Impact of Pneumococcal Vaccination in the Nasopharyngeal Carriage of Streptococcus pneumoniae in Healthy Children of the Murcia Region in Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Microbiological Processing of the Samples
Antimicrobial Susceptibility Testing
2.3. Statistical Analysis
3. Results
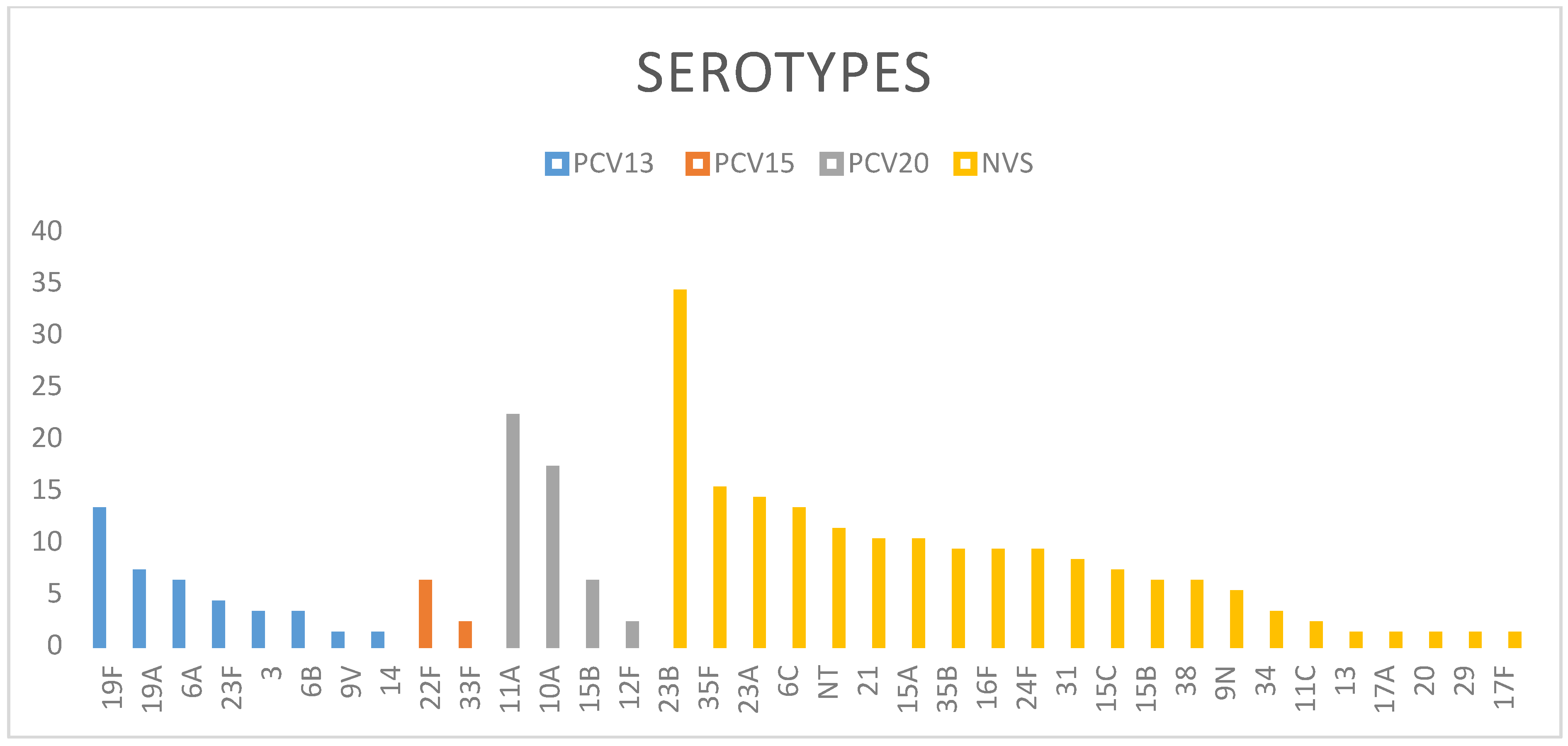
3.1. Pneumococcal Serotypes in Asymptomatic Carriers
3.2. Relationship between Antibiotic Resistance and Serotypes
4. Discussion
Strengths and Weaknesses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bogaert, D.; de Groot, R.; Hermans, P.W.M. Streptococcus pneumoniae colonisation: The key to pneumococcal disease. Lancet Infect. Dis. 2004, 4, 144–154. [Google Scholar] [CrossRef]
- Kaur, R.; Casey, J.R.; Pichichero, M.E. Emerging Streptococcus pneumoniae Strains Colonizing the Nasopharynx in Children After 13-valent Pneumococcal Conjugate Vaccination in Comparison to the 7-valent Era, 2006–2015. Pediatr. Infect. Dis. J. 2016, 35, 901–906. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lynch, J.P., III; Zhanel, G.G. Streptococcus pneumoniae: Epidemiology and risk factors, evolution of antimicrobial resistance, and impact of vaccines. Curr. Opin. Pulm. Med. 2010, 16, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Løvlie, A.; Vestrheim, D.F.; Aaberge, I.S.; Steens, A. Changes in pneumococcal carriage prevalence and factors associated with carriage in Norwegian children, four years after introduction of PCV13. BMC Infect. Dis. 2020, 20, 29. [Google Scholar] [CrossRef] [PubMed]
- Danino, D.; Givon-Lavi, N.; Ben-Shimol, S.; Greenberg, D.; Dagan, R. Understanding the Evolution of Antibiotic-nonsusceptible Pneumococcal Nasopharyngeal Colonization Following Pneumococcal Conjugate Vaccine Implementation in Young Children. Clin. Infect. Dis. 2019, 69, 648–656. [Google Scholar] [CrossRef] [PubMed]
- Ouldali, N.; Varon, E.; Levy, C.; Angoulvant, F.; Georges, S.; Ploy, M.-C.; Kempf, M.; Cremniter, J.; Cohen, R.; Bruhl, D.L.; et al. Invasive pneumococcal disease incidence in children and adults in France during the pneumococcal conjugate vaccine era: An interrupted time-series analysis of data from a 17-year national prospective surveillance study. Lancet Infect. Dis. 2020, 137–147. [Google Scholar] [CrossRef]
- de Miguel, S.; Domenech, M.; González-Camacho, F.; Sempere, J.; Vicioso, D.; Sanz, J.C.; Comas, L.G.; Ardanuy, C.; Fenoll, A.; Yuste, J. Nationwide Trends of Invasive Pneumococcal Disease in Spain from 2009 Through 2019 in Children and Adults During the Pneumococcal Conjugate Vaccine Era. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef]
- Richter, L.; Schmid, D.; Kanitz, E.E.; Zwazl, I.; Pöllabauer, E.; Jasinska, J.; Burgmann, H.; Kundi, M.; Wiedermann, U. Invasive pneumococcal diseases in children and adults before and after introduction of the 10-valent pneumococcal conjugate vaccine into the Austrian national immunization program. PLoS ONE 2019, 14, e0210081. [Google Scholar]
- Savulescu, C.; Krizova, P.; Lepoutre, A.; Mereckiene, J.; Vestrheim, D.F.; Ciruela, P.; Ordobas, M.; Guevara, M.; McDonald, E.; Morfeldt, E.; et al. Effect of high-valency pneumococcal conjugate vaccines on invasive pneumococcal disease in children in SpIDnet countries: An observational multicentre study. Lancet Respir. Med. 2017, 5, 648–656. [Google Scholar] [CrossRef] [Green Version]
- Instituto Nacional de Estadística. Available online: https://www.ine.es/jaxi/Datos.htm?path=/t20/e245/p08/l0/&file=02002.px#!tabs-tabla (accessed on 5 November 2020).
- The European Committee on Antimicrobial Susceptibility Testing. Breakpoint Tables for Interpretation of MICs and Zone Diameters. Available online: http://www.eucast.org (accessed on 5 November 2020).
- Performance Standards Antimicrobial Susceptibility Testing, 30th ed.; CLSI supplement M100; Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2020.
- Fenoll, A.; Granizo, J.-J.; Gimenez, M.-J.; Yuste, J.; Aguilar, L. Secular trends (1990–2013) in serotypes and associated non-susceptibility of S. pneumoniae isolates causing invasive disease in the pre-/post-era of pneumococcal conjugate vaccines in Spanish regions without universal paediatric pneumococcal vaccination. Vaccine 2015, 33, 5691–5699. [Google Scholar] [CrossRef]
- Elberse, K.; Van De Pol, I.; Witteveen, S.; van der Heide, H.G.J.; Schot, C.S.; Van Dijk, A.; Van Der Ende, A.; Schouls, L.M. Population Structure of Invasive Streptococcus pneumoniae in the Netherlands in the Pre-Vaccination Era Assessed by MLVA and Capsular Sequence Typing. PLoS ONE 2011, 6, e20390. [Google Scholar] [CrossRef] [PubMed]
- Harboe, Z.B.; Slotved, H.-C.; Konradsen, H.B.; Kaltoft, M.S. A Pneumococcal Carriage Study in Danish Pre-school Children before the introduction of Pneumococcal Conjugate Vaccination. Open Microbiol. J. 2012, 6, 40–44. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, G.M.; Kleinman, K.; Pelton, S.I.; Hanage, W.; Huang, S.S.; Lakoma, M.; Dutta-Linn, M.; Croucher, N.J.; Stevenson, A.; Finkelstein, J.A. Impact of 13-Valent Pneumococcal Conjugate Vaccination on Streptococcus pneumoniae Carriage in Young Children in Massachusetts. J. Pediatr. Infect. Dis. Soc. 2014, 3, 23–32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Southern, J.; Andrews, N.; Sandu, P.; Sheppard, C.; Waight, P.A.; Fry, N.K.; Van Hoek, A.J.; Miller, E. Pneumococcal carriage in children and their household contacts six years after introduction of the 13-valent pneumococcal conjugate vaccine in England. PLoS ONE 2018, 13, e0195799. [Google Scholar] [CrossRef] [PubMed]
- López, B.; Cima, M.D.; Vazquez, F.; Fenoll, A.; Gutiérrez, J.; Fidalgo, C.; Caicoya, M.; Méndez, F.J. Epidemiological study of Streptococcus pneumoniae carriage in healthy primary-school children. Eur. J. Clin. Microbiol. Infect. Dis. 1999, 18, 771–776. [Google Scholar] [CrossRef] [PubMed]
- Obando, I.; Sánchez-Tatay, D.; Molinos-Quintana, A.; Delgado-Pecellina, I.; Porras, A.; Morillo-Gutiérrez, B.; Fenolld, A.; Lirola, M.J. Epidemiología de la colonización nasofaríngea por Streptococcus pneumoniae en niños menores de 6 años de la ciudad de Sevilla. Enferm Infecc Microbiol Clin. 2011, 29, 581–586. [Google Scholar] [CrossRef]
- García Vera, C.; Ruiz Andrés, M.A.; Arana Navarro, T.; Moneo Hernández, I.; Castillo Laita, J.A.; Macipe Costa, R.M.; Revillo, M.J. Serotipos de neumococo en nasofaringe de niños preescolares sanos tras la vacunación antineumocócica conjugada heptavalente. Med. Clín. 2011, 137, 1–7. [Google Scholar]
- Kaur, R.; Pham, M.; Yu, K.O.A.; Pichichero, M.E. Rising Pneumococcal Antibiotic Resistance in the Post–13-Valent Pneumococcal Conjugate Vaccine Era in Pediatric Isolates from a Primary Care Setting. Clin. Infect. Dis. 2020, 157. [Google Scholar] [CrossRef]
- Lee, J.K.; Yun, K.W.; Choi, E.H.; Kim, S.J.; Lee, S.Y.; Lee, H.J. Changes in the Serotype Distribution among Antibiotic Resistant Carriage Streptococcus pneumoniae isolates in Children after the Introduction of the Extended-Valency Pneumococcal Conjugate Vaccine. J. Korean Med Sci. 2017, 32, 1431–1439. [Google Scholar] [CrossRef]
- Ricketson, L.J.; Wood, M.L.; Vanderkooi, O.G.; Macdonald, J.; Martin, I.E.; Demczuk, W.; Kellner, J.D. Trends in Asymptomatic Nasopharyngeal Colonization with Streptococcus pneumoniae After Introduction of the 13-valent Pneumococcal Conjugate Vaccine in Calgary, Canada. Pediatr. Infect. Dis. J. 2014, 33, 724–730. [Google Scholar] [CrossRef]
- Zhou, J.Y.; Isaacson-Schmid, M.; Utterson, E.C.; Todd, E.M.; McFarland, M.; Sivapalan, J.; Niehoff, J.M.; Burnham, C.-A.D.; Morley, S.C. Prevalence of nasopharyngeal pneumococcal colonization in children and antimicrobial susceptibility profiles of carriage isolates. Int. J. Infect. Dis. 2015, 39, 50–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dunais, B.; Bruno, P.; Touboul, P.; Degand, N.; Sakarovitch, C.; Fontas, E.; Haas, H.; Girard-Pipau, F.; Ruimy, R.; Pradier, C. Impact of the 13-valent Pneumococcal Conjugate Vaccine on Nasopharyngeal Carriage of Streptococcus pneumoniae Among Children Attending Group Daycare in Southeastern France. Pediatr. Infect. Dis. J. 2015, 34, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Sigurdsson, S.; Erlendsdóttir, H.; Quirk, S.J.; Kristjánsson, J.; Hauksson, K.; Andrésdóttir, B.D.I.; Jónsson, A.J.; Halldórsson, K.H.; Sæmundsson, Á.; Ólason, Ó.H.; et al. Pneumococcal vaccination: Direct and herd effect on carriage of vaccine types and antibiotic resistance in Icelandic children. Vaccine 2017, 35, 5242–5248. [Google Scholar] [CrossRef] [PubMed]
- Wouters, I.; Van Heirstraeten, L.; Desmet, S.; Blaizot, S.; Verhaegen, J.; Goossens, H.; Van Damme, P.; Malhotra-Kumar, S.; Theeten, H.; NPcarriage Study Group. Nasopharyngeal s. pneumoniae carriage and density in Belgian infants after 9 years of pneumococcal conjugate vaccine programme. Vaccine 2018, 36, 15–22. [Google Scholar] [CrossRef]
- Abu Seir, R.; Azmi, K.; Hamdan, A.; Namouz, H.; Jaar, F.; Jaber, H.; Rubin, C.; Doron, D.; Rahav, G.; Abdeen, Z.; et al. Comparison of early effects of pneumococcal conjugate vaccines: PCV7, PCV10 and PCV13 on Streptococcus pneumoniae nasopharyngeal carriage in a population based study; The Palestinian-Israeli Collaborative Research (PICR). PLoS ONE 2018, 13, e0206927. [Google Scholar] [CrossRef] [Green Version]
- Dagan, R.; Juergens, C.; Trammel, J.; Patterson, S.; Greenberg, D.; Givon-Lavi, N.; Porat, N.; Gruber, W.C.; Scott, D.A. PCV13-vaccinated children still carrying PCV13 additional serotypes show similar carriage density to a control group of PCV7-vaccinated children. Vaccine 2017, 35, 945–950. [Google Scholar] [CrossRef]
- Yildirim, I.; Little, B.; Finkelstein, J.; Lee, G.; Hanage, W.P.; Shea, K.; Pelton, S. Surveillance of pneumococcal colonization and invasive pneumococcal disease reveals shift in prevalent carriage serotypes in Massachusetts’ children to relatively low invasiveness. Vaccine 2017, 35, 4002–4009. [Google Scholar] [CrossRef]
- Ladhani, S.N.; Collins, S.; Djennad, A.; Sheppard, C.L.; Borrow, R.; Fry, N.K.; Andrews, N.J.; Miller, E.; Ramsay, M.E. Rapid increase in non-vaccine serotypes causing invasive pneumococcal disease in England and Wales, 2000–2017: A prospective national observational cohort study. Lancet Infect. Dis. 2018, 18, 441–451. [Google Scholar] [CrossRef] [Green Version]
- Koliou, M.; Andreou, K.; Lamnisos, D.; Lavranos, G.; Iakovides, P.; Economou, C.; Soteriades, E.S. Risk factors for carriage of Streptococcus pneumoniae in children. BMC Pediatr. 2018, 18, 144. [Google Scholar] [CrossRef] [Green Version]
- Reinert, R.R.; Reiner, S.; van der Linden, M.; Cil, M.Y.; Al-Lahham, A.; Appelbaum, P. Antimicrobial Susceptibility of Streptococcus pneumoniae in Eight European Countries from 2001 to 2003. Antimicrob. Agents Chemother. 2005, 49, 2903–2913. [Google Scholar] [CrossRef] [Green Version]
- Htar, M.T.T.; Biggelaar, A.H.V.D.; Sings, H.; Ferreira, G.; Moffatt, M.; Hall-Murray, C.; Verstraeten, T.; Gessner, B.D.; Schmitt, H.-J.; Jodar, L. The impact of routine childhood immunization with higher-valent pneumococcal conjugate vaccines on antimicrobial-resistant pneumococcal diseases and carriage: A systematic literature review. Expert Rev. Vaccines 2019, 18, 1069–1089. [Google Scholar] [CrossRef] [PubMed]
- Sexual Transmission of Dengue in Spain; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2019.
- Hauser, C.; Kronenberg, A.; Allemann, A.; Mühlemann, K.; Hilty, M. Serotype/serogroup-specific antibiotic non-susceptibility of invasive and non-invasive Streptococcus pneumoniae, Switzerland, 2004 to 2014. Eurosurveill 2016, 21, 30239. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaviria-Agudelo, C.L.; Jordan-Villegas, A.; Garcia, C.; McCracken, G.H., Jr. The Effect of 13-Valent Pneumococcal Conjugate Vaccine on the Serotype Distribution and Antibiotic Resistance Profiles in Children With Invasive Pneumococcal Disease. J. Pediatr. Infect. Dis. Soc. 2017, 6, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Mendes, R.E.; Costello, A.J.; Jacobs, M.R.; Biek, D.; Critchley, I.A.; Jones, R.N. Serotype distribution and antimicrobial susceptibility of USA Streptococcus pneumoniae isolates collected prior to and post introduction of 13-valent pneumococcal conjugate vaccine. Diagn. Microbiol. Infect. Dis. 2014, 80, 19–25. [Google Scholar] [CrossRef]
- Hjálmarsdóttir, M.Á.; Haraldsson, G.; Quirk, S.J.; Haraldsson, Á.; Erlendsdóttir, H.; Kristinsson, K.G. Reduction of antimicrobial resistant pneumococci seven years after introduction of pneumococcal vaccine in Iceland. PLoS ONE 2020, 15, e0230332. [Google Scholar] [CrossRef]
- Hadjipanayis, A.; Efstathiou, E.; Alexandrou, M.; Panayiotou, L.; Zachariadou, C.; Petrou, P.; Papaevangelou, V. Nasopharyngeal Pneumococcal Carriage among Healthy Children in Cyprus Post Widespread Simultaneous Implementation of PCV10 and PCV13 Vaccines. PLoS ONE 2016, 11, e0163269. [Google Scholar] [CrossRef]
- Gebre, T.; Tadesse, M.; Aragaw, D.; Feye, D.; Beyene, H.B.; Seyoum, D.; Mekonnen, M. Nasopharyngeal Carriage and Antimicrobial Susceptibility Patterns of Streptococcus pneumoniae among Children under Five in Southwest Ethiopia. Children 2017, 4, 27. [Google Scholar] [CrossRef] [Green Version]
- Mayansky, N.A.; Kulichenko, T.; Alyabieva, N.; Brzhozovskaya, E.; Ponomarenko, O.; Savinova, T.; Lazareva, A. Changing serotype distribution and resistance patterns among pediatric nasopharyngeal pneumococci collected in Moscow, 2010–2017. Diagn. Microbiol. Infect. Dis. 2019, 94, 385–390. [Google Scholar] [CrossRef]
- Sánchez-Tatay, D.; Arroyo, L.; Tarragό, D.; Lirola, M.; Porras, A.; Fenoll, A.; Hausdorff, W.; Brueggemann, A.B.; Obando, I. Antibiotic susceptibility and molecular epidemiology of nasopharyngeal pneumococci from Spanish children. Clin. Microbiol. Infect. 2008, 14, 797–801. [Google Scholar] [CrossRef] [Green Version]
- Antimicrobial Consumption in the EU/EEA Annual Epidemiological Report for 2018; European Centre for Disease Prevention and Control (ECDC): Stockholm, Sweden, 2019.
- Liñares, J.; Ardanuy, C.; Pallares, R.; Fenoll, A. Changes in antimicrobial resistance, serotypes and genotypes in Streptococcus pneumoniae over a 30-year period. Clin. Microbiol. Infect. 2010, 16, 402–410. [Google Scholar] [CrossRef] [Green Version]
| Characteristic/Variables | Frequency N (%) | ||
|---|---|---|---|
| 2014 | 2015 | Total | |
| No. of children | 812 (445) | 1009 (55.4) | 1821 |
| Age | |||
| 1 year | 401 (49.4) | 505 (50) | 906 (49.7) |
| 4 years | 411 (50.6) | 504 (50) | 915 (50.3) |
| Gender | |||
| Male | 350 (43.1) | 543 (53.8) | 893 (49) |
| Female | 462 (56.9) | 466 (46.2) | 928 (51) |
| Nasopharyngeal carriage | 138 (17.1) | 221 (21.9) | 359 (19.8) |
| Siblings ≥ 2 | 122 (15) | 131 (13) | 253 (13.9) |
| School attendance | 484 (59.6) | 599 (59.4) | 1079 (59.2) |
| Day Care attendance 1 year | 73 (9) | 95 (9.4) | 168 (9.2) |
| Antibiotics during last month | 55 | 114 | 169 (10.4) |
| Aged 1 year | 26 | 56 | |
| Aged 4 years | 29 | 58 | |
| Breastfeeding ≥6 months | 324 (39.9) | 333 (33) | 657 (36) |
| Smoke exposition | 323 (39.7) | 393 (38.9) | 716 (39.3) |
| PCV13-Vaccinated ≥2 doses | 585 (72) | 650 (64.4) | 1235 (67.8) |
| Colonized | Not Colonized | p | Multivariate OR (CI95%) | |
|---|---|---|---|---|
| Age (%): | ||||
| 1 years | 18.9 | 81.1 | ||
| 4 years | 21 | 79 | 0.28 | 0.73 (0.52; 1.03) |
| Sex: | ||||
| Male (%) | 19.7 | 80.3 | ||
| Female (%) | 20.2 | 79.8 | 0.78 | 0.98 (0.78; 1.25) |
| Vaccination (%): | ||||
| Full (Yes) | 18.5 | 81.5 | ||
| Full (No) | 21.6 | 78.4 | 0.26 | 0.77 (0.58; 1.02) |
| At least 1 dose (Yes) | 18.5 | 81.5 | ||
| At least 1 dose (No) | 20.7 | 79.3 | 0.27 | 0.85 (0.66; 1.11) |
| Day-care/School attendance (%): | ||||
| Yes | 22.1 | 77.9 | ||
| No | 16.7 | 83.3 | 0.005 | 1.78 (1.24; 1.53) |
| Breast feeding: | ||||
| number of months (Mean (SEM)) | 5.7 (0.4) | 5.95 (0.7) | 0.9 | 1.0 (0.99; 1.00) |
| Siblings (%): | ||||
| No | 41.5 | 58.5 | ||
| Yes | 47.2 | 52.8 | 0.055 | 1.16 (0.91; 1.47) |
| Antibiotics last month (%): | ||||
| Yes | 20.3 | 15.6 | ||
| No | 79.7 | 84.4 | 0.15 | 0.68 (0.43; 1.07) |
| Season (%): | ||||
| Summer | 17.1 | 82.9 | ||
| Winter | 21.6 | 78.4 | 0.019 | 1.35 (1.05; 1.73) |
| Antibiotic | Susceptible Isolates n/% | Resistant Isolates n/% | Intermediate Isolates n/% |
|---|---|---|---|
| Penicillin (non-meningitis) | 164/64.3 | 4/1.6 | 87/34.1 |
| Penicillin (meningitis) | 164/64.3 | 91/35.7 | |
| Oral Amoxicillin | 228/89.5 | 27/10.5 | |
| Cefotaxime | 231/90.6 | 1/0.4 | 23/9.1 |
| Vancomycin | 255/100 | ||
| Levofloxacin | 255/100 | ||
| Erythromycin | 173/67.8 | 82/32.1 | |
| Tetracycline | 187/73.3 | 68/26.7 | |
| Chloramphenicol | 244/95.7 | 11/4.3 | |
| Clindamycin | 188/73.7 | 67/26.3 | |
| Linezolid | 255/100 | ||
| Trimetroprim-sulfamethoxazole | 183/71.8 | 72/28.2 | |
| Rifampicin | 252/98.8 | 3/1.2 |
| Serotype | Number of Isolates | Penicillin Intermediate and Resistant Isolates n/(%) | Erythromycin Resistant Isolates n/(%) | Trimethoprim Sulfamethoxazole Resistant Isolates n/(%) |
|---|---|---|---|---|
| 11A | 22 | 11/(50) | 10/(45.5) | 16/(72.7%) |
| 23B | 34 | 17/(50) | 7/(43.8) | 14/(41.2) |
| 19F * | 13 | 9/(69) | 9/(69) | 9/(69.2) |
| 6C | 13 | 8/(61.5) | 8/(61.5) | 3/(23) |
| 35B | 9 | 7/(77.7) | 4/(44.4) | 1/(11) |
| 19A * | 7 | 5/(71.5) | 5/(71.5) | 2/(28.5) |
| 6A * | 6 | 4/(66.6) | 4/(66.6) | 5/(83) |
| 15A | 10 | 2/(20) | 5/(50) | 0/(0) |
| 23A | 14 | 1/(7) | 7/(50) | 4(28.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfayate Miguélez, S.; Yague Guirao, G.; Menasalvas Ruíz, A.I.; Sanchez-Solís, M.; Domenech Lucas, M.; González Camacho, F.; Ortíz Romero, M.M.; Espejo García, P.; Guerrero Gómez, C.; Iofrío de Arce, A.; et al. Impact of Pneumococcal Vaccination in the Nasopharyngeal Carriage of Streptococcus pneumoniae in Healthy Children of the Murcia Region in Spain. Vaccines 2021, 9, 14. https://doi.org/10.3390/vaccines9010014
Alfayate Miguélez S, Yague Guirao G, Menasalvas Ruíz AI, Sanchez-Solís M, Domenech Lucas M, González Camacho F, Ortíz Romero MM, Espejo García P, Guerrero Gómez C, Iofrío de Arce A, et al. Impact of Pneumococcal Vaccination in the Nasopharyngeal Carriage of Streptococcus pneumoniae in Healthy Children of the Murcia Region in Spain. Vaccines. 2021; 9(1):14. https://doi.org/10.3390/vaccines9010014
Chicago/Turabian StyleAlfayate Miguélez, Santiago, Genoveva Yague Guirao, Ana I. Menasalvas Ruíz, Manuel Sanchez-Solís, Mirian Domenech Lucas, Fernando González Camacho, M. Mar Ortíz Romero, Pilar Espejo García, Carmen Guerrero Gómez, Antonio Iofrío de Arce, and et al. 2021. "Impact of Pneumococcal Vaccination in the Nasopharyngeal Carriage of Streptococcus pneumoniae in Healthy Children of the Murcia Region in Spain" Vaccines 9, no. 1: 14. https://doi.org/10.3390/vaccines9010014
APA StyleAlfayate Miguélez, S., Yague Guirao, G., Menasalvas Ruíz, A. I., Sanchez-Solís, M., Domenech Lucas, M., González Camacho, F., Ortíz Romero, M. M., Espejo García, P., Guerrero Gómez, C., Iofrío de Arce, A., Moreno Parrado, L., Sánchez Andrada, R. M., Cascales Alcolea, E., Lorente García, S., Paredes Reyes, P., Casquet Barceló, Á., López Yepes, M. L., Vigueras Abellán, J. J., Sanz Mateo, G., & Murcian Pneumococcal Study Group. (2021). Impact of Pneumococcal Vaccination in the Nasopharyngeal Carriage of Streptococcus pneumoniae in Healthy Children of the Murcia Region in Spain. Vaccines, 9(1), 14. https://doi.org/10.3390/vaccines9010014








