Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Quality Assessment
2.5. Data Analysis
3. Results
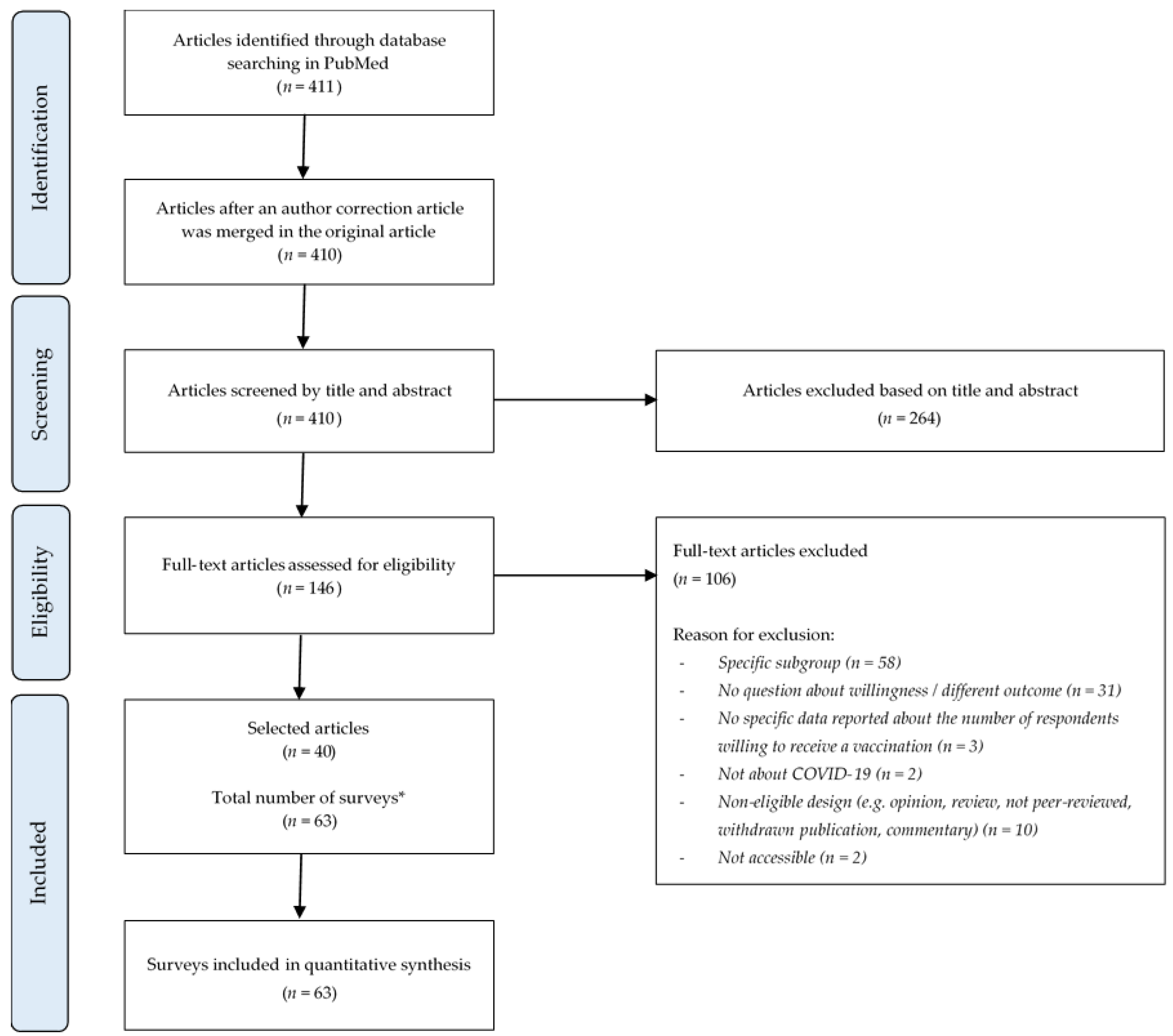
3.1. Search Results
3.2. Study Characteristics
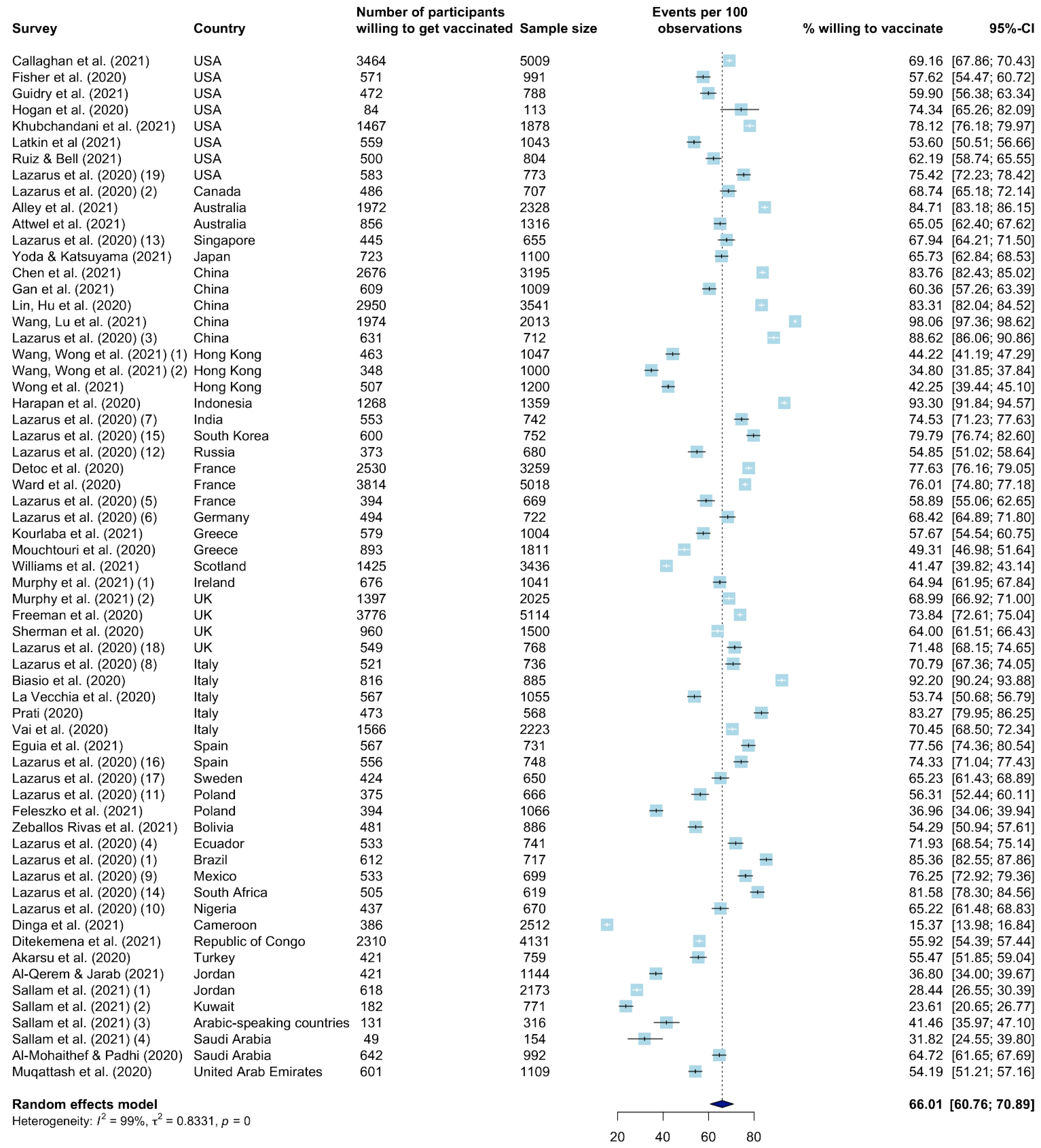
3.3. Worldwide Vaccination Willingness
3.4. Determinant Assessment
3.5. Risk of Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- MacDonald, N.E. SAGE Working Group on Vaccine Hesitancy Vaccine Hesitancy: Definition, Scope and Determinants. Vaccine 2015, 33, 4161–4164. [Google Scholar] [CrossRef] [PubMed]
- Sanyaolu, A.; Okorie, C.; Marinkovic, A.; Ayodele, O.; Abbasi, A.F.; Prakash, S.; Gosse, J.; Younis, S.; Mangat, J.; Chan, H. Measles Outbreak in Unvaccinated and Partially Vaccinated Children and Adults in the United States and Canada (2018–2019): A Narrative Review of Cases. Inquiry 2019, 56, 0046958019894098. [Google Scholar] [CrossRef] [PubMed]
- The Lancet Child & Adolescent Health Vaccine Hesitancy: A Generation at Risk. Lancet Child Adolesc. Health 2019, 3, 281. [CrossRef]
- World Health Organization [WHO]. Ten Threats to Global Health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 17 July 2021).
- Larson, H.J.; Jarrett, C.; Eckersberger, E.; Smith, D.M.D.; Paterson, P. Understanding Vaccine Hesitancy around Vaccines and Vaccination from a Global Perspective: A Systematic Review of Published Literature, 2007–2012. Vaccine 2014, 32, 2150–2159. [Google Scholar] [CrossRef]
- Timeline: WHO’s COVID-19 Response. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed on 17 July 2021).
- Troiano, G.; Nardi, A. Vaccine Hesitancy in the Era of COVID-19. Public Health 2021, 194, 245–251. [Google Scholar] [CrossRef]
- Afolabi, A.A.; Ilesanmi, O.S. Dealing with Vaccine Hesitancy in Africa: The Prospective COVID-19 Vaccine Context. Pan Afr. Med. J. 2021, 38, 3. [Google Scholar] [CrossRef]
- Neumann-Böhme, S.; Varghese, N.E.; Sabat, I.; Barros, P.P.; Brouwer, W.; van Exel, J.; Schreyögg, J.; Stargardt, T. Once We Have It, Will We Use It? A European Survey on Willingness to Be Vaccinated against COVID-19. Eur. J. Health Econ. 2020, 21, 977–982. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.Y.; Ho, K.F.; Cheung, A.W.L.; Chan, E.Y.Y.; Yeoh, E.K.; Wong, S.Y.S. Intention of Nurses to Accept Coronavirus Disease 2019 Vaccination and Change of Intention to Accept Seasonal Influenza Vaccination during the Coronavirus Disease 2019 Pandemic: A Cross-Sectional Survey. Vaccine 2020, 38, 7049–7056. [Google Scholar] [CrossRef]
- Dror, A.A.; Eisenbach, N.; Taiber, S.; Morozov, N.G.; Mizrachi, M.; Zigron, A.; Srouji, S.; Sela, E. Vaccine Hesitancy: The next Challenge in the Fight against COVID-19. Eur. J. Epidemiol. 2020, 35, 775–779. [Google Scholar] [CrossRef]
- Head, K.J.; Kasting, M.L.; Sturm, L.A.; Hartsock, J.A.; Zimet, G.D. A National Survey Assessing SARS-CoV-2 Vaccination Intentions: Implications for Future Public Health Communication Efforts. Sci. Commun. 2020, 42, 698–723. [Google Scholar] [CrossRef]
- Lin, C.; Tu, P.; Beitsch, L.M. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines 2020, 9, 16. [Google Scholar] [CrossRef]
- Wang, Q.; Yang, L.; Jin, H.; Lin, L. Vaccination against COVID-19: A Systematic Review and Meta-Analysis of Acceptability and Its Predictors. Prev. Med. 2021, 150, 106694. [Google Scholar] [CrossRef]
- Joanna Briggs Institute Critical Appraisal Tools|Joanna Briggs Institute. Available online: https://jbi.global/critical-appraisal-tools (accessed on 19 July 2021).
- Joanna Briggs Institute, Faculty of Health and Medical Sciences, The University of Adelaide. Critical Appraisal Tools|Joanna Briggs Institute. Available online: https://jbi.global/critical-appraisal-tools (accessed on 19 July 2021).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Lazarus, J.V.; Ratzan, S.C.; Palayew, A.; Gostin, L.O.; Larson, H.J.; Rabin, K.; Kimball, S.; El-Mohandes, A. A Global Survey of Potential Acceptance of a COVID-19 Vaccine. Nat. Med. 2021, 27, 225–228. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.; Dababseh, D.; Eid, H.; Al-Mahzoum, K.; Al-Haidar, A.; Taim, D.; Yaseen, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. High Rates of COVID-19 Vaccine Hesitancy and Its Association with Conspiracy Beliefs: A Study in Jordan and Kuwait among Other Arab Countries. Vaccines 2021, 9, 42. [Google Scholar] [CrossRef]
- Murphy, J.; Vallières, F.; Bentall, R.P.; Shevlin, M.; McBride, O.; Hartman, T.K.; McKay, R.; Bennett, K.; Mason, L.; Gibson-Miller, J.; et al. Psychological Characteristics Associated with COVID-19 Vaccine Hesitancy and Resistance in Ireland and the United Kingdom. Nat. Commun. 2021, 12, 29. [Google Scholar] [CrossRef]
- Wang, K.; Wong, E.L.-Y.; Ho, K.-F.; Cheung, A.W.-L.; Yau, P.S.-Y.; Dong, D.; Wong, S.Y.-S.; Yeoh, E.-K. Change of Willingness to Accept COVID-19 Vaccine and Reasons of Vaccine Hesitancy of Working People at Different Waves of Local Epidemic in Hong Kong, China: Repeated Cross-Sectional Surveys. Vaccines 2021, 9, 62. [Google Scholar] [CrossRef]
- Akarsu, B.; Canbay Özdemir, D.; Ayhan Baser, D.; Aksoy, H.; Fidancı, İ.; Cankurtaran, M. While Studies on COVID-19 Vaccine Is Ongoing, the Public’s Thoughts and Attitudes to the Future COVID-19 Vaccine. Int. J. Clin. Pract. 2021, 75, e13891. [Google Scholar] [CrossRef]
- Alley, S.J.; Stanton, R.; Browne, M.; To, Q.G.; Khalesi, S.; Williams, S.L.; Thwaite, T.L.; Fenning, A.S.; Vandelanotte, C. As the Pandemic Progresses, How Does Willingness to Vaccinate against COVID-19 Evolve? Int. J. Environ. Res. Public Health 2021, 18, 797. [Google Scholar] [CrossRef]
- Biasio, L.R.; Bonaccorsi, G.; Lorini, C.; Pecorelli, S. Assessing COVID-19 Vaccine Literacy: A Preliminary Online Survey. Hum. Vaccines Immunother. 2021, 17, 1304–1312. [Google Scholar] [CrossRef]
- Callaghan, T.; Moghtaderi, A.; Lueck, J.A.; Hotez, P.; Strych, U.; Dor, A.; Fowler, E.F.; Motta, M. Correlates and Disparities of Intention to Vaccinate against COVID-19. Soc. Sci. Med. 2021, 272, 113638. [Google Scholar] [CrossRef]
- Chen, M.; Li, Y.; Chen, J.; Wen, Z.; Feng, F.; Zou, H.; Fu, C.; Chen, L.; Shu, Y.; Sun, C. An Online Survey of the Attitude and Willingness of Chinese Adults to Receive COVID-19 Vaccination. Hum. Vaccines Immunother. 2021, 17, 2279–2288. [Google Scholar] [CrossRef]
- Dinga, J.N.; Sinda, L.K.; Titanji, V.P.K. Assessment of Vaccine Hesitancy to a COVID-19 Vaccine in Cameroonian Adults and Its Global Implication. Vaccines 2021, 9, 175. [Google Scholar] [CrossRef]
- Feleszko, W.; Lewulis, P.; Czarnecki, A.; Waszkiewicz, P. Flattening the Curve of COVID-19 Vaccine Rejection—An International Overview. Vaccines 2021, 9, 44. [Google Scholar] [CrossRef] [PubMed]
- Khubchandani, J.; Sharma, S.; Price, J.H.; Wiblishauser, M.J.; Sharma, M.; Webb, F.J. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. J. Community Health 2021, 46, 270–277. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.B.; Bell, R.A. Predictors of Intention to Vaccinate against COVID-19: Results of a Nationwide Survey. Vaccine 2021, 39, 1080–1086. [Google Scholar] [CrossRef]
- Hogan, C.; Atta, M.; Anderson, P.; Stead, T.; Solomon, M.; Banerjee, P.; Sleigh, B.; Shivdat, J.; Webb McAdams, A.; Ganti, L. Knowledge and Attitudes of Us Adults Regarding COVID-19. Int. J. Emerg. Med. 2020, 13, 53. [Google Scholar] [CrossRef] [PubMed]
- Freeman, D.; Loe, B.S.; Chadwick, A.; Vaccari, C.; Waite, F.; Rosebrock, L.; Jenner, L.; Petit, A.; Lewandowsky, S.; Vanderslott, S.; et al. COVID-19 Vaccine Hesitancy in the UK: The Oxford Coronavirus Explanations, Attitudes, and Narratives Survey (Oceans) II. Psychol. Med. 2020, 1–15. [Google Scholar] [CrossRef]
- Ward, J.K.; Alleaume, C.; Peretti-Watel, P.; Peretti-Watel, P.; Seror, V.; Cortaredona, S.; Launay, O.; Raude, J.; Verger, P.; Beck, F.; et al. The French Public’s Attitudes to a Future COVID-19 Vaccine: The Politicization of a Public Health Issue. Soc. Sci. Med. 2020, 265, 113414. [Google Scholar] [CrossRef]
- Fisher, K.A.; Bloomstone, S.J.; Walder, J.; Crawford, S.; Fouayzi, H.; Mazor, K.M. Attitudes Toward a Potential SARS-CoV-2 Vaccine: A Survey of U.S. Adults. Ann. Intern. Med. 2020, 173, 964–973. [Google Scholar] [CrossRef]
- Guidry, J.P.D.; Laestadius, L.I.; Vraga, E.K.; Miller, C.A.; Perrin, P.B.; Burton, C.W.; Ryan, M.; Fuemmeler, B.F.; Carlyle, K.E. Willingness to Get the COVID-19 Vaccine with and without Emergency Use Authorization. Am. J. Infect. Control 2021, 49, 137–142. [Google Scholar] [CrossRef]
- Latkin, C.A.; Dayton, L.; Yi, G.; Colon, B.; Kong, X. Mask Usage, Social Distancing, Racial, and Gender Correlates of COVID-19 Vaccine Intentions among Adults in the US. PLoS ONE 2021, 16, e0246970. [Google Scholar] [CrossRef]
- La Vecchia, C.; Negri, E.; Alicandro, G.; Scarpino, V. Attitudes towards Influenza Vaccine and a Potential COVID-19 Vaccine in Italy and Differences across Occupational Groups, September 2020: Attitudes towards Influenza Vaccine and a Potential COVID-19 Vaccine in Italy. Med. Del. Lav. Work Environ. Health 2020, 111, 445–448. [Google Scholar] [CrossRef]
- Vai, B.; Cazzetta, S.; Ghiglino, D.; Parenti, L.; Saibene, G.; Toti, M.; Verga, C.; Wykowska, A.; Benedetti, F. Risk Perception and Media in Shaping Protective Behaviors: Insights From the Early Phase of COVID-19 Italian Outbreak. Front. Psychol. 2020, 11, 563426. [Google Scholar] [CrossRef]
- Prati, G. Intention to Receive a Vaccine against SARS-CoV-2 in Italy and Its Association with Trust, Worry and Beliefs about the Origin of the Virus. Health Educ. Res. 2020, 35, 505–511. [Google Scholar] [CrossRef]
- Al-Mohaithef, M.; Padhi, B.K. Determinants of COVID-19 Vaccine Acceptance in Saudi Arabia: A Web-Based National Survey. JMDH 2020, 13, 1657–1663. [Google Scholar] [CrossRef]
- Al-Qerem, W.A.; Jarab, A.S. COVID-19 Vaccination Acceptance and Its Associated Factors among a Middle Eastern Population. Front. Public Health 2021, 9, 632914. [Google Scholar] [CrossRef]
- Attwell, K.; Lake, J.; Sneddon, J.; Gerrans, P.; Blyth, C.; Lee, J. Converting the Maybes: Crucial for a Successful COVID-19 Vaccination Strategy. PLoS ONE 2021, 16, e0245907. [Google Scholar] [CrossRef] [PubMed]
- Detoc, M.; Bruel, S.; Frappe, P.; Tardy, B.; Botelho-Nevers, E.; Gagneux-Brunon, A. Intention to Participate in a COVID-19 Vaccine Clinical Trial and to Get Vaccinated against COVID-19 in France during the Pandemic. Vaccine 2020, 38, 7002–7006. [Google Scholar] [CrossRef] [PubMed]
- Ditekemena, J.D.; Nkamba, D.M.; Mutwadi, A.; Mavoko, H.M.; Siewe Fodjo, J.N.; Luhata, C.; Obimpeh, M.; Van Hees, S.; Nachega, J.B.; Colebunders, R. COVID-19 Vaccine Acceptance in the Democratic Republic of Congo: A Cross-Sectional Survey. Vaccines 2021, 9, 153. [Google Scholar] [CrossRef] [PubMed]
- Eguia, H.; Vinciarelli, F.; Bosque-Prous, M.; Kristensen, T.; Saigí-Rubió, F. Spain’s Hesitation at the Gates of a COVID-19 Vaccine. Vaccines 2021, 9, 170. [Google Scholar] [CrossRef]
- Gan, L.; Chen, Y.; Hu, P.; Wu, D.; Zhu, Y.; Tan, J.; Li, Y.; Zhang, D. Willingness to Receive SARS-CoV-2 Vaccination and Associated Factors among Chinese Adults: A Cross Sectional Survey. Int. J. Environ. Res. Public Health 2021, 18, 1993. [Google Scholar] [CrossRef]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Winardi, W.; Anwar, S.; Gan, A.K.; Setiawan, A.M.; Rajamoorthy, Y.; Sofyan, H.; Vo, T.Q.; et al. Willingness-to-Pay for a COVID-19 Vaccine and Its Associated Determinants in Indonesia. Hum. Vaccines Immunother. 2020, 16, 3074–3080. [Google Scholar] [CrossRef] [PubMed]
- Kourlaba, G.; Kourkouni, E.; Maistreli, S.; Tsopela, C.-G.; Molocha, N.-M.; Triantafyllou, C.; Koniordou, M.; Kopsidas, I.; Chorianopoulou, E.; Maroudi-Manta, S.; et al. Willingness of Greek General Population to Get a COVID-19 Vaccine. Glob. Health Res. Policy 2021, 6, 3. [Google Scholar] [CrossRef]
- Lin, Y.; Hu, Z.; Zhao, Q.; Alias, H.; Danaee, M.; Wong, L.P. Understanding COVID-19 Vaccine Demand and Hesitancy: A Nationwide Online Survey in China. PLoS Negl. Trop. Dis. 2020, 14, e0008961. [Google Scholar] [CrossRef]
- Mouchtouri, V.A.; Agathagelidou, E.; Kofonikolas, K.; Rousou, X.; Dadouli, K.; Pinaka, O.; Agathocleous, E.; Anagnostopoulou, L.; Chatziligou, C.; Christoforidou, E.P.; et al. Nationwide Survey in Greece about Knowledge, Risk Perceptions, and Preventive Behaviors for COVID-19 during the General Lockdown in April 2020. Int. J. Environ. Res. Public Health 2020, 17, 8854. [Google Scholar] [CrossRef]
- Muqattash, R.; Niankara, I.; Traoret, R.I. Survey Data for COVID-19 Vaccine Preference Analysis in the United Arab Emirates. Data Brief 2020, 33, 106446. [Google Scholar] [CrossRef] [PubMed]
- Sherman, S.M.; Smith, L.E.; Sim, J.; Amlôt, R.; Cutts, M.; Dasch, H.; Rubin, G.J.; Sevdalis, N. COVID-19 Vaccination Intention in the UK: Results from the COVID-19 Vaccination Acceptability Study (CoVAccS), a Nationally Representative Cross-Sectional Survey. Hum. Vaccin. Immunother. 2021, 17, 1612–1621. [Google Scholar] [CrossRef]
- Wang, J.; Lu, X.; Lai, X.; Lyu, Y.; Zhang, H.; Fenghuang, Y.; Jing, R.; Li, L.; Yu, W.; Fang, H. The Changing Acceptance of COVID-19 Vaccination in Different Epidemic Phases in China: A Longitudinal Study. Vaccines 2021, 9, 191. [Google Scholar] [CrossRef]
- Williams, L.; Flowers, P.; McLeod, J.; Young, D.; Rollins, L. The CATALYST Project Team The CATALYST Project Team Social Patterning and Stability of Intention to Accept a COVID-19 Vaccine in Scotland: Will Those Most at Risk Accept a Vaccine? Vaccines 2021, 9, 17. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Wong, E.L.Y.; Huang, J.; Cheung, A.W.L.; Law, K.; Chong, M.K.C.; Ng, R.W.Y.; Lai, C.K.C.; Boon, S.S.; Lau, J.T.F.; et al. Acceptance of the COVID-19 Vaccine Based on the Health Belief Model: A Population-Based Survey in Hong Kong. Vaccine 2021, 39, 1148–1156. [Google Scholar] [CrossRef]
- Yoda, T.; Katsuyama, H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines 2021, 9, 48. [Google Scholar] [CrossRef] [PubMed]
- Zeballos Rivas, D.R.; Lopez Jaldin, M.L.; Nina Canaviri, B.; Portugal Escalante, L.F.; Alanes Fernández, A.M.C.; Aguilar Ticona, J.P. Social Media Exposure, Risk Perception, Preventive Behaviors and Attitudes during the COVID-19 Epidemic in La Paz, Bolivia: A Cross Sectional Study. PLoS ONE 2021, 16, e0245859. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M. COVID-19 Vaccine Hesitancy Worldwide: A Concise Systematic Review of Vaccine Acceptance Rates. Vaccines 2021, 9, 160. [Google Scholar] [CrossRef] [PubMed]
- Cochrane Consumers and Communication Review Group. Ryan R Heterogeneity and Subgroup Analyses in Cochrane Consumers and Communication Group Reviews: Planning the Analysis at Protocol Stage. Available online: https://cccrg.cochrane.org/ (accessed on 20 September 2021).
- Flanagan, K.L.; Fink, A.L.; Plebanski, M.; Klein, S.L. Sex and Gender Differences in the Outcomes of Vaccination over the Life Course. Annu. Rev. Cell Dev. Biol. 2017, 33, 577–599. [Google Scholar] [CrossRef] [PubMed]
- Raja, A.S.; Niforatos, J.D.; Anaya, N.; Graterol, J.; Rodriguez, R.M. Vaccine Hesitancy and Reasons for Refusing the COVID-19 Vaccination among the U.S. Public: A Cross-Sectional Survey. medRxiv 2021. [Google Scholar] [CrossRef]
- Robertson, E.; Reeve, K.S.; Niedzwiedz, C.L.; Moore, J.; Blake, M.; Green, M.; Katikireddi, S.V.; Benzeval, M.J. Predictors of COVID-19 Vaccine Hesitancy in the UK Household Longitudinal Study. Brain Behav. Immun. 2021, 94, 41–50. [Google Scholar] [CrossRef]
- Khaled, S.M.; Petcu, C.; Bader, L.; Amro, I.; Al-Hamadi, A.M.H.A.; Al Assi, M.; Ali, A.A.M.; Le Trung, K.; Diop, A.; Bellaj, T.; et al. Prevalence and Potential Determinants of COVID-19 Vaccine Hesitancy and Resistance in Qatar: Results from a Nationally Representative Survey of Qatari Nationals and Migrants between December 2020 and January 2021. Vaccines (Basel) 2021, 9, 471. [Google Scholar] [CrossRef] [PubMed]
- Male, V. Are COVID-19 Vaccines Safe in Pregnancy? Nat. Rev. Immunol. 2021, 21, 200–201. [Google Scholar] [CrossRef]
- Kreps, S.; Dasgupta, N.; Brownstein, J.S.; Hswen, Y.; Kriner, D.L. Public Attitudes toward COVID-19 Vaccination: The Role of Vaccine Attributes, Incentives, and Misinformation. NPJ Vaccines 2021, 6, 73. [Google Scholar] [CrossRef]
- Paul, E.; Steptoe, A.; Fancourt, D. Attitudes towards Vaccines and Intention to Vaccinate against COVID-19: Implications for Public Health Communications. Lancet Reg. Health Eur. 2021, 1. [Google Scholar] [CrossRef]
- Turhan, Z.; Dilcen, H.Y.; Dolu, İ. The Mediating Role of Health Literacy on the Relationship between Health Care System Distrust and Vaccine Hesitancy during COVID-19 Pandemic. Curr. Psychol. 2021, 1–10. [Google Scholar] [CrossRef]
- Heidari, S.; Durrheim, D.N.; Faden, R.; Kochhar, S.; MacDonald, N.; Olayinka, F.; Goodman, T.S. Time for Action: Towards an Intersectional Gender Approach to COVID-19 Vaccine Development and Deployment That Leaves No One Behind. BMJ Glob. Health 2021, 6, e006854. [Google Scholar] [CrossRef] [PubMed]
- Bianconi, V.; Mannarino, M.R.; Bronzo, P.; Marini, E.; Pirro, M. Time-Related Changes in Sex Distribution of COVID-19 Incidence Proportion in Italy. Heliyon 2020, 6, e05304. [Google Scholar] [CrossRef] [PubMed]
- Elfil, M.; Negida, A. Sampling Methods in Clinical Research; an Educational Review. Emergency (Tehran) 2017, 5, e52. [Google Scholar]
- Bono, S.A.; Faria de Moura Villela, E.; Siau, C.S.; Chen, W.S.; Pengpid, S.; Hasan, M.T.; Sessou, P.; Ditekemena, J.D.; Amodan, B.O.; Hosseinipour, M.C.; et al. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines 2021, 9, 515. [Google Scholar] [CrossRef]
- Thomson, A.; Watson, M. Listen, Understand, Engage. Sci. Transl. Med. 2012, 4, 138ed6. [Google Scholar] [CrossRef] [Green Version]
| (“coronavirus”[MeSH Terms] OR “coronavirus”[All Fields] OR “coronaviruses”[All Fields] OR “COVID 19”[All Fields] OR “SARS-2”[All Fields] OR “severe acute respiratory syndrome coronavirus 2”[All Fields] OR “severe acute respiratory syndrome coronavirus 2”[Supplementary Concept] OR “ncov”[All Fields] OR “2019 ncov”[All Fields] OR “sars cov 2”[All Fields]) AND (“vaccines”[MeSH Terms] OR “vaccin”[All Fields] OR “vaccination”[MeSH Terms] OR “vaccination”[All Fields] OR “vaccinable”[All Fields] OR “vaccinal”[All Fields] OR “vaccinate”[All Fields] OR “vaccinated”[All Fields] OR “vaccinates”[All Fields] OR “vaccinating”[All Fields] OR “vaccinations”[All Fields] OR “vaccination’s”[All Fields] OR “vaccinator”[All Fields] OR “vaccinators”[All Fields] OR “vaccine s”[All Fields] OR “vaccined”[All Fields] OR “vaccines”[All Fields] OR “vaccine”[All Fields] OR “vaccins”[All Fields] OR “vaccin”[Supplementary Concept]) AND (“surveys and questionnaires”[MeSH Terms] OR “survey”[All Fields] OR “surveys”[All Fields] OR “survey’s”[All Fields] OR “surveyed”[All Fields] OR “surveying”[All Fields] OR (“surveys”[All Fields] AND “questionnaires”[All Fields]) OR “surveys and questionnaires”[All Fields] OR (“questionnair”[All Fields] OR “questionnaire’s”[All Fields] OR “surveys and questionnaires”[MeSH Terms] OR (“surveys”[All Fields] AND “questionnaires”[All Fields]) OR “surveys and questionnaires”[All Fields] OR “questionnaire”[All Fields] OR “questionnaires”[All Fields]) OR “poll”[All Fields]) |
| Questioned | Responses |
|---|---|
| Vaccination willingness | yes/yes, I will be vaccinated/yes if it’s free/strongly agree/agree/yes certainly/yes possibly/definitely/probably/definitely planning/probably planning/yes (only when the vaccine is provided for free)/yes (willing to pay for a vaccine)/very likely/somewhat likely/probably yes/completely agree/somewhat agree/definitely yes/quite a bit/extremely likely/8–10 (very likely)/I probably would want to receive it/I definitely would want to receive it/high 6–7 |
| Vaccination refusal or hesitancy | probably not/certainly not/accepting of a COVID-19 vaccine |
| Author | Country | Survey Date | Main Survey Question | Answer Options | Vaccination Willing (n) | Sample Size (n) |
|---|---|---|---|---|---|---|
| Akarsu et al. (2020) [21] | Turkey | 10 June 2020–20 July 2020 | If a vaccine for COVID-19 is developed, would you be vaccinated against COVID-19? | yes, I will be vaccinated/yes, if it’s free/no, I don’t/undecided | 421 | 759 |
| Alley et al. (2021) [23] | Australia | 9 April 2020–16 August 2020 | If a new vaccine for COVID-19 was released that was proven to be safe and effective, I would get vaccinated immediately. | strongly agree/agree/neither agree nor disagree/disagree/strongly disagree | 1972 | 2328 |
| Al-Mohaithef and Padhi (2020) [40] | Saudi Arabia | Not reported | If a vaccine against coronavirus is available, I will take it. | yes/no/not sure | 642 | 992 |
| Al-Qerem and Jarab (2021) [41] | Jordan | 1 October 2020–31 October 2020 | If a vaccine is available for COVID-19, are you willing to take it? | yes/no/not sure | 421 | 1144 |
| Attwel et al. (2021) [42] | Australia | 18 May 2020–29 May 2020 | If a COVID-19 vaccine were available today, would you get it? | yes/maybe/no | 856 * | 1316 |
| Biasio et al. (2020) [24] | Italy | 5 June 2020–13 June 2020 | Will you get vaccinated, if possible? | yes/no | 816 | 885 |
| Callaghan et al. (2021) [25] | USA | 28 May 2020–08 June 2020 | If a COVID-19 vaccine is developed, would you pursue getting vaccinated for the coronavirus? | yes/no | 3464 */** | 5009 |
| Chen et al. (2021) [26] | China | 1 May 2020–30 June 2020 | Willing to receive a COVID-19 vaccine. | yes/no/unsure | 2676 | 3195 |
| Detoc et al. (2020) [43] | France | 26 March 2020–20 April 2020 | If a vaccine against the new coronavirus was available for next season, would you get vaccinated? | yes, certainly/yes, possibly/I don’t know/no, possibly/definitely no | 2530 | 3259 |
| Dinga et al. (2021) [27] | Cameroon | 1 May 2020–31 August 2020 | Would you agree to receive a COVID-19 vaccine? | yes/no/I will need more information/I don’t know | 386 | 2512 |
| Ditekemena et al. (2021) [44] | Republic of Congo | 24 August 2020–8 September 2020 | Would you consent to receive a COVID-19 vaccine if it becomes available in our country? | yes/no | 2310 | 4131 |
| Eguia et al. (2021) [45] | Spain | 10 September 2020–23 November 2020 | Intention to get vaccinated. | yes/no | 567 | 731 |
| Feleszko et al. (2021) [28] | Poland | 2 June 2020–9 June 2020 | If a vaccine against coronavirus disease 2019 (COVID-19) is available and safe, do you plan to vaccinate? | yes/no/I do not know or it is difficult to answer | 394 | 1066 |
| Fisher et al. (2020) [34] | USA | 16 April 2020–20 April 2020 | When a vaccine for the coronavirus becomes available, will you get vaccinated? | yes/no/not sure | 571 | 991 |
| Freeman et al. (2020) [32] | UK | 24 September 2020–17 October 2020 | Would you take a COVID-19 vaccine (approved for use in the UK) if offered? | definitely/probably/I may or I may not/probably not/definitely not/don’t know | 3776 | 5114 |
| Gan et al. (2021) [46] | China | 23 October 2020–10 November 2020 | Would you be vaccinated against COVID-19? | yes/no/unsure | 609 | 1009 |
| Guidry et al. (2021) [35] | USA | 1 July 2020–31 July 2020 | I intend to get the COVID-19 vaccine when it becomes available. | definitely planning/probably planning/neutral/probably not planning/definitely not planning | 472 * | 788 |
| Harapan et al. (2020) [47] | Indonesia | 25 March 2020–6 April 2020 | Would you accept a COVID-19 vaccine? | no/yes (only when the vaccine is provided for free)/yes (willing to pay for a vaccine) | 1268 | 1359 |
| Hogan et al. (2020) [31] | USA | 1 April 2020–30 April 2020 | If a vaccine becomes available for COVID-19, would you get it? | yes/no | 84 * | 113 |
| Khubchandani et al. (2021) [29] | USA | 1 June 2020–30 June 2020 | If a vaccine was available that would prevent coronavirus infection, how likely is it that you would get the vaccine/shot? | very likely/somewhat likely/not likely/definitely not | 1467 | 1878 |
| Kourlaba et al. (2021) [48] | Greece | 28 April 2020–3 May 2020 | Willingness to be vaccinated against Coronavirus if a vaccine was to become available. | yes/no/do not know | 579 | 1004 |
| La Vecchia et al. (2020) [37] | Italy | 16 September 2020–28 September 2020 | Attitude towards a potential COVID-19 vaccine. | yes/probably yes/probably no/no | 567 * | 1055 |
| Latkin et al. (2021) [36] | USA | 14 May 2020–18 May 2020 | If a vaccine against the coronavirus becomes available, do you plan to get vaccinated, or not? | yes, I will get a coronavirus vaccine/no, I will not get a coronavirus vaccine/not sure | 559 | 1043 |
| Lazarus et al. (2020) [18] | Brazil | 1 June 2020–30 June 2020 • | Would you take a proven, safe and effective COVID-19 vaccine? • | completely agree/somewhat agree/neutral or no opinion/somewhat disagree/completely disagree • | 612 | 717 |
| Canada | 486 | 707 | ||||
| China | 631 | 712 | ||||
| Ecuador | 533 | 741 | ||||
| France | 394 | 669 | ||||
| Germany | 494 | 722 | ||||
| India | 553 | 742 | ||||
| Italy | 521 | 736 | ||||
| Mexico | 533 | 699 | ||||
| Nigeria | 437 | 670 | ||||
| Poland | 375 | 666 | ||||
| Russia | 373 | 680 | ||||
| Singapore | 445 | 655 | ||||
| South Africa | 505 | 619 | ||||
| South Korea | 600 | 752 | ||||
| Spain | 556 | 748 | ||||
| Sweden | 424 | 650 | ||||
| UK | 549 | 768 | ||||
| USA | 583 | 773 | ||||
| Lin, Hu et al. (2020) [49] | China | 1 May 2020–19 May 2020 | Intention to take the COVID-19 vaccine. | definitely yes/probably yes/probably no/definitely no | 2950 | 3541 |
| Mouchtouri et al. (2020) [50] | Greece | 15 April 2020–02 May 2020 | Should a vaccine be available for COVID-19, I will receive it. | definitely yes/yes/maybe/no | 893 | 1811 |
| Muqattash et al. (2020) [51] | United Arab Emirates | 4 July 2020–04 August 2020 | How willing are you to get the COVID-19 vaccine, once discovered? | not at all/a little/a moderate amount/quite a bit | 601 | 1109 |
| Murphy et al. (2021) [20] | Ireland | Not reported | Prevalence of vaccine hesitancy and resistance in Ireland. | accepting of a COVID-19 vaccine/hesitant about such a vaccine/resistant towards a vaccine | 676 * | 1041 |
| UK | 1397 * | 2025 | ||||
| Prati (2020) [39] | Italy | 1 April 2020–30 April 2020 | Assume that your local health authority makes a vaccine against SARS-CoV-2 freely available. Do you intend to get the vaccine? | yes/no/do not know | 473 | 568 |
| Ruiz and Bell (2021) [30] | USA | 15 June 2020–16 June 2020 | All things considered, how likely are you to get a coronavirus vaccine when one becomes available? | extremely likely/somewhat likely/unsure/somewhat unlikely/extreme unlikely | 500 * | 804 |
| Sallam et al. (2021) [19] | Jordan | 14 December 2020–18 December 2020 | Will you get the coronavirus vaccine when available? | yes/no | 618 | 2173 |
| Kuwait | 182 | 771 | ||||
| Arabic speaking countries # | 131 | 316 | ||||
| Saudi Arabia | 49 | 154 | ||||
| Sherman et al. (2020) [52] | UK | 14 July 2020–17 July 2020 | When a coronavirus vaccination becomes available to you, how likely is it you will have one? | 0–2 = very unlikely 3–7 = uncertain 8–10 = very likely | 960 * | 1500 |
| Vai et al. (2020) [38] | Italy | 27 February 2020–8 March 2020 | Declare if you would have vaccinated for SARS-CoV-2. | yes/no | 1566 | 2223 |
| Wang, Lu et al. (2021) [53] | China | 15 November 2020–15 December 2020 | Accept vaccination if the COVID-19 vaccine is successfully developed and approved for listing in the future. | yes/no | 1974 | 2013 |
| Wang, Wong et al. (2021) [21] | Hong Kong | 17 February 2020–27 February 2020 | If a COVID-19 vaccine is available now, whether or not will you choose to accept it. | yes (accept)/no (refuse)/undecided | 463 * | 1047 |
| 24 August 2020–7 September 2020 | 348 * | 1000 | ||||
| Ward et al. (2020) [33] | France | 1 April 2020–30 April 2020 | Would you refuse a vaccine against the COVID-19 when available? | certainly/probably/probably not/certainly not | 3814 | 5018 |
| Williams et al. (2021) [54] | Scotland | 1 August 2020–31 August 2020 | If a vaccine for coronavirus (COVID-19) becomes available, would you want to receive it? | I definitely would not want to receive it/I probably would not want to receive it/unsure/I probably would want to receive it/I definitely would want to receive it | 1425 | 3436 |
| Wong et al. (2021) [55] | Hong Kong | 27 July 2020–27 August 2020 | If the Government will provide a free-of-charge COVID19 vaccine within the next 12 months, will you receive it? | yes/no/not sure | 507 | 1200 |
| Yoda and Katsuyama (2021) [56] | Japan | 1 September 2020–30 September 2020 | Would you be willing to be vaccinated when the COVID-19 vaccine is developed? | yes/unsure/no | 723 | 1100 |
| Zeballos Rivas et al. (2021) [57] | Bolivia | 29 April 2020–9 May 2020 | Would you use a COVID-19 vaccine if it were available? | null or low 1–3/moderate 4–5/high 6–7 | 481 | 886 |
| Alley [23] | Al-Mohaithef [40] | Al-Qerem [41] | Attwell [42] | Callaghan [25] - | Chen [26] | Detoc [43] | Ditekemena [44] | Fisher [34] | Freeman [32] | Gan [46] | Guidry [35] | Khubchandani [29] | Kourlaba [48] | Latkin [36] | Lazarus [18] - | Lin [49] | Murphy [20] | Prati [39] | Ruiz [30] | Sallam [19] | Sherman [52] | Vai [38] | Wang, Wong [21] | Wang, Lu [53] | Ward [33] | Williams [54] | Wong [55] | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sociodemographics | Living location | ● | ꙱ * | ◊ | ◊ * | ◊ | ▫ | ● * | ● | ● | ● | ● | ●/■ * | ▫ | ● * | ■ * | ◊ * | ◊ | ● | ● * | |||||||||
| Ethnicity | ▫ | ■ | ▫ | ▫ | ■ | ● | ▫ | ▫ | ● | ● | ● | ■ | |||||||||||||||||
| Gender/sex | ● | ● | ▫ | ▫ | ▫ | ■ | ■ | ● | ▫ | ▫ | ● | ● | ▫ | ● | ▫ | ■ | ● | ▫ | ● | ■ | ■ | ● | ● | ■ | ■ | ▫ | ● | ● | |
| Age | ● | ■ | ● | ꙱ | ● | ● | ■ | ◊ | ▫ | ▫ | ■ | ● | ● | ● | ▫ | ■ | ● | ▫ | ▫ | ● | ● | ■ | ▫ | ■ | ◊ | ▫ | ● | ● | |
| Political preferences | ▫ | ▫ | ● | ▫ | ▫ | ▫ | ■ | ▫ | |||||||||||||||||||||
| Religion | ▫ | ● | ▫ | ● | ● | ◊ | ● | ||||||||||||||||||||||
| SES indicators | Education | ■ | ꙱ | ▫ | ꙱ | ● | ■ | ● | ▫ | ▫ | ■ | ■ | ▫ | ● | ● | ■ | ● | ■ | ● | ▫ | ● | ◊ | ● | ■ | ● | ||||
| Income/insurance | ● | ◊ | ● | ▫ | ■ | ■ | ● | ▫ | ● | ■ | ▫ | ▫ | ■ | ● | ▫ | ꙱ | ■ | ◊ | ◊ | ◊ | ■ | ▫ | ■ | ● | |||||
| Occupation/ Employment status | ꙱ | ● | ◊ | ◊ | ▫ | ꙱ | ▫ | ■ | ● | ■ | ● | ■ | ● | ● | |||||||||||||||
| Health-related occupation | ● | ◊ | ■ | ■ | ◊ | ◊ | ● | ||||||||||||||||||||||
| Family composition | Children in household/household size | ● | ꙱ | ● | ● | ▫ | ● | ◊ | ◊ | ||||||||||||||||||||
| Marital status | ■ | ▫ | ◊ | ◊ | ꙱ | ● | ● | ꙱ | ● | ■ | ■ | ||||||||||||||||||
| Health status | Risk group or conditions | ꙱ | ● | ● | ● | ◊ | ● | ● | ■ | ■ | ▫ | ■ | ■ | ● | ● | ● | ■ | ■ | |||||||||||
| Vaccine history | ◊ | ▫ | ◊ | ▫ | ■ | ● | ■ | ◊ | ■ | ■ | ■ | ||||||||||||||||||
| Experiences with COVID-19 | Suspected or laboratory COVID-19 diagnosis (self) | ▫ | ■ | ◊ | ◊ | ● | ■ | ● | ◊ | ◊ | ● | ● | ● | ||||||||||||||||
| Suspected or laboratory COVID-19 diagnosis (others) | ◊ | ◊ | ◊ | ◊ | ● | ||||||||||||||||||||||||
| Perceived risk for self or others in direct network | Concerns about (risk of) COVID-19 | ■ | ● | ▫ | ● | ■ | ◊ | ■ | ▫ | ● | ■ | ▫ | ■ | ● | ▫ | ■ | ▫ | ● | |||||||||||
| Perceived disease severity | ▫ | ▫ | ● | ▫ | ▫ | ● | ● | ● | ■ | ||||||||||||||||||||
| (Concerns about) vulnerable household/network | ◊ | ▫ | ● | ● | ● | ||||||||||||||||||||||||
| Severity of disease in region | ■ | ■ | ■ | ||||||||||||||||||||||||||
| Attitudes, beliefs and perceptions about vaccination | Benefits of vaccines | ▫ | ■ | ■ | ● | ■ | ■ | ||||||||||||||||||||||
| Harm and/or barriers of vaccines | ■ | ■ | ■ | ■ | ■ | ■ | |||||||||||||||||||||||
| Other beliefs and attitudes about vaccines | ▫ | ■ | ■ | ■ | ■ | ■ | ■ | ||||||||||||||||||||||
| Attitudes, beliefs and perceptions about COVID-19 | COVID-19-related knowledge or behavior | ● | ◊ | ◊ | ● | ■ | ● | ■ | ◊ | ◊ | |||||||||||||||||||
| Attitudes and beliefs about COVID-19 | ◊ | ◊ | ■ | ■ | ■ | ■ | ▫ | ||||||||||||||||||||||
| Impact of pandemic on life, work, and/or income | ◊ | ◊ | ● | ▫ | ● | ■ | |||||||||||||||||||||||
| Expressions of mistrust about COVID-19 and/or vaccination | ◊ | ▫ | ■ | ◊ | ■ | ◊ | ● | ■ | ■ | ||||||||||||||||||||
| Trust in health system/government | ■ | ◊ | ■ | ■ | ◊ | ▫ | ◊ | ● | ■ | ||||||||||||||||||||
| Trust in science/manufacturer | ◊ | ▫ | ◊ | ◊ | ● | ■ | |||||||||||||||||||||||
| Informants | Media use | ▫ | ◊ | ◊ | ■ | ● | ◊ | ■ | ◊ | ◊ | |||||||||||||||||||
| Cues to action (e.g., from others in network, doctors) | ◊ | ■ | ■ | ◊ | ■ | ■ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nehal, K.R.; Steendam, L.M.; Campos Ponce, M.; van der Hoeven, M.; Smit, G.S.A. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines 2021, 9, 1071. https://doi.org/10.3390/vaccines9101071
Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines. 2021; 9(10):1071. https://doi.org/10.3390/vaccines9101071
Chicago/Turabian StyleNehal, Kimberly R., Lieke M. Steendam, Maiza Campos Ponce, Marinka van der Hoeven, and G. Suzanne A. Smit. 2021. "Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis" Vaccines 9, no. 10: 1071. https://doi.org/10.3390/vaccines9101071
APA StyleNehal, K. R., Steendam, L. M., Campos Ponce, M., van der Hoeven, M., & Smit, G. S. A. (2021). Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines, 9(10), 1071. https://doi.org/10.3390/vaccines9101071






