Ethics of Vaccination in Childhood—A Framework Based on the Four Principles of Biomedical Ethics
Abstract
1. Introduction
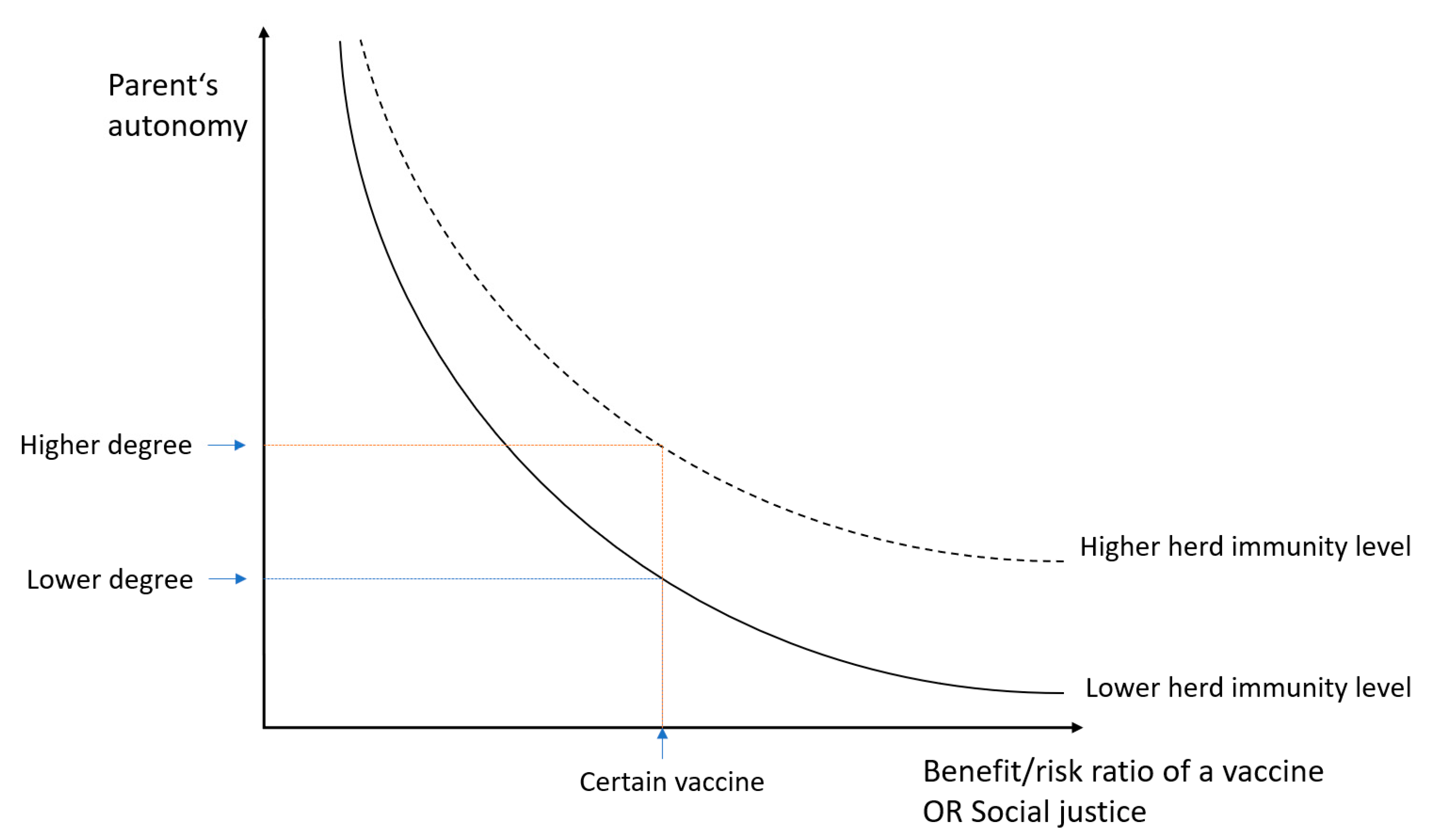
2. Respect for Autonomy
2.1. Decision Making Capacity
2.2. Disclosure of Information and Adequate Understanding
2.3. Voluntariness
2.4. Conscientious Objection of Parents and Medical Personnel
3. Nonmaleficence
3.1. Adverse Events
3.2. Contraindications for Immunisation
3.3. Vaccine Development
4. Beneficence
From Individual’s to Public Health Benefit of Vaccination
5. Justice
5.1. Need to Define Herd Immunity as a Common Good
5.2. Ethical Justification of Obligatory Medical Procedure
5.3. State’s Responsibility and Policies
6. The Four Principles Practical Application: Two Clinical Vignettes
6.1. Clinical Vignette #1
6.2. Clinical Vignette #2
7. Discussion
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Ten Great Public Health Achievements—United States, 1900–1999. MMWR Morb. Mortal. Wkly. Rep. 1999, 48, 241–243. [Google Scholar]
- Dubé, E.; Vivion, M.; MacDonald, N.E. Vaccine hesitancy, vaccine refusal and the anti-vaccine movement: Influence, impact and implications. Expert Rev. Vaccines 2015, 14, 99–117. [Google Scholar] [CrossRef] [PubMed]
- Salmon, D.A.; Dudley, M.Z.; Glanz, J.M.; Omer, S.B. Vaccine hesitancy: Causes, consequences, and a call to action. Vaccine 2015, 33 (Suppl. 4), D66–D71. [Google Scholar] [CrossRef] [PubMed]
- Olson, O.; Berry, C.; Kumar, N. Addressing Parental Vaccine Hesitancy towards Childhood Vaccines in the United States: A Systematic Literature Review of Communication Interventions and Strategies. Vaccines 2020, 8, 590. [Google Scholar] [CrossRef] [PubMed]
- Giubilini, A.; Douglas, T.; Savulescu, J. The moral obligation to be vaccinated: Utilitarianism, contractualism, and collective easy rescue. Med. Health Care Philos. 2018, 21, 547–560. [Google Scholar] [CrossRef]
- Giubilini, A. The Ethics of Vaccination, 1st ed.; Palgrave Pivot: Cham, Switzerland, 2019. [Google Scholar] [CrossRef]
- Williamson, L.; Glaab, H. Addressing vaccine hesitancy requires an ethically consistent health strategy. BMC Med. Ethics 2018, 19, 84. [Google Scholar] [CrossRef]
- McIntosh, E.D.; Janda, J.; Ehrich, J.H.; Pettoello-Mantovani, M.; Somekh, E. Vaccine Hesitancy and Refusal. J. Pediatr. 2016, 175, 248–249.e1. [Google Scholar] [CrossRef]
- Peretti-Watel, P.; Larson, H.J.; Ward, J.K.; Schulz, W.S.; Verger, P. Vaccine hesitancy: Clarifying a theoretical framework for an ambiguous notion. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef]
- Bedford, H.; Attwell, K.; Danchin, M.; Marshall, H.; Corben, P.; Leask, J. Vaccine hesitancy, refusal and access barriers: The need for clarity in terminology. Vaccine 2018, 36, 6556–6558. [Google Scholar] [CrossRef]
- Schwartz, J.L.; Caplan, A.L. Vaccination refusal: Ethics, individual rights, and the common good. Prim. Care 2011, 38, 717–728. [Google Scholar] [CrossRef]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Lane, S.; MacDonald, N.E.; Marti, M.; Dumolard, L. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015–2017. Vaccine 2018, 36, 3861–3867. [Google Scholar] [CrossRef] [PubMed]
- Wagner, A.L.; Masters, N.B.; Domek, G.J.; Mathew, J.L.; Sun, X.; Asturias, E.J.; Ren, J.; Huang, Z.; Contreras-Roldan, I.L.; Gebremeskel, B.; et al. Comparisons of Vaccine Hesitancy across Five Low- and Middle-Income Countries. Vaccines 2019, 7, 155. [Google Scholar] [CrossRef] [PubMed]
- Opel, D.J.; Schwartz, J.L.; Omer, S.B.; Silverman, R.; Duchin, J.; Kodish, E.; Diekema, D.S.; Marcuse, E.K.; Orenstein, W. Achieving an Optimal Childhood Vaccine Policy. JAMA Pediatr. 2017, 171, 893–896. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Luyten, J.; Bruyneel, L.; van Hoek, A.J. Assessing vaccine hesitancy in the UK population using a generalized vaccine hesitancy survey instrument. Vaccine 2019, 37, 2494–2501. [Google Scholar] [CrossRef]
- Hanna, J.N.; Symons, D.J.; Lyon, M.J. A measles outbreak in the Whitsundays, Queensland: The shape of things to come? Commun. Dis. Intell. Q. Rep. 2002, 26, 589–592. [Google Scholar]
- Bechini, A.; Boccalini, S.; Ninci, A.; Zanobini, P.; Sartor, G.; Bonaccorsi, G.; Grazzini, M.; Bonanni, P. Childhood vaccination coverage in Europe: Impact of different public health policies. Expert Rev. Vaccines 2019, 18, 693–701. [Google Scholar] [CrossRef]
- Phadke, V.K.; Bednarczyk, R.A.; Salmon, D.A.; Omer, S.B. Association Between Vaccine Refusal and Vaccine-Preventable Diseases in the United States: A Review of Measles and Pertussis. JAMA 2016, 315, 1149–1158. [Google Scholar] [CrossRef]
- Angelo, K.M.; Gastañaduy, P.A.; Walker, A.T.; Patel, M.; Reef, S.; Lee, C.V.; Nemhauser, J. Spread of Measles in Europe and Implications for US Travelers. Pediatrics 2019, 144. [Google Scholar] [CrossRef]
- World Health Organisation. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 20 October 2020).
- Iserson, K.V. SARS-CoV-2 (COVID-19) Vaccine Development and Production: An Ethical Way Forward. Camb. Q. Healthc. Ethics 2021, 30, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Folayan, M.O.; Yakubu, A.; Haire, B.; Peterson, K. Ebola vaccine development plan: Ethics, concerns and proposed measures. BMC Med. Ethics 2016, 17, 10. [Google Scholar] [CrossRef] [PubMed]
- Schaefer, G.O.; Tam, C.C.; Savulescu, J.; Voo, T.C. COVID-19 vaccine development: Time to consider SARS-CoV-2 challenge studies? Vaccine 2020, 38, 5085–5088. [Google Scholar] [CrossRef] [PubMed]
- Venkatramanan, S.; Chen, J.; Fadikar, A.; Gupta, S.; Higdon, D.; Lewis, B.; Marathe, M.; Mortveit, H.; Vullikanti, A. Optimizing spatial allocation of seasonal influenza vaccine under temporal constraints. PLoS Comput. Biol. 2019, 15, e1007111. [Google Scholar] [CrossRef]
- Freedman, D.O.; Chen, L.H. Vaccines for International Travel. Mayo Clin. Proc. 2019, 94, 2314–2339. [Google Scholar] [CrossRef]
- Haviari, S.; Bénet, T.; Saadatian-Elahi, M.; André, P.; Loulergue, P.; Vanhems, P. Vaccination of healthcare workers: A review. Hum. Vaccines Immunother. 2015, 11, 2522–2537. [Google Scholar] [CrossRef]
- Krantz, I.; Sachs, L.; Nilstun, T. Ethics and vaccination. Scand. J. Public Health 2004, 32, 172–178. [Google Scholar] [CrossRef]
- Greenberg, J.; Dubé, E.; Driedger, M. Vaccine Hesitancy: In Search of the Risk Communication Comfort Zone. PLoS Curr. 2017, 9. [Google Scholar] [CrossRef]
- Fernbach, A. Parental rights and decision making regarding vaccinations: Ethical dilemmas for the primary care provider. J. Am. Acad. Nurse Pract. 2011, 23, 336–345. [Google Scholar] [CrossRef]
- Chadwick, R.; Wilson, D. The Emergence and Development of Bioethics in the Uk. Med. Law Rev. 2018, 26, 183–201. [Google Scholar] [CrossRef]
- Evans, J.H. A sociological account of the growth of principlism. Hastings Center Rep. 2000, 30, 31–38. [Google Scholar] [CrossRef]
- Herissone-Kelly, P. Determining the common morality’s norms in the sixth edition of Principles of Biomedical Ethics. J. Med. Ethics 2011, 37, 584–587. [Google Scholar] [CrossRef] [PubMed]
- Shea, M. Principlism’s Balancing Act: Why the Principles of Biomedical Ethics Need a Theory of the Good. J. Med. Philos. 2020, 45, 441–470. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, T.L.; Childress, J.F. Response to Commentaries. J. Med. Philos. 2020, 45, 560–579. [Google Scholar] [CrossRef] [PubMed]
- Harris, J. In praise of unprincipled ethics. J. Med. Ethics 2003, 29, 303–306. [Google Scholar] [CrossRef] [PubMed]
- Gillon, R. Ethics needs principles—Four can encompass the rest—And respect for autonomy should be “first among equals”. J. Med. Ethics 2003, 29, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, T.; Childress, J. Principles of Biomedical Ethics: Marking Its Fortieth Anniversary. Am. J. Bioeth. AJOB 2019, 19, 9–12. [Google Scholar] [CrossRef] [PubMed]
- Hine, K. What is the outcome of applying principlism? Theor. Med. Bioeth. 2011, 32, 375–388. [Google Scholar] [CrossRef]
- Beauchamp TL, C.J. The Principles of Biomedical Ethics, 6th ed.; Oxford University Press: New York, NY, USA, 2009. [Google Scholar]
- Stammers, T. The Evolution of Autonomy. New Bioeth. Multidiscip. J. Biotechnol. Body 2015, 21, 155–163. [Google Scholar] [CrossRef]
- Saad, T.C. The history of autonomy in medicine from antiquity to principlism. Med. Health Care Philos. 2018, 21, 125–137. [Google Scholar] [CrossRef]
- Stirrat, G.M.; Gill, R. Autonomy in medical ethics after O’Neill. J. Med. Ethics 2005, 31, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Cocanour, C.S. Informed consent-It’s more than a signature on a piece of paper. Am. J. Surg. 2017, 214, 993–997. [Google Scholar] [CrossRef] [PubMed]
- Sugarman, J. Ethics of Primary Care; McGraw-Hill: New York, NY, USA, 2000. [Google Scholar]
- Katz, A.L.; Webb, S.A. Informed Consent in Decision-Making in Pediatric Practice. Pediatrics 2016, 138. [Google Scholar] [CrossRef] [PubMed]
- Groselj, U. The concepts of assent and parental permission in pediatrics. World J. Pediatr. WJP 2014, 10, 89. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Chantler, T.; Letley, L.; Paterson, P.; Yarwood, J.; Saliba, V.; Mounier-Jack, S. Optimising informed consent in school-based adolescent vaccination programmes in England: A multiple methods analysis. Vaccine 2019, 37, 5218–5224. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Recommended Child and Adolescent Immunization Schedule for Ages 18 Years or Younger, United States. 2020. Available online: https://www.cdc.gov/vaccines/schedules/hcp/imz/child-adolescent.html (accessed on 5 November 2020).
- Jones, A.M.; Omer, S.B.; Bednarczyk, R.A.; Halsey, N.A.; Moulton, L.H.; Salmon, D.A. Parents’ source of vaccine information and impact on vaccine attitudes, beliefs, and nonmedical exemptions. Adv. Prev. Med. 2012, 2012, 932741. [Google Scholar] [CrossRef]
- Bedford, H.E.; Elliman, D.A.C. Fifteen-minute consultation: Vaccine-hesitant parents. Arch. Dis. Child. Educ. Pract. Ed. 2020, 105, 194–199. [Google Scholar] [CrossRef]
- Storr, C.; Sanftenberg, L.; Schelling, J.; Heininger, U.; Schneider, A. Measles Status-Barriers to Vaccination and Strategies for Overcoming Them. Dtsch. Arztebl. Int. 2018, 115, 723–730. [Google Scholar] [CrossRef] [PubMed]
- McKee, C.; Bohannon, K. Exploring the Reasons Behind Parental Refusal of Vaccines. J. Pediatr. Pharmacol. Ther. 2016, 21, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Swaney, S.E.; Burns, S. Exploring reasons for vaccine-hesitancy among higher-SES parents in Perth, Western Australia. Health Promot. J. Aust. 2019, 30, 143–152. [Google Scholar] [CrossRef]
- Nihlén Fahlquist, J. Vaccine hesitancy and trust. Ethical aspects of risk communication. Scand. J. Public Health 2018, 46, 182–188. [Google Scholar] [CrossRef] [PubMed]
- Danchin, M.; Nolan, T. A positive approach to parents with concerns about vaccination for the family physician. Aust. Fam. Physician 2014, 43, 690–694. [Google Scholar] [PubMed]
- Ahlin Marceta, J. A non-ideal authenticity-based conceptualization of personal autonomy. Med. Health Care Philos. 2019, 22, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Salmon, D.A.; Siegel, A.W. Religious and philosophical exemptions from vaccination requirements and lessons learned from conscientious objectors from conscription. Public Health Rep. 2001, 116, 289–295. [Google Scholar] [CrossRef]
- Clarke, S.; Giubilini, A.; Walker, M.J. Conscientious Objection to Vaccination. Bioethics 2017, 31, 155–161. [Google Scholar] [CrossRef] [PubMed]
- Gostin, L.O.; Hodge, J.G., Jr.; Bloom, B.R.; El-Mohandes, A.; Fielding, J.; Hotez, P.; Kurth, A.; Larson, H.J.; Orenstein, W.A.; Rabin, K.; et al. The public health crisis of underimmunisation: A global plan of action. Lancet Infect. Dis. 2020, 20, e11–e16. [Google Scholar] [CrossRef]
- National Conference on State Legislatures. States with Religious and Philosophical Exemptions from School Immunization Requirements. Available online: https://www.ncsl.org/research/health/school-immunization-exemption-state-laws.aspx (accessed on 6 November 2020).
- Vaz, O.M.; Ellingson, M.K.; Weiss, P.; Jenness, S.M.; Bardají, A.; Bednarczyk, R.A.; Omer, S.B. Mandatory Vaccination in Europe. Pediatrics 2020, 145. [Google Scholar] [CrossRef]
- Rhodes, R. Conscience, conscientious objections, and medicine. Theor. Med. Bioeth. 2019, 40, 487–506. [Google Scholar] [CrossRef]
- McAndrew, S. Internal morality of medicine and physician autonomy. J. Med. Ethics 2019, 45, 198–203. [Google Scholar] [CrossRef] [PubMed]
- Eberl, J.T. Conscientious objection in health care. Theor. Med. Bioeth. 2019, 40, 483–486. [Google Scholar] [CrossRef]
- Forster, M. Ethical position of medical practitioners who refuse to treat unvaccinated children. J. Med. Ethics 2019, 45, 552–555. [Google Scholar] [CrossRef] [PubMed]
- Shanawani, H. The Challenges of Conscientious Objection in Health care. J. Relig. Health 2016, 55, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Gillon, R. “Primum non nocere” and the principle of non-maleficence. Br. Med. J. (Clin. Res. Ed.) 1985, 291, 130–131. [Google Scholar] [CrossRef] [PubMed]
- Spencer, J.P.; Trondsen Pawlowski, R.H.; Thomas, S. Vaccine Adverse Events: Separating Myth from Reality. Am. Fam. Physician 2017, 95, 786–794. [Google Scholar] [PubMed]
- Smith, M. Vaccine safety: Medical contraindications, myths, and risk communication. Pediatr. Rev. 2015, 36, 227–238. [Google Scholar] [CrossRef]
- Fisman, D.N.; Laupland, K.B. The sounds of silence: Public goods, externalities, and the value of infectious disease control programs. Can. J. Infect. Dis. Med. Microbiol. J. Can. Mal. Infect. Microbiol. Med. 2009, 20, 39–41. [Google Scholar] [CrossRef]
- Committee to Review Adverse Effects of Vaccines; Institute of Medicine. Adverse Effects of Vaccines: Evidence and Causality; Stratton, K., Ford, A., Rusch, E., Clayton, E.W., Eds.; National Academies Press (US): Washington, DC, USA, 2011. [CrossRef]
- Grignolio, A. Kdo se Boji Cepiv; *Cf.: Ljubljana, Slovenia, 2018. [Google Scholar]
- Hviid, A.; Hansen, J.V.; Frisch, M.; Melbye, M. Measles, Mumps, Rubella Vaccination and Autism: A Nationwide Cohort Study. Ann. Intern. Med. 2019, 170, 513–520. [Google Scholar] [CrossRef]
- Opri, R.; Zanoni, G.; Caffarelli, C.; Bottau, P.; Caimmi, S.; Crisafulli, G.; Franceschini, F.; Liotti, L.; Saretta, F.; Vernich, M.; et al. True and false contraindications to vaccines. Allergol. Immunopathol. 2018, 46, 99–104. [Google Scholar] [CrossRef]
- Jacobson, R.M.; Ovsyannikova, I.G.; Poland, G.A. Testing vaccines in pediatric research subjects. Vaccine 2009, 27, 3291–3294. [Google Scholar] [CrossRef][Green Version]
- Giubilini, A. Vaccination ethics. Br. Med. Bull. 2020. [Google Scholar] [CrossRef]
- Davidson, A.J.; O’Brien, M. Ethics and medical research in children. Paediatr. Anaesth. 2009, 19, 994–1004. [Google Scholar] [CrossRef] [PubMed]
- Mintz, K.; Jardas, E.; Shah, S.; Grady, C.; Danis, M.; Wendler, D. Enrolling Minors in COVID-19 Vaccine Trials. Pediatrics 2020. [Google Scholar] [CrossRef]
- Taylor, R.M. Ethical principles and concepts in medicine. Handb. Clin. Neurol. 2013, 118, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Haire, B.; Komesaroff, P.; Leontini, R.; Raina MacIntyre, C. Raising Rates of Childhood Vaccination: The Trade-off Between Coercion and Trust. J. Bioethical Inq. 2018, 15, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Doherty, M.; Buchy, P.; Standaert, B.; Giaquinto, C.; Prado-Cohrs, D. Vaccine impact: Benefits for human health. Vaccine 2016, 34, 6707–6714. [Google Scholar] [CrossRef]
- Jennings, B.; Arras, J.D.; Drue, H.B.; Barbara, A.E. (Eds.) Emergency Ethics: Public Health Preparedness and Response; Oxford University Press: Oxford, UK, 2016. [Google Scholar] [CrossRef]
- Bester, J.C. Not a matter of parental choice but of social justice obligation: Children are owed measles vaccination. Bioethics 2018, 32, 611–619. [Google Scholar] [CrossRef]
- Hendrix, K.S.; Sturm, L.A.; Zimet, G.D.; Meslin, E.M. Ethics and Childhood Vaccination Policy in the United States. Am. J. Public Health 2016, 106, 273–278. [Google Scholar] [CrossRef]
- Verweij, M.F.; Houweling, H. What is the responsibility of national government with respect to vaccination? Vaccine 2014, 32, 7163–7166. [Google Scholar] [CrossRef]
- Ter Meulen, R. Solidarity, justice, and recognition of the other. Theor. Med. Bioeth. 2016, 37, 517–529. [Google Scholar] [CrossRef]
- Davies, B.; Savulescu, J. Solidarity and Responsibility in Health Care. Public Health Ethics 2019, 12, 133–144. [Google Scholar] [CrossRef]
- Browne, K. The Measles and Free Riders. Camb. Q. Healthc. Ethics CQ Int. J. Healthc. Ethics Comm. 2016, 25, 472–478. [Google Scholar] [CrossRef] [PubMed]
- Rakar, I.; Tičar, B.; Sever, T. Water Protection in Slovenia: Constitutional and Administrative Law Perspectives. In Water, Governance, and Crime Issues; Eman, K., Meško, G., Segato, L., Migliorini, M., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 129–155. [Google Scholar] [CrossRef]
- Grzybowski, A.; Patryn, R.K.; Sak, J.; Zagaja, A. Vaccination refusal. Autonomy and permitted coercion. Pathog. Glob. Health 2017, 111, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Flanigan, J. A defense of compulsory vaccination. HEC Forum Interdiscip. J. Hosp. Ethical Legal Issues 2014, 26, 5–25. [Google Scholar] [CrossRef]
- Navin, M.C.; Attwell, K. Vaccine mandates, value pluralism, and policy diversity. Bioethics 2019, 33, 1042–1049. [Google Scholar] [CrossRef] [PubMed]
- Blunden, C.T. Libertarianism and collective action: Is there a libertarian case for mandatory vaccination? J. Med. Ethics 2019, 45, 71–74. [Google Scholar] [CrossRef]
- Gostin, L.O. Public Health Law: Power, Duty, Restraint; University of California Press: Berkeley, CA, USA, 2008. [Google Scholar]
- Cohen, R.; Gaudelus, J.; Leboucher, B.; Stahl, J.P.; Denis, F.; Subtil, D.; Pujol, P.; Lepetit, H.; Longfier, L.; Martinot, A. Impact of mandatory vaccination extension on infant vaccine coverages: Promising preliminary results. Med. Mal. Infect. 2019, 49, 34–37. [Google Scholar] [CrossRef]
- Giubilini, A.; Savulescu, J. Vaccination, Risks, and Freedom: The Seat Belt Analogy. Public Health Ethics 2019, 12, 237–249. [Google Scholar] [CrossRef]
- Odone, A.; Fara, G.M.; Giammaco, G.; Blangiardi, F.; Signorelli, C. The future of immunization policies in Italy and in the European Union: The Declaration of Erice. Hum. Vaccines Immunother. 2015, 11, 1268–1271. [Google Scholar] [CrossRef]
- Field, R.I.; Caplan, A.L. A proposed ethical framework for vaccine mandates: Competing values and the case of HPV. Kennedy Inst. Ethics J. 2008, 18, 111–124. [Google Scholar] [CrossRef]
- Bennett, B.; Cohen, I.G.; Davies, S.E.; Gostin, L.O.; Hill, P.S.; Mankad, A.; Phelan, A.L. Future-proofing global health: Governance of priorities. Glob. Public Health 2018, 13, 519–527. [Google Scholar] [CrossRef]
- Spielthenner, G. The Principle-Based Method of Practical Ethics. Health Care Anal. HCA J. Health Philos. Policy 2017, 25, 275–289. [Google Scholar] [CrossRef] [PubMed]
- Braun, C.; O’Leary, S.T. Recent advances in addressing vaccine hesitancy. Curr. Opin. Pediatr. 2020, 32, 601–609. [Google Scholar] [CrossRef] [PubMed]
- Dubé, E. Addressing vaccine hesitancy: The crucial role of healthcare providers. Clin. Microbiol. Infect. 2017, 23, 279–280. [Google Scholar] [CrossRef] [PubMed]
- Gagneur, A.; Battista, M.C.; Boucher, F.D.; Tapiero, B.; Quach, C.; De Wals, P.; Lemaitre, T.; Farrands, A.; Boulianne, N.; Sauvageau, C.; et al. Promoting vaccination in maternity wards—Motivational interview technique reduces hesitancy and enhances intention to vaccinate, results from a multicentre non-controlled pre- and post-intervention RCT-nested study, Quebec, March 2014 to February 2015. Euro Surveill. Bull. Eur. Mal. Transm. Eur. Commun. Dis. Bull. 2019, 24. [Google Scholar] [CrossRef]
- Jarrett, C.; Wilson, R.; O’Leary, M.; Eckersberger, E.; Larson, H.J. Strategies for addressing vaccine hesitancy—A systematic review. Vaccine 2015, 33, 4180–4190. [Google Scholar] [CrossRef]
- Gagneur, A. Motivational interviewing: A powerful tool to address vaccine hesitancy. Can. Commun. Dis. Rep. Relev. Mal. Transm. Can. 2020, 46, 93–97. [Google Scholar] [CrossRef]
- Dzansi, D.Y. Finding an Equilibrium Ethical Framework in a Heterogeneous Society: The Role of Rules and Values. J. Sociol. Soc. Anthropol. 2013, 4. [Google Scholar] [CrossRef]
| RESPECT FOR AUTONOMY | NONMALEFICENCE |
| Respect for patient’s or parent’s will. | First, do no harm. |
Of physicians—to treat children whose parents refuse vaccination. |
|
| BENEFICENCE | JUSTICE |
| What is patient’s and society’s best interest? | Just distribution of benefits, risks and burdens. |
|
|
ETHICAL EQUILIBRIUM
| |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rus, M.; Groselj, U. Ethics of Vaccination in Childhood—A Framework Based on the Four Principles of Biomedical Ethics. Vaccines 2021, 9, 113. https://doi.org/10.3390/vaccines9020113
Rus M, Groselj U. Ethics of Vaccination in Childhood—A Framework Based on the Four Principles of Biomedical Ethics. Vaccines. 2021; 9(2):113. https://doi.org/10.3390/vaccines9020113
Chicago/Turabian StyleRus, Meta, and Urh Groselj. 2021. "Ethics of Vaccination in Childhood—A Framework Based on the Four Principles of Biomedical Ethics" Vaccines 9, no. 2: 113. https://doi.org/10.3390/vaccines9020113
APA StyleRus, M., & Groselj, U. (2021). Ethics of Vaccination in Childhood—A Framework Based on the Four Principles of Biomedical Ethics. Vaccines, 9(2), 113. https://doi.org/10.3390/vaccines9020113







