Predictors of COVID-19 Vaccine Hesitancy: Socio-Demographics, Co-Morbidity, and Past Experience of Racial Discrimination
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient and Public Involvement
2.2. Study Design
2.3. Dependent Variable
2.4. Independent Variables
2.5. Statistical Analyses
3. Results
3.1. Socio-Demographic Characteristics of the Study Population
3.2. Previous COVID-19 Diagnosis, Clinical Risk, and Risk Perceptions
3.3. Past Experience with Discrimination and Vaccine Hesitancy
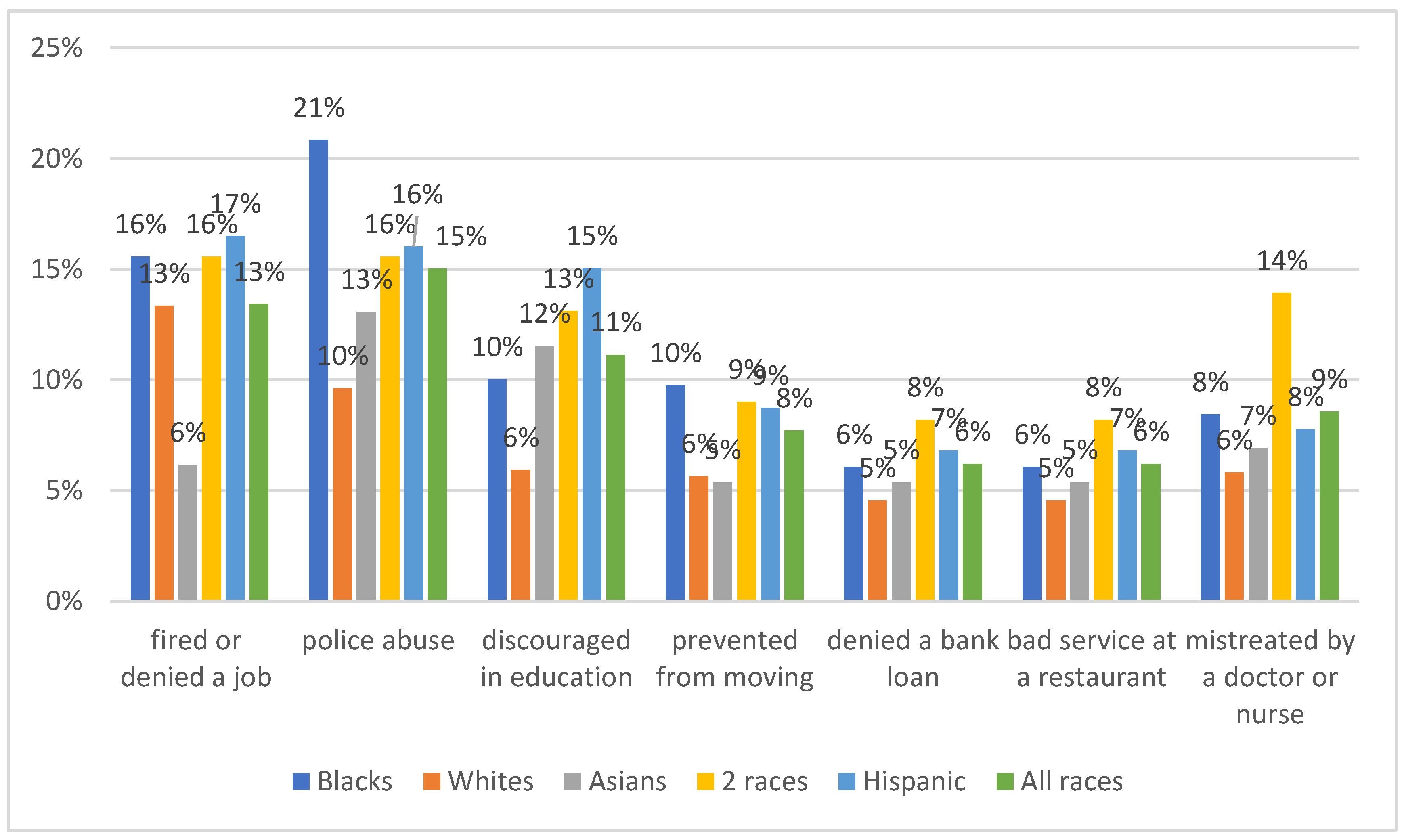
3.4. Logistic Regression Models
4. Discussion
Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fact Sheet: Explaining Operation Warp Speed. Available online: https://www.hhs.gov/coronavirus/explaining-operation-warp-speed/index.html (accessed on 11 January 2021).
- Pfizer and BioNTech Announce Vaccine Candidate against COVID-19 Achieved Success in First Interim Analysis from Phase 3 study. Press Release. 9 November 2020. Available online: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-and-biontech-announce-vaccine-candidate-against (accessed on 8 January 2021).
- Moderna Announces Primary Efficacy Analysis in Phase 3 COVE Study for Its COVID-19 Vaccine Candidate and Filing Today with U.S. FDA for Emergency Use Authorization. Press Release. 30 November 2020. Available online: https://investors.modernatx.com/news-releases/news-release-details/moderna-announces-primary-efficacy-analysis-phase-3-cove-study (accessed on 8 January 2021).
- FDA Takes Key Action in Fight against COVID-19 by Issuing Emergency Use Authorization for First COVID-19 Vaccine. Press Release. 11 December 2020. Available online: https://www.fda.gov/news-events/press-announcements/fda-takes-key-action-fight-against-covid-19-issuing-emergency-use-authorization-first-covid-19 (accessed on 8 January 2021).
- FDA Takes Additional Action in Fight against COVID-19 by Issuing Emergency Use Authorization for Second COVID-19 Vaccine. Press Release. 18 December 2020. Available online: https://www.fda.gov/news-events/press-announcements/fda-takes-additional-action-fight-against-covid-19-issuing-emergency-use-authorization-second-covid (accessed on 8 January 2021).
- COVID-19 Vaccination Program Interim Playbook for Jurisdictional Operations. CDC. 29 October 2020. Version 2.0. Available online: https://www.cdc.gov/vaccines/imz-managers/downloads/COVID-19-Vaccination-Program-Interim_Playbook.pdf (accessed on 11 January 2021).
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef] [PubMed]
- SteelFisher, G.K.; Blendon, R.J.; Caporello, H. An Uncertain Public—Encouraging Acceptance of Covid-19 Vaccines. N. Engl. J. Med. 2021, 384, 1483–1487. [Google Scholar] [CrossRef] [PubMed]
- Jamison, A.M.; Quinn, S.C.; Freimuth, V.S. “You don’t trust a government vaccine”: Narratives of institutional trust and influenza vaccination among African American and white adults. Soc. Sci. Med. 2019, 221, 87–94. [Google Scholar] [CrossRef]
- Hamel, L.; Kirzinger, A.; Munana, C.; Brodie, M. KFF COVID-19 Vaccine Monitor. Press Release. December 2020. Available online: https://www.kff.org/coronavirus-covid-19/report/kff-covid-19-vaccine-monitor-december-2020/?utm_campaign=KFF-2020-polling-surveys&utm_medium=email&_hsmi=2&_hsenc=p2ANqtz-9EpdM8wscJHy__FjpP9PJ67CUSXfk4f_VyZdVC652V5zIy4qBzDeO-0b5iDXeDertNU8W0VOp6xcGENlKJvugasI_0OA&utm_content=2&utm_source=hs_email (accessed on 8 January 2021).
- Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2015–2016 Influenza Season. 2016. Available online: https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm (accessed on 7 July 2021).
- Bleser, W.K.; Miranda, P.Y.; Jean-Jacques, M. Racial/Ethnic Disparities in Influenza Vaccination of Chronically Ill US Adults: The Mediating Role of Perceived Discrimination in Health Care. Med. Care 2016, 54, 570–577. [Google Scholar] [CrossRef] [PubMed]
- Quinn, S.C.; Jamison, A.M.; An, J.; Hancock, G.R.; Freimuth, V.S. Measuring vaccine hesitancy, confidence, trust and flu vaccine uptake: Results of a national survey of White and African American adults. Vaccine 2019, 37, 1168–1173. [Google Scholar] [CrossRef] [PubMed]
- Artiga, S.; Michaud, J.; Kates, J.; Orgera, K. Racial Disparities in Flu Vaccination: Implications for COVID-19 Vaccination Efforts. Available online: https://www.kff.org/policy-watch/racial-disparities-flu-vaccination-implications-covid-19-vaccination-efforts/ (accessed on 8 January 2021).
- Dooling, K.; Marin, M.; Wallace, M.; McClung, N.; Chamberland, M.; Lee, G.; Talbot, H.K.; Romero, J.R.; Bell, B.P.; Oliver, S.E. The Advisory Committee on Immunization Practices’ Updated Interim Recommendation for Allocation of COVID-19 Vaccine—United States, December 2020. MMWR Morb. Mortal. Wkly Rep. 2021, 69, 1657–1660. [Google Scholar] [CrossRef] [PubMed]
- Sternthal, M.J.; Slopen, N.; Williams, D.R. Racial Disparities in Health. Du Bois Rev. Soc. Sci. Res. Race 2011, 8, 95–113. [Google Scholar] [CrossRef] [PubMed]
- Woko, C.; Siegel, L.; Hornik, R. An Investigation of Low COVID-19 Vaccination Intentions among Black Americans: The Role of Behavioral Beliefs and Trust in COVID-19 Information Sources. J. Health Commun. 2020, 25, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Public Health Emergency Preparedness and Response Capabilities. Centers for Disease Control and Prevention. October 2018. Updated January 2019. Available online: https://www.cdc.gov/cpr/readiness/00_docs/CDC_PreparednesResponseCapabilities_October2018_Final_508.pdf (accessed on 11 January 2021).
- Warren, R.C.; Forrow, L.; Hodge, D.A., Sr.; Truog, R.D. Trustworthiness before Trust—Covid-19 Vaccine Trials and the Black Community. N. Engl. J. Med. 2020, 383, e121. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, S.S.; Stanford, F.C. Beyond Tuskegee—Vaccine Distrust and Everyday Racism. N. Engl. J. Med. 2021, 384, e12. [Google Scholar] [CrossRef] [PubMed]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. SAGE Working Group on Vaccine Hesitancy. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Taylor-Clark, K.; Viswanath, K.; Blendon, R. Communication inequalities during Public Health disasters: Katrina’s wake. Health Commun. 2010, 25, 221–229. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Savoia, E.; Agboola, F.; Viswanath, K. What have we learned about communication inequalities during the H1N1 pandemic: A systematic review of the literature. BMC Public Health 2014, 14, 484. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Savoia, E.; Testa, M.A.; Viswanath, K. Predictors of knowledge of H1N1 infection and transmission in the U.S. population. BMC Public Health 2012, 12, 328. [Google Scholar] [CrossRef] [Green Version]
- Blendon, R.J.; Benson, J.M.; Desroches, C.M.; Weldon, K.J. Using opinion surveys to track the public’s response to a bioterrorist attack. J. Health Commun. 2003, 8 (Suppl. 1), 83–92. [Google Scholar] [CrossRef] [PubMed]
- Hand, D.J.; Till, R.J. A Simple Generalization of the Area Under the ROC Curve for Multiple Class Classification Problems. Mach. Learn. 2001, 45, 171–186. [Google Scholar] [CrossRef]
| Age | N (%) |
|---|---|
| 18–24 | 354 (13.4%) |
| 25–34 | 841 (31.7%) |
| 35–44 | 906 (34.2%) |
| 45–54 | 339 (12.8%) |
| 55–64 | 152 (5.7%) |
| 65–74 | 47 (1.8%) |
| ≥75 | 11 (0.4%) |
| Gender | N (%) |
| Male | 1417 (53.5%) |
| Female | 1213 (45.8%) |
| Other | 20 (0.7%) |
| Education | N (%) |
| Less than high school | 92 (3.2%) |
| High school/GED | 539 (20.3%) |
| Some college | 579 (21.9%) |
| Bachelor’s degree | 615 (23.3%) |
| Post-graduate degree | 825 (31.3%) |
| Race | N (%) |
| White, non-Hispanic | 1754 (66.2%) |
| Black, non-Hispanic | 379 (14.3%) |
| Hispanic | 206 (7.8%) |
| Asian, non-Hispanic | 130 (4.9%) |
| 2+ races | 122 (4.6%) |
| Prefer not to say | 40 (1.5%) |
| Other | 19 (0.7%) |
| Employment status | N (%) |
| Paid employee | 2032 (76.7%) |
| Self-employed | 243 (9.2%) |
| On unemployment | 101 (3.8%) |
| Not working-searching for work | 96 (3.6%) |
| On paid leave or furloughed | 41 (1.6%) |
| Retired | 41 (1.6%) |
| Not working-and not looking for a job | 39 (1.4%) |
| On disability or worker’s compensation | 35 (1.3%) |
| Other | 22 (0.8%) |
| Job category (multiple choice question) | N (%) |
| Hospital and emergency department workers | 624 (23.5%) |
| Nursing home, long-term care, and home health care workers | 413 (15.6%) |
| Public health workers | 284 (10.7%) |
| Grocery store workers | 283 (10.7%) |
| Teachers and school staff | 251 (9.5%) |
| Food processing workers | 222 (8.4%) |
| Emergency Medical Services workers | 186 (7.0%) |
| Other health care workers | 170 (6.4%) |
| Volunteer (i.e., CERT, MRC, Red Cross) | 168 (6.3%) |
| Private transportation workers | 156 (5.9%) |
| Sanitation workers | 131 (4.9%) |
| Vaccine manufacturing workers | 121 (4.6%) |
| Postal and shipping workers | 120 (4.5%) |
| Pharmacy workers | 117 (4.4%) |
| Correctional facilities workers | 116 (4.4%) |
| Police or firefighters | 116 (4.4%) |
| Vaccine distribution workers | 95 (3.6%) |
| Other first responders | 93 (3.5%) |
| Public transportation workers | 90 (3.4%) |
| Co-Morbidity (Diabetes, Obesity, Rheumatological Disease, Immunocompromised Status, Cancer, Cardiovascular Disease, Chronic Respiratory Disease) | N (%) |
|---|---|
| No medical condition | 1764 (66.6%) |
| One medical condition | 685 (25.8%) |
| Two or more medical conditions | 201 (7.6%) |
| Have you been diagnosed with COVID-19? | N (%) |
| No | 1961 (74%) |
| I am not sure | 57 (2.2%) |
| Yes, with no symptoms | 266 (10%) |
| Yes, with mild symptoms | 259 (9.8%) |
| Yes, with severe symptoms | 107 (4%) |
| Experience of unfair treatment | N (%) |
| Attributed to any of the following reasons: race, religion, gender and sexual orientation | 1680 (63.4%) |
| Race was the only reason or one of the reasons | 915 (34.5%) |
| Religion was the only reason or one of the reasons | 318 (12%) |
| Gender was the only reason or one of the reasons | 549 (20.7%) |
| Sexual orientation was the only reason or one of the reasons | 361 (13.6%) |
| How concerned are you about any of the following situations? | N (%) |
| Contracting COVID-19 at work? (For example: hospital, office, and other work settings that are not your home) | |
| Very concerned | 1542 (58.3%) |
| Somewhat concerned | 792 (29.9%) |
| Not concerned | 312 (11.8%) |
| Contracting COVID-19 outside of work? (For example: at the grocery store, when you are using transportation, or in other aspects of your daily life) | |
| Very concerned | 1266 (47.9%) |
| Somewhat concerned | 1007 (38.1%) |
| Not concerned | 371 (14%) |
| Infecting your family or friends with COVID-19? | |
| Very concerned | 1653 (62.5%) |
| Somewhat concerned | 664 (25.1%) |
| Not concerned | 326 (12.4%) |
| COVID-19 overall risk perception | N (%) |
| Low risk | 382 (14.5%) |
| Medium risk | 813 (30.1%) |
| High risk | 1439 (54.6%) |
| If you were offered a COVID-19 vaccine within two months from now-at no cost to you- how likely are you to take it? | N (%) |
| Very likely (low hesitancy) | 1059 (40%) |
| Somewhat likely | 523 (19.7%) |
| I would not take it within 2 months but would consider it later on | 188 (7.1%) |
| Not sure | 388 (14.6%) |
| Somewhat unlikely | 153 (5.8%) |
| Very unlikely (high hesitancy) | 339 (12.8%) |
| Simple Models | Multiple Model | |||
|---|---|---|---|---|
| Independent Variable | OR | 95% C.I. | OR | 95% C.I. |
| Age | ||||
| 18–24 | - | - | - | - |
| 25–34 | 1.07 | 0.86–1.34 | - | - |
| 35–44 | 0.99 | 0.80–1.24 | - | - |
| 45–54 | 1.03 | 0.79–1.35 | - | - |
| 55–64 | 0.97 | 0.69–1.36 | - | - |
| 65–74 | 0.75 | 0.43–1.32 | - | - |
| ≥75 | 1.16 | 0.41–3.24 | - | - |
| Gender | ||||
| Female vs. male | 0.85 * | 0.74–0.98 | 0.91 | 0.78–1.05 |
| Other than female or male vs. male | 0.59 | 0.26–1.33 | 0.62 | 0.27–1.42 |
| Employment status | ||||
| Paid employee and self-employed vs. other categories | 1.14 | 0.94–1.39 | - | - |
| Education | ||||
| Less than high school | - | - | - | - |
| High school/GED | 0.78 | 0.52–1.15 | 0.78 | 0.52–1.17 |
| Some college | 0.66 * | 0.44–0.99 | 0.68 | 0.45–1.01 |
| Bachelor’s degree | 0.77 | 0.52–1.13 | 0.78 | 0.52–1.16 |
| Post-graduate degree | 0.97 | 0.66–1.43 | 0.95 | 0.64–1.40 |
| Race | ||||
| White non-Hispanic vs. all other races | 0.94 | 0.81–1.1 | - | - |
| Black non-Hispanic vs. all other races | 1.22 * | 1.00–1.48 | 1.18 | 0.96–1.44 |
| Asian non-Hispanic vs. all other races | 0.87 | 0.63–1.20 | - | - |
| Hispanic vs. all other races | 0.92 | 0.71–1.20 | - | - |
| Type of job | ||||
| Healthcare sector employee vs. other job categories | 1.09 | 0.94–1.25 | - | - |
| Medical conditions | ||||
| No medical condition | - | - | - | - |
| One medical condition | 1.06 | 0.90–1.24 | - | - |
| Two medical conditions | 1.23 | 0.90–1.69 | - | - |
| Three or more medical conditions | 0.75 | 0.46–1.22 | ||
| Risk perception | ||||
| Low risk perception | - | - | - | - |
| Medium risk perception | 1.14 | 0.92–1.42 | 1.10 | 0.88–1.38 |
| High risk perception | 1.30 * | 1.06–1.60 | 1.18 | 0.95–1.47 |
| COVID-19 diagnosis | ||||
| No diagnosis | - | - | - | - |
| Not sure | 1.05 | 0.65–1.68 | 1.01 | 0.62–1.63 |
| Yes–no symptoms | 1.02 | 0.81–1.29 | 0.89 | 0.69–1.13 |
| Yes–mild symptoms | 1.13 | 0.89–1.43 | 1.02 | 0.80–1.29 |
| Yes–severe symptoms | 1.42 * | 1.01–1.99 | 1.27 | 0.90–1.79 |
| Experience of unfair treatment | ||||
| Attributed to any of the following reasons: race, religion, gender or sexual orientation | 1.19 * | 1.03–1.37 | 0.97 | 0.82–1.16 |
| Race was the only reason or one of the reasons | 1.30 ** | 1.12–1.50 | 1.21 * | 1.01–1.45 |
| Religion was the only reason or one of the reasons | 1.21 | 0.98–1.49 | - | - |
| Gender was the only reason or one of the reasons | 0.97 | 0.83–1.14 | - | - |
| Sexual orientation was the only reason or one of the reasons | 0.97 | 0.80–1.19 | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savoia, E.; Piltch-Loeb, R.; Goldberg, B.; Miller-Idriss, C.; Hughes, B.; Montrond, A.; Kayyem, J.; Testa, M.A. Predictors of COVID-19 Vaccine Hesitancy: Socio-Demographics, Co-Morbidity, and Past Experience of Racial Discrimination. Vaccines 2021, 9, 767. https://doi.org/10.3390/vaccines9070767
Savoia E, Piltch-Loeb R, Goldberg B, Miller-Idriss C, Hughes B, Montrond A, Kayyem J, Testa MA. Predictors of COVID-19 Vaccine Hesitancy: Socio-Demographics, Co-Morbidity, and Past Experience of Racial Discrimination. Vaccines. 2021; 9(7):767. https://doi.org/10.3390/vaccines9070767
Chicago/Turabian StyleSavoia, Elena, Rachael Piltch-Loeb, Beth Goldberg, Cynthia Miller-Idriss, Brian Hughes, Alberto Montrond, Juliette Kayyem, and Marcia A. Testa. 2021. "Predictors of COVID-19 Vaccine Hesitancy: Socio-Demographics, Co-Morbidity, and Past Experience of Racial Discrimination" Vaccines 9, no. 7: 767. https://doi.org/10.3390/vaccines9070767
APA StyleSavoia, E., Piltch-Loeb, R., Goldberg, B., Miller-Idriss, C., Hughes, B., Montrond, A., Kayyem, J., & Testa, M. A. (2021). Predictors of COVID-19 Vaccine Hesitancy: Socio-Demographics, Co-Morbidity, and Past Experience of Racial Discrimination. Vaccines, 9(7), 767. https://doi.org/10.3390/vaccines9070767





