Review: Vaccines and Vaccination against Lumpy Skin Disease
Abstract
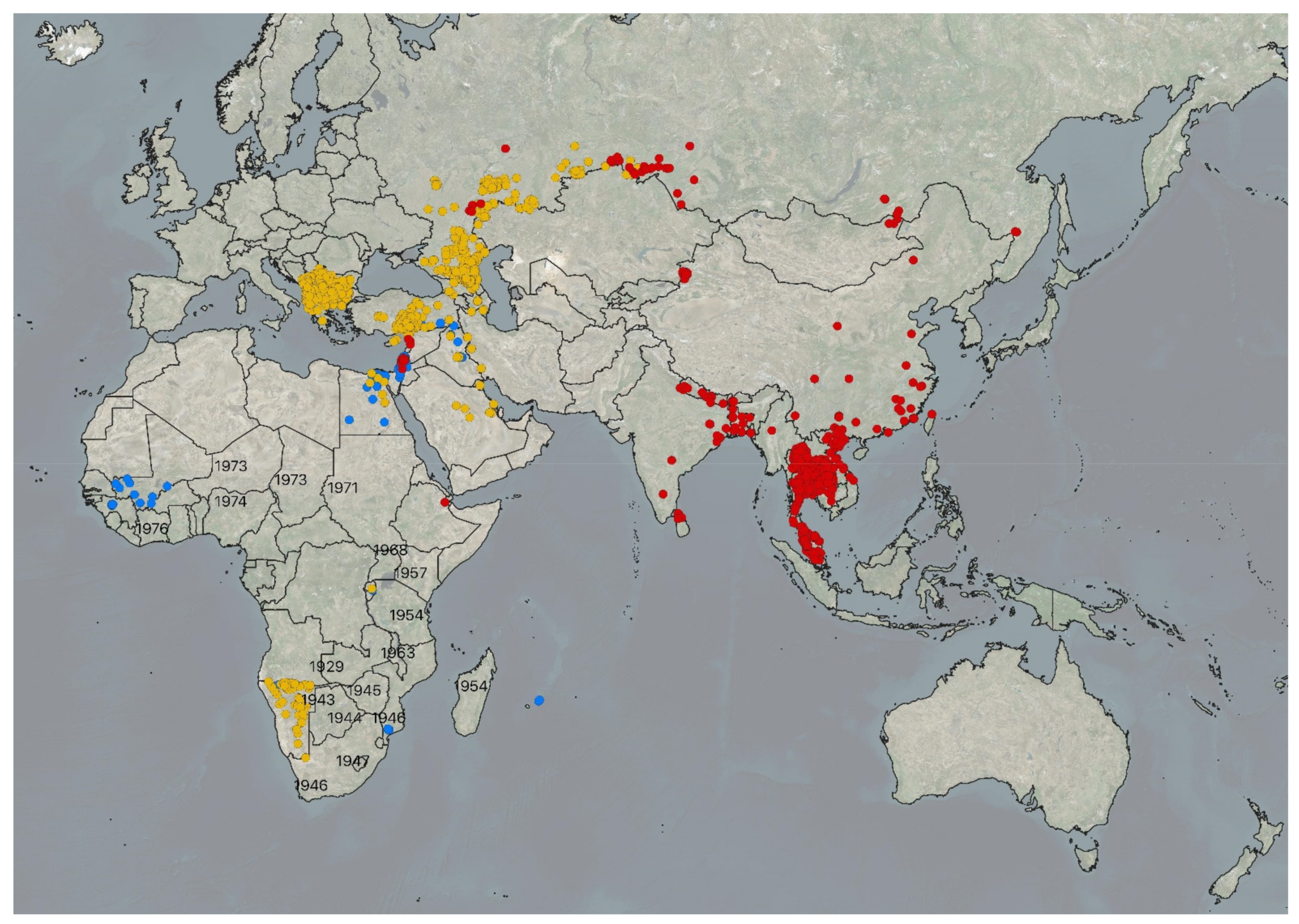
:1. Introduction
2. Production, Quality, Transport, Storage, and Handling of the LSD Vaccines
3. Live Attenuated Homologous Vaccines
4. Heterologous Vaccines
4.1. Goatpox Virus-Based Vaccines
4.2. Sheeppox Virus-Based Vaccines
4.3. Inactivated Vaccines
5. Seroconversion and Duration of Immunity after Vaccination with LSD Vaccines
6. Experimental Evaluation of the Efficacy of a Vaccine and Vaccination Effectiveness Studies
7. Vaccine Side Effects and Safety
8. The Role of Vaccination in LSD Prevention and Control
8.1. Strategic Considerations in LSD Vaccination
8.2. Vaccination-Oriented Risk Assessment
9. Development of Future Vaccines
10. Challenges with Transboundary LSD in Low-Income Countries and One Health Capacity Building
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- EFSA. Lumpy skin disease II. Data collection and analysis. EFSA J. 2018, 32. [Google Scholar] [CrossRef]
- Roche, X.; Rozstalnyy, A.; TagoPacheco, D.; Pittiglio, C.; Kamata, A.; Beltran Alcrudo, D.; Bisht, K.; Karki, S.; Kayamori, J.; Larfaoui, F.; et al. Introduction and Spread of Lumpy Skin Disease in South, East and Southeast Asia: Qualitative Risk Assessment and Management; FAO: Rome, Italy, 2020. [Google Scholar]
- Gupta, T.; Patial, V.; Bali, D.; Angaria, S.; Sharma, M.; Chahota, R. A review: Lumpy skin disease and its emergence in India. Vet. Res. Commun. 2020, 44, 111–118. [Google Scholar] [CrossRef]
- Lu, G.; Xie, J.X.; Luo, J.L.; Shao, R.; Jia, K.; Li, S.J. Lumpy skin disease outbreaks in China, since 3 August 2019. Transbound. Emerg. Dis. 2021, 68, 216–219. [Google Scholar] [CrossRef] [PubMed]
- Badhy, S.C.; Chowdhury, M.G.A.; Settypalli, T.B.K.; Cattoli, G.; Lamien, C.E.; Fakir, M.A.U.; Akter, S.; Osmani, M.G.; Talukdar, F.; Begum, N.; et al. Molecular characterization of lumpy skin disease virus (LSDV) emerged in Bangladesh reveals unique genetic features compared to contemporary field strains. BMC Vet. Res. 2021, 17, 61. [Google Scholar] [CrossRef]
- Tran, H.T.T.; Truong, A.D.; Dang, A.K.; Ly, D.V.; Nguyen, C.T.; Chu, N.T.; Hoang, T.V.; Nguyen, H.T.; Nguyen, V.T.; Dang, H.V. Lumpy skin disease outbreaks in vietnam, 2020. Transbound. Emerg. Dis. 2021, 68, 977–980. [Google Scholar] [CrossRef] [PubMed]
- EFSA; Calistri, P.; De Clercq, K.; Gubbins, S.; Klement, E.; Stegeman, A.; Cortinas Abrahantes, J.; Marojevic, D.; Antoniou, S.E.; Broglia, A.; et al. Scientific report on the lumpy skin disease epidemiological report IV: Data collection and analysis. EFSA J. 2020, 18, e06010. [Google Scholar] [CrossRef] [Green Version]
- Woods, J.A. Lumpy Skin Disease Virus. In Virus Infections of Ruminants; Dinter, Z., Morein, B., Eds.; Elsevier: Amsterdam, The Netherlands, 1990; Volume 3, pp. 53–67. [Google Scholar]
- Buller, R.M.; Arif, B.M.; Black, D.N.; Dumbell, K.R.; Esposito, J.J.; Lefkowitz, E.J.; McFadden, G.; Moss, B.; Mercer, A.A.; Moyer, R.W.; et al. Poxviridae. In Virus Taxonomy: Eight Report of the International Committee on the Taxonomy of Viruses; Fauquet, C.M., Mayo, M.A., Maniloff, J., Desselberger, U., Ball, L.A., Eds.; Elsevier Academic Press: Oxford, UK, 2005. [Google Scholar]
- Prozesky, L.; Barnard, B.J.H. A Study of the Pathology of Lumpy Skin-Disease in Cattle. Onderstepoort J. Vet. 1982, 49, 167–175. [Google Scholar]
- Weiss, K.E. Lumpy skin disease virus. Virololy Monogr. 1968, 3, 111–131. [Google Scholar]
- Casal, J.; Allepuz, A.; Miteva, A.; Pite, L.; Tabakovsky, B.; Terzievski, D.; Alexandrov, T.; Beltran-Alcrudo, D. Economic cost of lumpy skin disease outbreaks in three Balkan countries: Albania, Bulgaria and the Former Yugoslav Republic of Macedonia (2016–2017). Transbound. Emerg. Dis. 2018, 65, 1680–1688. [Google Scholar] [CrossRef] [PubMed]
- Katsoulos, P.D.; Chaintoutis, S.C.; Dovas, C.I.; Polizopoulou, Z.S.; Brellou, G.D.; Agianniotaki, E.I.; Tasioudi, K.E.; Chondrokouki, E.; Papadopoulos, O.; Karatzias, H.; et al. Investigation on the incidence of adverse reactions, viraemia and haematological changes following field immunization of cattle using a live attenuated vaccine against lumpy skin disease. Transbound. Emerg. Dis. 2018, 65, 174–185. [Google Scholar] [CrossRef]
- Chihota, C.M.; Rennie, L.F.; Kitching, R.P.; Mellor, P.S. Mechanical transmission of lumpy skin disease virus by Aedes aegypti (Diptera: Culicidae). Epidemiol. Infect. 2001, 126, 317–321. [Google Scholar] [CrossRef] [Green Version]
- Sohier, C.; Haegeman, A.; Mostin, L.; De Leeuw, I.; Campe, W.V.; De Vleeschauwer, A.; Tuppurainen, E.S.M.; van den Berg, T.; De Regge, N.; De Clercq, K. Experimental evidence of mechanical lumpy skin disease virus transmission by Stomoxys calcitrans biting flies and Haematopota spp. horseflies. Sci. Rep. 2019, 9, 20076. [Google Scholar] [CrossRef] [PubMed]
- Tuppurainen, E.S.M.; Lubinga, J.C.; Stoltsz, W.H.; Troskie, M.; Carpenter, S.T.; Coetzer, J.A.W.; Venter, E.H.; Oura, C.A.L. Mechanical transmission of lumpy skin disease virus by Rhipicephalus appendiculatus male ticks. Epidemiol. Infect. 2013, 141, 425–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lubinga, J.C.; Tuppurainen, E.S.M.; Stoltsz, W.H.; Ebersohn, K.; Coetzer, J.A.W.; Venter, E.H. Detection of lumpy skin disease virus in saliva of ticks fed on lumpy skin disease virus-infected cattle. Exp. Appl. Acarol. 2013, 61, 129–138. [Google Scholar] [CrossRef]
- Rouby, S.R.; Hussein, K.H.; Aboelhadid, S.M.; El-Sherif, A.M. Role of Rhipicephalus annulatus tick in transmission of lumpy skin disease virus in naturally infected cattle in Egypt. Adv. Anim. Vet. Sci. 2017, 5, 185–191. [Google Scholar] [CrossRef]
- Kononov, A.; Byadovskaya, O.; Wallace, D.B.; Prutnikov, P.; Pestova, Y.; Kononova, S.; Nesterov, A.; Rusaleev, V.; Lozovoy, D.; Sprygin, A. Non-vector-borne transmission of lumpy skin disease virus. Sci. Rep. 2020, 10, 7436. [Google Scholar]
- Annandale, C.H.; Holm, D.E.; Ebersohn, K.; Venter, E.H. Seminal Transmission of Lumpy Skin Disease Virus in Heifers. Transbound. Emerg. Dis. 2014, 61, 443–448. [Google Scholar] [CrossRef] [Green Version]
- Rouby, S.; Aboulsoud, E. Evidence of intrauterine transmission of lumpy skin disease virus. Vet. J. 2016, 209, 193–195. [Google Scholar] [CrossRef]
- Ince, O.B.; Cakir, S.; Dereli, M.A. Risk analysis of lumpy skin disease in Turkey. Indian J. Anim Res. 2016, 50, 1013–1017. [Google Scholar] [CrossRef] [Green Version]
- Ince, O.B.; Turk, T. Analyzing risk factors for lumpy skin disease by a geographic information system (GIS) in Turkey. J. Hell. Vet. Med. Soc. 2019, 70, 1797–1804. [Google Scholar]
- Sevik, M.; Dogan, M. Epidemiological and Molecular Studies on Lumpy Skin Disease Outbreaks in Turkey during 2014–2015. Transbound. Emerg. Dis. 2017, 64, 1268–1279. [Google Scholar] [CrossRef]
- Tuppurainen, E.; Alexandrov, T.; Beltrán-Alcrudo, D. Lumpy Skin Disease Field Manual—A Manual for Veterinarians; Food and Agriculture Organization of the United Nations (FAO): Roma, Italy, 2017; Volume 20, p. 60. [Google Scholar]
- OIE. Minimum Requirements for the Production and Quality Control of Vaccines (NB: Version adopted in May 2018) In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals; World Organisation for Animal Health (OIE): Paris, France, 2019; Volume 1. [Google Scholar]
- OIE. Tests for sterility and freedom from contamination of biological materials intended for veterinary use. In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals; World Organisation for Animal Health: Paris, France, 2019; Volume 1. [Google Scholar]
- OIE. Lumpy skin disease. In Manual of Diagnostic Tests and Vaccines for Terrestrial Animals; World Organisation for Animal Health: Paris, France, 2021; Volume 3. [Google Scholar]
- Tuppurainen, E.S.M.; Pearson, C.R.; Bachanek-Bankowska, K.; Knowles, N.J.; Amareen, S.; Frost, L.; Henstock, M.R.; Lamien, C.E.; Diallo, A.; Mertens, P.P.C. Characterization of sheep pox virus vaccine for cattle against lumpy skin disease virus. Antivir. Res. 2014, 109, 1–6. [Google Scholar] [CrossRef] [Green Version]
- Sprygin, A.; Pestova, Y.; Bjadovskaya, O.; Prutnikov, P.; Zinyakov, N.; Kononova, S.; Ruchnova, O.; Lozovoy, D.; Chvala, I.; Kononov, A. Evidence of recombination of vaccine strains of lumpy skin disease virus with field strains, causing disease. PLoS ONE 2020, 15, e0232584. [Google Scholar] [CrossRef]
- Kitching, R.P. Vaccines for lumpy skin disease, sheep pox and goat pox. In Vaccines for OIE List A and Emerging Animal Diseases, Proceedings of a Symposium, Ames, Iowa, USA, 16–18 September 2002: Proceedings (Developments in Biologicals, Vol. 114); Brown, F., Roth, J., Eds.; S. Karger: Basel, Switzerland, 2013; pp. 161–167. ISBN 9783805575775. [Google Scholar]
- Tuppurainen, E.S.M.; Venter, E.H.; Coetzer, J.A.W.; Bell-Sakyi, L. Lumpy skin disease: Attempted propagation in tick cell lines and presence of viral DNA in field ticks collected from naturally-infected cattle. Ticks Tick-Borne Dis. 2015, 6, 134–140. [Google Scholar] [CrossRef] [Green Version]
- Wallace, D.B.; Viljoen, G.J. Immune responses to recombinants of the South African vaccine strain of lumpy skin disease virus generated by using thymidine kinase gene insertion. Vaccine 2005, 23, 3061–3067. [Google Scholar] [CrossRef]
- Tuppurainen, E.S.M.; Antoniou, S.E.; Tsiamadis, E.; Topkaridou, M.; Labus, T.; Debeljak, Z.; Plavsic, B.; Miteva, A.; Alexandrov, T.; Pite, L.; et al. Field observations and experiences gained from the implementation of control measures against lumpy skin disease in South-East Europe between 2015 and 2017. Prev. Vet. Med. 2020, 181, 104600. [Google Scholar] [CrossRef] [PubMed]
- Haegeman, A.; De Leeuw, I.; Mostin, L.; Van Campe, W.; Aerts, L.; Venter, E.; Tuppurainen, E.; Saegerman, C.; De Clercq, K. Comparative Evaluation of Lumpy Skin Disease Virus-Based Live Attenuated Vaccines. Vaccines 2021, 9, 473. [Google Scholar] [CrossRef] [PubMed]
- Ayelet, G.; Abate, Y.; Sisay, T.; Nigussie, H.; Gelaye, E.; Jemberie, S.; Asmare, K. Lumpy skin disease: Preliminary vaccine efficacy assessment and overview on outbreak impact in dairy cattle at Debre Zeit, central Ethiopia. Antivir. Res. 2013, 98, 261–265. [Google Scholar] [CrossRef]
- Yeruham, I.; Nir, O.; Braverman, Y.; Davidson, M.; Grinstein, H.; Haymovitch, M.; Zamir, O. Spread of Lumpy Skin-Disease in Israeli Dairy Herds. Vet. Rec. 1995, 137, 91–93. [Google Scholar] [CrossRef]
- Salib, F.A.; Osman, A.H. Incidence of lumpy skin disease among Egyptian cattle in Giza Governorate, Egypt. Vet. World 2011, 4, 162–167. [Google Scholar] [CrossRef]
- Lamien, C.E.; Le Goff, C.; Silber, R.; Wallace, D.B.; Gulyaz, V.; Tuppurainen, E.; Madani, H.; Caufour, P.; Adam, T.; El Harrak, M.; et al. Use of the Capripoxvirus homologue of Vaccinia virus 30 kDa RNA polymerase subunit (RPO30) gene as a novel diagnostic and genotyping target: Development of a classical PCR method to differentiate Goat poxvirus from Sheep poxvirus. Vet. Microbiol. 2011, 149, 30–39. [Google Scholar] [CrossRef]
- Le Goff, C.; Lamien, C.E.; Fakhfakh, E.; Chadeyras, A.; Aba-Adulugba, E.; Libeau, G.; Tuppurainen, E.; Wallace, D.B.; Adam, T.; Silber, R.; et al. Capripoxvirus G-protein-coupled chemokine receptor: A host-range gene suitable for virus animal origin discrimination. J. Gen. Virol. 2009, 90, 1967–1977. [Google Scholar] [CrossRef] [PubMed]
- Tulman, E.R.; Afonso, C.L.; Lu, Z.; Zsak, L.; Sur, J.H.; Sandybaev, N.T.; Kerembekova, U.Z.; Zaitsev, V.L.; Kutish, G.F.; Rock, D.L. The genomes of sheeppox and goatpox viruses. J. Virol. 2002, 76, 6054–6061. [Google Scholar] [CrossRef] [Green Version]
- Davies, F.G.; Otema, C. Antibody-Response in Sheep Infected with a Kenyan Sheep and Goat Pox Virus. J. Comp. Pathol. 1978, 88, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Davies, F.G. Characteristics of a Virus Causing a Pox Disease in Sheep and Goats in Kenya, with Observations on Epidemiology and Control. J. Hyg. 1976, 76, 163–171. [Google Scholar] [CrossRef]
- Babiuk, S. Vaccines against lumpy skin disease virus and vaccination strategies. In Lumpy Skin Disease; Tuppurainen, E., Babiuk, S., Klement, E., Eds.; Springer: Berlin, Germany, 2018. [Google Scholar]
- Mathijs, E.; Vandenbussche, F.; Haegeman, A.; King, A.; Nthangeni, B.; Potgieter, C.; Maartens, L.; Van Borm, S.; De Clercq, K. Complete Genome Sequences of the Neethling-Like Lumpy Skin Disease Virus Strains Obtained Directly from Three Commercial Live Attenuated Vaccines. Genome Announc. 2016, 4, e01255-16, Erratum in Genome Announc. 2017, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gari, G.; Abie, G.; Gizaw, D.; Wubete, A.; Kidane, M.; Asgedom, H.; Bayissa, B.; Ayelet, G.; Oura, C.A.L.; Roger, F.; et al. Evaluation of the safety, immunogenicity and efficacy of three capripoxvirus vaccine strains against lumpy skin disease virus. Vaccine 2015, 33, 3256–3261. [Google Scholar] [CrossRef]
- Varshovi, H.R.; Norian, R.; Azadmehr, A.; Ahangaran, N.A. Immune response characteristics of Capri pox virus vaccines following emergency vaccination of cattle against lumpy skin disease virus. Iran. J. Vet. Sci. Technol. 2018, 9, 33–40. [Google Scholar] [CrossRef]
- Zhugunissov, K.; Bulatov, Y.; Orynbayev, M.; Kutumbetov, L.; Abduraimov, Y.; Shayakhmetov, Y.; Taranov, D.; Amanova, Z.; Mambetaliyev, M.; Absatova, Z.; et al. Goatpox virus (G20-LKV) vaccine strain elicits a protective response in cattle against lumpy skin disease at challenge with lumpy skin disease virulent field strain in a comparative study. Vet. Microbiol. 2020, 245, 108695. [Google Scholar] [CrossRef] [PubMed]
- Kayesh, M.E.H.; Hussan, M.T.; Hashem, M.A.; Eliyas, M.; Anower, A.K.M.M. Lumpy skin disease virus infection: An emerging threat to cattle health in Bangladesh. Hosts Viruses 2020, 7, 97–108. [Google Scholar]
- Ben-Gera, J.; Klement, E.; Khinich, E.; Stram, Y.; Shpigel, N.Y. Comparison of the efficacy of Neethling lumpy skin disease virus and x10RM65 sheep-pox live attenuated vaccines for the prevention of lumpy skin disease—The results of a randomized controlled field study. Vaccine 2015, 33, 4837–4842. [Google Scholar] [CrossRef] [PubMed]
- Abutarbush, S.M. Efficacy of vaccination against lumpy skin disease in Jordanian cattle. Vet. Rec. 2014, 175. [Google Scholar] [CrossRef]
- Abdallah, F.M.; El Damaty, H.M.; Kotb, G.F. Sporadic cases of lumpy skin disease among cattle in Sharkia province, Egypt: Genetic characterization of lumpy skin disease virus isolates and pathological findings. Vet. World 2018, 11, 1150–1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kasem, S.; Saleh, M.; Qasim, I.; Hashim, O.; Alkarar, A.; Abu-Obeida, A.; Gaafer, A.; Hussien, R.; AL-Sahaf, A.; Al-Doweriej, A.; et al. Outbreak investigation and molecular diagnosis of Lumpy skin disease among livestock in Saudi Arabia 2016. Transbound. Emerg. Dis. 2018, 65, e494–e500. [Google Scholar] [CrossRef] [PubMed]
- Somasundaram, M.K. An outbreak of lumpy skin disease in a Holstein dairy herds in Oman: A clinical report. Asian J. Anim. Vet. Adv. 2011, 6, 851–859. [Google Scholar]
- Khalafalla, A.I.; Gaffar Elamin, M.A.; Abbas, Z. Lumpy skin disease: Observations on the recent outbreaks of the disease in the Sudan. Rev. Elev. Med. Vet. Pays. Trop. 1993, 46, 548–550. [Google Scholar]
- Tageldin, M.H.; Wallace, D.B.; Gerdes, G.H.; Putterill, J.F.; Greyling, R.R.; Phosiwa, M.N.; Al Busaidy, R.M.; Al Ismaaily, S.I. Lumpy skin disease of cattle: An emerging problem in the Sultanate of Oman. Trop. Anim. Health Prod. 2014, 46, 241–246. [Google Scholar] [CrossRef] [Green Version]
- Brenner, J.; Bellaiche, M.; Gross, E.; Elad, D.; Oved, Z.; Haimovitz, M.; Wasserman, A.; Friedgut, O.; Stram, Y.; Bumbarov, V.; et al. Appearance of skin lesions in cattle populations vaccinated against lumpy skin disease: Statutory challenge. Vaccine 2009, 27, 1500–1503. [Google Scholar] [CrossRef]
- Rozstalnyy, A.; Aguanno, R.; Beltran-Alcrudo, D. Lumpy skin disease: Country situation and capacity reports. EMPRES-Anim. Health 360 2017, 47, 45–47. [Google Scholar]
- Abutarbush, S.M.; Tuppurainen, E.S.M. Serological and clinical evaluation of the Yugoslavian RM65 sheep pox strain vaccine use in cattle against lumpy skin disease. Transbound. Emerg. Dis. 2018, 65, 1657–1663. [Google Scholar] [CrossRef]
- Boumart, Z.; Daouam, S.; Belkourati, I.; Rafi, L.; Tuppurainen, E.; Tadlaoui, K.O.; El Harrak, M. Comparative innocuity and efficacy of live and inactivated sheeppox vaccines. BMC Vet. Res. 2016, 12, 133. [Google Scholar] [CrossRef] [Green Version]
- Hamdi, J.; Boumart, Z.; Daouam, S.; El Arkam, A.; Bamouh, Z.; Jazouli, M.; Tadlaoui, K.O.; Fihri, O.F.; Gavrilov, B.; El Harrak, M. Development and Evaluation of an Inactivated Lumpy Skin Disease Vaccine for Cattle. Vet. Microbiol. 2020, 245, 108689. [Google Scholar] [CrossRef]
- OIE. Infection with lumpy skin disease virus. In Terrestrial Animal Health Code; World Organization for Animal Health: Paris, France, 2021; Volume 2. [Google Scholar]
- Nash, A.A.; Dalziel, R.G.; Fitzgerald, J.R. (Eds.) Vaccines and How They Work. In Mims’ Pathogenesis of Infectious Disease, 6th ed.; Academic Press: Boston, MA, USA, 2015; pp. 291–303. [Google Scholar]
- Siegrist, C.-A. Vaccine Immunology. In Plotkin’s Vaccines, 7th ed.; Plotkin, S.A., Orenstein, W.A., Offit, P.A., Edwards, K.M., Eds.; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Kitching, P. Progress towards sheep and goat pox vaccines. Vaccine 1983, 1, 4–9. [Google Scholar] [CrossRef]
- Kitching, R.P. The control of sheep and goat pox. Rev. Sci. Tech. 1986, 5, 503–511. [Google Scholar] [CrossRef]
- Solyom, F.; Perenlei, L.; Roith, J. Sheep-pox vaccine prepared from formaldehyde inactivated virus adsorbed to aluminium hydroxide gel. Acta Microbiol. Acad. Sci. Hung. 1982, 29, 69–75. [Google Scholar] [PubMed]
- Wolff, J.; Moritz, T.; Schlottau, K.; Hoffmann, D.; Beer, M.; Hoffmann, B. Development of a Safe and Highly Efficient Inactivated Vaccine Candidate against Lumpy Skin Disease Virus. Vaccines 2021, 9, 4. [Google Scholar] [CrossRef]
- Norian, R.; Afzal Ahangaran, N.; Vashovi, H.R.; Azadmehr, A. Evaluation of Humoral and Cell-mediated Immunity of Two Capripoxvirus Vaccine Strains against Lumpy Skin Disease Virus. Iran. J. Virol. 2016, 10, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Norian, R.; Afzal Ahangaran, N.; Varshovi, H.R.; Azadmehr, A. Evaluation of Cell-mediated Immune Response in PBMCs of Calves Vaccinated by Capri Pox Vaccines Using ELISA and Real-time RT-PCR. Res. Mol. Med. 2017, 5, 3–8. [Google Scholar] [CrossRef] [Green Version]
- Carn, V.M. Control of Capripoxvirus Infections. Vaccine 1993, 11, 1275–1279. [Google Scholar] [CrossRef]
- Kitching, R.P.; Hammond, J.M.; Black, D.N. Studies on the major common precipitating antigen of capripoxvirus. J. Gen. Virol. 1986, 67, 139–148. [Google Scholar] [CrossRef]
- Milovanovic, M.; Dietze, K.; Milicevic, V.; Radojicic, S.; Valcic, M.; Moritz, T.; Hoffmann, B. Humoral immune response to repeated lumpy skin disease virus vaccination and performance of serological tests. BMC Vet. Res. 2019, 15, 80. [Google Scholar] [CrossRef] [Green Version]
- Haralambieva, I.H.; Oberg, A.L.; Dhiman, N.; Ovsyannikova, I.G.; Kennedy, R.B.; Grill, D.E.; Jacobson, R.M.; Poland, G.A. High-Dimensional Gene Expression Profiling Studies in High and Low Responders to Primary Smallpox Vaccination. J. Infect. Dis. 2012, 206, 1512–1520. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kennedy, R.B.; Oberg, A.L.; Ovsyannikova, I.G.; Haralambieva, I.H.; Grill, D.; Poland, G.A. Transcriptomic profiles of high and low antibody responders to smallpox vaccine. Genes Immun. 2013, 14, 277–285. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Agianniotaki, E.I.; Babiuk, S.; Katsoulos, P.D.; Chaintoutis, S.C.; Praxitelous, A.; Quizon, K.; Boscos, C.; Polizopoulou, Z.S.; Chondrokouki, E.D.; Dovas, C.I. Colostrum transfer of neutralizing antibodies against lumpy skin disease virus from vaccinated cows to their calves. Transbound. Emerg. Dis. 2018, 65, 2043–2048. [Google Scholar] [CrossRef]
- Samojlovic, M.; Polacek, V.; Gurjanov, V.; Lupulovic, D.; Lazic, G.; Petrovic, T.; Lazic, S. Detection of Antibodies against Lumpy Skin Disease Virus by Virus Neutralization Test and Elisa Methods. Acta Vet. 2019, 69, 47–60. [Google Scholar] [CrossRef] [Green Version]
- Milovanovic, M.; Milicevic, V.; Radojicic, S.; Valcic, M.; Hoffmann, B.; Dietze, K. Suitability of individual and bulk milk samples to investigate the humoral immune response to lumpy skin disease vaccination by ELISA. Virol. J. 2020, 17, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wolff, J.; Krstevski, K.; Beer, M.; Hoffmann, B. Minimum Infective Dose of a Lumpy Skin Disease Virus Field Strain from North Macedonia. Viruses 2020, 12, 768. [Google Scholar] [CrossRef]
- Agianniotaki, E.I.; Chaintoutis, S.C.; Haegeman, A.; Tasioudi, K.E.; De Leeuw, I.; Katsoulos, P.D.; Sachpatzidis, A.; De Clercq, K.; Alexandropoulos, T.; Polizopoulou, Z.S.; et al. Development and validation of a TaqMan probe-based real-time PCR method for the differentiation of wild type lumpy skin disease virus from vaccine virus strains. J. Virol. Methods 2017, 249, 48–57. [Google Scholar] [CrossRef]
- Menasherow, S.; Erster, O.; Rubinstein-Giuni, M.; Kovtunenko, A.; Eyngor, E.; Gelman, B.; Khinich, E.; Stram, Y. A high-resolution melting (HRM) assay for the differentiation between Israeli field and Neethling vaccine lumpy skin disease viruses. J. Virol. Methods 2016, 232, 12–15. [Google Scholar] [CrossRef]
- Sprygin, A.; Pestova, Y.; Prutnikov, P.; Kononov, A. Detection of vaccine-like lumpy skin disease virus in cattle and Musca domestica L. flies in an outbreak of lumpy skin disease in Russia in 2017. Transbound. Emerg. Dis. 2018, 65, 1137–1144. [Google Scholar] [CrossRef]
- Vidanovic, D.; Sekler, M.; Petrovic, T.; Debeljak, Z.; Vaskovic, N.; Matovic, K.; Hoffmann, B. Real-Time Pcr Assays for the Specific Detection of Field Balkan Strains of Lumpy Skin Disease Virus. Acta Vet. 2016, 66, 444–454. [Google Scholar] [CrossRef]
- Kitching, R.P.; Hammond, J.M. Poxvirus, infection and immunity. In Encyclopaedia of Immunology; Roitt, I.M., Delves, P.J., Eds.; Academic Press: London, UK, 1992; pp. 1261–1264. [Google Scholar]
- Morgenstern, M.; Klement, E. The Effect of Vaccination with Live Attenuated Neethling Lumpy Skin Disease Vaccine on Milk Production and Mortality-An Analysis of 77 Dairy Farms in Israel. Vaccines 2020, 8, 324. [Google Scholar] [CrossRef]
- Bedekovic, T.; Simic, I.; Kresic, N.; Lojkic, I. Detection of lumpy skin disease virus in skin lesions, blood, nasal swabs and milk following preventive vaccination. Transbound. Emerg. Dis. 2018, 65, 491–496. [Google Scholar] [CrossRef]
- Lojkic, I.; Simic, I.; Kresic, N.; Bedekovic, T. Complete Genome Sequence of a Lumpy Skin Disease Virus Strain Isolated from the Skin of a Vaccinated Animal. Genome Announc. 2018, 6, e00482-18. [Google Scholar] [CrossRef]
- Gershon, P.D.; Black, D.N. A Capripoxvirus Pseudogene Whose Only Intact Homologs Are in Other Poxvirus Genomes. Virology 1989, 172, 350–354. [Google Scholar] [CrossRef]
- Sprygin, A.; Artyuchova, E.; Babin, Y.; Prutnikov, P.; Kostrova, E.; Byadovskaya, O.; Kononov, A. Epidemiological characterization of lumpy skin disease outbreaks in Russia in 2016. Transbound. Emerg. Dis. 2018, 65, 1514–1521. [Google Scholar] [CrossRef]
- Sprygin, A.; Babin, Y.; Pestova, Y.; Kononova, S.; Wallace, D.B.; Van Schalkwyk, A.; Byadovskaya, O.; Diev, V.; Lozovoy, D.; Kononov, A. Analysis and insights into recombination signals in lumpy skin disease virus recovered in the field. PLoS ONE 2018, 13, e0207480. [Google Scholar] [CrossRef]
- Fenner, F.; Comben, B.M. Genetic studies with mammalian poxviruses. I. Demonstration of recombination between two strains of vaccina virus. Virology 1958, 5, 530–548. [Google Scholar] [CrossRef] [PubMed]
- Woodroofe, G.M.; Fenner, F. Genetic Studies with Mammalian Poxviruses: IV. Hybridization between Several Different Poxviruses. Virology 1960, 12, 272–282. [Google Scholar] [CrossRef]
- Bedson, H.S.; Dumbell, K.R. Hybrids Derived from Viruses of Variola Major and Cowpox. J. Hyg. 1964, 62, 147–158. [Google Scholar] [CrossRef] [Green Version]
- Qin, L.; Favis, N.; Famulski, J.; Evans, D.H. Evolution of and Evolutionary Relationships between Extant Vaccinia Virus Strains. J. Virol. 2015, 89, 1809–1824. [Google Scholar] [CrossRef] [Green Version]
- Qin, L.; Upton, C.; Hazes, B.; Evans, D.H. Genomic Analysis of the Vaccinia Virus Strain Variants Found in Dryvax Vaccine. J. Virol. 2011, 85, 13049–13060. [Google Scholar] [CrossRef] [Green Version]
- Saltykov, Y.V.; Kolosova, A.A.; Filonova, N.N.; Chichkin, A.N.; Feodorova, V.A. Genetic Evidence of Multiple Introductions of Lumpy Skin Disease Virus into Saratov Region, Russia. Pathogens 2021, 10, 716. [Google Scholar] [CrossRef] [PubMed]
- Disney, W.T.; Green, J.W.; Forsythe, K.W.; Wiemers, J.F.; Weber, S. Benefit-cost analysis of animal identification for disease prevention and control. Rev. Sci. Tech. 2001, 20, 385–405. [Google Scholar] [CrossRef] [PubMed]
- Davies, F.G. Lumpy skin disease of cattle: A growing problem in Africa and the Near East. World Anim. Rev. 1991, 68, 37–42. [Google Scholar]
- Ochwo, S.; VanderWaal, K.; Munsey, A.; Ndekezi, C.; Mwebe, R.; Okurut, A.R.A.; Nantima, N.; Mwiine, F.N. Spatial and temporal distribution of lumpy skin disease outbreaks in Uganda (2002–2016). BMC Vet. Res. 2018, 14, 174. [Google Scholar] [CrossRef]
- Molla, W.; de Jong, M.C.M.; Gari, G.; Frankena, K. Economic impact of lumpy skin disease and cost effectiveness of vaccination for the control of outbreaks in Ethiopia. Prev. Vet. Med. 2017, 147, 100–107. [Google Scholar] [CrossRef] [Green Version]
- Molini, U.; Aikukutu, G.; Khaiseb, S.; Haindongo, N.N.; Lilungwe, A.C.; Cattoli, G.; Dundon, W.G.; Lamien, C.E. Molecular characterization of lumpy skin disease virus in Namibia, 2017. Arch. Virol. 2018, 163, 2525–2529. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, F.G. Lumpy skin disease, an African capripox virus disease of cattle. Br. Vet. J. 1991, 147, 489–503. [Google Scholar] [CrossRef]
- Osuagwuh, U.I.; Bagla, V.; Venter, E.H.; Annandale, C.H.; Irons, P.C. Absence of lumpy skin disease virus in semen of vaccinated bulls following vaccination and subsequent experimental infection. Vaccine 2007, 25, 2238–2243. [Google Scholar] [CrossRef] [Green Version]
- EFSA. Scientific Opinion on lumpy skin disease. EFSA J. 2015, 13, 73. [Google Scholar] [CrossRef]
- Calistri, P.; DeClercq, K.; De Vleeschauwer, A.; Gubbins, S.; Klement, E.; Stegeman, A.; Abrahantes, J.C.; Antoniou, S.E.; Broglia, A.; Gogin, A.; et al. Lumpy skin disease: Scientific and technical assistance on control and surveillance activities. EFSA J. 2018, 16, e05452. [Google Scholar] [CrossRef] [PubMed]
- Bessell, P.R.; Auty, H.K.; Roberts, H.; McKendrick, I.J.; Bronsvoort, B.M.D.; Boden, L.A. A Tool for Prioritizing Livestock Disease Threats to Scotland. Front. Vet. Sci. 2020, 7, 223. [Google Scholar] [CrossRef] [PubMed]
- Gale, P.; Kelly, L.; Snary, E.L. Qualitative assessment of the entry of capripoxviruses into Great Britain from the European Union through importation of ruminant hides, skins and wool. Microb. Risk Anal. 2016, 1, 13–18. [Google Scholar] [CrossRef] [Green Version]
- Horigan, V.; Beard, P.M.; Roberts, H.; Adkin, A.; Gale, P.; Batten, C.A.; Kelly, L. Assessing the probability of introduction and transmission of Lumpy skin disease virus within the United Kingdom. Microb. Risk Anal. 2018, 9, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Friedrich-Loeffler-Institut. Qualitative Risikobewertung zur Einschleppung von Lumpy Skin Disease (LSD; auch Dermatitis nodularis) in die Bundesrepublik Deutschland. 2016. Available online: https://www.openagrar.de/servlets/MCRFileNodeServlet/openagrar_derivate_00000698/LSD_Risikobewertung_2016-11-10.pdf (accessed on 5 October 2021).
- Saegerman, C.; Bertagnoli, S.; Meyer, G.; Ganiere, J.P.; Caufour, P.; De Clercq, K.; Jacquiet, P.; Fournie, G.; Hautefeuille, C.; Etore, F.; et al. Risk of introduction of lumpy skin disease in France by the import of vectors in animal trucks. PLoS ONE 2018, 13, e0198506. [Google Scholar] [CrossRef]
- Allepuz, A.; Casal, J.; Beltran-Alcrudo, D. Spatial analysis of lumpy skin disease in Eurasia-Predicting areas at risk for further spread within the region. Transbound. Emerg. Dis. 2019, 66, 813–822. [Google Scholar] [CrossRef]
- Taylor, R.A.; Berriman, A.D.C.; Gale, P.; Kelly, L.A.; Snary, E.L. A generic framework for spatial quantitative risk assessments of infectious diseases: Lumpy skin disease case study. Transbound. Emerg. Dis. 2019, 66, 131–143. [Google Scholar] [CrossRef] [Green Version]
- Kahana-Sutin, E.; Klement, E.; Lensky, I.; Gottlieb, Y. High relative abundance of the stable fly Stomoxys calcitrans is associated with lumpy skin disease outbreaks in Israeli dairy farms. Med. Vet. Entomol. 2017, 31, 150–160. [Google Scholar] [CrossRef]
- Babiuk, S.; Bowden, T.R.; Boyle, D.B.; Wallace, D.B.; Kitching, R.P. Capripoxviruses: An emerging worldwide threat to sheep, goats and cattle. Transbound. Emerg. Dis. 2008, 55, 263–272. [Google Scholar] [CrossRef] [Green Version]
- Machado, G.; Korennoy, F.; Alvarez, J.; Picasso-Risso, C.; Perez, A.; VanderWaal, K. Mapping changes in the spatiotemporal distribution of lumpy skin disease virus. Transbound. Emerg. Dis. 2019, 66, 2045–2057. [Google Scholar] [CrossRef]
- Annandale, C.H.; Smuts, M.P.; Ebersohn, K.; du Plessis, L.; Thompson, P.N.; Venter, E.H.; Stout, T.A.E. Effect of using frozen-thawed bovine semen contaminated with lumpy skin disease virus on in vitro embryo production. Transbound. Emerg. Dis. 2019, 66, 1539–1547. [Google Scholar] [CrossRef]
- Ochwo, S.; VanderWaal, K.; Munsey, A.; Nkamwesiga, J.; Ndekezi, C.; Auma, E.; Mwiine, F.N. Seroprevalence and risk factors for lumpy skin disease virus seropositivity in cattle in Uganda. BMC Vet. Res. 2019, 15, 236. [Google Scholar] [CrossRef] [Green Version]
- Kiplagat, S.K.; Kitala, P.M.; Onono, J.O.; Beard, P.M.; Lyons, N.A. Risk Factors for Outbreaks of Lumpy Skin Disease and the Economic Impact in Cattle Farms of Nakuru County, Kenya. Front. Vet. Sci. 2020, 7, 259. [Google Scholar] [CrossRef]
- Chamchod, F. Modeling the spread of capripoxvirus among livestock and optimal vaccination strategies. J. Biol. 2018, 437, 179–186. [Google Scholar] [CrossRef]
- EFSA. Urgent advice on lumpy skin disease. EFSA J. 2016, 14. [Google Scholar] [CrossRef]
- Givens, M.D. Review: Risks of disease transmission through semen in cattle. Animal 2018, 12, S165–S171. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sprygin, A.; Pestova, Y.; Wallace, D.B.; Tuppurainen, E.; Kononov, A.V. Transmission of lumpy skin disease virus: A short review. Virus Res. 2019, 269, 197637. [Google Scholar] [CrossRef] [PubMed]
- Beard, P.M. Lumpy skin disease: A direct threat to Europe. Vet. Rec. 2016, 178, 557–558. [Google Scholar] [CrossRef] [Green Version]
- Aspden, K.; van Dijk, A.A.; Bingham, J.; Cox, D.; Passmore, J.A.; Williamson, A.L. Immunogenicity of a recombinant lumpy skin disease virus (neethling vaccine strain) expressing the rabies virus glycoprotein in cattle. Vaccine 2002, 20, 2693–2701. [Google Scholar] [CrossRef]
- Ngichabe, C.K.; Binepal, Y.S.; Njiru, J.W.; Carn, V.M. Evaluation of an immunocapture enzyme-linked immunosorbent assay for detection of capripoxviruses. Vet. Rec. 1999, 145, 231–232. [Google Scholar] [CrossRef]
- Ngichabe, C.K.; Wamwayi, H.M.; Barrett, T.; Ndungu, E.K.; Black, D.N.; Bostock, C.J. Trial of a capripoxvirus-rinderpest recombinant vaccine in African cattle. Epidemiol. Infect. 1997, 118, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.B.; Mather, A.; Kara, P.D.; Naicker, L.; Mokoena, N.B.; Pretorius, A.; Nefefe, T.; Thema, N.; Babiuk, S. Protection of Cattle Elicited Using a Bivalent Lumpy Skin Disease Virus-Vectored Recombinant Rift Valley Fever Vaccine. Front. Vet. Sci. 2020, 7, 256. [Google Scholar] [CrossRef]
- Burgers, W.A.; Ginbot, Z.; Shen, Y.J.; Chege, G.K.; Soares, A.P.; Muller, T.L.; Bunjun, R.; Kiravu, A.; Munyanduki, H.; Douglass, N.; et al. The novel Capripoxvirus vector lumpy skin disease virus efficiently boosts modified vaccinia Ankara human immunodeficiency virus responses in rhesus macaques. J. Gen. Virol. 2014, 95, 2267–2272. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.; Douglass, N.J.; Shephard, E.; Williamson, A. Lumpy Skin Disease Virus, a Novel Poxvirus Vector for Candidate HIV-1 Vaccines. Aids Res. Hum. Retrov. 2008, 24, 137–138. [Google Scholar]
- FAO. Emergence of lumpy skin disease in the Eastern Mediterranean Basin countries. EMPRES Watch 2013, 29. [Google Scholar]
- FAO. Emergence of lumpy skin disease (LSD) in Europe. EMPRES Watch 2015, 33. [Google Scholar]
- FAO. Sustainable prevention, control and elimination of Lumpy Skin Disease—Eastern Europe and the Balkans. FAO Anim. Prod. Health Position Pap. 2017, 2. [Google Scholar]
- Mainda, G.; Bessell, P.R.; Muma, J.B.; McAteer, S.P.; Chase-Topping, M.E.; Gibbons, J.; Stevens, M.P.; Gally, D.L.; deC Bronsvoort, B.M. Prevalence and patterns of antimicrobial resistance among Escherichia coli isolated from Zambian dairy cattle across different production systems. Sci. Rep. 2015, 5, 12439. [Google Scholar] [CrossRef] [Green Version]
- Mainda, G.; Bessell, P.R.; Muma, J.B.; McAteer, S.P.; Chase-Topping, M.E.; Gibbons, J.; Stevens, M.P.; Gally, D.L.; deC Bronsvoort, B.M. Erratum: Prevalence and patterns of antimicrobial resistance among Escherichia coli isolated from Zambian dairy cattle across different production systems. Sci. Rep. 2015, 5, 14162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zinsstag, J.; Schelling, E.; Walter-Toews, D.; Whittaker, M.; Tanner, M. One Health: The Theory and Practice of Integrated Health Approaches; CABI: Oxfordshire, UK, 2015. [Google Scholar]
- Schelling, E.; Wyss, K.; Bechir, M.; Moto, D.D.; Zinsstag, J. Synergy between public health and veterinary services to deliver human and animal health interventions in rural low income settings. BMJ-Brit. Med. J. 2005, 331, 1264–1267. [Google Scholar] [CrossRef] [Green Version]
- Schelling, E.; Bechir, M.; Ahmed, M.A.; Wyss, K.; Randolph, T.F.; Zinsstag, J. Human and animal vaccination delivery to remote nomadic families, Chad. Emerg. Infect. Dis. 2007, 13, 373–379. [Google Scholar] [CrossRef] [PubMed]
| Manufacturer | Product Name and Virus Strain | Target Species | Titre, Dose, Administration | Presentation Doses/Vial |
|---|---|---|---|---|
| Onderstepoort Biological Products (OBP) South Africa Email: info@obpvaccines.co.za http://www.obpvaccines.co.za (accessed on 22 September 2021) | Lumpy Skin Disease Vaccine for Cattle (LSD Neethling strain) | Cattle | Not known 2 ml SC | 25/50 |
| Intervet (Pty) South Africa/MSD Animal Healthhttp://www.msd-animal-health.co.za (accessed on 29 September 2021) | Lumpyvax™ (LSD SIS Neethling type strain) | Cattle | 104.0TCID50/dose 1 ml SC | 20/100 |
| MCI Santé Animale Morocco Email: contact@mci-santeanimale.com http://www.mci-santeanimale.com/en/ (accessed on 29 September 2021) | Bovivax-LSD™ (LSD Neethling strain) | Cattle | 103.5TCID50/dose 2 ml SC | 25/50/100 |
| Jordan Bio-Industries Center (JOVAC) Jordan Email: sales@jovaccenter.com http://www.jovaccenter.com (accessed on 29 September 2021) | LumpyShield-N™ (LSD Neethling strain) | Cattle | 104.0TCID50/dose 1 ml SC | 5/10/25/50/100 |
| Middle East for Vaccines (MEVAC) Egypt Email: marketing@me_vac.com https://www.me-vac.com/about (accessed on 29 September 2021) | MEVAC LSD (LSD Neethling strain) | Cattle | 103.5TCID50/dose 1 ml SC | 10/25/50 |
| National Veterinary Institute (NVI) Ethiopia Email: nvi-rt@ethionet.et | Lumpy Skin Disease Vaccine (LSD Neethling strain) | Cattle | 103.0TCID50/dose 1 ml SC | 5/20/100 |
| Kenya Veterinary Vaccines Production Institute (KEVEVAPI) http://www.kevevapi.org/ (accessed on 29 September 2021) | Lumpivax™ (Live attenuated LSDV) | Cattle | TCID50 not known 2 ml SC | 50/100/150 |
| Pendik Veterinary Control Institute/ Ministry of Agriculture, Turkey | Penpox-M™ Live SPPV (Bakirköy SPPV strain) | Cattle | 102.5TCID50/dose 3 ml SC | |
| Vetal Company Turkey Email: vetal@vetal.com.tr http://www.vetal.com.tr (accessed on 29 September 2021) | Poxvac™ (Bakirköy SPPV strain) Lumpyvac™ (LSD Neethling strain) | Sheep Cattle Cattle | 102.5TCID50/dose 3ml SC 103.5TCID50/dose 2 ml SC | 20/50/100/200 10/25/50/100 |
| Dollvet Turkey Email: dollvet@dollvet.com.tr http://www.dollvet.com.tr (accessed on 29 September 2021) | Poxdoll™ (Bakirköy SPPV strain) LSD-NDOLL (LSD Neethling strain) | Cattle Sheep Goats Cattle | 102.5TCID50/dose 3ml SC 103.5TCID50/dose3ml SC | 50/100 10/25/50/100 |
| FGBI-Federal Centre for Animal Health, The Russian Federation Email: mail@arriah.ru http://www.arriah.ru (accessed on 29 September 2021) | Sheep Pox Cultyral Dry™(Arriah SPPV strain) | Sheep Cattle | Not known | 50/100 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tuppurainen, E.; Dietze, K.; Wolff, J.; Bergmann, H.; Beltran-Alcrudo, D.; Fahrion, A.; Lamien, C.E.; Busch, F.; Sauter-Louis, C.; Conraths, F.J.; et al. Review: Vaccines and Vaccination against Lumpy Skin Disease. Vaccines 2021, 9, 1136. https://doi.org/10.3390/vaccines9101136
Tuppurainen E, Dietze K, Wolff J, Bergmann H, Beltran-Alcrudo D, Fahrion A, Lamien CE, Busch F, Sauter-Louis C, Conraths FJ, et al. Review: Vaccines and Vaccination against Lumpy Skin Disease. Vaccines. 2021; 9(10):1136. https://doi.org/10.3390/vaccines9101136
Chicago/Turabian StyleTuppurainen, Eeva, Klaas Dietze, Janika Wolff, Hannes Bergmann, Daniel Beltran-Alcrudo, Anna Fahrion, Charles Euloge Lamien, Frank Busch, Carola Sauter-Louis, Franz J. Conraths, and et al. 2021. "Review: Vaccines and Vaccination against Lumpy Skin Disease" Vaccines 9, no. 10: 1136. https://doi.org/10.3390/vaccines9101136
APA StyleTuppurainen, E., Dietze, K., Wolff, J., Bergmann, H., Beltran-Alcrudo, D., Fahrion, A., Lamien, C. E., Busch, F., Sauter-Louis, C., Conraths, F. J., De Clercq, K., Hoffmann, B., & Knauf, S. (2021). Review: Vaccines and Vaccination against Lumpy Skin Disease. Vaccines, 9(10), 1136. https://doi.org/10.3390/vaccines9101136







