Compliance Indicators of COVID-19 Prevention and Vaccines Hesitancy in Kenya: A Random-Effects Endogenous Probit Model
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data and Sampling Procedures
2.2. Estimated Models
3. Results
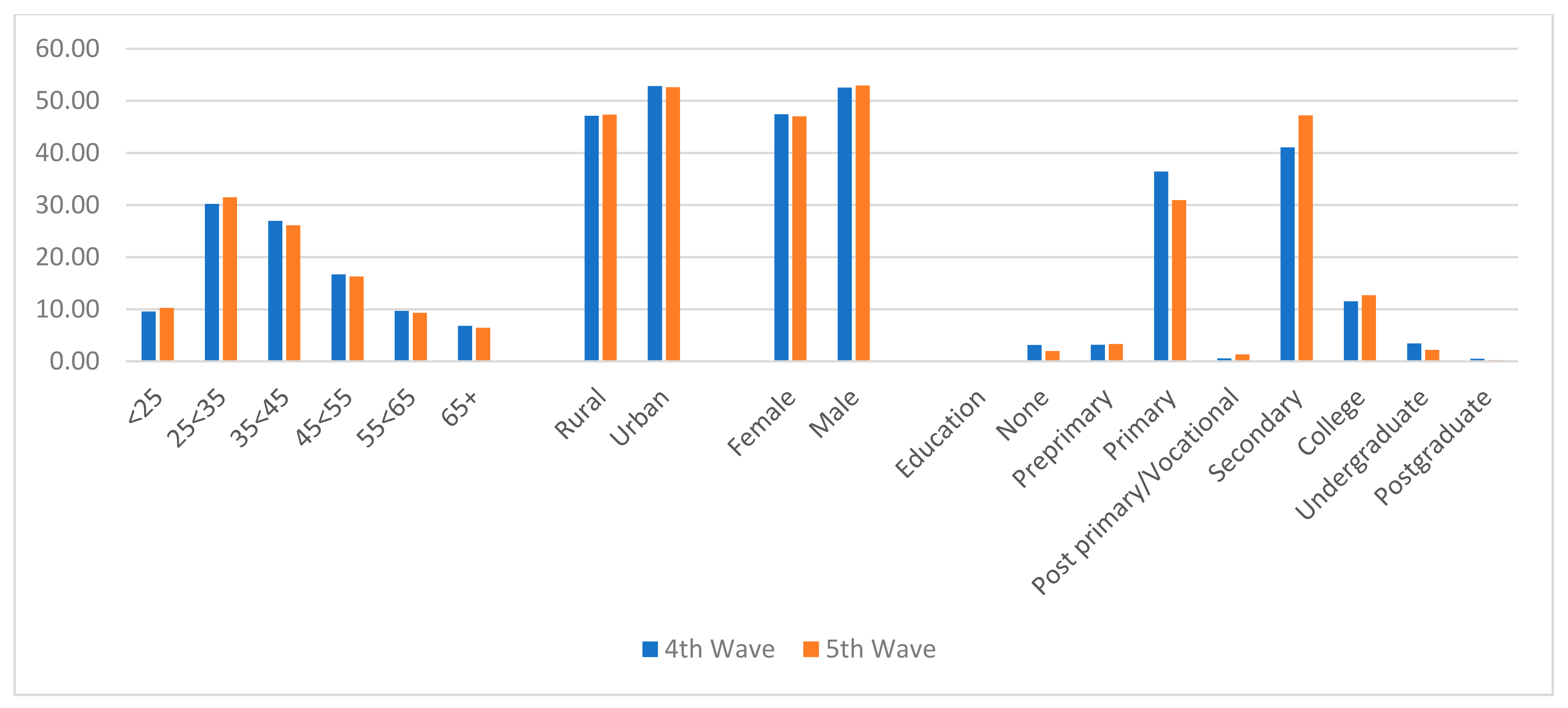
3.1. Selected Demographic Characteristics of the Respondents
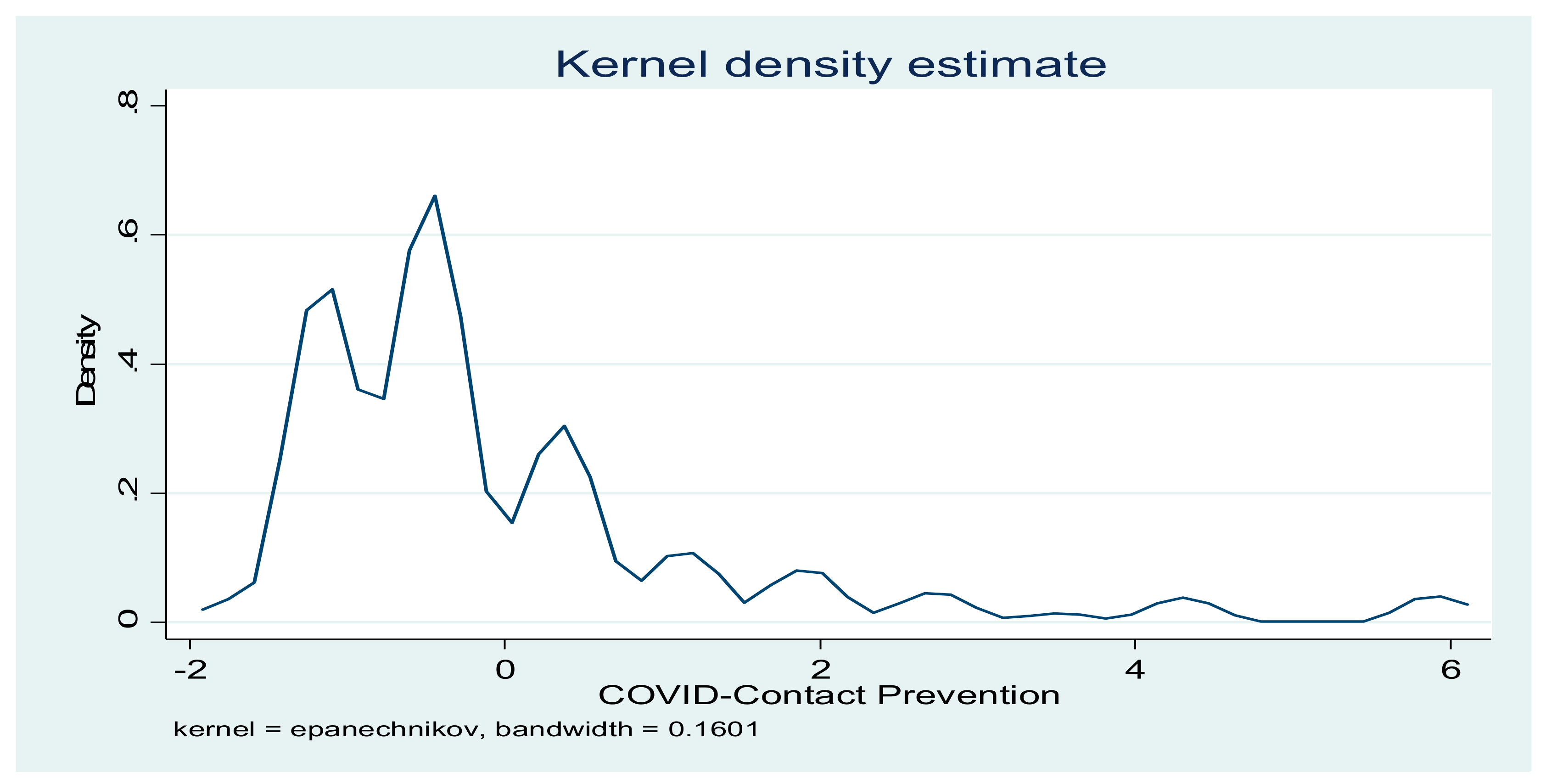
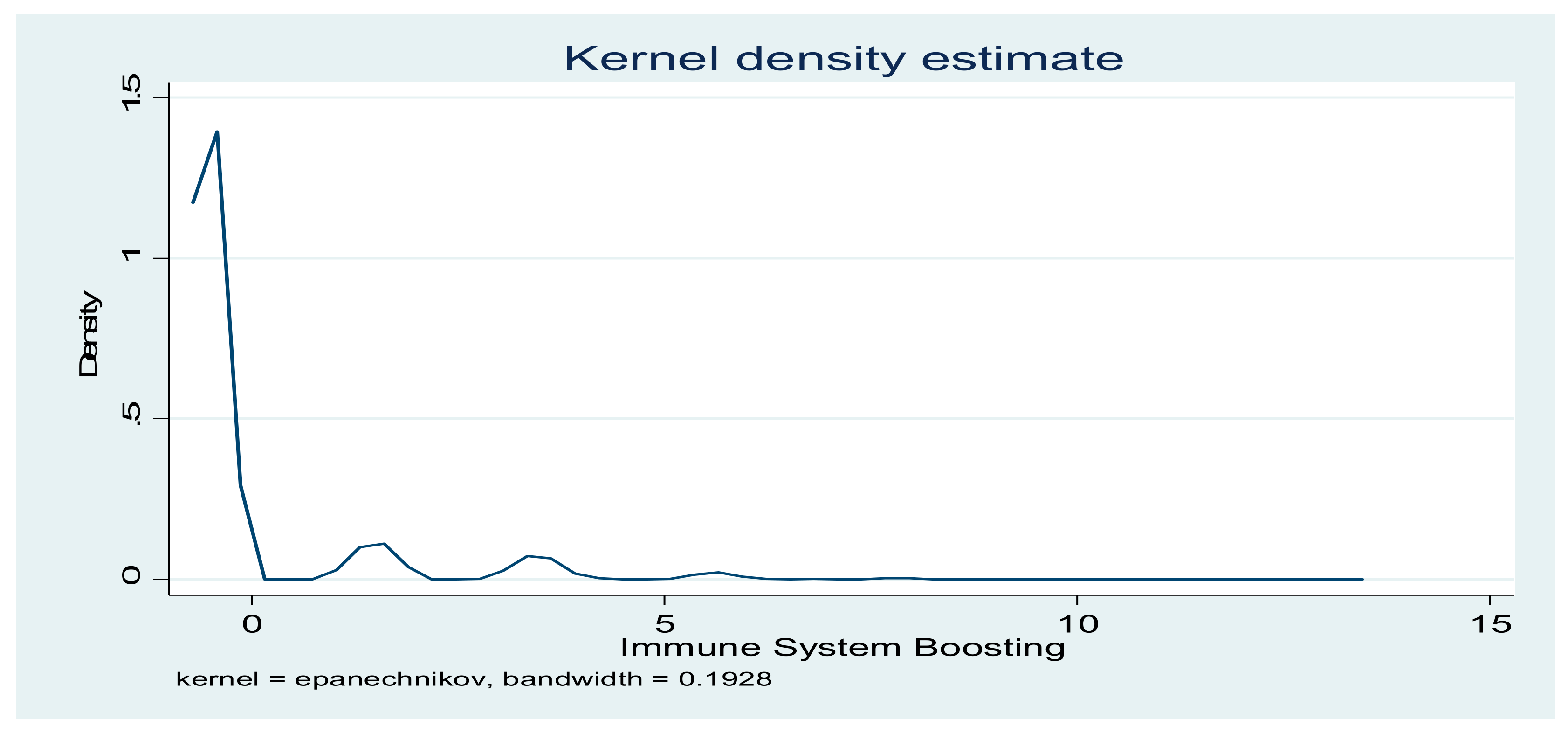
3.2. Compliance with COVID-19 Preventive Behaviours and Computed Indicators
3.3. Determinants of Contact-Prevention and Immune System-Boosting Compliance
3.4. Determinants of Willingness to Take COVID-19 Vaccines
4. Discussion
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ministry of Health. First Case of Coronavirus Disease Confirmed in Kenya. Available online: https://www.health.go.ke/first-case-of-coronavirus-disease-confirmed-in-kenya/ (accessed on 22 July 2021).
- Ministry of Health. National Emergency Response Committee on Coronavirus Update on COVID-19 in the Country and Response Measures, as at 26 October 2021. Available online: https://www.health.go.ke/wp-content/uploads/2021/10/Press-Statement-on-Covid-19-26th-October-2021.pdf (accessed on 27 October 2021).
- COVID Live Update: 217,920,243 Cases and 4,524,009 Deaths from the Coronavirus—Worldometer. Available online: https://www.worldometers.info/coronavirus/ (accessed on 31 August 2021).
- Ogunleye, O.O.; Basu, D.; Mueller, D.; Sneddon, J.; Seaton, R.A.; Yinka-Ogunleye, A.F.; Wamboga, J.; Miljković, N.; Mwita, J.C.; Rwegerera, G.M.; et al. Response to the Novel Corona Virus (COVID-19) pandemic across Africa: Successes, challenges, and implications for the future. Front. Pharmacol. 2020, 11, 1205. [Google Scholar] [CrossRef] [PubMed]
- Pinchoff, J.; Austrian, K.; Rajshekhar, N.; Abuya, T.; Kangwana, B.; Ochako, R.; Tidwell, J.B.; Mwanga, D.; Muluve, E.; Mbushi, F.; et al. Gendered economic, social and health effects of the COVID-19 pandemic and mitigation policies in Kenya: Evidence from a prospective cohort survey in Nairobi informal settlements. BMJ Open 2021, 11, e042749. [Google Scholar] [CrossRef]
- Pandey, K. COVID-19 in Africa: Nearly Half the Nations Going through Deadlier 3rd Wave. 2021. Available online: https://www.downtoearth.org.in/news/africa/covid-19-in-africa-nearly-half-the-nations-going-through-deadlier-3rd-wave-77986 (accessed on 23 July 2021).
- World Bank. Socioeconomic Impacts of COVID-19 in Kenya on Households: Rapid Response Phone Survey, Round 1. 2021. Available online: https://openknowledge.worldbank.org/handle/10986/35173 (accessed on 30 September 2021).
- United Nations. COVID-19: Africa ‘Third Wave’ Not Yet Over, while Vaccine Inequity Threatens All. 2021. Available online: https://news.un.org/en/story/2021/07/1096252 (accessed on 25 July 2021).
- Mwai, P. Coronavirus in Africa: Concern Grows Over Third Wave of Infection. 2021. Available online: https://www.bbc.com/news/world-africa-53181555 (accessed on 28 July 2021).
- Wako, A. Kenya: COVID-19—As Fourth Wave Spreads, Nairobians Let Down Their Guard. 2021. Available online: https://allafrica.com/stories/202107130906.html. (accessed on 28 July 2021).
- Hampton, L.; Graham-Rowe, D. How Do You Stop a Pandemic? 2020. Available online: https://www.gavi.org/vaccineswork/how-do-you-stop-pandemic (accessed on 18 April 2020).
- World Health Organisation. Overview of Public Health and Social Measures in the Context of COVID-19. 2020. Available online: https://www.who.int/publications/i/item/overview-of-public-health-andsocial-measures-in-the-context-of-covid-19 (accessed on 30 September 2021).
- Opanga, S.A.; Rizvi, N.; Wamaitha, A.; Sefah, I.A.; Godman, B. Availability of medicines in community pharmacy to manage patients with COVID-19 in Kenya; pilot study and implications. SAJP 2021, 10, 36–42. [Google Scholar] [CrossRef]
- Monye, I.; Adelowo, A.B. Strengthening immunity through healthy lifestyle practices: Recommendations for lifestyle interventions in the management of COVID-19. Lifestyle Med. 2020, 1, e7. [Google Scholar] [CrossRef]
- Rachul, C.; Marcon, A.R.; Collins, B.; Caulfield, T. COVID-19 and ‘Immune Boosting’ on the internet: A content analysis of Google Search results. BMJ Open 2020, 10, e040989. [Google Scholar] [CrossRef]
- Kumar, P.; Kumar, M.; Bedi, O.; Gupta, M.; Kumar, S.; Jaiswal, G.; Rahi, V.; Yedke, N.G.; Bijalwan, A.; Sharma, S.; et al. Role of vitamins and minerals as immunity boosters in COVID-19. Inflammopharmacology 2021, 29, 1–16. [Google Scholar] [CrossRef]
- Patterson, T.; Isales, C.M.; Fulzele, S. Low level of Vitamin C and dysregulation of Vitamin C transporter might be involved in the severity of COVID-19 infection. Aging Dis. 2021, 12, 14–26. [Google Scholar] [CrossRef] [PubMed]
- Derbyshire, E.; Delange, J. COVID-19: Is there a role for immunonutrition, particularly in the over 65s? BMJ Nutr. Prev. Health 2020, 3, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Prompetchara, E.; Ketloy, C.; Palaga, T. Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic. Asian Pac. J. Allergy Immunol. 2020, 38, 1–9. [Google Scholar] [CrossRef]
- Shakoor, H.; Feehan, J.; Mikkelsen, K.; Al Dhaheri, A.S.; Ali, H.I.; Platat, C.; Ismail, L.C.; Stojanovska, L.; Apostolopoulos, V. Be well: A potential role for Vitamin B in COVID-19. Maturitas 2021, 144, 108–111. [Google Scholar] [CrossRef]
- Martineau, A.R.; Jolliffe, D.A.; Hooper, R.L.; Greenberg, L.; Aloia, J.F.; Bergman, P.; Dubnov-Raz, G.; Esposito, S.; Ganmaa, D.; Ginde, A.A.; et al. Vitamin D supplementation to prevent acute respiratory tract infections: Systematic review and meta-analysis of individual participant data. BMJ 2017, 356, i6583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gombart, A.F.; Pierre, A.; Maggini, S. A Review of micronutrients and the immune system–Working in harmony to reduce the risk of infection. Nutrients 2020, 12, 236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Machado, P.R.L.; Araújo, M.I.A.S.; Carvalho, L.; Carvalho, E.M. Immune response mechanisms to infections. An. Bras. Dermatol. 2004, 79, 647–664. [Google Scholar] [CrossRef] [Green Version]
- Rouse, B.T.; Sehrawat, S. Immunity and immunopathology to viruses: What decides the outcome? Nat. Rev. Immunol. 2010, 10, 514–526. [Google Scholar] [CrossRef]
- Liu, B.; Li, M.; Zhou, Z.; Guan, X.; Xiang, Y. Can we use interleukin-6 (IL-6) blockade for coronavirus disease 2019 (COVID-19)-induced cytokine release syndrome (CRS)? J. Autoimmun. 2020, 111, 102452. [Google Scholar] [CrossRef]
- Sheybani, Z.; Dokoohaki, M.H.; Negahdaripour, M.; Dehdashti, M.; Zolghadr, H.; Moghadami, M.; Masoompour, S.M.; Zolghadr, A.R. The role of folic acid in the management of respiratory disease caused by COVID-19. ChemRxiv 2020. [Google Scholar] [CrossRef]
- Mehmel, M.; Jovanović, N.; Spitz, U. Nicotinamide Riboside—The current state of research and therapeutic uses. Nutrientes 2020, 12, 1616. [Google Scholar] [CrossRef]
- Kumar, V.; Kancharla, S.; Jena, M.K. In silico virtual screening-based study of nutraceuticals predicts the therapeutic potentials of folic acid and its derivatives against COVID-19. VirusDisease 2021, 32, 29–37. [Google Scholar] [CrossRef]
- Calder, P.C. Nutrition, immunity and COVID-19. BMJ Nutr. Prev. Health 2020, 3, 74–92. [Google Scholar] [CrossRef]
- Calder, P.C.; Carr, A.C.; Gombart, A.F.; Eggersdorfer, M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients 2020, 12, 1181. [Google Scholar] [CrossRef] [Green Version]
- Kashiouris, M.G.; L’Heureux, M.; Cable, C.A.; Fisher, B.J.; Leichtle, S.W.; Fowler, A.A. The emerging role of Vitamin C as a treatment for Sepsis. Nutrients 2020, 12, 292. [Google Scholar] [CrossRef] [Green Version]
- OECD. Enhancing Public Trust in COVID-19 Vaccination: The Role of Governments. OECD Policy Responses to Coronavirus (COVID-19). 2021. Available online: https://www.oecd.org/coronavirus/policy-responses/enhancing-public-trust-in-covid-19-vaccination-the-role-of-governments-eae0ec5a/ (accessed on 28 July 2021).
- Ezeh, A.; Oyebode, O.; Satterthwaite, D.; Chen, Y.-F.; Ndugwa, R.; Sartori, J.; Mberu, B.; Melendez-Torres, G.J.; Haregu, T.N.; Watson, S.I.; et al. The history, geography, and sociology of slums and the health problems of people who live in slums. Lancet 2017, 389, 547–558. [Google Scholar] [CrossRef]
- Ministry of Health. National Policy Guidelines on Immunization 2013. Available online: http://e-cavi.com/wp-content/uploads/2014/11/KENYA-NATIONAL-POLICY-ON-IMMUNIZATION-2013.pdf (accessed on 2 August 2021).
- Larson, H.J.; Schulz, W.S.; Tucker, J.D.; Smith, D.M.D. Measuring vaccine confidence: Introducing a global vaccine confidence index. PLoS Curr. 2015, 7, ecurrents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4. [Google Scholar] [CrossRef]
- De Figueiredo, A.; Simas, C.; Karafillakis, E.; Paterson, P.; Larson, H.J. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: A large-scale retrospective temporal modelling study. Lancet 2020, 396, 898–908. [Google Scholar] [CrossRef]
- Machingaidze, S.; Wiysonge, C.S. Understanding COVID-19 vaccine hesitancy. Nat. Med. 2021, 27, 1338–1339. [Google Scholar] [CrossRef]
- Wiysonge, C.S.; Ndwandwe, D.; Ryan, J.; Jaca, A.; Batouré, O.; Anya, B.-P.M.; Cooper, S. Vaccine hesitancy in the era of COVID-19: Could lessons from the past help in divining the future? Hum. Vaccin. Immunother. 2021, 8, 1–3. [Google Scholar] [CrossRef]
- Saied, S.M.; Saied, E.M.; Kabbash, I.A.; Abdo, S.A.E. Vaccine hesitancy: Beliefs and barriers associated with COVID-19 vaccination among Egyptian medical students. J. Med. Virol. 2021, 93, 4280–4291. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef]
- Sallam, M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://apps.who.int/gb/ebwha/pdf_fles/WHA73/A73_R1-en.pdf (accessed on 19 May 2020).
- Ong, S.W.X.; Young, B.E.; Lye, D.C. Lack of detail in population-level data impedes analysis of SARS-CoV-2 variants of concern and clinical outcomes. Lancet Infect. Dis. 2021, 21, 1195–1197. [Google Scholar] [CrossRef]
- SARS-CoV-2 Variants: The Need for Urgent Public Health Action beyond Vaccines. Available online: https://covid19commission.org/public-health-measures (accessed on 30 September 2021).
- Gibson, D.G.; Ochieng, B.; Kagucia, E.W.; Were, J.; Hayford, K.; Moulton, L.H.; Levine, O.S.; Odhiambo, F.; O’Brien, K.; Feikin, D.R. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): A cluster randomised controlled trial. Lancet Glob. Heal. 2017, 5, e428–e438. [Google Scholar] [CrossRef] [Green Version]
- Valenti, G.D.; Faraci, P. Identifying predictive factors in compliance with the COVID-19 containment measures: A mediation analysis. Psychol. Res. Behav. Manag. 2021, 14, 1325–1338. [Google Scholar] [CrossRef] [PubMed]
- Deeks, A.; Lombard, C.; Michelmore, J.; Teede, H. The effects of gender and age on health related behaviors. BMC Public Health 2009, 9, 213. [Google Scholar] [CrossRef] [Green Version]
- Vaidya, V.; Partha, G.; Karmakar, M. Gender differences in utilization of preventive care services in the United States. J. Women’s Health 2012, 21, 140–145. [Google Scholar] [CrossRef] [PubMed]
- Orangi, S.; Pinchoff, J.; Mwanga, D.; Abuya, T.; Hamaluba, M.; Warimwe, G.; Austrian, K.; Barasa, E. Assessing the level and determinants of COVID-19 vaccine confidence in Kenya. Vaccines 2021, 9, 936. [Google Scholar] [CrossRef]
- Chen, T.; Dai, M.; Xia, S.; Zhou, Y. Do messages matter? Investigating the combined effects of framing, outcome uncertainty, and number format on COVID-19 vaccination attitudes and intention. Health Commun. 2021, 1–8. [Google Scholar] [CrossRef]
- Chen, M.; Li, Y.; Chen, J.; Wen, Z.; Feng, F.; Zou, H.; Fu, C.; Chen, L.; Shu, Y.; Sun, C. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum. Vaccines Immunother. 2021, 17, 2279–2288. [Google Scholar] [CrossRef]
- McAbee, L.; Tapera, O.; Kanyangarara, M. Factors associated with COVID-19 vaccine intentions in Eastern Zimbabwe: A cross-sectional study. Vaccines 2021, 9, 1109. [Google Scholar] [CrossRef]
- Al-Mohaithef, M.; Padhi, B.K. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: A web-based national survey. J. Multidiscip. Health 2020, 13, 1657–1663. [Google Scholar] [CrossRef]
- Coustasse, A.; Kimble, C.; Maxik, K. COVID-19 and vaccine hesitancy. J. Ambul. Care Manag. 2021, 44, 71–75. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and receptivity for COVID-19 vaccines: A rapid systematic review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef]
- Hursh, S.R.; Strickland, J.C.; Schwartz, L.P.; Reed, D.D. Quantifying the impact of public perceptions on vaccine acceptance using behavioral economics. Front. Public Health 2020, 8, 608852. [Google Scholar] [CrossRef]
- Bell, S.; Clarke, R.; Mounier-Jack, S.; Walker, J.L.; Paterson, P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: A multi-methods study in England. Vaccine 2021, 38, 7789–7798. [Google Scholar] [CrossRef]
- Robles, A.S.; Gallahue, A.; Bennett, S.; Nerida, T.; Larson, T.; Parker, H.; Riddle, M. Determinants of COVID-19 vaccine acceptance among health care providers and citizens in Nevada. J. Investig. Med. 2021, 69, 235. [Google Scholar]
- Nguyen, K.H.; Srivastav, A.; Razzaghi, H.; Williams, W.; Lindley, M.C.; Jorgensen, C.; Abad, N.; Singleton, J.A. COVID-19 vaccination intent, perceptions, and reasons for not vaccinating among groups prioritized for early vaccination—United States, september and december 2020. Morb. Mortal. Wkly. Rep. 2021, 70, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Guidry, J.P.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am. J. Infect. Control. 2021, 49, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Schmid, P.; Heinemeier, D.; Korn, L.; Holtmann, C.; Bohm, R. Beyond confidence: Development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE 2018, 13, e0208601. [Google Scholar] [CrossRef] [Green Version]
- Thomson, A.; Robinson, K.; Vallée-Tourangeau, G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine 2016, 34, 1018–1024. [Google Scholar] [CrossRef] [Green Version]
- Dryhurst, S.; Schneider, C.R.; Kerr, J.; Freeman, A.L.J.; Recchia, G.; van der Bles, A.M.; Spiegelhalter, D.; van der Linden, S. Risk perceptions of COVID-19 around the world. J. Risk Res. 2020, 23, 994–1006. [Google Scholar] [CrossRef]
- Kwok, K.O.; Li, K.K.; Chan, H.H.H.; Yi, Y.Y.; Tang, A.; Wei, W.I.; Wong, S.Y.S. Community responses during early phase of COVID-19 epidemic, Hong Kong. Emerg. Infect. Dis. 2020, 26, 1575–1579. [Google Scholar] [CrossRef]
- Wise, T.; Zbozinek, T.D.; Michelini, G.; Hagan, C.C.; Mobbs, D. Changes in risk perception and self-reported protective behaviour during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 2020, 7, 7. [Google Scholar] [CrossRef] [PubMed]
- Janz, N.K.; Becker, M.H. The health belief model: A decade later. Health Educ. Q. 1984, 11, 1–47. [Google Scholar] [CrossRef] [Green Version]
- Rogers, R.W. Cognitive and Physiological Processes in Fear Appeals and Attitude Change: A Revised Theory of Protection Motivation; Cacioppo, J., Petty, R., Eds.; Social Psychophysiology: New York, NY, USA, 1983. [Google Scholar]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Graffigna, G.; Palamenghi, L.; Boccia, S.; Barello, S. Relationship between citizens’ health engagement and intention to take the COVID-19 vaccine in Italy: A mediation analysis. Vaccines 2020, 8, 576. [Google Scholar] [CrossRef] [PubMed]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef]
- Pape, U.J.; Sinha, N.; Delius, A.J.S. Kenya COVID-19 Rapid Response Phone Survey Households 2020–2021, Panel. Available online: https://microdata.worldbank.org/index.php/catalog/3774 (accessed on 15 August 2021).
- Jolliffe, I.T.; Cadima, J. Principal component analysis: A review and recent developments. Phil. Trans. R. Soc. A 2016, 374, 20150202. [Google Scholar] [CrossRef]
- Jaadi, Z. A Step-by-Step Explanation of Principal Component Analysis. Available online: https://builtin.com/data-science/step-step-explanation-principal-component-analysis (accessed on 23 July 2021).
- StataCorp. Xtprobit—Random-Effects and Population-Averaged Probit Models. Available online: https://www.stata.com/manuals/xtxtprobit.pdf (accessed on 22 September 2021).
- Wooldridge, J.M. Introductory Econometrics: A Modern Approach, 5th ed.; Centage Learning: Boston, MA, USA, 2012. [Google Scholar]
- Kollamparambil, U.; Oyenubi, A. Behavioural response to the COVID-19 pandemic in South Africa. PLoS ONE 2021, 16, e0250269. [Google Scholar] [CrossRef] [PubMed]
- Petherick, A.; Goldszmidt, R.; Andrade, E.B.; Furst, R.; Hale, T.; Pott, A.; Wood, A. A worldwide assessment of changes in adherence to COVID-19 protective behaviours and hypothesized pandemic fatigue. Nat. Hum. Behav. 2021, 5, 1145–1160. [Google Scholar] [CrossRef]
- Saketkhoo, K.; Januszkiewicz, A.; Sackner, M. Effects of drinking hot water, cold water, and chicken soup on nasal mucus velocity and nasal airflow resistance. Chest 1978, 74, 408–410. [Google Scholar] [CrossRef]
- Arreola, R.; Quintero-Fabian, S.; López-Roa, R.I.; Flores-Gutiérrez, E.O.; Reyes, J.P.; Carrera-Quintanar, L.; Ortuño-Sahagún, D. Immunomodulation and anti-inflammatory effects of garlic compounds. J. Immunol. Res. 2015, 2015, 1–13. [Google Scholar] [CrossRef]
- Shimizu, C.; Wakita, Y.; Inoue, T.; Hiramitsu, M.; Okada, M.; Mitani, Y.; Segawa, S.; Tsuchiya, Y.; Nabeshima, T. Effects of lifelong intake of lemon polyphenols on aging and intestinal microbiome in the senescence-accelerated mouse prone 1 (SAMP1). Sci. Rep. 2019, 9, 3671. [Google Scholar] [CrossRef] [Green Version]
- Amado, D.A.V.; Bet Helmann, G.A.; Detoni, A.M.; De Carvalho, S.L.C.; De Aguiar, C.M.; Martin, C.A.; Tiuman, T.S.; Cottica, S.M. Antioxidant and antibacterial activity and preliminary toxicity analysis of four varieties of avocado (Persea americana Mill.). Braz. J. Food Technol. 2019, 22, 2018044. [Google Scholar] [CrossRef]
- Dodd, R.H.; Cvejic, E.; Bonner, C.; Pickles, K.; McCaffery, K.J.; Ayre, J.; Batcup, C.; Copp, T.; Cornell, S.; Dakin, T.; et al. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, 318–319. [Google Scholar] [CrossRef]
- Rhodes, A.; Hoq, M.; Measey, M.-A.; Danchin, M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, e110. [Google Scholar] [CrossRef]
- Padidar, S.; Liao, S.-M.; Magagula, S.; Mahlaba, T.A.M.; Nhlabatsi, N.M.; Lukas, S. Assessment of early COVID-19 compliance to and challenges with public health and social prevention measures in the Kingdom of Eswatini, using an online survey. PLoS ONE 2021, 16, e0253954. [Google Scholar] [CrossRef] [PubMed]
- Al-Rahimi, J.S.; Nass, N.M.; Hassoubah, S.A.; Wazqar, D.Y.; Alamoudi, S.A. Levels and predictors of fear and health anxiety during the current outbreak of COVID-19 in immunocompromised and chronic disease patients in Saudi Arabia: A cross-sectional correlational study. PLoS ONE 2021, 16, e0250554. [Google Scholar] [CrossRef]
- Posel, D.; Oyenubi, A.; Kollamparambil, U. Job loss and mental health during the COVID-19 lockdown: Evidence from South Africa. PLoS ONE 2021, 16, e0249352. [Google Scholar] [CrossRef]
- Bendau, A.; Plag, J.; Petzold, M.B.; Ströhle, A. COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 2021, 97, 107724. [Google Scholar] [CrossRef] [PubMed]
- Perez-Arce, F.; Angrisani, M.; Bennett, D.; Darling, J.; Kapteyn, A.; Thomas, K. COVID-19 vaccines and mental distress. PLoS ONE 2021, 16, e0256406. [Google Scholar] [CrossRef]
- Kejriwal, M.; Shen, K. COVID-19 Vaccine hesitancy is positively associated with affective wellbeing. PsyArXiv 2021. [Google Scholar] [CrossRef]
| Variable | Mean | Std. Dev. | Min | Max |
|---|---|---|---|---|
| Dependent variable | ||||
| Agree to vaccinate (yes = 1, 0 otherwise) | 0.774 | - | 0 | 1 |
| Endogenous regressors | ||||
| Contact-prevention compliance | 1.69 × 10−8 | 1.458 | −1.758 | 5.944 |
| Immune-boosting compliance | −2.12 × 10−8 | 1.370 | −0.519 | 13.270 |
| Exogenous variables | ||||
| Days felt depressed in a week | 0.428 | 0.761 | 0 | 3 |
| Days felt lonely in a week | 0.410 | 0.752 | 0 | 3 |
| Days felt hopeful in a week | 1.272 | 1.274 | 0 | 3 |
| Days of physical reactions—nausea, sweating, breathing problem | 0.298 | 0.668 | 0 | 3 |
| Urban resident (yes = 1, 0 otherwise) | 0.527 | - | 0 | 1 |
| Age of the respondent | 40.014 | 13.822 | 18 | 98 |
| Gender (male) (yes = 1, 0 otherwise) | 0.528 | - | 0 | 1 |
| Household size | 3.793 | 2.118 | 1 | 17 |
| Formal education (yes = 1, 0 otherwise) | 0.975 | - | 0 | 1 |
| Know infected person (yes = 1, 0 otherwise) | 0.051 | - | 0 | 1 |
| Instrumental variables | ||||
| Feeling anxious (yes = 1, 0 otherwise) | 0.556 | - | 0 | 1 |
| Days felt nervous in a week | 0.468 | 0.788 | 0 | 3 |
| COVID-19 Preventive/Immune-Boosting Behaviours | Wave 4 (n = 4867) | Wave 5 (n = 5835) | Both Waves (n = 10,702) | |||
|---|---|---|---|---|---|---|
| Contact Avoidance Attributes | Frequency | % | Frequency | % | Frequency | % |
| Hand-washing | 4346 | 89.30 | 5433 | 93.11 | 9779 | 91.38 |
| Avoiding handshakes | 4392 | 90.24 | 5638 | 96.62 | 10,030 | 93.72 |
| Wearing masks | 3891 | 79.95 | 4719 | 80.87 | 8610 | 80.45 |
| Avoiding groups of more than 10 persons | 3440 | 70.68 | 4766 | 81.68 | 8206 | 76.68 |
| Hand sanitizer | 2477 | 50.89 | 2995 | 51.33 | 5472 | 51.13 |
| Covering mouth if coughing | 1399 | 28.74 | 1568 | 26.87 | 2967 | 27.72 |
| Staying at home more | 1335 | 27.43 | 1376 | 23.58 | 2711 | 25.33 |
| Traveling less | 570 | 11.71 | 422 | 7.23 | 992 | 9.27 |
| Working less | 405 | 8.32 | 365 | 6.26 | 770 | 7.19 |
| Stocking up food at home | 542 | 11.14 | 584 | 10.01 | 1126 | 10.52 |
| Immune-Boosting Attributes | ||||||
| Drinking tea with lemon | 404 | 8.30 | 319 | 5.47 | 723 | 6.76 |
| Drinking warm water | 404 | 8.30 | 600 | 10.28 | 1004 | 9.38 |
| Taking vitamin C rich fruits | 134 | 2.75 | 120 | 2.06 | 254 | 2.37 |
| Eating lemons, garlic, avocadoes, mangoes | 144 | 2.96 | 460 | 7.88 | 604 | 5.64 |
| Eating alkaline foods | 44 | 0.90 | 60 | 1.03 | 104 | 0.97 |
| Taking bicarbonate | 88 | 1.81 | 34 | 0.58 | 122 | 1.14 |
| COVID-19 Contact-Prevention Indicator | Immune System-Boosting Indicator | |||||
|---|---|---|---|---|---|---|
| Component | Eigenvalue | Proportion | Cumulative | Eigenvalue | Proportion | Cumulative |
| Comp1 | 2.03128 | 0.2257 | 0.2257 | 1.87751 | 0.3129 | 0.3129 |
| Comp2 | 1.51467 | 0.1683 | 0.3940 | 1.07646 | 0.1794 | 0.4923 |
| Comp3 | 0.990668 | 0.1101 | 0.5041 | 0.950245 | 0.1584 | 0.6507 |
| Comp4 | 0.928001 | 0.1031 | 0.6072 | 0.858807 | 0.1431 | 0.7938 |
| Comp5 | 0.891516 | 0.0991 | 0.7062 | 0.702411 | 0.1171 | 0.9109 |
| Comp6 | 0.730758 | 0.0812 | 0.7874 | 0.534568 | 1.0000 | |
| Comp7 | 0.662303 | 0.0736 | 0.8610 | |||
| Comp8 | 0.644016 | 0.0716 | 0.9326 | |||
| Comp9 | 0.606791 | 0.0674 | 1.0000 | |||
| 4th Wave | 5th Wave | Both Waves | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Freq | % Willingness | Total | Freq | % Willingness | Total | Freq | % Willingness | Total |
| Age | |||||||||
| <25 | 335 | 71.89 | 466 | 464 | 77.33 | 600 | 799 | 74.95 | 1066 |
| 25<35 | 1047 | 71.13 | 1472 | 1452 | 79.00 | 1838 | 2499 | 75.50 | 3310 |
| 35<45 | 957 | 72.89 | 1313 | 1256 | 82.41 | 1524 | 2213 | 78.00 | 2837 |
| 45<55 | 632 | 77.83 | 812 | 774 | 81.39 | 951 | 1406 | 79.75 | 1763 |
| 55<65 | 349 | 73.94 | 472 | 454 | 83.30 | 545 | 803 | 78.96 | 1017 |
| 65+ | 260 | 78.31 | 332 | 304 | 80.64 | 377 | 564 | 79.55 | 709 |
| Sector | |||||||||
| Rural | 1725 | 75.16 | 2295 | 2203 | 79.70 | 2764 | 3928 | 77.64 | 5059 |
| Urban | 1855 | 72.12 | 2572 | 2501 | 81.44 | 3071 | 4356 | 77.19 | 5643 |
| Gender | |||||||||
| Female | 1687 | 73.06 | 2309 | 2197 | 80.04 | 2745 | 3884 | 76.85 | 5054 |
| Male | 1893 | 74.00 | 2558 | 2507 | 81.13 | 3090 | 4400 | 77.90 | 5648 |
| Education | |||||||||
| None | 109 | 70.78 | 154 | 82 | 70.69 | 116 | 191 | 70.74 | 270 |
| Preprimary | 99 | 63.46 | 156 | 115 | 58.97 | 195 | 214 | 60.97 | 351 |
| Primary | 1286 | 72.53 | 1773 | 1387 | 76.76 | 1807 | 2673 | 74.66 | 3580 |
| Post primary/Vocational | 23 | 79.31 | 29 | 63 | 80.77 | 78 | 86 | 80.37 | 107 |
| Secondary | 1499 | 74.95 | 2000 | 2288 | 83.08 | 2754 | 3787 | 79.66 | 4754 |
| College | 426 | 75.80 | 562 | 640 | 86.37 | 741 | 1066 | 81.81 | 1303 |
| Undergraduate | 119 | 70.83 | 168 | 116 | 89.92 | 129 | 235 | 79.12 | 297 |
| Postgraduate | 19 | 76.00 | 25 | 13 | 86.67 | 15 | 32 | 80.00 | 40 |
| Total | 3580 | 73.56 | 4867 | 4704 | 80.62 | 5835 | 8284 | 77.41 | 10,702 |
| COVID-19 Contact-Prevention Model | Immune System-Boosting Model | |||||
|---|---|---|---|---|---|---|
| Variables | Coef. | Robust Std Error | t Stat | Coef. | Robust Std Error | t Stat |
| Feel Anxious | 0.6949034 *** | 0.0267955 | 25.93 | 0.6239946 *** | 0.0253449 | 24.62 |
| Days depressed | 0.4954908 *** | 0.0343624 | 14.42 | 0.3213363 *** | 0.0313333 | 10.26 |
| Days nervous | −0.2574125 *** | 0.0293624 | −8.77 | −00.0349017 | 0.0301548 | −1.16 |
| Days felt lonely | 0.2634849 *** | 0.0274009 | 9.62 | −00.0553346 ** | 0.0259778 | −2.13 |
| Days felt hopeful | −0.1187308 *** | 0.0108604 | −10.93 | −00.0488207 *** | 0.0102056 | −4.78 |
| Days of physical reactions | 0.1869977 *** | 0.0378865 | 4.94 | −00.071272 ** | 0.0307028 | −2.32 |
| Urban resident | −0.0094086 | 0.0261114 | −0.36 | 0.0006897 | 0.0256915 | 0.03 |
| Age | −0.0000723 | 0.0009683 | −0.07 | 0.0000127 | 0.0009425 | 0.01 |
| Gender (male) | −0.081161 *** | 0.0259716 | −3.12 | −00.0447487 | 0.0256916 | −1.74 |
| Household size | −0.0020518 | 0.0061486 | −0.33 | −00.0082851 | 0.0061396 | −1.35 |
| Formal education | 0.1381852 | 0.079267 | 1.74 | 0.0132153 | 0.0895285 | 0.15 |
| Know infected person | −0.3011192 *** | 0.0571598 | −5.27 | −0.1179174 | 0.0638923 | −1.85 |
| Constant | −0.5513398 *** | 0.0996041 | −5.54 | −0.314684 *** | 0.1058094 | −2.97 |
| Number of observations | 10,702 | 10,702 | ||||
| F(12, 10,689) | 128.21 *** | 67.44 *** | ||||
| R-squared | 0.1640 | 0.0711 | ||||
| Variance Inflation Factor (VIF) | 1.48 | 1.48 | ||||
| Variables | Coef. | Standard Error | Z Statistics |
|---|---|---|---|
| Contact-prevention compliance | −1.610935 *** | 0.2495848 | −6.45 |
| Immune-boosting compliance | 203449 *** | 0.305411 | 6.66 |
| Days felt nervous in a week | −0.3476006 *** | 0.0545842 | −6.37 |
| Days felt lonely in a week | 0.4853005 *** | 0.0937532 | 5.18 |
| Days felt hopeful in a week | −0.0357433 | 0.019011 | −1.88 |
| Days of physical reactions—nausea, sweating, breathing problems | 0.1555594 | 0.0807415 | 1.93 |
| Urban resident | −0.0438994 | 0.0298572 | −1.47 |
| Age of the respondent | 0.0045713 *** | 0.0011037 | 4.14 |
| Gender (male} | 0.0179088 | 0.0301979 | 0.59 |
| Household size | −0.0113539 | 0.0073404 | −1.55 |
| Formal education | 0.4981303 *** | 0.0952476 | 5.23 |
| Know infected person | −0.0993262 | 0.0786707 | −1.26 |
| Error term 1 | 1.502961 *** | 0.2493549 | 6.03 |
| Error term 2 | −1.922836 *** | 0.305118 | −6.30 |
| Constant | 0.1769253 | 0.1235355 | 1.43 |
| lnsig2u | −2.35439 *** | 0.3840399 | |
| Sigma_u | 0.3081418 *** | 0.0591694 | |
| Rho | 0.0867174 *** | 0.030415 | |
| Number of observations | 10,702 | ||
| Integration points | 12 | ||
| Wald chi2(14) | 505.46 *** | ||
| Likelihood-ratio test of rho = 0 | 8.08 *** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oyekale, A.S. Compliance Indicators of COVID-19 Prevention and Vaccines Hesitancy in Kenya: A Random-Effects Endogenous Probit Model. Vaccines 2021, 9, 1359. https://doi.org/10.3390/vaccines9111359
Oyekale AS. Compliance Indicators of COVID-19 Prevention and Vaccines Hesitancy in Kenya: A Random-Effects Endogenous Probit Model. Vaccines. 2021; 9(11):1359. https://doi.org/10.3390/vaccines9111359
Chicago/Turabian StyleOyekale, Abayomi Samuel. 2021. "Compliance Indicators of COVID-19 Prevention and Vaccines Hesitancy in Kenya: A Random-Effects Endogenous Probit Model" Vaccines 9, no. 11: 1359. https://doi.org/10.3390/vaccines9111359
APA StyleOyekale, A. S. (2021). Compliance Indicators of COVID-19 Prevention and Vaccines Hesitancy in Kenya: A Random-Effects Endogenous Probit Model. Vaccines, 9(11), 1359. https://doi.org/10.3390/vaccines9111359





