60.9%) | (138) | 0.51 3 |
| Family history of KD | 6 (6.2%) | (97) | 10 (7.3%) | (137) | 0.80 3 |
| Housing style (detached house) | 33 (32.7%) | (101) | 37 (27.6%) | (134) | 0.47 3 |
| KD (n = 102) | Control (n = 139) | Univariate Analysis | Multivariable Analysis | |||
|---|---|---|---|---|---|---|
| Vaccines | Crude OR (95%CI) | p | Adjusted OR (95%CI) | p | ||
| Vaccines with alum adjuvants | ||||||
| PCV13 | 92 (90.2%) | 115 (82.7%) | 1.92 (0.87–4.22) | 0.10 | 0.98 (0.32–2.95) | 0.97 |
| HBV vaccine | 89 (87.3%) | 110 (79.1%) | 1.80 (0.89–3.68) | 0.10 | 0.78 (0.28–2.17) | 0.64 |
| DPT-IPV | 75 (73.5%) | 98 (70.5%) | 1.16 (0.65–2.06) | 0.60 | 0.39 (0.14–1.09) | 0.07 |
| Vaccines without alum adjuvants | ||||||
| Hib vaccine | 93 (91.2%) | 115 (82.7%) | 2.15 (0.95–4.86) | 0.06 | 1.19 (0.37–3.85) | 0.77 |
| Rotavirus vaccine | 64 (62.7%) | 74 (53.2%) | 1.47 (0.88–2.49) | 0.14 | 1.32 (0.62–2.77) | 0.47 |
| BCG vaccine | 48 (47.1%) | 48 (34.5%) | 1.68 (0.99–2.84) | 0.05 | 0.58 (0.17–1.96) | 0.38 |
| Vaccines | Number of Subjects Who Received Vaccine in the Case Period | Number of Subjects Who Received Vaccine in the Control Period | IRMH | (95%CI) |
|---|---|---|---|---|
| (S) 7 days | ||||
| PCV13 | 9 | 9 | 1.00 | (0.40–2.52) |
| HBV vaccine | 7 | 6 | 1.17 | (0.39–3.47) |
| DPT-IPV | 7 | 5 | 1.40 | (0.44–4.41) |
| Hib vaccine | 9 | 8 | 1.13 | (0.43–2.92) |
| Rotavirus vaccine | 4 | 2 | 2.00 | (0.37–10.92) |
| BCG vaccine | 2 | 3 | 0.67 | (0.11–3.99) |
| (L) 28 days | ||||
| PCV13 | 29 | 33 | 0.88 | (0.53–1.45) |
| HBV vaccine | 24 | 27 | 0.89 | (0.51–1.54) |
| DPT-IPV | 20 | 30 | 0.67 | (0.37–1.17) |
| Hib vaccine | 29 | 33 | 0.88 | (0.53–1.45) |
| Rotavirus vaccine | 15 | 23 | 0.65 | (0.34–1.25) |
| BCG vaccine | 7 | 17 | 0.41 | (0.17–0.99) |
| 2007–2011 | 2014–2018 | p | |
|---|---|---|---|
| Number of patients | |||
| Total of all ages | 11,970 (775) | 16,020 (375) | <0.0001 |
| <1 year old | 3073 (180) | 3161 (111) | 0.38 |
| 0–2 months | 235 (9) | 240 (9) | 0.68 |
| 3–5 months | 839 (52) | 702 (13) | 0.0004 |
| 6–8 months | 997 (66) | 1013 (57) | 0.70 |
| 9–11 months | 1001 (86) | 1206 (62) | 0.0025 |
| Incidence rate 1 | |||
| Total of all ages | 224.6 (16.0) | 324.0 (21.6) | <0.0001 |
| 0–2 months | 87.8 (7.0) | 99.9 (9.1) | 0.046 |
| 3–5 months | 313.4 (21.9) | 291.4 (10.8) | 0.078 |
| 6–8 months | 372.0 (24.6) | 420.6 (28.6) | 0.021 |
| 9–11 months | 373.8 (32.2) | 500.6 (20.7) | < 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Murata, K.; Onoyama, S.; Yamamura, K.; Mizuno, Y.; Furuno, K.; Matsubara, K.; Hatae, K.; Masuda, K.; Nomura, Y.; Ohno, T.; et al. Kawasaki Disease and Vaccination: Prospective Case-Control and Case-Crossover Studies among Infants in Japan. Vaccines 2021, 9, 839. https://doi.org/10.3390/vaccines9080839
Murata K, Onoyama S, Yamamura K, Mizuno Y, Furuno K, Matsubara K, Hatae K, Masuda K, Nomura Y, Ohno T, et al. Kawasaki Disease and Vaccination: Prospective Case-Control and Case-Crossover Studies among Infants in Japan. Vaccines. 2021; 9(8):839. https://doi.org/10.3390/vaccines9080839
Chicago/Turabian StyleMurata, Kenji, Sagano Onoyama, Kenichiro Yamamura, Yumi Mizuno, Kenji Furuno, Keita Matsubara, Ken Hatae, Kiminori Masuda, Yuichi Nomura, Takuro Ohno, and et al. 2021. "Kawasaki Disease and Vaccination: Prospective Case-Control and Case-Crossover Studies among Infants in Japan" Vaccines 9, no. 8: 839. https://doi.org/10.3390/vaccines9080839
APA StyleMurata, K., Onoyama, S., Yamamura, K., Mizuno, Y., Furuno, K., Matsubara, K., Hatae, K., Masuda, K., Nomura, Y., Ohno, T., Kinumaki, A., Miura, M., Sakai, Y., Ohga, S., Fukushima, W., Kishimoto, J., Nakamura, Y., & Hara, T. (2021). Kawasaki Disease and Vaccination: Prospective Case-Control and Case-Crossover Studies among Infants in Japan. Vaccines, 9(8), 839. https://doi.org/10.3390/vaccines9080839






