Microparticles and Nanoparticles from Plants—The Benefits of Bioencapsulation
Abstract
1. Introduction
2. The Benefits of Encapsulation and Particulate Formulations
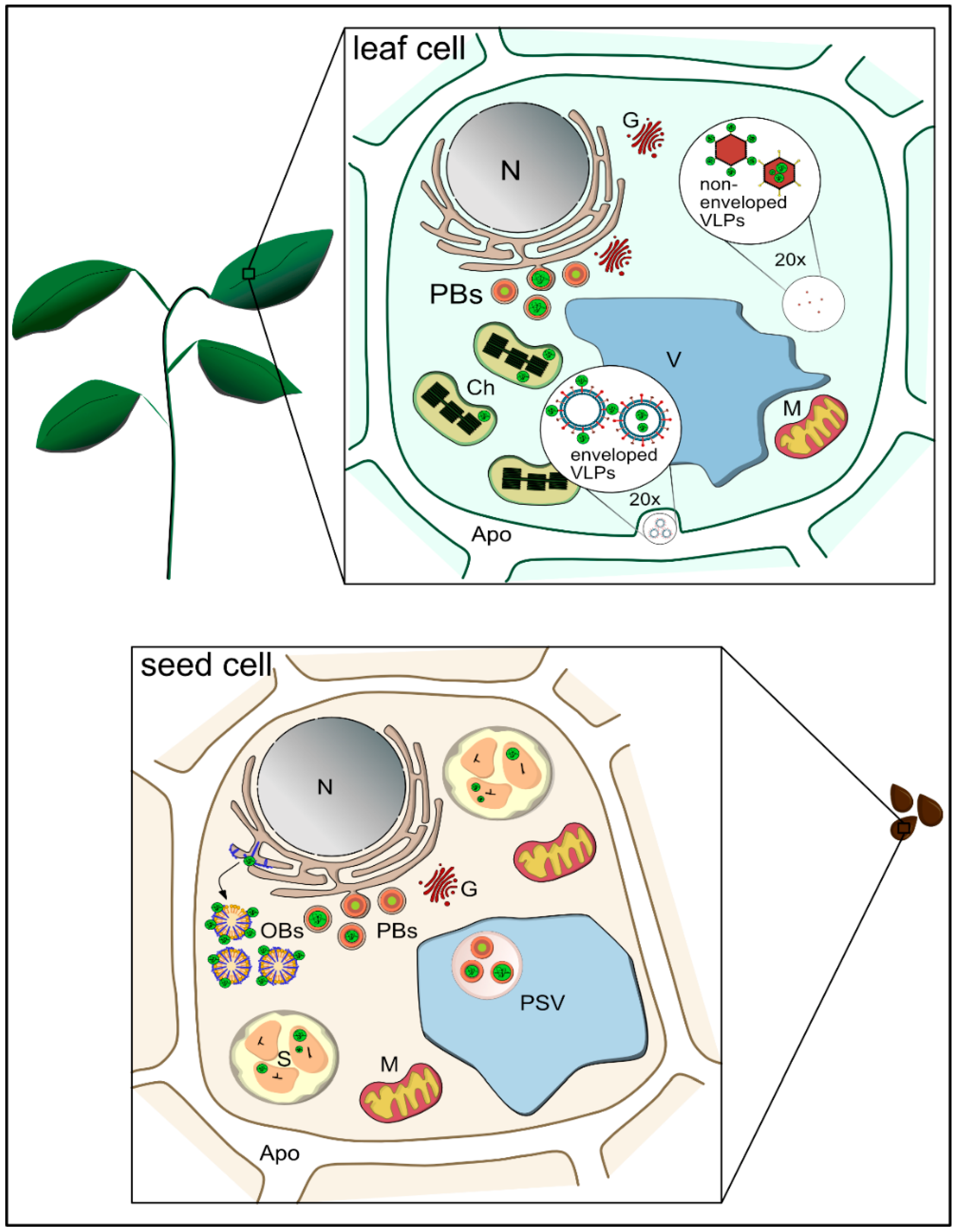
3. Plants as a Means to Achieve Bioencapsulation
4. Plant-Derived Microparticles: Storage Organelles for Bioencapsulation
4.1. Encapsulation in Protein Bodies
4.2. Oleosin-Targeted Deposition
4.3. Deposition in Starch Granules
5. Plant-Derived Nanoparticles
5.1. Animal-Derived VLPs Expressed in Plants
| Virus-Like Particles | Expression System | Size | In Vivo Studies | Ref. |
|---|---|---|---|---|
| Enveloped | Tobacco | 0.05–0.150 | Immunization against H5/H1 | [123] |
| Tobacco | 0.025–0.04 | Immunization against dengue viral protein | [124,125] | |
| Tobacco | ~0.1 | Immunization against SARS-CoV-2 | [56] | |
| Non-enveloped | Cowpea | 0.030 | Adjuvant in anti-cancer vaccines | [126,127] |
| Tobacco | 0.07 | Immunization against African horse sickness | [128,129] | |
| Tobacco | 0.016 | Immunization against PCV-2 | [130] | |
| Tobacco | 0.025–0.039 | Immunization against various HPV types | [117] | |
| Tobacco | 0.025–0.03 | Immunization against VNN | [131] | |
| Tobacco | ~0.03 | Enhanced immunogenicity of ZE3 antigen via RIC vaccine platform | [132] | |
| Tobacco | 0.025–0.03 | Immunization against WNV | [133] |
5.2. Plant-Derived VLPs and Viral Nanoparticles
6. Remaining Challenges
7. Conclusions and Perspectives
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anselmo, A.C.; Gokarn, Y.; Mitragotri, S. Non-invasive delivery strategies for biologics. Nat. Rev. Drug Discov. 2019, 18, 19–40. [Google Scholar] [CrossRef] [PubMed]
- Sahni, N.; Cheng, Y.; Middaugh, C.R.; Volkin, D.B. Vaccine Delivery. In Drug Delivery, 2nd ed.; Wang, B., Hu, L., Siahaan, T.J., Eds.; John Wiley & Sons Inc.: Hoboken, NJ, USA, 2016; pp. 623–654. [Google Scholar] [CrossRef]
- Jones, D.; Caballero, S.; Davidov-Pardo, G. Bioavailability of nanotechnology-based bioactives and nutraceuticals. Adv. Food Nutr. Res. 2019, 88, 235–273. [Google Scholar] [CrossRef] [PubMed]
- Yeung, A.W.K.; Souto, E.B.; Durazzo, A.; Lucarini, M.; Novellino, E.; Tewari, D.; Wang, D.; Atanasov, A.G.; Santini, A. Big impact of nanoparticles: Analysis of the most cited nanopharmaceuticals and nanonutraceuticals research. Curr. Res. Biotechnol. 2020, 2, 53–63. [Google Scholar] [CrossRef]
- Souto, E.B.; Zielinska, A.; Souto, S.B.; Durazzo, A.; Lucarini, M.; Santini, A.; Silva, A.M.; Atanasov, A.G.; Marques, C.; Andrade, L.N.; et al. (+)-Limonene 1,2-Epoxide-Loaded SLNs: Evaluation of Drug Release, Antioxidant Activity, and Cytotoxicity in an HaCaT Cell Line. Int. J. Mol. Sci. 2020, 21, 449. [Google Scholar] [CrossRef]
- Boyd, B.J. Past and future evolution in colloidal drug delivery systems. Expert Opin. Drug Deliv. 2008, 5, 69–85. [Google Scholar] [CrossRef]
- Perry, S.L.; McClements, D.J. Recent advances in encapsulation, protection, and oral delivery of bioactive proteins and peptides using colloidal systems. Molecules 2020, 25, 1161. [Google Scholar] [CrossRef]
- John, R.P.; Tyagi, R.D.; Brar, S.K.; Surampalli, R.Y.; Prevost, D. Bio-encapsulation of microbial cells for targeted agricultural delivery. Crit. Rev. Biotechnol. 2011, 31, 211–226. [Google Scholar] [CrossRef]
- Majewski, R.L.; Zhang, W.; Ma, X.; Cui, Z.; Ren, W.; Markel, D.C. Bioencapsulation technologies in tissue engineering. J. Appl. Biomater. Funct. Mater. 2016, 14, e395–e403. [Google Scholar] [CrossRef]
- Raave, R.; van Kuppevelt, T.H.; Daamen, W.F. Chemotherapeutic drug delivery by tumoral extracellular matrix targeting. J. Control. Release 2018, 274, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Sutradhar, K.B.; Amin, M.L. Nanotechnology in Cancer Drug Delivery and Selective Targeting. ISRN Nanotechnol. 2014, 2014, 1–12. [Google Scholar] [CrossRef]
- Daniell, H.; Kulis, M.; Herzog, R.W. Plant cell-made protein antigens for induction of Oral tolerance. Biotechnol. Adv. 2019, 37, 107413. [Google Scholar] [CrossRef]
- Snapper, C.M. Distinct Immunologic Properties of Soluble Versus Particulate Antigens. Front. Immunol. 2018, 9, 598. [Google Scholar] [CrossRef]
- Zhu, M.; Wang, R.; Nie, G. Applications of nanomaterials as vaccine adjuvants. Hum. Vaccines Immunother. 2014, 10, 2761–2774. [Google Scholar] [CrossRef] [PubMed]
- Jiao, Q.; Li, L.; Mu, Q.; Zhang, Q. Immunomodulation of nanoparticles in nanomedicine applications. Biomed. Res. Int. 2014, 2014, 426028. [Google Scholar] [CrossRef]
- Torres, F.G.; Troncoso, O.P.; Pisani, A.; Gatto, F.; Bardi, G. Natural Polysaccharide Nanomaterials: An Overview of Their Immunological Properties. Int. J. Mol. Sci. 2019, 20, 92. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Jang, Y.S. The development of mucosal vaccines for both mucosal and systemic immune induction and the roles played by adjuvants. Clin. Exp. Vaccine Res. 2017, 6, 15–21. [Google Scholar] [CrossRef]
- Zhu, Q.; Berzofsky, J.A. Oral vaccines: Directed safe passage to the front line of defense. Gut Microbes 2013, 4, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Shim, S.; Yoo, H.S. The Application of Mucoadhesive Chitosan Nanoparticles in Nasal Drug Delivery. Mar. Drugs 2020, 18, 605. [Google Scholar] [CrossRef] [PubMed]
- Lima, I.A.; Khalil, N.M.; Tominaga, T.T.; Lechanteur, A.; Sarmento, B.; Mainardes, R.M. Mucoadhesive chitosan-coated PLGA nanoparticles for oral delivery of ferulic acid. Artif. Cells Nanomed. Biotechnol. 2018, 46, 993–1002. [Google Scholar] [CrossRef] [PubMed]
- Topp, E.; Irwin, R.; McAllister, T.; Lessard, M.; Joensuu, J.J.; Kolotilin, I.; Conrad, U.; Stoger, E.; Mor, T.; Warzecha, H.; et al. The case for plant-made veterinary immunotherapeutics. Biotechnol. Adv. 2016, 34, 597–604. [Google Scholar] [CrossRef] [PubMed]
- Mohan, T.; Berman, Z.; Luo, Y.; Wang, C.; Wang, S.; Compans, R.W.; Wang, B.Z. Chimeric virus-like particles containing influenza HA antigen and GPI-CCL28 induce long-lasting mucosal immunity against H3N2 viruses. Sci. Rep. 2017, 7, 40226. [Google Scholar] [CrossRef]
- Vacher, G.; Kaeser, M.D.; Moser, C.; Gurny, R.; Borchard, G. Recent advances in mucosal immunization using virus-like particles. Mol. Pharm. 2013, 10, 1596–1609. [Google Scholar] [CrossRef] [PubMed]
- Kwon, K.C.; Daniell, H. Oral Delivery of Protein Drugs Bioencapsulated in Plant Cells. Mol. Ther. 2016, 24, 1342–1350. [Google Scholar] [CrossRef] [PubMed]
- Stoger, E.; Ma, J.K.; Fischer, R.; Christou, P. Sowing the seeds of success: Pharmaceutical proteins from plants. Curr. Opin. Biotechnol. 2005, 16, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Shukla, R.; Cheryan, M. Zein: The industrial protein from corn. Ind. Crop. Prod. 2001, 13, 171–192. [Google Scholar] [CrossRef]
- Patel, A.; Hu, Y.; Tiwari, J.K.; Velikov, K.P. Synthesis and characterisation of zein–curcumin colloidal particles. Soft Matter 2010, 6. [Google Scholar] [CrossRef]
- Karthikeyan, K.; Vijayalakshmi, E.; Korrapati, P.S. Selective interactions of zein microspheres with different class of drugs: An in vitro and in silico analysis. AAPS PharmSciTech 2014, 15, 1172–1180. [Google Scholar] [CrossRef]
- Penalva, R.; Gonzalez-Navarro, C.J.; Gamazo, C.; Esparza, I.; Irache, J.M. Zein nanoparticles for oral delivery of quercetin: Pharmacokinetic studies and preventive anti-inflammatory effects in a mouse model of endotoxemia. Nanomedicine 2017, 13, 103–110. [Google Scholar] [CrossRef]
- Luo, Y.; Zhang, B.; Whent, M.; Yu, L.L.; Wang, Q. Preparation and characterization of zein/chitosan complex for encapsulation of alpha-tocopherol, and its in vitro controlled release study. Colloids Surf. B Biointerfaces 2011, 85, 145–152. [Google Scholar] [CrossRef]
- Troncoso, O.P.; Torres, F.G. Non-conventional starch nanoparticles for drug delivery applications. Med. Devices Sens. 2020, 3. [Google Scholar] [CrossRef]
- Moreno-Mendieta, S.; Barrios-Payan, J.; Mata-Espinosa, D.; Sanchez, S.; Hernandez-Pando, R.; Rodriguez-Sanoja, R. Raw starch microparticles have immunostimulant activity in mice vaccinated with BCG and challenged with Mycobacterium tuberculosis. Vaccine 2017, 35, 5123–5130. [Google Scholar] [CrossRef]
- Qiu, C.; Wang, C.; Gong, C.; McClements, D.J.; Jin, Z.; Wang, J. Advances in research on preparation, characterization, interaction with proteins, digestion and delivery systems of starch-based nanoparticles. Int. J. Biol. Macromol. 2020, 152, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Mackenzie, G.; Boa, A.N.; Diego-Taboada, A.; Atkin, S.L.; Sathyapalan, T. Sporopollenin, The Least Known Yet Toughest Natural Biopolymer. Front. Mater. 2015, 2. [Google Scholar] [CrossRef]
- Yilmaz, E. Enantioselective enzymatic hydrolysis of racemic drugs by encapsulation in sol-gel magnetic sporopollenin. Bioprocess. Biosyst. Eng. 2012, 35, 493–502. [Google Scholar] [CrossRef] [PubMed]
- Diego-Taboada, A.; Cousson, P.; Raynaud, E.; Huang, Y.; Lorch, M.; Binks, B.P.; Queneau, Y.; Boa, A.N.; Atkin, S.L.; Beckett, S.T.; et al. Sequestration of edible oil from emulsions using new single and double layered microcapsules from plant spores. J. Mater. Chem. 2012, 22. [Google Scholar] [CrossRef]
- Lale, S.V.; Gill, H.S. Pollen grains as a novel microcarrier for oral delivery of proteins. Int. J. Pharm. 2018, 552, 352–359. [Google Scholar] [CrossRef]
- Uddin, M.J.; Gill, H.S. Ragweed pollen as an oral vaccine delivery system: Mechanistic insights. J. Control. Release 2017, 268, 416–426. [Google Scholar] [CrossRef]
- Hiatt, A.; Caffferkey, R.; Bowdish, K. Production of antibodies in transgenic plants. Nature 1989, 342, 76–78. [Google Scholar] [CrossRef]
- Sijmons, P.; Dekker, B.; Schrammeijer, B.; Verwoerd, T.; van den Elzen, P.; Hoekema, A. Production of correctly processed human serum albumin in transgenic plants. Biotechnology 1990, 8, 217–221. [Google Scholar] [CrossRef]
- Haq, T.; Mason, H.; Clements, J.; Arntzen, C.J. Oral immunization with a recombinant bacterial antigen produced in transgenic plants. Science 1995, 268, 714–716. [Google Scholar] [CrossRef]
- Tacket, C.; Mason, H.; Losonsky, G.; Clements, J.D.; Levine, M.M.; Arntzen, C.J. Immunogenicity in humans of a recombinant bacterial antigen delivered in a transgenic potato. Nat. Med. 1998, 4, 607–609. [Google Scholar] [CrossRef]
- Richter, L.J.; Thanavala, Y.; Arntzen, C.J.; Mason, H.S. Production of hepatitis B surface antigen in transgenic plants for oral immunization. Nat. Biotechnol. 2000, 18, 1167–1171. [Google Scholar] [CrossRef]
- Daniell, H.; Mangu, V.; Yakubov, B.; Park, J.; Habibi, P.; Shi, Y.; Gonnella, P.A.; Fisher, A.; Cook, T.; Zeng, L.; et al. Investigational new drug enabling angiotensin oral-delivery studies to attenuate pulmonary hypertension. Biomaterials 2020, 233, 119750. [Google Scholar] [CrossRef]
- Herzog, R.W.; Nichols, T.C.; Su, J.; Zhang, B.; Sherman, A.; Merricks, E.P.; Raymer, R.; Perrin, G.Q.; Hager, M.; Wiinberg, B.; et al. Oral Tolerance Induction in Hemophilia B Dogs Fed with Transplastomic Lettuce. Mol. Ther. 2017, 25, 512–522. [Google Scholar] [CrossRef]
- Su, J.; Zhu, L.; Sherman, A.; Wang, X.; Lin, S.; Kamesh, A.; Norikane, J.H.; Streatfield, S.J.; Herzog, R.W.; Daniell, H. Low cost industrial production of coagulation factor IX bioencapsulated in lettuce cells for oral tolerance induction in hemophilia B. Biomaterials 2015, 70, 84–93. [Google Scholar] [CrossRef] [PubMed]
- Fischer, R.; Buyel, J.F. Molecular farming—The slope of enlightenment. Biotechnol. Adv. 2020, 40, 107519. [Google Scholar] [CrossRef]
- Bock, R. Transgenic plastids in basic research and plant biotechnology. J. Mol. Biol. 2001, 312, 425–438. [Google Scholar] [CrossRef] [PubMed]
- Daniell, H.; Chan, H.T.; Pasoreck, E.K. Vaccination via Chloroplast Genetics: Affordable Protein Drugs for the Prevention and Treatment of Inherited or Infectious Human Diseases. Annu. Rev. Genet. 2016, 50, 595–618. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Yan, G.; Kwon, K.C.; Liu, M.; Gonnella, P.A.; Yang, S.; Daniell, H. Oral delivery of novel human IGF-1 bioencapsulated in lettuce cells promotes musculoskeletal cell proliferation, differentiation and diabetic fracture healing. Biomaterials 2020, 233, 119591. [Google Scholar] [CrossRef]
- Daniell, H.; Rai, V.; Xiao, Y. Cold chain and virus-free oral polio booster vaccine made in lettuce chloroplasts confers protection against all three poliovirus serotypes. Plant. Biotechnol. J. 2019, 17, 1357–1368. [Google Scholar] [CrossRef]
- Van Eerde, A.; Gottschamel, J.; Bock, R.; Hansen, K.E.A.; Munang’andu, H.M.; Daniell, H.; Liu Clarke, J. Production of tetravalent dengue virus envelope protein domain III based antigens in lettuce chloroplasts and immunologic analysis for future oral vaccine development. Plant. Biotechnol. J. 2019, 17, 1408–1417. [Google Scholar] [CrossRef]
- Tregoning, J.S.; Nixon, P.; Kuroda, H.; Svab, Z.; Clare, S.; Bowe, F.; Fairweather, N.; Ytterberg, J.; van Wijk, K.J.; Dougan, G.; et al. Expression of tetanus toxin Fragment C in tobacco chloroplasts. Nucleic Acids Res. 2003, 31, 1174–1179. [Google Scholar] [CrossRef] [PubMed]
- Lakshmi, P.S.; Verma, D.; Yang, X.; Lloyd, B.; Daniell, H. Low cost tuberculosis vaccine antigens in capsules: Expression in chloroplasts, bio-encapsulation, stability and functional evaluation in vitro. PLoS ONE 2013, 8, e54708. [Google Scholar] [CrossRef] [PubMed]
- Ward, B.J.; Makarkov, A.; Séguin, A.; Pillet, S.; Trépanier, S.; Dhaliwall, J.; Libman, M.D.; Vesikari, T.; Landry, N. Efficacy, immunogenicity, and safety of a plant-derived, quadrivalent, virus-like particle influenza vaccine in adults (18–64 years) and older adults (≥65 years): Two multicentre, randomised phase 3 trials. Lancet 2020, 396, 1491–1503. [Google Scholar] [CrossRef]
- Ward, B.J.; Gobeil, P.; Séguin, A.; Atkins, J.; Boulay, I.; Charbonneau, P.-Y.; Couture, M.; D’Aoust, M.-A.; Dhaliwall, J.; Finkle, C.; et al. Phase 1 trial of a Candidate Recombinant Virus-Like Particle Vaccine for Covid-19 Disease Produced in Plants. medRxiv 2020. [Google Scholar] [CrossRef]
- Capell, T.; Twyman, R.M.; Armario-Najera, V.; Ma, J.K.; Schillberg, S.; Christou, P. Potential Applications of Plant Biotechnology against SARS-CoV-2. Trends Plant. Sci. 2020, 25, 635–643. [Google Scholar] [CrossRef]
- Rybicki, E.P. Plant molecular farming of virus-like nanoparticles as vaccines and reagents. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2020, 12, e1587. [Google Scholar] [CrossRef]
- Vamvaka, E.; Arcalis, E.; Ramessar, K.; Evans, A.; O’Keefe, B.R.; Shattock, R.J.; Medina, V.; Stoger, E.; Christou, P.; Capell, T. Rice endosperm is cost-effective for the production of recombinant griffithsin with potent activity against HIV. Plant. Biotechnol. J. 2016, 14, 1427–1437. [Google Scholar] [CrossRef]
- Juarez, P.; Presa, S.; Espi, J.; Pineda, B.; Anton, M.T.; Moreno, V.; Buesa, J.; Granell, A.; Orzaez, D. Neutralizing antibodies against rotavirus produced in transgenically labelled purple tomatoes. Plant. Biotechnol. J. 2012, 10, 341–352. [Google Scholar] [CrossRef]
- Nandi, S.; Yalda, D.; Lu, S.; Nikolov, Z.; Misaki, R.; Fujiyama, K.; Huang, N. Process development and economic evaluation of recombinant human lactoferrin expressed in rice grain. Transgenic Res. 2005, 14, 237–249. [Google Scholar] [CrossRef]
- Takaiwa, F.; Wakasa, Y.; Hayashi, S.; Kawakatsu, T. An overview on the strategies to exploit rice endosperm as production platform for biopharmaceuticals. Plant. Sci. 2017, 263, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Takaiwa, F.; Yang, L.; Takagi, H.; Maruyama, N.; Wakasa, Y.; Ozawa, K.; Hiroi, T. Development of Rice-Seed-Based Oral Allergy Vaccines Containing Hypoallergenic Japanese Cedar Pollen Allergen Derivatives for Immunotherapy. J. Agric. Food Chem. 2019, 67, 13127–13138. [Google Scholar] [CrossRef] [PubMed]
- Hofbauer, A.; Melnik, S.; Tschofen, M.; Arcalis, E.; Phan, H.T.; Gresch, U.; Lampel, J.; Conrad, U.; Stoger, E. The Encapsulation of Hemagglutinin in Protein Bodies Achieves a Stronger Immune Response in Mice than the Soluble Antigen. Front. Plant. Sci. 2016, 7, 142. [Google Scholar] [CrossRef]
- Van Zyl, A.R.; Meyers, A.E.; Rybicki, E.P. Development of plant-produced protein body vaccine candidates for bluetongue virus. BMC Biotechnol. 2017, 17, 47. [Google Scholar] [CrossRef] [PubMed]
- Cai, J.; Wen, R.; Li, W.; Wang, X.; Tian, H.; Yi, S.; Zhang, L.; Li, X.; Jiang, C.; Li, H. Oil body bound oleosin-rhFGF9 fusion protein expressed in safflower (Carthamus tinctorius L.) stimulates hair growth and wound healing in mice. BMC Biotechnol. 2018, 18, 51. [Google Scholar] [CrossRef] [PubMed]
- Qiang, W.; Zhou, T.; Lan, X.; Zhang, X.; Guo, Y.; Noman, M.; Du, L.; Zheng, J.; Li, W.; Li, H.; et al. A new nanoscale transdermal drug delivery system: Oil body-linked oleosin-hEGF improves skin regeneration to accelerate wound healing. J. Nanobiotechnol. 2018, 16, 62. [Google Scholar] [CrossRef]
- Chikwamba, R.K.; Scott, M.P.; Mejía, L.B.; Mason, H.S.; Wang, K. Localization of a bacterial protein in starch granules of transgenic maize kernels. Proc. Natl. Acad. Sci. USA 2003, 100, 11127–11132. [Google Scholar] [CrossRef]
- Dauvillee, D.; Delhaye, S.; Gruyer, S.; Slomianny, C.; Moretz, S.E.; d’Hulst, C.; Long, C.A.; Ball, S.G.; Tomavo, S. Engineering the chloroplast targeted malarial vaccine antigens in Chlamydomonas starch granules. PLoS ONE 2010, 5, e15424. [Google Scholar] [CrossRef]
- Vitale, A.; Raikhel, N. What do proteins need to reach different vacuoles? Trends Plant. Sci. 1999, 4, 149–155. [Google Scholar] [CrossRef]
- Peters, J.; Stoger, E. Transgenic crops for the production of recombinant vaccines and anti-microbial antibodies. Hum. Vaccines 2011, 7, 367–374. [Google Scholar] [CrossRef] [PubMed]
- Arcalis, E.; Ibl, V.; Peters, J.; Melnik, S.; Stoger, E. The dynamic behavior of storage organelles in developing cereal seeds and its impact on the production of recombinant proteins. Front. Plant. Sci. 2014, 5, 439. [Google Scholar] [CrossRef]
- Canonica, G.W.; Passalacqua, G. Noninjection routes for immunotherapy. J. Allergy. Clin. Immunol. 2003, 111, 437–448. [Google Scholar] [CrossRef]
- Takagi, H.; Hiroi, T.; Hirose, S.; Yang, L.; Takaiwa, F. Rice seed ER-derived protein body as an efficient delivery vehicle for oral tolerogenic peptides. Peptides 2010, 31, 1421–1425. [Google Scholar] [CrossRef]
- Herman, E.M.; Larkins, B.A. Protein storage bodies and vacuoles. Plant. Cell 1999, 11, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Argos, P.; Pedersen, K.; Marks, M.D.; Larkins, B.A. A structural model for maize zein proteins. J. Biol. Chem. 1982, 257, 9984–9990. [Google Scholar] [CrossRef]
- Llop-Tous, I.; Madurga, S.; Giralt, E.; Marzabal, P.; Torrent, M.; Ludevid, M.D. Relevant elements of a maize gamma-zein domain involved in protein body biogenesis. J. Biol. Chem. 2010, 285, 35633–35644. [Google Scholar] [CrossRef]
- Shewry, P.R.; Napier, J.A.; Tatham, A.S. Seed Storage Proteins: Structures and Biosynthesis. Plant. Cell 1995, 7, 945–956. [Google Scholar] [CrossRef] [PubMed]
- Woo, Y.M.; Hu, D.W.; Larkins, B.A.; Jung, R. Genomics analysis of genes expressed in maize endosperm identifies novel seed proteins and clarifies patterns of zein gene expression. Plant. Cell 2001, 13, 2297–2317. [Google Scholar] [CrossRef] [PubMed]
- Geli, M.I.; Torrent, M.; Ludevid, D. Two Structural Domains Mediate Two Sequential Events in [gamma]-Zein Targeting: Protein Endoplasmic Reticulum Retention and Protein Body Formation. Plant. Cell 1994, 6, 1911–1922. [Google Scholar] [CrossRef]
- Torrent, M.; Llompart, B.; Lasserre-Ramassamy, S.; Llop-Tous, I.; Bastida, M.; Marzabal, P.; Westerholm-Parvinen, A.; Saloheimo, M.; Heifetz, P.B.; Ludevid, M.D. Eukaryotic protein production in designed storage organelles. BMC Biol. 2009, 7, 5. [Google Scholar] [CrossRef]
- Heifetz, P.B.; Royo, B.L.; Luna, P.M.; Virgili, M.B.; Mugica, M.D.L.; Quetglas, M.T.; O’Connor, K.J.; Bergwerf, R.P.; Tous, M.I.I. Production of Biologically Active Proteins. Patent EP 2 351 834 A2, 26 May 2015. [Google Scholar]
- Ludevid, D.; Torrent, M.; Lasserre-Ramassamy, S. Production of Peptides and Proteins by Accumulation in Plant Endoplasmic Reticulum-Derived Protein Bodies. Patent WO/2004/003207, 8 January 2004. [Google Scholar]
- Torrent, M.; Llop-Tous, I.; Ludevid, M.D. Protein body induction: A new tool to produce and recover recombinant proteins in plants. Methods Mol. Biol. 2009, 483, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Yuan, L.; Chen, H.; Sato, S.J.; Clemente, T.E.; Holding, D.R. Nonredundant function of zeins and their correct stoichiometric ratio drive protein body formation in maize endosperm. Plant. Physiol. 2013, 162, 1359–1369. [Google Scholar] [CrossRef] [PubMed]
- Whitehead, M.; Ohlschlager, P.; Almajhdi, F.N.; Alloza, L.; Marzabal, P.; Meyers, A.E.; Hitzeroth, I.I.; Rybicki, E.P. Human papillomavirus (HPV) type 16 E7 protein bodies cause tumour regression in mice. BMC Cancer 2014, 14, 367. [Google Scholar] [CrossRef]
- Fernandez-Carneado, J.; Kogan, M.J.; Castel, S.; Giralt, E. Potential peptide carriers: Amphipathic proline-rich peptides derived from the N-terminal domain of gamma-zein. Angew. Chem. Int. Ed. Engl. 2004, 43, 1811–1814. [Google Scholar] [CrossRef]
- Kogan, M.J.; Dalcol, I.; Gorostiza, P.; Lopez-Iglesias, C.; Pons, M.; Sanz, F.; Ludevid, D.; Giralt, E. Self-assembly of the amphipathic helix (VHLPPP)8. A mechanism for zein protein body formation. J. Mol. Biol. 2001, 312, 907–913. [Google Scholar] [CrossRef]
- Schwestka, J.; Tschofen, M.; Vogt, S.; Marcel, S.; Grillari, J.; Raith, M.; Swoboda, I.; Stoger, E. Plant-derived protein bodies as delivery vehicles for recombinant proteins into mammalian cells. Biotechnol. Bioeng. 2020, 117, 1037–1047. [Google Scholar] [CrossRef]
- De Virgilio, M.; De Marchis, F.; Bellucci, M.; Mainieri, D.; Rossi, M.; Benvenuto, E.; Arcioni, S.; Vitale, A. The human immunodeficiency virus antigen Nef forms protein bodies in leaves of transgenic tobacco when fused to zeolin. J. Exp. Bot. 2008, 59, 2815–2829. [Google Scholar] [CrossRef]
- Frandsen, G.I.; Mundy, J.; Tzen, J.T. Oil bodies and their associated proteins, oleosin and caleosin. Physiol. Plant. 2001, 112, 301–307. [Google Scholar] [CrossRef] [PubMed]
- Ling, H. Oleosin fusion expression systems for the production of recombinant proteins. Biologia 2007, 62. [Google Scholar] [CrossRef]
- Wahlroos, T.; Soukka, J.; Denesyuk, A.; Wahlroos, R.; Korpela, T.; Kilby, N.J. Oleosin expression and trafficking during oil body biogenesis in tobacco leaf cells. Genesis 2003, 35, 125–132. [Google Scholar] [CrossRef]
- Tzen, J.T.C. Integral Proteins in Plant Oil Bodies. Int. Sch. Res. Not. Bot. 2012, 2012, 1–16. [Google Scholar] [CrossRef]
- Parmenter, D.L.; Boothe, J.G.; van Rooijen, G.J.H.; Yeung, E.C.; Moloney, M.M. Production of biologically active hirudin in plant seeds using oleosin partitioning. Plant. Mol. Biol. 1995, 29, 1167–1180. [Google Scholar] [CrossRef] [PubMed]
- Van Rooijen, G.J.H.; Motoney, M.M. Plant Seed Oil-bodies as Carriers for Foreign Proteins. Nat. Biotechnol. 1995, 13, 72–77. [Google Scholar] [CrossRef]
- Liu, J.; Selinger, L.B.; Cheng, K.; Beauchemin, K.A.; Moloney, M.M. Plant seed oil-bodies as an immobilization matrix for a recombinant xylanase from the rumen fungus Neocallimastix patriciarum. Mol. Breed. 1997, 3, 463–470. [Google Scholar] [CrossRef]
- Nykiforuk, C.L.; Boothe, J.G.; Murray, E.W.; Keon, R.G.; Goren, H.J.; Markley, N.A.; Moloney, M.M. Transgenic expression and recovery of biologically active recombinant human insulin from Arabidopsis thaliana seeds. Plant. Biotechnol. J. 2006, 4, 77–85. [Google Scholar] [CrossRef]
- Qiang, W.; Gao, T.; Lan, X.; Guo, J.; Noman, M.; Li, Y.; Guo, Y.; Kong, J.; Li, H.; Du, L.; et al. Molecular Pharming of the Recombinant Protein hEGF-hEGF Concatenated with Oleosin Using Transgenic Arabidopsis. Genes 2020, 11, 959. [Google Scholar] [CrossRef] [PubMed]
- Yi, S.; Yang, J.; Huang, J.; Guan, L.; Du, L.; Guo, Y.; Zhai, F.; Wang, Y.; Lu, Z.; Wang, L.; et al. Expression of bioactive recombinant human fibroblast growth factor 9 in oil bodies of Arabidopsis thaliana. Protein Expr. Purif. 2015, 116, 127–132. [Google Scholar] [CrossRef] [PubMed]
- Bundo, M.; Shi, X.; Vernet, M.; Marcos, J.F.; Lopez-Garcia, B.; Coca, M. Rice Seeds as Biofactories of Rationally Designed and Cell-Penetrating Antifungal PAF Peptides. Front. Plant. Sci. 2019, 10, 731. [Google Scholar] [CrossRef]
- Montesinos, L.; Bundo, M.; Izquierdo, E.; Campo, S.; Badosa, E.; Rossignol, M.; Montesinos, E.; San Segundo, B.; Coca, M. Production of Biologically Active Cecropin A Peptide in Rice Seed Oil Bodies. PLoS ONE 2016, 11, e0146919. [Google Scholar] [CrossRef] [PubMed]
- Chatrenet, B.; Chang, J.Y. The disulfide folding pathway of hirudin elucidated by stop/go folding experiments. J. Biol. Chem. 1993, 268, 20988–20996. [Google Scholar] [CrossRef]
- Gallier, S.; Singh, H. Behavior of almond oil bodies during in vitro gastric and intestinal digestion. Food Funct. 2012, 3, 547–555. [Google Scholar] [CrossRef]
- Ahmed, S.; Zhou, X.; Pang, Y.; Jin, L.; Bao, J. Improving Starch-Related Traits in Potato Crops: Achievements and Future Challenges. Starch-Stärke 2018, 70. [Google Scholar] [CrossRef]
- Bull, S.E.; Seung, D.; Chanez, C.; Mehta, D.; Kuon, J.-E.; Truernit, E.; Hochmuth, A.; Zurkirchen, I.; Zeeman, S.C.; Gruissem, W.; et al. Accelerated ex situ breeding of GBSS- and PTST1-edited cassava for modified starch. Sci. Adv. 2018, 4. [Google Scholar] [CrossRef] [PubMed]
- Mu-Forster, C.; Wasserman, B.P. Surface Localization of Zein Storage Proteins in Starch Granules from Maize Endosperm: Proteolytic Removal by Thermolysin and in Vitro Cross-Linking of Granule-Associated Polypeptides. Plant Physiol. 1998, 116, 1563–1571. [Google Scholar] [CrossRef]
- Ivanovsky, D. Concerning the mosaic disease of the tobacco plant. St. Petersburg Acad. Imp. Sci. Bull. 1882, 35, 67–70. [Google Scholar]
- Kausche, G.A.; Ruska, H. Die Struktur der “kristallinen Aggregate” des Tabakmosaikvirus-proteins. Biochem. Z 1939, 303, 211. [Google Scholar]
- Wen, A.M.; Steinmetz, N.F. Design of virus-based nanomaterials for medicine, biotechnology, and energy. Chem. Soc. Rev. 2016, 45, 4074–4126. [Google Scholar] [CrossRef] [PubMed]
- Qian, C.; Liu, X.; Xu, Q.; Wang, Z.; Chen, J.; Li, T.; Zheng, Q.; Yu, H.; Gu, Y.; Li, S.; et al. Recent Progress on the Versatility of Virus-Like Particles. Vaccines 2020, 8, 139. [Google Scholar] [CrossRef] [PubMed]
- Lizotte, P.H.; Wen, A.M.; Sheen, M.R.; Fields, J.; Rojanasopondist, P.; Steinmetz, N.F.; Fiering, S. In situ vaccination with cowpea mosaic virus nanoparticles suppresses metastatic cancer. Nat. Nanotechnol. 2016, 11, 295–303. [Google Scholar] [CrossRef] [PubMed]
- Murray, K.; Bruce, S.A.; Hinnen, A.; Wingfield, P.; van Erd, P.M.; de Reus, A.; Schellekens, H. Hepatitis B virus antigens made in microbial cells immunise against viral infection. EMBO J. 1984, 3, 645–650. [Google Scholar] [CrossRef]
- Valenzuela, P.; Medina, A.; Rutter, W.J.; Ammerer, G.; Hall, B.D. Synthesis and assembly of hepatitis B virus surface antigen particles in yeast. Nature 1982, 298, 347–350. [Google Scholar] [CrossRef]
- Huzair, F.; Sturdy, S. Biotechnology and the transformation of vaccine innovation: The case of the hepatitis B vaccines 1968-2000. Stud. Hist. Philos. Biol. Biomed. Sci. 2017, 64, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Schiller, J.T.; Castellsague, X.; Villa, L.L.; Hildesheim, A. An update of prophylactic human papillomavirus L1 virus-like particle vaccine clinical trial results. Vaccine 2008, 26 (Suppl. 10), K53–K61. [Google Scholar] [CrossRef]
- Naupu, P.N.; van Zyl, A.R.; Rybicki, E.P.; Hitzeroth, I.I. Immunogenicity of plant-produced human papillomavirus (HPV) virus-like particles (VLPs). Vaccines 2020, 8, 740. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.K.; Drake, P.M.; Christou, P. The production of recombinant pharmaceutical proteins in plants. Nat. Rev. Genet. 2003, 4, 794–805. [Google Scholar] [CrossRef]
- Mason, H.S.; Lam, D.M.; Arntzen, C.J. Expression of hepatitis B surface antigen in transgenic plants. Proc. Natl. Acad. Sci. USA 1992, 89, 11745–11749. [Google Scholar] [CrossRef]
- Marsian, J.; Lomonossoff, G.P. Molecular pharming—VLPs made in plants. Curr. Opin. Biotechnol. 2016, 37, 201–206. [Google Scholar] [CrossRef]
- Scotti, N.; Rybicki, E.P. Virus-like particles produced in plants as potential vaccines. Expert Rev. Vaccines 2013, 12, 211–224. [Google Scholar] [CrossRef]
- Thuenemann, E.C.; Lenzi, P.; Love, A.J.; Taliansky, M.; Bécares, M.; Zuñiga, S.; Enjuanes, L.; Zahmanova, G.G.; Minkov, I.N.; Matić, S.; et al. The use of transient expression systems for the rapid production of virus-like particles in plants. Curr. Pharm. Des. 2013, 19, 5564–5573. [Google Scholar] [CrossRef] [PubMed]
- D’Aoust, M.A.; Lavoie, P.O.; Couture, M.M.; Trepanier, S.; Guay, J.M.; Dargis, M.; Mongrand, S.; Landry, N.; Ward, B.J.; Vezina, L.P. Influenza virus-like particles produced by transient expression in Nicotiana benthamiana induce a protective immune response against a lethal viral challenge in mice. Plant. Biotechnol. J. 2008, 6, 930–940. [Google Scholar] [CrossRef]
- Pang, E.L.; Peyret, H.; Ramirez, A.; Loh, H.S.; Lai, K.S.; Fang, C.M.; Rosenberg, W.M.; Lomonossoff, G.P. Epitope Presentation of Dengue Viral Envelope Glycoprotein Domain III on Hepatitis B Core Protein Virus-Like Particles Produced in Nicotiana benthamiana. Front. Plant. Sci. 2019, 10, 455. [Google Scholar] [CrossRef] [PubMed]
- Ponndorf, D.; Meshcheriakova, Y.; Thuenemann, E.C.; Dobon Alonso, A.; Overman, R.; Holton, N.; Dowall, S.; Kennedy, E.; Stocks, M.; Lomonossoff, G.P.; et al. Plant-made dengue virus-like particles produced by co-expression of structural and non-structural proteins induce a humoral immune response in mice. Plant. Biotechnol. J. 2020. [Google Scholar] [CrossRef] [PubMed]
- Stump, C.T.; Ho, G.; Mao, C.; Veliz, F.A.; Beiss, V.; Fields, J.; Steinmetz, N.F.; Fiering, S. Remission-Stage Ovarian Cancer Cell Vaccine with Cowpea Mosaic Virus Adjuvant Prevents Tumor Growth. Cancers 2021, 13, 627. [Google Scholar] [CrossRef] [PubMed]
- Duval, K.E.A.; Wagner, R.J.; Beiss, V.; Fiering, S.N.; Steinmetz, N.F.; Hoopes, P.J. Cowpea Mosaic Virus Nanoparticle Enhancement of Hypofractionated Radiation in a B16 Murine Melanoma Model. Front. Oncol. 2020, 10, 594614. [Google Scholar] [CrossRef] [PubMed]
- Dennis, S.J.; Meyers, A.E.; Guthrie, A.J.; Hitzeroth, I.I.; Rybicki, E.P. Immunogenicity of plant-produced African horse sickness virus-like particles: Implications for a novel vaccine. Plant Biotechnol. J. 2018, 16, 442–450. [Google Scholar] [CrossRef] [PubMed]
- Dennis, S.J.; O’Kennedy, M.M.; Rutkowska, D.; Tsekoa, T.; Lourens, C.W.; Hitzeroth, I.I.; Meyers, A.E.; Rybicki, E.P. Safety and immunogenicity of plant-produced African horse sickness virus-like particles in horses. Vet. Res. 2018, 49, 105. [Google Scholar] [CrossRef]
- Gunter, C.J.; Regnard, G.L.; Rybicki, E.P.; Hitzeroth, I.I. Immunogenicity of plant-produced porcine circovirus-like particles in mice. Plant Biotechnol. J. 2019, 17, 1751–1759. [Google Scholar] [CrossRef] [PubMed]
- Marsian, J.; Hurdiss, D.L.; Ranson, N.A.; Ritala, A.; Paley, R.; Cano, I.; Lomonossoff, G.P. Plant-Made Nervous Necrosis Virus-Like Particles Protect Fish Against Disease. Front. Plant. Sci. 2019, 10, 880. [Google Scholar] [CrossRef] [PubMed]
- Diamos, A.G.; Pardhe, M.D.; Sun, H.; Hunter, J.G.L.; Mor, T.; Meador, L.; Kilbourne, J.; Chen, Q.; Mason, H.S. Codelivery of improved immune complex and virus-like particle vaccines containing Zika virus envelope domain III synergistically enhances immunogenicity. Vaccine 2020, 38, 3455–3463. [Google Scholar] [CrossRef]
- He, J.; Lai, H.; Esqueda, A.; Chen, Q. Plant-Produced Antigen Displaying Virus-Like Particles Evokes Potent Antibody Responses against West Nile Virus in Mice. Vaccines 2021, 9, 60. [Google Scholar] [CrossRef]
- Pumpens, P.; Borisova, G.P.; Crowther, R.A.; Grens, E. Hepatitis B virus core particles as epitope carriers. Intervirology 1995, 38, 63–74. [Google Scholar] [CrossRef]
- Peyret, H.; Gehin, A.; Thuenemann, E.C.; Blond, D.; El Turabi, A.; Beales, L.; Clarke, D.; Gilbert, R.J.; Fry, E.E.; Stuart, D.I.; et al. Tandem fusion of hepatitis B core antigen allows assembly of virus-like particles in bacteria and plants with enhanced capacity to accommodate foreign proteins. PLoS ONE 2015, 10, e0120751. [Google Scholar] [CrossRef]
- Peyret, H.; Ponndorf, D.; Meshcheriakova, Y.; Richardson, J.; Lomonossoff, G.P. Covalent protein display on Hepatitis B core-like particles in plants through the in vivo use of the SpyTag/SpyCatcher system. Sci. Rep. 2020, 10, 17095. [Google Scholar] [CrossRef]
- Ward, B.J.; Landry, N.; Trepanier, S.; Mercier, G.; Dargis, M.; Couture, M.; D’Aoust, M.A.; Vezina, L.P. Human antibody response to N-glycans present on plant-made influenza virus-like particle (VLP) vaccines. Vaccine 2014, 32, 6098–6106. [Google Scholar] [CrossRef]
- Chung, Y.H.; Cai, H.; Steinmetz, N.F. Viral nanoparticles for drug delivery, imaging, immunotherapy, and theranostic applications. Adv. Drug Deliv. Rev. 2020, 156, 214–235. [Google Scholar] [CrossRef] [PubMed]
- Sainsbury, F.; Canizares, M.C.; Lomonossoff, G.P. Cowpea mosaic virus: The plant virus-based biotechnology workhorse. Annu. Rev. Phytopathol. 2010, 48, 437–455. [Google Scholar] [CrossRef]
- Shin, M.D.; Shukla, S.; Chung, Y.H.; Beiss, V.; Chan, S.K.; Ortega-Rivera, O.A.; Wirth, D.M.; Chen, A.; Sack, M.; Pokorski, J.K.; et al. COVID-19 vaccine development and a potential nanomaterial path forward. Nat. Nanotechnol. 2020, 15, 646–655. [Google Scholar] [CrossRef]
- Shukla, S.; Hu, H.; Cai, H.; Chan, S.K.; Boone, C.E.; Beiss, V.; Chariou, P.L.; Steinmetz, N.F. Plant viruses and bacteriophage-based reagents for diagnosis and therapy. Annu. Rev. Virol. 2020, 7, 559–587. [Google Scholar] [CrossRef] [PubMed]
- Steinmetz, N.F.; Lim, S.; Sainsbury, F. Protein cages and virus-like particles: From fundamental insight to biomimetic therapeutics. Biomater. Sci. 2020, 8, 2771–2777. [Google Scholar] [CrossRef]
- Steinmetz, N.F.; Cho, C.F.; Ablack, A.; Lewis, J.D.; Manchester, M. Cowpea mosaic virus nanoparticles target surface vimentin on cancer cells. Nanomedicine 2011, 6, 351–364. [Google Scholar] [CrossRef]
- Koudelka, K.J.; Destito, G.; Plummer, E.M.; Trauger, S.A.; Siuzdak, G.; Manchester, M. Endothelial targeting of cowpea mosaic virus (CPMV) via surface vimentin. PLoS Pathog. 2009, 5, e1000417. [Google Scholar] [CrossRef] [PubMed]
- Berardi, A.; Evans, D.J.; Baldelli Bombelli, F.; Lomonossoff, G.P. Stability of plant virus-based nanocarriers in gastrointestinal fluids. Nanoscale 2018, 10, 1667–1679. [Google Scholar] [CrossRef] [PubMed]


| Particles | Expression System | Size [µm] | PTMs | In Vivo Studies | Ref. |
|---|---|---|---|---|---|
| Protein bodies | Rice | ~1 | + | ASIT against Japanese Cedar pollen allergen | [62,63] |
| Tobacco | 1–2 | + | Immunization against H5 | [64] | |
| Tobacco | 0.6–1 | n.d. | Immunization against BTV serotypes | [65] | |
| Oil bodies | Safflower seeds | 0.5–2.5 | - | Transdermal drug delivery of hormones: rhFGF9, hEGF | [66,67] |
| Starch granules | Maize | ~2 | - | n.a.; only in vitro digestion of encapsulated LT-B antigen | [68] |
| Algae | ~1.5 | - | Immunization against plasmodial antigens | [69] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schwestka, J.; Stoger, E. Microparticles and Nanoparticles from Plants—The Benefits of Bioencapsulation. Vaccines 2021, 9, 369. https://doi.org/10.3390/vaccines9040369
Schwestka J, Stoger E. Microparticles and Nanoparticles from Plants—The Benefits of Bioencapsulation. Vaccines. 2021; 9(4):369. https://doi.org/10.3390/vaccines9040369
Chicago/Turabian StyleSchwestka, Jennifer, and Eva Stoger. 2021. "Microparticles and Nanoparticles from Plants—The Benefits of Bioencapsulation" Vaccines 9, no. 4: 369. https://doi.org/10.3390/vaccines9040369
APA StyleSchwestka, J., & Stoger, E. (2021). Microparticles and Nanoparticles from Plants—The Benefits of Bioencapsulation. Vaccines, 9(4), 369. https://doi.org/10.3390/vaccines9040369






