Public Willingness and Determinants of COVID-19 Vaccination at the Initial Stage of Mass Vaccination in China
Abstract
:1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Measurements and Covariates
2.2.1. Willingness of COVID-19 Vaccination
2.2.2. Sociodemographic Characteristics, Epidemic-Related Factors, Vaccination-Specific Factors, and Health Status
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics
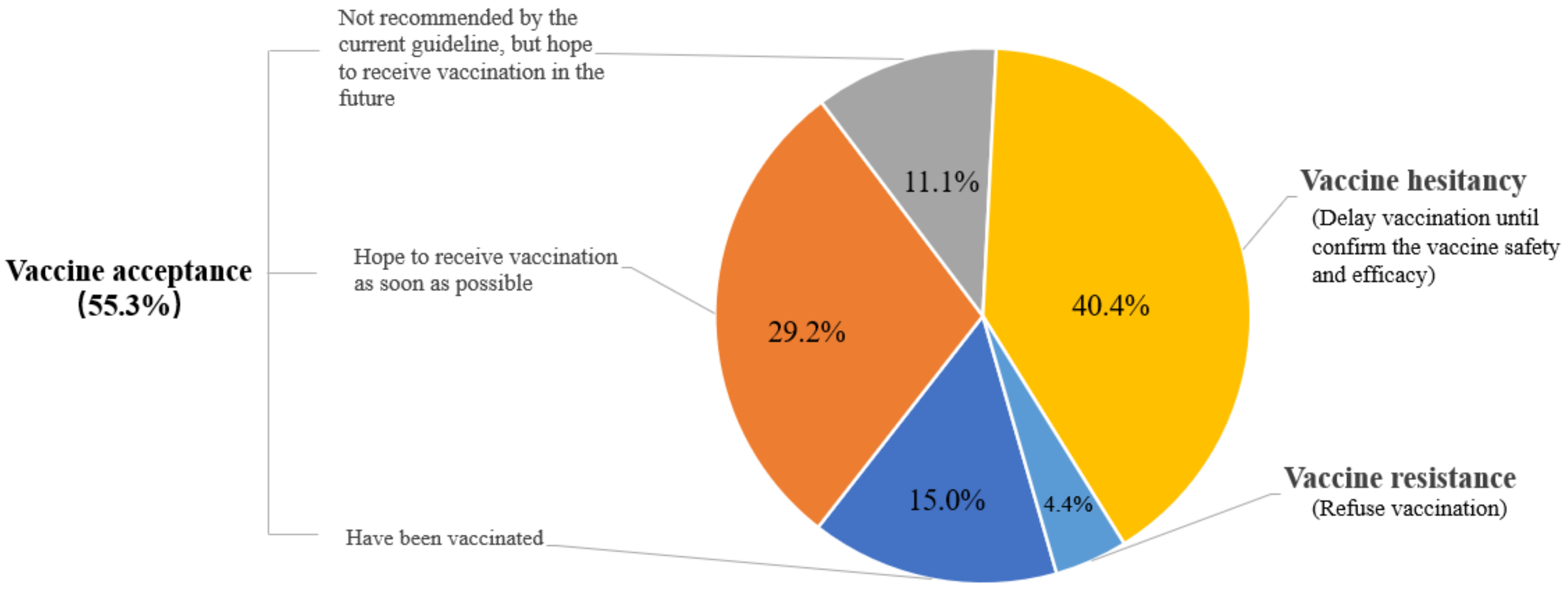
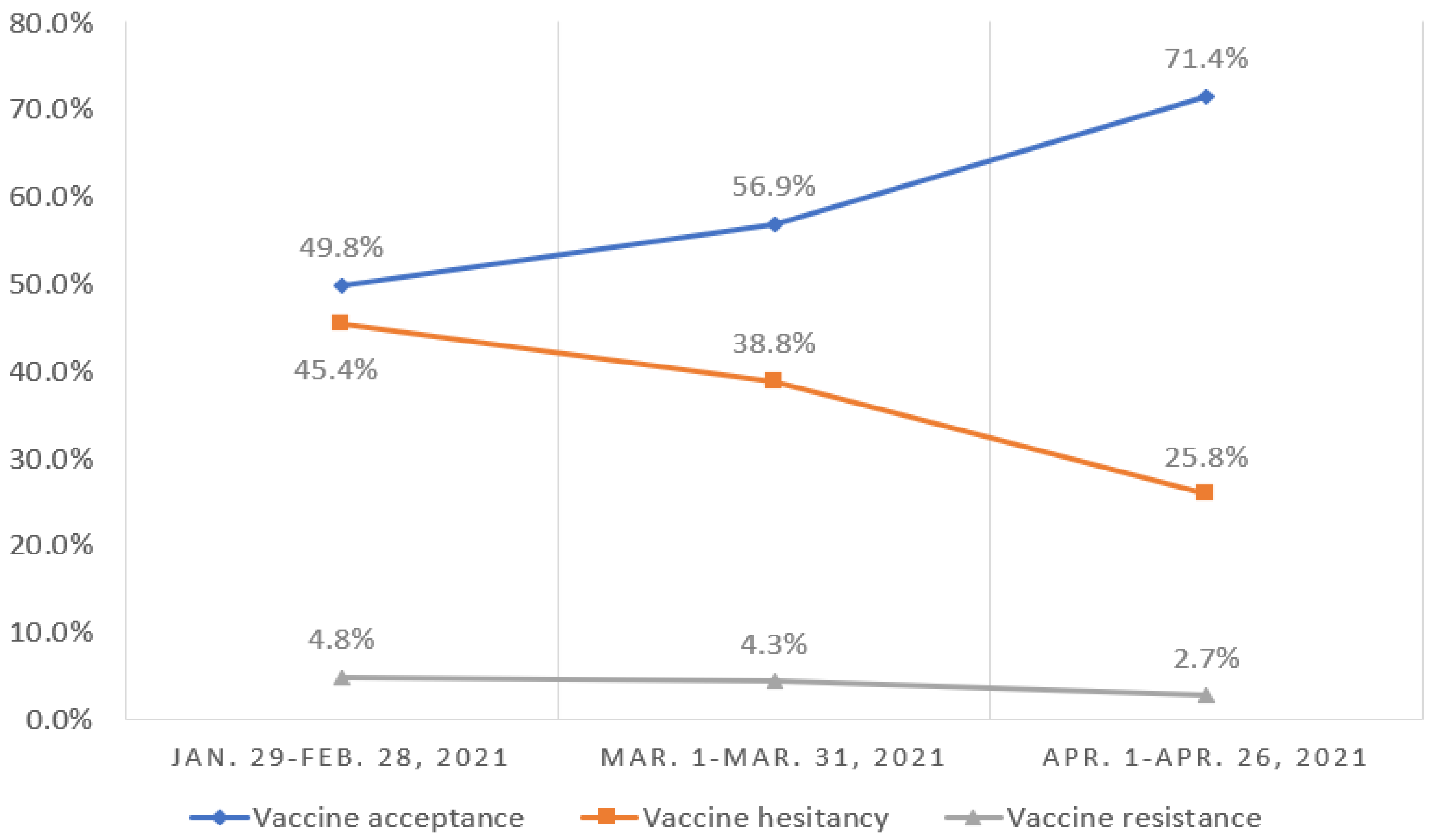
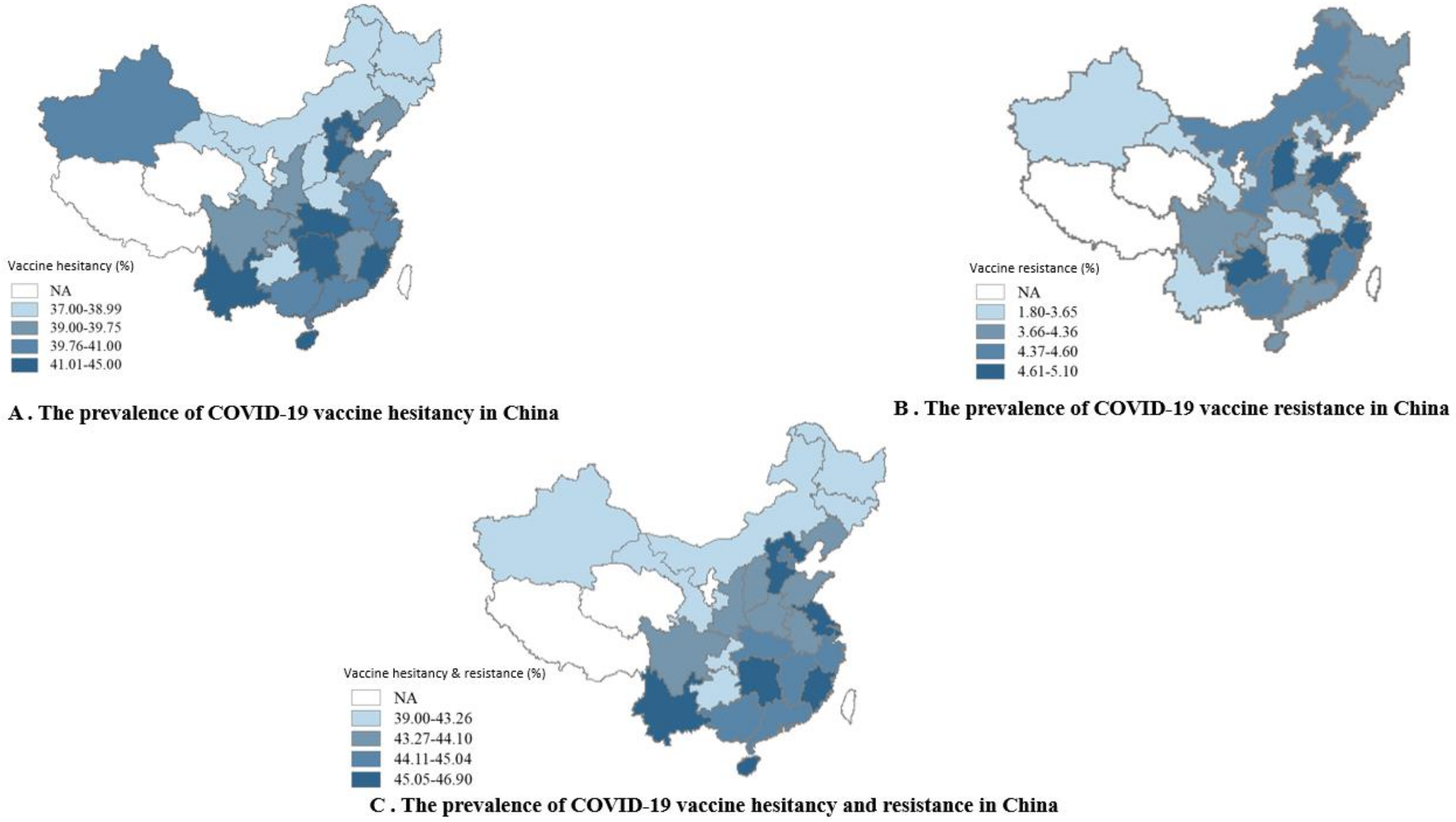
3.2. Prevalence of Vaccine Acceptance, Hesitancy, and Resistance
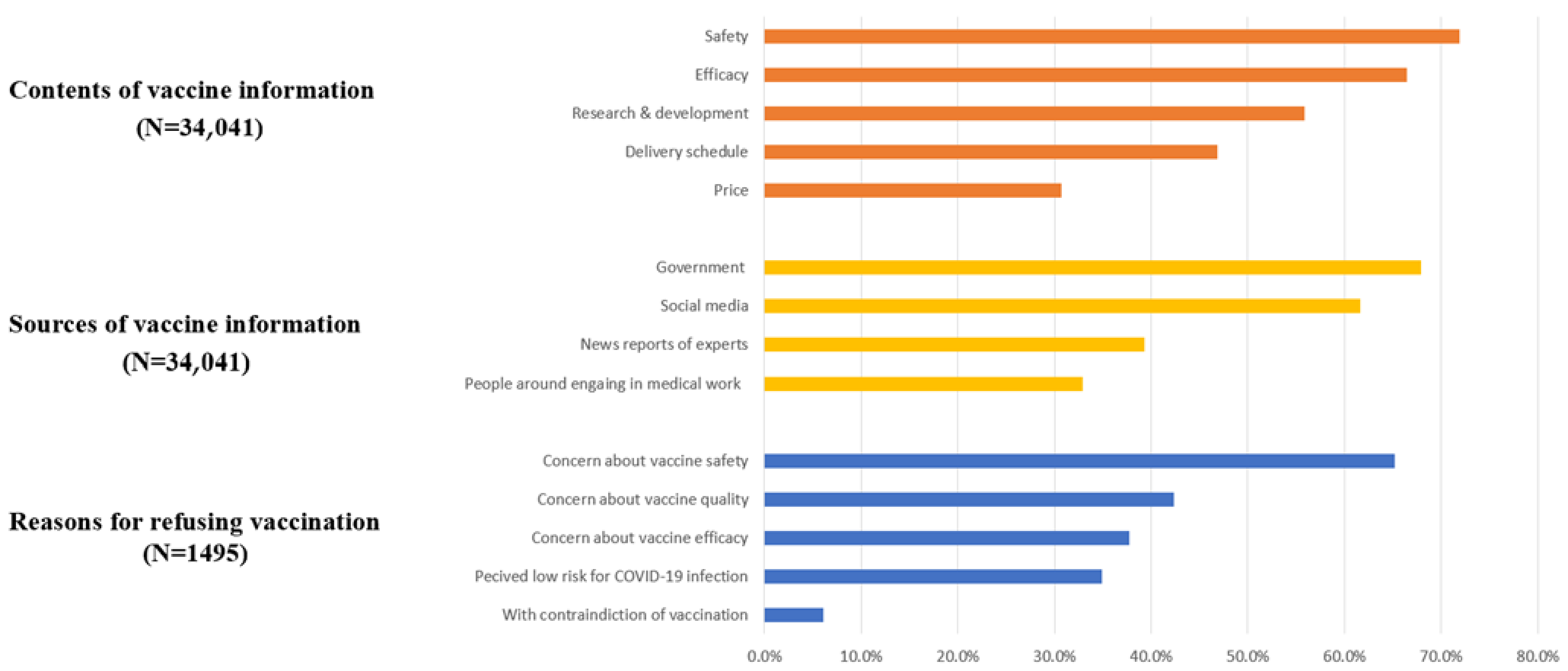
3.3. Contents and Sources of COVID-19 Vaccine Information and Reasons for Refusing Vaccination
3.4. Factors Associated with Vaccine Hesitancy and Resistance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 22 August 2021).
- WHO COVID-19 Vaccine Tracker and Landscape. Available online: https://www.who.int/publications/m/item/draft-landscape-of-covid-19-candidate-vaccines (accessed on 22 August 2021).
- World Health Organization Emergency Use Listing (EUL) of COVID-19 Vaccines. Available online: https://www.who.int/teams/regulation-prequalification/eul/covid-19 (accessed on 22 August 2021).
- Wouters, O.J.; Shadlen, K.C.; Salcher-Konrad, M.; Pollard, A.J.; Larson, H.J.; Teerawattananon, Y.; Jit, M. Challenges in ensuring global access to COVID-19 vaccines: Production, affordability, allocation, and deployment. Lancet 2021, 397, 1023–1034. [Google Scholar] [CrossRef]
- Solís Arce, J.S.; Warren, S.S.; Meriggi, N.F.; Scacco, A.; McMurry, N.; Voors, M.; Syunyaev, G.; Malik, A.A.; Aboutajdine, S.; Adeojo, O.; et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat. Med. 2021, 27, 1385–1394. [Google Scholar] [CrossRef] [PubMed]
- Sanche, S.; Lin, Y.T.; Xu, C.; Romero-Severson, E.; Hengartner, N.; Ke, R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg. Infect. Dis. 2020, 26, 1470–1477. [Google Scholar] [CrossRef]
- Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 22 August 2021).
- MacDonald, N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A global survey of potential acceptance of a COVID-19 vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lu, X.; Lai, X.; Lyu, Y.; Zhang, H.; Fenghuang, Y.; Jing, R.; Li, L.; Yu, W.; Fang, H. The changing acceptance of COVID-19 vaccination in different epidemic phases in China: A longitudinal study. Vaccines 2021, 9, 191. [Google Scholar] [CrossRef] [PubMed]
- Schwarzinger, M.; Watson, V.; Arwidson, P.; Alla, F.; Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: A survey experiment based on vaccine characteristics. Lancet Public Health 2021, 6, e210–e221. [Google Scholar] [CrossRef]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Kreps, S.; Prasad, S.; Brownstein, J.S.; Hswen, Y.; Garibaldi, B.T.; Zhang, B.; Kriner, D.L. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw. Open 2020, 3, e2025594. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes toward a potential SARS-CoV-2 vaccine: A survey of U.S. adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef]
- Wang, J.; Jing, R.; Lai, X.; Zhang, H.; Lyu, Y.; Knoll, M.D.; Fang, H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines 2020, 8, 482. [Google Scholar] [CrossRef]
- Shi, L.; Lu, Z.A.; Que, J.Y.; Huang, X.L.; Liu, L.; Ran, M.S.; Gong, Y.M.; Yuan, K.; Yan, W.; Sun, Y.K.; et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 2020, 3, e2014053. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.Y.; Li, Y.X.; Yu, C.Q.; Li, L.M. Reliability and validity of depression scales of Chinese version: A systematic review. Zhonghua Liu Xing Bing Xue Za Zhi 2017, 38, 110–116. [Google Scholar] [CrossRef]
- Qu, S.; Sheng, L. Diagnostic test of screening generalized anxiety disorders in general hospital psychological department with GAD-7. Chin. Mental Health J. 2015, 29, 939–944. [Google Scholar] [CrossRef]
- Rhodes, A.; Hoq, M.; Measey, M.A.; Danchin, M. Intention to vaccinate against COVID-19 in Australia. Lancet Infect. Dis. 2021, 21, e110. [Google Scholar] [CrossRef]
- Bono, S.A.; Faria de Moura Villela, E.; Siau, C.S.; Chen, W.S.; Pengpid, S.; Hasan, M.T.; Sessou, P.; Ditekemena, J.D.; Amodan, B.O.; Hosseinipour, M.C.; et al. Factors affecting COVID-19 vaccine acceptance: An international survey among low- and middle-income countries. Vaccines 2021, 9. [Google Scholar] [CrossRef] [PubMed]
- Kalok, A.; Loh, S.Y.E.; Chew, K.T.; Abdul Aziz, N.H.; Shah, S.A.; Ahmad, S.; Mohamed Ismail, N.A.; Abdullah Mahdy, Z. Vaccine hesitancy towards childhood immunisation amongst urban pregnant mothers in Malaysia. Vaccine 2020, 38, 2183–2189. [Google Scholar] [CrossRef] [PubMed]
- Ratzan, S.; Schneider, E.C.; Hatch, H.; Cacchione, J. Missing the point: How primary care can overcome COVID-19 vaccine "hesitancy". N. Engl. J. Med. 2021, 384, e100. [Google Scholar] [CrossRef]
- Wei, F.; Mullooly, J.P.; Goodman, M.; McCarty, M.C.; Hanson, A.M.; Crane, B.; Nordin, J.D. Identification and characteristics of vaccine refusers. BMC Pediatrics 2009, 9, 18. [Google Scholar] [CrossRef] [Green Version]
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.; Paterson, P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: A systematic review of published literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Ding, L.; Pan, X.; Shen, L.; Zhu, Y.; Chen, F.; Fu, J.; Gao, F.; Lv, H. Willingness to receive novel coronavirus vaccine and factors influencing willingness among healthcare workers in Zhejiang province. Zhongguo Yi Miao He Mian Yi 2021, 1–7. [Google Scholar] [CrossRef]
- Urrunaga-Pastor, D.; Bendezu-Quispe, G.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Toro-Huamanchumo, C.J.; Rodriguez-Morales, A.J.; Hernandez, A.V.; Benites-Zapata, V.A. Cross-sectional analysis of COVID-19 vaccine intention, perceptions and hesitancy across Latin America and the Caribbean. Travel Med. Infect. Dis. 2021, 41, 102059. [Google Scholar] [CrossRef] [PubMed]
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef] [Green Version]
- Grasselli, G.; Greco, M.; Zanella, A.; Albano, G.; Antonelli, M.; Bellani, G.; Bonanomi, E.; Cabrini, L.; Carlesso, E.; Castelli, G.; et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern. Med. 2020, 180, 1345–1355. [Google Scholar] [CrossRef] [PubMed]
- Li, H.; Liu, Z.; Ge, J. Scientific research progress of COVID-19/SARS-CoV-2 in the first five months. J. Cell. Mol. Med. 2020, 24, 6558–6570. [Google Scholar] [CrossRef]
- Larson, H.J.; Cooper, L.Z.; Eskola, J.; Katz, S.L.; Ratzan, S. Addressing the vaccine confidence gap. Lancet 2011, 378, 526–535. [Google Scholar] [CrossRef]
- Malik, A.A.; McFadden, S.M.; Elharake, J.; Omer, S.B. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020, 26, 100495. [Google Scholar] [CrossRef]
- Verger, P.; Peretti-Watel, P. Understanding the determinants of acceptance of COVID-19 vaccines: A challenge in a fast-moving situation. Lancet Public Health 2021, 6, e195–e196. [Google Scholar] [CrossRef]
- Khan, M.S.; Ali, S.A.M.; Adelaine, A.; Karan, A. Rethinking vaccine hesitancy among minority groups. Lancet 2021, 397, 1863–1865. [Google Scholar] [CrossRef]
- Wang, Y.; Shi, L.; Que, J.; Lu, Q.; Liu, L.; Lu, Z.; Xu, Y.; Liu, J.; Sun, Y.; Meng, S.; et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol. Psychiatry 2021, 1–10. [Google Scholar] [CrossRef]
- Habibovic, M.; Widdershoven, J.; Wetzels, M.; Piera-Jimenez, J.; Kop, W. Association between behavioral flexibility and psychological distress in patients with cardiovascular disease: Data from the do cardiac health: Advanced new generation ecosystem study. Heart Mind 2021, 5, 33–39. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine hesitancy: The next challenge in the fight against COVID-19. Eur. J. Health Econ. 2020, 35, 775–779. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Participants, n (%) |
|---|---|
| Gender | |
| Male | 15,732 (46.2) |
| Female | 18,309 (53.8) |
| Age, years | |
| 18–39 | 20,727 (60.9) |
| 40–59 | 12,713 (37.3) |
| ≥60 | 601 (1.8) |
| Survey time | |
| 29 January–28 February 2021 | 13,739 (40.4) |
| 1–31 March 2021 | 17,396 (51.1) |
| 1–26 April 2021 | 2906 (8.5) |
| Geographical region, China a | |
| Eastern | 13,321 (39.2) |
| Northern | 6382 (18.8) |
| Southern | 6064 (17.8) |
| Central | 2965 (8.7) |
| Northeast | 2398 (7.1) |
| Southwest | 1957 (5.8) |
| Northwest | 920 (2.7) |
| Living area | |
| Urban | 26,942 (79.1) |
| Rural | 7099 (20.9) |
| Education attainment | |
| College degree or higher | 26,957 (79.2) |
| Less than college | 7084 (20.8) |
| Marital status | |
| Married | 26,392 (77.5) |
| Unmarried b | 7649 (22.5) |
| Monthly family income, RMB c | |
| <5000 | 8438 (24.8) |
| 5000–11,999 | 15,961 (46.9) |
| ≥12,000 | 9642 (28.3) |
| Frontline worker d | |
| Yes | 1074 (3.2) |
| No | 32,967 (96.8) |
| COVID-19 infection status | |
| Confirmed or suspected | 104 (0.3) |
| Not infected | 33,937 (99.7) |
| Experience of quarantine | |
| Centralized quarantine | 493 (1.4) |
| Home confinement | 3388 (10.0) |
| No | 30,160 (88.6) |
| Local rebound of epidemic | |
| Yes | 6013 (17.7) |
| No | 28,028 (82.3) |
| History of chronic diseases | |
| Yes | 3103 (9.1) |
| Unknown | 2392 (7.0) |
| No | 28,546 (83.9) |
| Depression symptoms | |
| Moderate to severe | 3470 (10.2) |
| Mild | 4393 (12.9) |
| Normal | 26,178 (76.9) |
| Anxiety symptoms | |
| Moderate to severe | 2638 (7.7) |
| Mild | 4555 (13.4) |
| Normal | 26,848 (78.9) |
| Characteristic | Intent to Be Vaccinated, n (%)/Mean (SD) | p | ||
|---|---|---|---|---|
| Vaccine Acceptance (n = 18,810) | Vaccine Hesitancy (n = 13,736) | Vaccine Resistance (n = 1495) | ||
| Sociodemographic Factor | ||||
| Sex | <0.001 | |||
| Male | 9110 (57.9) | 5886 (37.4) a | 736 (4.7) | |
| Female | 9700 (53.0) | 7850 (42.9) | 759 (4.1) | |
| Age, years | <0.001 | |||
| 18–39 | 11,264 (54.3) | 8591 (41.4) a | 872 (4.2) | |
| 40–59 | 7158 (56.3) | 4967 (39.1) | 588 (4.6) | |
| ≥60 | 388 (64.6) | 178 (29.6) | 35 (5.8) | |
| Survey time | <0.001 | |||
| 29 January–28 February 2021 | 6840 (49.8) | 6236 (45.4) a | 663 (4.8) b | |
| 1–31 March 2021 | 9894 (56.9) | 6749 (38.8) | 753 (4.3) | |
| 1– 26 April 2021 | 2076 (71.4) | 751 (25.8) | 79 (2.7) | |
| Geographical region, China | 0.421 | |||
| Eastern | 7275 (54.6) | 5419 (40.7) | 627 (4.7) | |
| Northwest | 518 (56.3) | 361 (39.2) | 41 (4.5) | |
| Northern | 3527 (55.3) | 2575 (40.3) | 280 (4.4) | |
| Northeast | 1362 (56.8) | 933 (38.9) | 103 (4.3) | |
| Southern | 3355 (55.3) | 2455 (40.5) | 254 (4.2) | |
| Southwest | 1103 (56.4) | 775 (39.6) | 79 (4.0) | |
| Central | 1649 (55.6) | 1206 (40.7) | 110 (3.7) | |
| Living area | <0.001 | |||
| Urban | 14,698 (54.6) | 11,025 (40.9) a | 1219 (4.5) b | |
| Rural | 4112 (57.9) | 2711 (38.2) | 276 (3.9) | |
| Education attainment | <0.001 | |||
| Less than college | 4054 (57.2) | 2694 (38)a | 336 (4.7) | |
| College degree or higher | 14,756 (54.7) | 11,042 (41) | 1159 (4.3) | |
| Monthly family income, RMB | <0.001 | |||
| 0–4999 | 4712 (55.8) | 3292 (39) | 434 (5.1) b | |
| 5000–19,999 | 8843 (55.4) | 6517 (40.8) | 601 (3.8) | |
| ≥12,000 | 5255 (54.5) | 3927 (40.7) | 460 (4.8) | |
| Marital status | <0.001 | |||
| Married | 14,736 (55.8) | 10,551 (40)a | 1105 (4.2) b | |
| Unmarried | 4074 (53.3) | 3185 (41.6) | 390 (5.1) | |
| Epidemic-related factors | ||||
| COVID-19 infection status | 0.575 | |||
| Confirmed or suspected case | 62 (59.6) | 39 (37.5) | 3 (2.9) | |
| Not infected | 18,748 (55.2) | 13,697 (40.4) | 1492 (4.4) | |
| Frontline worker | <0.001 | |||
| Yes | 794 (73.9) | 250 (23.3) a | 30 (2.8) b | |
| No | 18,016 (54.6) | 13,486 (40.9) | 1465 (4.4) | |
| Local rebound of epidemic | 0.069 | |||
| Yes | 3312 (55.1) | 2468 (41) | 233 (3.9) | |
| No | 15,498 (55.3) | 11,268 (40.2) | 1262 (4.5) | |
| Quarantine experience | <0.001 | |||
| Centralized quarantine | 347 (70.4) | 131 (26.6) a | 15 (3.0) b | |
| Home confinement | 2075 (61.2) | 1213 (35.8) | 100 (3.0) | |
| None | 16,388 (54.3) | 12,392 (41.1) | 1380 (4.6) | |
| Perceived risk of infection | <0.001 | |||
| Low or very low | 16,923 (55.3) | 12,328 (40.3) a | 1351 (4.4) | |
| Medium | 1567 (53.0) | 1275 (43.2) | 112 (3.8) | |
| High or very high | 320 (66.0) | 133 (27.4) | 32 (6.6) | |
| Perceived effectiveness of protective measures | <0.001 | |||
| Vaccination | 7.6 (2.2) | 7.1 (2.0) a | 6.0 (2.3) b | |
| Social distancing | 7.3 (2.2) | 7.1 (2.1) a | 6.7 (2.5) b | |
| Wear a mask | 7.6 (2.1) | 7.4 (2.0) a | 6.9 (2.4) b | |
| Maintain personal hygiene | 7.7 (2.2) | 7.5 (2.1) a | 7.1 (2.5) b | |
| Vaccination-specific factors | ||||
| Proactively access COVID-19 vaccine information | <0.001 | |||
| Yes | 16,791 (57.1) | 11,668 (39.7) a | 937 (3.2) b | |
| No | 2019 (43.5) | 2068 (44.5) | 558 (12.0) | |
| History of receiving influenza vaccines | <0.001 | |||
| Yes | 7347 (63.8) | 3889 (33.8) a | 279 (2.4) | |
| No | 11,463 (50.9) | 9847 (43.7) | 1216 (5.4) | |
| History of allergic reactions to other vaccines | <0.001 | |||
| Yes | 2174 (53.7) | 1630 (40.2) | 246 (6.1) b | |
| No | 16,636 (55.5) | 12,106 (40.4) | 1249 (4.2) | |
| Health status | ||||
| History of chronic diseases | 0.965 | |||
| Yes | 1721 (55.5) | 1242 (40) | 140 (4.5) | |
| Unknown | 1328 (55.5) | 955 (39.9) | 109 (4.6) | |
| No | 15,761 (55.2) | 11,539 (40.4) | 1246 (4.4) | |
| Depression symptoms | <0.001 | |||
| Moderate to severe | 1903 (54.8) | 1344 (38.7) a | 223 (6.4) b | |
| Mild | 2293 (52.2) | 1894 (43.1) | 206 (4.7) | |
| Normal | 14,614 (55.8) | 10,498 (40.1) | 1066 (4.1) | |
| Anxiety symptoms | <0.001 | |||
| Moderate to severe | 1483 (56.2) | 986 (37.4) a | 169 (6.4) b | |
| Mild | 2351 (51.6) | 1987 (43.6) | 217 (4.8) | |
| Normal | 14,976 (55.8) | 10,763 (40.1) | 1109 (4.1) | |
| Characteristic | Vaccine Hesitancy vs. Acceptance, OR (95% CI) | Vaccine Resistance vs. Acceptance, OR (95% CI) |
|---|---|---|
| Sociodemographic factors | ||
| Gender | ||
| Male | 1 [Reference] | 1 [Reference] |
| Female | 1.21 (1.16–1.27) | 0.91 (0.82–1.02) |
| Age, years | ||
| 18–39 | 1.67 (1.38–2.01) | 1.00 (0.69–1.45) |
| 40–59 | 1.53 (1.27–1.84) | 1.18 (0.82–1.71) |
| ≥60 | 1 [Reference] | 1 [Reference] |
| Living area | ||
| Rural | 1 [Reference] | 1 [Reference] |
| Urban | 1.13 (1.07–1.20) | 1.26 (1.09–1.45) |
| Monthly family income, RMB | ||
| 0–4999 | 1 [Reference] | 1 [Reference] |
| 5000–19,999 | 1.07 (1.01–1.13) | 0.81 (0.71–0.92) |
| ≥12,000 | 1.10 (1.03–1.17) | 1.08 (0.93–1.25) |
| Epidemic-related factors | ||
| Survey time | ||
| 29 January–28 February 2021 | 1 [Reference] | 1 [Reference] |
| 1–31 March 2021 | 0.77 (0.73–0.81) | 0.84 (0.75–0.94) |
| 1–26 April 2021 | 0.41 (0.38–0.45) | 0.43 (0.34–0.55) |
| Frontline worker | ||
| Yes vs. No | 0.43 (0.37–0.50) | 0.50 (0.34–0.73) |
| Local rebound of epidemic | ||
| Yes vs. No | 1.01 (0.95–1.07) | 0.84 (0.73–0.98) |
| Quarantine experience | ||
| Centralized quarantine | 0.52 (0.42–0.64) | 0.43 (0.25–0.74) |
| Home confinement | 0.80 (0.74–0.86) | 0.59 (0.48–0.74) |
| None | 1 [Reference] | 1 [Reference] |
| Vaccine offers less protection than other protective measures | ||
| Yes vs. No | 1.52 (1.45–1.60) | 2.22 (1.99–2.48) |
| Perceived low risk of infection | ||
| Low or very low | 1.57 (1.27–1.94) | 1.00 (0.67–1.47) |
| Medium | 1.77 (1.41–2.20) | 0.82 (0.53–1.25) |
| High or very high | 1 [Reference] | 1 [Reference] |
| Vaccination-specific factors | ||
| Proactively access COVID-19 vaccine information | ||
| Yes vs. No | 0.74 (0.69–0.79) | 0.22 (0.20–0.25) |
| History of receiving influenza vaccines | ||
| Yes vs. No | 0.62 (0.59–0.65) | 0.40 (0.35–0.46) |
| History of allergic reactions to other vaccines | ||
| Yes vs. No | 1.07 (0.99–1.15) | 1.45 (1.25–1.69) |
| Health status | ||
| History of chronic diseases | ||
| Yes vs. No/Unknown | 0.88 (0.81–0.96) | 1.00 (0.83–1.21) |
| Depression symptoms a | ||
| Yes vs. No | 1.03 (0.98–1.09) | 1.20 (1.06–1.36) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.-M.; Liu, L.; Sun, J.; Yan, W.; Yuan, K.; Zheng, Y.-B.; Lu, Z.-A.; Liu, L.; Ni, S.-Y.; Su, S.-Z.; et al. Public Willingness and Determinants of COVID-19 Vaccination at the Initial Stage of Mass Vaccination in China. Vaccines 2021, 9, 1172. https://doi.org/10.3390/vaccines9101172
Zhao Y-M, Liu L, Sun J, Yan W, Yuan K, Zheng Y-B, Lu Z-A, Liu L, Ni S-Y, Su S-Z, et al. Public Willingness and Determinants of COVID-19 Vaccination at the Initial Stage of Mass Vaccination in China. Vaccines. 2021; 9(10):1172. https://doi.org/10.3390/vaccines9101172
Chicago/Turabian StyleZhao, Yi-Miao, Lin Liu, Jie Sun, Wei Yan, Kai Yuan, Yong-Bo Zheng, Zheng-An Lu, Lin Liu, Shu-Yu Ni, Si-Zhen Su, and et al. 2021. "Public Willingness and Determinants of COVID-19 Vaccination at the Initial Stage of Mass Vaccination in China" Vaccines 9, no. 10: 1172. https://doi.org/10.3390/vaccines9101172
APA StyleZhao, Y.-M., Liu, L., Sun, J., Yan, W., Yuan, K., Zheng, Y.-B., Lu, Z.-A., Liu, L., Ni, S.-Y., Su, S.-Z., Zhu, X.-M., Zeng, N., Gong, Y.-M., Wu, P., Ran, M.-S., Leng, Y., Shi, J., Shi, L., Lu, L., & Bao, Y.-P. (2021). Public Willingness and Determinants of COVID-19 Vaccination at the Initial Stage of Mass Vaccination in China. Vaccines, 9(10), 1172. https://doi.org/10.3390/vaccines9101172







