Novel Candidates for Vaccine Development Against Mycoplasma Capricolum Subspecies Capripneumoniae (Mccp)—Current Knowledge and Future Prospects
Abstract
1. Introduction
2. Need for CCPP Vaccines
3. CCPP Vaccines: Historical Perspective and Development
4. The Current State of CCPP Vaccine Development
5. Proteomic Approaches
6. Genomic Approaches
7. Other Possibilities
8. Clues from Other Novel Vaccines
9. Conclusions and Future Prospects
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- AU-IBAR. Contagious Caprine Pleuropneumonia. 2013. Available online: http://www.au-ibar.org/contagious-caprine-pleuropneumonia (accessed on 11 June 2019).
- OIE (World Organization for Animal Health). Manual of Diagnostic Tests and Vaccines for Terrestrial Animals 2018. Contagious Caprine Pleuropneumonia. Chapter 3.7.4. 2018. Available online: http://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.07.04_CCPP.pdf (accessed on 11 June 2019).
- OIE (World Organization for Animal Health). Contagious Caprine Pleuropneumonia. 2019. Available online: http://www.oie.int/fileadmin/Home/eng/Animal_Health_in_the_World/docs/pdf/Disease-cards/contagious_caprine_pleuro.pdf (accessed on 11 June 2019).
- Parray, O.R.; Yatoo, M.I.; Bhat, R.A.; Malik, H.U.; Bashir, S.T.; Magray, S.N. Seroepidemiology and risk factor analysis of contagious caprine pleuropneumonia in Himalayan Pashmina Goats. Small Ruminant Res. 2019, 171, 23–36. [Google Scholar] [CrossRef]
- Yatoo, M.I.; Parray, O.R.; Bashir, S.T.; Muheet Bhat, R.A.; Gopalakrishnan, A.; Karthik, K.; Dhama, K.; Singh, S.V. Contagious caprine pleuropneumonia—A comprehensive review. Vet. Q. 2019, 39, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Rurangirwa, F.R.; Masiga, W.N.; Muthomi, E. Immunity to contagious caprine pleuropneumonia caused by F-38 strain of mycoplasma. Vet. Rec. 1981, 109, 310. [Google Scholar] [CrossRef] [PubMed]
- Rurangirwa, F.R.; McGuire, T.C.; Chema, S.; Kibor, A. Vaccination against contagious caprine pleuropneumonia caused by F38. Isr. J. Med. Sci. 1987, 23, 641–643. [Google Scholar]
- Litamoi, J.K.; Lijodi, F.K.; Nandokha, E. Contagious caprine pleuropneumonia: Some observations in a field vaccination trial using inactivated Mycoplasma strain F38. Trop. Anim. Health Prod. 1989, 21, 146–150. [Google Scholar] [CrossRef] [PubMed]
- Provost, A. Mycoplasmal vaccines. In Vaccine Manual: The Production and Quality Control of Veterinary Vaccines for Use in Developing Countries; Mowat, N., Rweyemamu, M., Eds.; Food and Agricultural Organization of the United Nations: Rome, Italy, 1997; pp. 63–74. [Google Scholar]
- Rurangirwa, F.R.; Masiga, W.N.; Muthomi, E.K. Immunization of goats against contagious caprine pleuropneumonia using sonicated antigens of F-38 strain of mycoplasma. Res. Vet. Sci. 1984, 36, 174–176. [Google Scholar] [CrossRef]
- Rurangirwa, F.R.; McGuire, T.C.; Kibor, A.; Chema, S. An inactivated vaccine for contagious caprine pleuropneumonia. Vet. Rec. 1987, 121, 397–400. [Google Scholar] [CrossRef]
- Ayelet, G.; Laekemariam, Y.; Aschalew, Z.; Esayas, G.; Kassahun, A. Validation of immunity induced by inactivated CCPP vaccine with different adjuvants. Small Ruminant Res. 2007, 73, 200–205. [Google Scholar] [CrossRef]
- Thiaucourt, F.; Pible, O.; Miotello, G.; Nwankpa, N.; Armengaud, J. Improving quality control of contagious caprine pleuropneumonia vaccine with tandem mass spectrometry. Proteomics 2018, 18, e1800088. [Google Scholar] [CrossRef]
- Yatoo, M.I.; Parray, O.R.; Mir, M.S.; Qureshi, S.; Amin, Z.; Kashoo, M.N.; Fazili, M.U.R.; Tufani, N.A.; Singh, M.; Kanwar, S.C.; et al. Mycoplasmosis in small ruminants in India: A review. J. Exp. Biol. Agri. Sci. 2018, 6, 264–281. [Google Scholar] [CrossRef]
- March, J.B.; Gammack, C.; Nicholas, R. Rapid detection of contagious caprine pleuropneumonia using a Mycoplasma capricolum subsp. capripneumoniae capsular polysaccharide-specific antigen detection latex agglutination test. J. Clin. Microbiol. 2000, 38, 4152–4159. [Google Scholar] [PubMed]
- Zhao, P.; He, Y.; Chu, Y.F.; Gao, P.C.; Zhang, X.; Zhang, N.Z.; Zhao, H.Y.; Zhang, K.S.; Lu, Z.X. Identification of novel immunogenic proteins in Mycoplasma capricolum subsp. capripneumoniae strain M1601. J. Vet. Med. Sci. 2012, 74, 1109–1115. [Google Scholar] [CrossRef] [PubMed]
- Zhao, P.; He, Y.; Chu, Y.; Li, B.; Gao, P.; Zhang, X.; Zhao, H.; Shang, Y.; Lu, Z. Optimizing and expressing of proteins including PDHA, PDHB and PDHC of Mycoplasma capricolum sub sp. capripneumoniae. Asian J. Anim. Vet. Adv. 2013, 8, 723–731. [Google Scholar]
- March, J.B.; Harrison, J.C.; Borich, S.M. Humoral immune responses following experimental infection of goats with Mycoplasma capricolum subsp. capripneumoniae. Vet. Microbial. 2002, 84, 29–45. [Google Scholar] [CrossRef]
- Liljander, A.; Sacchini, F.; Stoffel, M.H.; Schieck, E.; Stokar-Regenscheit, N.; Labroussaa, F.; Heller, M.; Salt, J.; Frey, J.; Falquet, L.; et al. Reproduction of contagious caprine pleuropneumonia reveals the ability of convalescent sera to reduce hydrogen peroxide production in vitro. Vet. Res. 2019, 50, 10. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.; Hao, H.; Zhao, P.; Thiaucourt, F.; He, Y.; Gao, P.; Guo, H.; Ji, W.; Wang, Z.; Lu, Z.; et al. Genome-wide analysis of the first sequenced Mycoplasma capricolum subsp. capripneumoniae strain M1601. G3 (Bethesda) 2017, 7, 2899–2906. [Google Scholar] [CrossRef]
- Chu, Y.; Gao, P.; Zhao, P.; He, Y.; Liao, N.; Jackman, S.; Zhao, Y.; Birol, I.; Duan, X.; Lu, Z. Genome sequence of Mycoplasma capricolum subsp. capripneumoniae strain M1601. J. Bacteriol. 2011, 193, 6098–6099. [Google Scholar] [CrossRef] [PubMed]
- Peyraud, A.; Poumarat, F.; Tardy, F.; Manso-Silván, L.; Hamroev, K.; Tilloev, T.; Amirbekov, M.; Tounkara, K.; Bodjo, C.; Wesonga, H.; et al. An international collaborative study to determine the prevalence of contagious caprine pleuropneumonia by monoclonal antibody-based cELISA. BMC. Vet. Res. 2014, 10, 48. [Google Scholar] [CrossRef]
- Muheet Malik, H.U.; Parray, O.R.; Bhat, R.A.; Yatoo, M.I. Seasonal and periodic rhythmicity of respiratory infections in small ruminants. Biol. Rhythm Res. 2019, 50, 1–9. [Google Scholar] [CrossRef]
- Bahir, W.; Omar, O.; Rosales, R.S.; Hlusek, M.; Ziay, G.; Schauwers, W.; Whatmore, A.M.; Nicholas, R.A.J. Search for OIE-listed ruminant mycoplasma diseases in Afghanistan. BMC Vet. Res. 2017, 13, 149. [Google Scholar] [CrossRef]
- Amirbekov, M.; Murvatulloev, S.; Ferrari, G. Contagious caprine pleuropneumonia detected for the first time in Tajikistan. EMPRES Transboundary. Anim. Dis. Bull. 2010, 35, 20–22. [Google Scholar]
- Awan, M.A.; Abbas, F.; Yasinzai, M.; Nicholas, R.A.; Babar, S.; Ayling, R.D.; Attique, M.A.; Ahmed, Z.; Wadood, A.; Khan, F.A. First report on the molecular prevalence of Mycoplasma capricolum subspecies capripneumoniae (Mccp) in goats the cause of contagious caprine pleuropneumonia (CCPP) in Balochistan province of Pakistan. Mol. Biol. Rep. 2010, 37, 3401–3406. [Google Scholar] [CrossRef] [PubMed]
- Manso-Silván, L.; Dupuy, V.; Chu, Y.; Thiaucourt, F. Multi-locus sequence analysis of Mycoplasma capricolum subsp. capripneumoniae for the molecular epidemiology of contagious caprine pleuropneumonia. Vet. Res. 2011, 42, 86. [Google Scholar]
- Wang, H.; Ni, L.; Yang, H.; Xu, L.; Ma, N.; Ding, H. Isolation and identification of Mycoplasma mycoides cluster strains from goats in Chongqing, China. Bull. Vet. Inst. Pulawy 2014, 58, 11–15. [Google Scholar] [CrossRef][Green Version]
- El-Deeb, W.; Almujalli, A.A.; Eljalii, I.; Elmoslemany, A.; Fayez, M. Contagious caprine pleuropneumonia: The first isolation and molecular characterization of Mycoplasma capricolum subsp. capripneumoniae in the Kingdom of Saudi Arabia. Acta Trop. 2017, 168, 74–79. [Google Scholar] [CrossRef] [PubMed]
- Arif, A.; Schulz, J.; Thiaucourt, F.; Taha, A.; Hammer, S. Contagious caprine pleuropneumonia outbreak in captive wild ungulates at Al Wabra Wildlife Preservation, State of Qatar. J. Zoo. Wildl. Med. 2007, 38, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Teshome, D.; Sori, T.; Sacchini, F.; Wieland, B. Epidemiological investigations of contagious caprine pleuropneumonia in selected districts of Borana zone, Southern Oromia, Ethiopia. Trop. Anim. Health Prod. 2019, 51, 703–711. [Google Scholar] [CrossRef] [PubMed]
- Wesonga, H.O.; Bölske, G.; Thiaucourt, F.; Wanjohi, C.; Lindberg, R. Experimental contagious caprine pleuropneumonia: A long-term study on the course of infection and pathology in a flock of goats infected with Mycoplasma capricolum subsp. capripneumoniae. Acta Vet. Scand. 2004, 45, 167. [Google Scholar] [CrossRef]
- Kipronoh, K.A.; Ombui, J.N.; Binepal, Y.S.; Wesonga, H.O.; Gitonga, E.K.; Thuranira, E.; Kiara, H.K. Risk factors associated with contagious caprine pleuropneumonia in goats in pastoral areas in the Rift Valley region of Kenya. Prev. Vet. Med. 2016, 132, 107–112. [Google Scholar] [CrossRef]
- Mbyuzi, A.O.; Komba, E.V.; Kimera, S.I.; Kambarage, D.M. Sero-prevalence and associated risk factors of peste des petits ruminants and contagious caprine pleuro-pneumonia in goats and sheep in the Southern Zone of Tanzania. Prev. Vet. Med. 2014, 116, 138–144. [Google Scholar] [CrossRef]
- Ozdemir, U.; Turkyilaz, M.A.; Sayi, O.; Erpeck, S.H.; Nicholas, R.A.J. Survey for contagious caprine pleuropneumonia in the Thrace region of Turkey. Rev. Sci. Tech. Off. Int. Epi. 2018, 37, In press. [Google Scholar]
- Yu, Z.; Wang, T.; Sun, H.; Xia, Z.; Zhang, K.; Chu, D.; Xu, Y.; Xin, Y.; Xu, W.; Cheng, K.; et al. Contagious caprine pleuropneumonia in endangered Tibetan antelope, China, 2012. Emerg. Infect. Dis. 2013, 19, 2051. [Google Scholar] [CrossRef] [PubMed]
- Chaber, A.L.; Lignereux, L.; Al Qassimi, M.; Saegerman, C.; Manso-Silvan, L.; Dupuy, V.; Thiaucourt, F. Fatal transmission of contagious caprine pleuropneumonia to an Arabian oryx (Oryx leucoryx). Vet. Microbiol. 2014, 173, 156–159. [Google Scholar] [CrossRef] [PubMed]
- Lignereux, L.; Chaber, A.L.; Saegerman, C.; Manso-Silván, L.; Peyraud, A.; Apolloni, A.; Thiaucourt, F. Unexpected field observations and transmission dynamics of contagious caprine pleuropneumonia in a sand gazelle herd. Prev. Vet. Med. 2018, 157, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Nicholas, R.A.J.; Churchward, C. Contagious caprine pleuropneumonia: New aspects of an old disease. Transboud. Emerg. Dis. 2012, 59, 189–196. [Google Scholar] [CrossRef]
- EFSA AHAW Panel (European Food Safety Authority (EFSA)-Panel on Animal Health and Welfare (AWAH); More, S.; Bøtner, A. Scientific Opinion on the assessment of listing and categorisation of animal diseases within the framework of the Animal Health Law (Regulation (EU) No 2016/429): contagious caprine pleuropneumonia. EFSA J. 2017, 15, 4996. [Google Scholar]
- Thiaucourt, F.; Bölske, G.; Leneguersh, B.; Smith, D.; Wesonga, H. Diagnosis and control of contagious caprine pleuropneumonia. Rev. Sci. Tech. 1996, 15, 1415–1429. [Google Scholar] [CrossRef]
- Yatoo, M.I.; Parray, O.R.; Bhat, R.A.; Muheet; Gopalakrishnan, A.; Saxena, A.; Chakraborty, S.; Tiwari, R.; Khurana, S.K.; Singh, S.V.; et al. Emerging antibiotic resistance in Mycoplasma microorganisms, designing effective and novel drugs/therapeutic targets: Current knowledge and futuristic prospects. J. Pure. Appl. Microbiol. 2019, 13, 27–44. [Google Scholar] [CrossRef]
- Yatoo, M.I.; Parray, O.R.; Muheet Bhat, R.A.; Malik, H.U.; Fazili, M.R.; Qureshi, S.; Mir, M.S.; Yousuf, R.W.; Tufani, N.A.; Dhama, K.; et al. Comparative evaluation of different therapeutic protocols for contagious caprine pleuropneumonia in Himalayan Pashmina goats. Trop. Anim. Health Prod. 2019. [Google Scholar] [CrossRef]
- Spickler, A.R. Contagious caprine pleuropneumonia. 2015. Available online: http://www.cfsph.iastate.edu/DiseaseInfo/factsheets.php (accessed on 11 of June 2019).
- Lipner, M.E.; Brown, R.B. Constraints to the integration of the contagious caprine pleuropneumonia (CCPP) vaccine into Kenya’s animal health delivery system. Agric. Hum. Values 1995, 12, 19–28. [Google Scholar] [CrossRef]
- Hutcheon, D. Contagious pleuro-pneumonia in goats at Cape Colony, South Africa. Veterinary J. Ann. Comp. Pathol. 1889, 29, 399–404. [Google Scholar] [CrossRef]
- MacOwan, K.J.; Minette, J.E. The effect of high passage Mycoplasma strain F38 on the course of contagious caprine pleuropneumonia (CCPP). Trop. Anim. Health Prod. 1978, 10, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Muthomi, E.K.; Rurangirwa, F.R. Passive haemagglutination and complement fixation as diagnostic tests for contagious caprine pleuropneumonia caused by the F-38 strain of mycoplasma. Res. Vet. Sci. 1983, 35, 1–4. [Google Scholar] [CrossRef]
- Perreau, P.; Breard, A.; le Goff, C. Experimental infection of goats with type F38 mycoplasma strains (CCPP). Ann. Microbiol. 1984, 135A, 119–124. [Google Scholar]
- King, G.J. Optimum age to vaccinate for contagious caprine pleuropneumonia. Vet Rec. 1988, 123, 572–573. [Google Scholar] [CrossRef] [PubMed]
- Rurangirwa, F.R.; Kouyate, B.; Niang, M.; McGuire, T.C. CCPP: Antibodies to F38 polysaccharide in Mali goats. Vet. Rec. 1990, 127, 353. [Google Scholar] [PubMed]
- Rurangirwa, F.R.; McGuire, T.C.; Mbai, L.; Ndung’u, L.; Wambugu, A. Preliminary field test of lyophilised contagious caprine pleuropneumonia vaccine. Res. Vet. Sci. 1991, 50, 240–241. [Google Scholar] [CrossRef]
- Thiaucourt, F.; Gu6rin, C.; Mady, V.; Lefvre, P.C. Diagnostic de la pleuropneumonie contagieuse caprine (PPCC): amé1iorations récentes. Rev. Sci. Tech. Off. Int. Epiz. 1992, 11, 859–865. [Google Scholar] [CrossRef]
- Thiaucourt, F.; Bölske, G.; Libeau, G.; Le Goff, C.; Lefèvre, P.C. The use of monoclonal antibodies in the diagnosis of contagious caprine pleuropneumonia (CCPP). Vet. Microbiol. 1994, 41, 191–203. [Google Scholar] [CrossRef]
- Rurangirwa, F.R.; Shompole, P.S.; Wambugu, A.N.; Kihara, S.M.; McGuire, T.C. Monoclonal antibody E8-18 identifies an integral membrane surface protein unique to Mycoplasma capricolum subsp. capripneumoniae. Clin. Diagn. Lab. Immunol. 1997, 4, 615–619. [Google Scholar]
- March, J.B.; Jones, G.E. Inhibitory effects of vaccines containing subunit fractions of Mycoplasma capricolum subsp. capripneumoniae. In Mycoplasmas of Ruminants: Pathogenicity, Diagnostics, Epidemiology and Molecular Genetics; Bergonnier, D., Berthelot, X., Frey, J., Eds.; European Commission: Luxembourg, 1998; Volume 2, pp. 44–49. [Google Scholar]
- March, J.B.; Foster, N.; Harrison, J.C.; Gammack, C.; Hyndman, L.; Borich, S.M.; Jones, G.E. Immune responses following experimental infection of goats with Mycoplasma capricolum subsp. capripneumoniae, causal agent of contagious caprine pleuropneumonia. In Mycoplasmas of Ruminants: Pathogenicity, Diagnostics, Epidemiology and Molecular Genetics; Bergonnier, D., Berthelot, X., Frey, J., Eds.; European Commission: Luxembourg, 2000; Volume 4, pp. 205–208. [Google Scholar]
- Radostitis, O.M.; Gay, C.C.; Constable, P.D.; Hinchcliff, K.W. A textbook of the diseases of cattle, sheep, pigs, goats and horses, 10th ed.; W.B. Saunders Co.: Philadelphia, PA, USA, 2009. [Google Scholar]
- Tarekegn, S.; Temesgen, W.; Alemu, S.; Ayelet, G. An experimental live vaccine trial against contagious caprine pleuropneumonia. Afr. J. Microbiol. Res. 2012, 6, 3085–3087. [Google Scholar]
- Lakew, M.; Sisay, T.; Ayelet, G.; Eshetu, E.; Dawit, G.; Tolosa, T. Seroprevalence of contagious caprine pleuropneumonia and field performance of inactivated vaccine in Borana pastoral area, southern Ethiopia. Afr J Microbiol Res 2014, 8, 2344–2351. [Google Scholar]
- Tesgera, T.; Sori, H.; Yami, M.; Mamo, B. Evaluation of safety and immunogenicity of inactivated whole culture contagious caprine pleuropneumonia trial vaccine in National Veterinary Institute, Ethiopia. African J Micro Res. 2017, 11, 466–473. [Google Scholar]
- Samiullah, S. Contagious caprine pleuropneumonia and its current picture in Pakistan: A review. Vet. Med. 2013, 58, 389–398. [Google Scholar] [CrossRef]
- Mulira, G.L.; Masiga, W.N.; Nandokha, E. Efficacy of different adjuvants to potentiate the immune response to mycoplasma strain F-38. Trop. Anim. Health Prod. 1988, 20, 30–34. [Google Scholar] [CrossRef]
- Rurangirwa, F.R.; Wambugu, A.N.; Kihara, S.M.; Mcguire, T.C. A Mycoplasma strain F38 growth-inhibiting monoclonal antibody (WM-25) identifies an epitope on a surface-exposed polysaccharide antigen. Infect. Immun. 1995, 63, 1415–1420. [Google Scholar]
- Pettersson, B.; Bölske, G.; Thiaucourt, F.; Uhlén, M.; Johansson, K.E. Molecular evolution of Mycoplasma capricolum subsp. capripneumoniae strains, based on polymorphisms in the 16S rRNA genes. J. Bacteriol. 1998, 180, 2350–2358. [Google Scholar]
- Lorenzon, S.; Wesonga, H.; Ygesu, L.; Tekleghiorgis, T.; Maikano, Y.; Angaya, M.; Hendrikx, P.; Thiaucourt, F. Genetic evolution of Mycoplasma capricolum subsp. capripneumoniae strains and molecular epidemiology of contagious caprine pleuropneumonia by sequencing of locus H2. Vet. Microbiol. 2002, 85, 111–123. [Google Scholar] [CrossRef]
- Woubit, S.; Lorenzon, S.; Peyraud, A.; Manso-Silvan, L.; Thiaucourt, F. A specific PCR for the identification of Mycoplasma capricolum subsp. capripneumoniae, the causative agent of contagious caprine pleuropneumonia (CCPP). Vet. Microbiol. 2004, 104, 125–132. [Google Scholar] [CrossRef]
- Dupuy, V.; Verdier, A.; Thiaucourt, F.; Manso-Silván, L. A large-scale genomic approach affords unprecedented resolution for the molecular epidemiology and evolutionary history of contagious caprine pleuropneumonia. Vet. Res. 2015, 46, 74. [Google Scholar] [CrossRef]
- Pelley, J.W. Glycolysis and Pyruvate Oxidation; Elsevier’s Integrated Biochemistry: Amsterdam, The Netherlands, 2007. [Google Scholar]
- Byron, O.; Lindsay, J.G. The pyruvate dehydrogenase complex and related assemblies in health and disease. Subcell. Biochem. 2017, 83, 523–550. [Google Scholar]
- Multhoff, G. Heat shock protein 70 (Hsp70): Membrane location, export and immunological relevance. Methods 2007, 43, 229–237. [Google Scholar] [CrossRef]
- Schenk, G.; Duggleby, R.G.; Nixon, P.F. Properties and functions of the thiamin diphosphate dependent enzyme transketolase. Int. J. Biochem. Cell Biol. 1998, 30, 1297–1318. [Google Scholar] [CrossRef]
- Wintermeyer, W.; Savelsbergh, A.; Konevega, A.L.; Peske, F.; Katunin, V.I.; Semenkov, Y.P.; Fischer, N.; Stark, H.; Rodnina, M.V. Functions of elongation factor G in translocation and ribosome recycling. In Ribosomes; Springer: Vienna, Austria, 2011; pp. 329–338. [Google Scholar]
- Postma, P.W.; Roseman, S. The bacterial phosphoenolpyruvate: Sugar phosphotransferase system. Biochim. Biophys. Acta Rev. Biomembr. 1976, 457, 213–257. [Google Scholar] [CrossRef]
- Markert, C.L. Lactate dehydrogenase. Biochemistry and function of lactate dehydrogenase. Cell Biochem. Funct. 1984, 2, 131–134. [Google Scholar] [CrossRef]
- Jarocki, V.M.; Santos, J.; Tacchi, J.L.; Raymond, B.B.; Deutscher, A.T.; Jenkins, C.; Padula, M.P.; Djordjevic, S.P. MHJ_0461 is a multifunctional leucine aminopeptidase on the surface of Mycoplasma hyopneumoniae. Open Biol. 2015, 5, 140175. [Google Scholar] [CrossRef] [PubMed]
- Mustacich, D.; Powis, G. Thioredoxin reductase. Biochem. J. 2000, 346, 1–8. [Google Scholar] [CrossRef]
- Yamamoto, H.; Qin, Y.; Achenbach, J.; Li, C.; Kijek, J.; Spahn, C.M.; Nierhaus, K.H. EF-G and EF4: Translocation and back-translocation on the bacterial ribosome. Nat. Rev. Microbiol. 2014, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Dupuy, V.; Thiaucourt, F. Complete genome sequence of Mycoplasma capricolum subsp. capripneumoniae strain 9231-Abomsa. Genome Announc. 2014, 2, e01067-14. [Google Scholar] [CrossRef]
- Falquet, L.; Liljander, A.; Schieck, E.; Gluecks, I.; Frey, J.; Jores, J. Complete genome sequences of virulent Mycoplasma capricolum subsp. capripneumoniae strains F38 and ILRI181. Genome Announc. 2014, 2, e01041-14. [Google Scholar] [CrossRef] [PubMed]
- Calcutt, M.J.; Foecking, M.F. Comparative analysis of the Mycoplasma capricolum subsp. capricolum GM508D genome reveals subrogation of phase-variable contingency genes and a novel integrated genetic element. Pathog. Dis. 2015, 73, 1–3. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Li, Y.; Wang, R.; Sun, W.; Song, Z.; Bai, F.; Zheng, H.; Xin, J. Comparative genomics analysis of Mycoplasma capricolum subsp. capripneumoniae 87001. Genomics 2019, S0888-754330138-7. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.; Auon, M.; Khan, A.; Khan, M.Z.; Mahmood, F.; Ur-Rehman, S. Contagious caprine pleuropneumonia in Beetal goats. Trop. Anim. Health. Prod. 2012, 44, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, B.; Leitner, T.; Ronaghi, M.; Bölske, G.; Uhlen, M.; Johansson, K.E. Phylogeny of the Mycoplasma mycoides cluster as determined by sequence analysis of the 16S rRNA genes from the two rRNA operons. J. Bacteriol. 1996, 178, 4131–4142. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fischer, A.; Shapiro, B.; Muriuki, C.; Heller, M.; Schnee, C.; Bongcam-Rudloff, E.; Vilei, E.M.; Frey, J.; Jores, J. The origin of the Mycoplasma mycoides cluster coincides with domestication of ruminants. PLoS ONE 2012, 7, e36150. [Google Scholar] [CrossRef] [PubMed]
- Al-Aubaidi, J.M.; Dardiri, A.H.; Fabricant, J. Biochemical characterization and antigenic relationship of Mycoplasma mycoides subsp. mycoides, Freundt and Mycoplasma mycoides subsp. capri (Edward) Freundt. Int. J. Syst. Evol. Microbiol. 1972, 22, 155–164. [Google Scholar] [CrossRef]
- Cottew, G.S.; Breard, A.; DaMassa, A.J.; Ernø, H.; Leach, R.H.; Lefevre, P.C.; Rodwell, A.W.; Smith, G.R. Taxonomy of the Mycoplasma mycoides cluster. Isr. J. Med. Sci. 1987, 23, 632–635. [Google Scholar]
- Corona, L.; Cillara, G.; Tola, S. Proteomic approach for identification of immunogenic proteins of Mycoplasma mycoides subsp. capri. Vet. Microbiol. 2013, 167, 434–439. [Google Scholar] [CrossRef][Green Version]
- Monnerat, M.P.; Thiaucourt, F.; Nicolet, J.; Frey, J. Comparative analysis of the lppA locus in Mycoplasma capricolum subsp. capricolum and Mycoplasma capricolum subsp. capripneumoniae. Vet. Microbiol. 1999, 69, 157–172. [Google Scholar] [CrossRef]
- Robino, P.; Alberti, A.; Chessa, B.; Pittau, M.; Profiti, M.; Rosati, S. Molecular cloning and expression of a surface lipoprotein of Mycoplasma capricolum as a potential antigen for serological diagnosis. Vet. Res. Commun. 2007, 31, 257. [Google Scholar] [CrossRef]
- Neiman, M.; Hamsten, C.; Schwenk, J.M.; Bölske, G.; Persson, A. Multiplex screening of surface proteins from Mycoplasma mycoides subsp. mycoides small colony for an antigen cocktail enzyme-linked immunosorbent assay. Clin. Vaccine Immunol. 2009, 16, 1665–1674. [Google Scholar] [CrossRef] [PubMed]
- Fleury, B.; Bergonier, D.; Berthelot, X.; Schlatter, Y.; Frey, J.; Vilei, E.M. Characterization and analysis of a stable serotype-associated membrane protein (P30) of Mycoplasma agalactiae. J. Clin. Microbiol. 2001, 39, 2814–2822. [Google Scholar] [CrossRef] [PubMed]
- Fleury, B.; Bergonier, D.; Berthelot, X.; Peterhans, E.; Frey, J.; Vilei, E.M. Characterization of P40, a cytadhesin of Mycoplasma agalactiae. Infect. Immun. 2002, 70, 5612–5621. [Google Scholar] [CrossRef] [PubMed]
- Jores, J.; Schieck, E.; Liljander, A.; Sacchini, F.; Posthaus, H.; Lartigue, C.; Blanchard, A.; Labroussaa, F.; Vashee, S. Capsular polysaccharide in Mycoplasma mycoides is a virulence factor. J. Infect. Dis. 2018, 219, 1559–1563. [Google Scholar] [CrossRef]
- Khan, F.A.; Faisal, M.; Chao, J.; Liu, K.; Chen, X.; Zhao, G.; Menghwar, H.; Zhang, H.; Zhu, X.; Rasheed, M.A.; et al. Immunoproteomic identification of MbovP579, a promising diagnostic biomarker for serological detection of Mycoplasma bovis infection. Oncotarget 2016, 7, 39376. [Google Scholar] [CrossRef]
- Cacciotto, C.; Addis, M.F.; Pagnozzi, D.; Chessa, B.; Coradduzza, E.; Carcangiu, L.; Uzzau, S.; Alberti, A.; Pittau, M. The liposoluble proteome of Mycoplasma agalactiae: An insight into the minimal protein complement of a bacterial membrane. BMC Microbiol. 2010, 10, 225. [Google Scholar] [CrossRef] [PubMed]
- Chopra-Dewasthaly, R.; Citti, C.; Glew, M.D.; Zimmermann, M.; Rosengarten, R.; Jechlinger, W. Phase-locked mutants of Mycoplasma agalactiae: Defining the molecular switch of high-frequency Vpma antigenic variation. Mol. Microbiol. 2008, 67, 1196–1210. [Google Scholar] [CrossRef]
- Gaurivaud, P.; Persson, A.; Le Grand, D.; Westberg, J.; Solsona, M.; Johansson, K.E.; Poumarat, F. Variability of a glucose phosphotransferase system permease in Mycoplasma mycoides subsp. mycoides Small Colony. Microbiology 2004, 150, 4009–4022. [Google Scholar] [CrossRef][Green Version]
- Sun, Z.; Fu, P.; Wei, K.; Zhang, H.; Zhang, Y.; Xu, J.; Jiang, F.; Liu, X.; Xu, W.; Wu, W. Identification of novel immunogenic proteins from Mycoplasma bovis and establishment of an indirect ELISA based on recombinant E1 beta subunit of the pyruvate dehydrogenase complex. PLoS ONE 2014, 19, e88328. [Google Scholar] [CrossRef]
- Soayfane, Z.; Houshaymi, B.; Nicholas, R.A.J. Mycoplasma capricolum subsp. capripneumoniae, the cause of contagious caprine pleuropneumonia, comprises two distinct biochemical groups. Open Vet. J. 2018, 8, 393–400. [Google Scholar] [CrossRef]
- Chernova, O.A.; Medvedeva, E.S.; Mouzykantov, A.A.; Baranova, N.B.; Chernov, V.M. Mycoplasmas and their antibiotic resistance: The problems and prospects in controlling infections. Acta Nat. 2016, 8, 24–34. [Google Scholar] [CrossRef]
- Gründel, A.; Pfeiffer, M.; Jacobs, E.; Dumke, R. Network of surface-displayed glycolytic enzymes in Mycoplasma pneumoniae and their interactions with human plasminogen. Infect. Immun. 2016, 84, 666–676. [Google Scholar] [CrossRef] [PubMed]
- Voorde, J.V.; Sabuncuoğlu, S.; Noppen, S.; Hofer, A.; Ranjbarian, F.; Fieuws, S.; Balzarini, J.; Liekens, S. Nucleoside-catabolizing enzymes in mycoplasma-infected tumor cell cultures compromise the cytostatic activity of the anticancer drug gemcitabine. J. Biol. Chem. 2014, 289, 13054–13065. [Google Scholar] [CrossRef] [PubMed]
- Voorde, J.V.; Gago, F.; Vrancken, K.; Liekens, S.; Balzarini, J. Characterization of pyrimidine nucleoside phosphorylase of Mycoplasma hyorhinis: Implications for the clinical efficacy of nucleoside analogues. Biochem. J. 2012, 445, 113–123. [Google Scholar] [CrossRef] [PubMed]
- Schmidl, S.R.; Otto, A.; Lluch-Senar, M.; Piñol, J.; Busse, J.; Becher, D.; Stülke, J. A trigger enzyme in Mycoplasma pneumoniae: Impact of the glycerophosphodiesterase GlpQ on virulence and gene expression. PLoS Pathog. 2011, 7, 1002263. [Google Scholar] [CrossRef] [PubMed]
- Blötz, C.; Stülke, J. Glycerol metabolism and its implication in virulence in Mycoplasma. FEMS Microbiol Rev. 2017, 41, 640–652. [Google Scholar] [CrossRef] [PubMed]
- Großhennig, S.; Schmidl, S.R.; Schmeisky, G.; Busse, J.; Stülke, J. Implication of glycerol and phospholipid transporters in Mycoplasma pneumoniae growth and virulence. Infect. Immun. 2013, 81, 896–904. [Google Scholar] [CrossRef] [PubMed]
- You, X.X.; Zeng, Y.H.; Wu, Y.M. Interactions between mycoplasma lipid-associated membrane proteins and the host cells. J. Zhejiang Uni. Sci. B. 2006, 7, 342–350. [Google Scholar] [CrossRef]
- He, Y.; Zhang, N.-Z.; Zhao, P.; Chu, Y.-F.; Gao, P.-C.; Zhang, J.-J.; Liu, X.-T.; Lu, Z.-X. Sensitive and rapid detection of Mycoplasma capricolum subsp. capripneumoniae by Loop-mediated isothermal amplification. Afr. J. Biotechnol. 2014, 13, 2113–2118. [Google Scholar] [CrossRef]
- Szczepanek, S.M.; Frasca, S.; Schumacher, V.L.; Liao, X.; Padula, M.; Djordjevic, S.P.; Geary, S.J. Identification of lipoprotein MslA as a neoteric virulence factor of Mycoplasma gallisepticum. Infect. Immun. 2010, 78, 3475–3483. [Google Scholar] [CrossRef]
- Shimizu, T.; Kida, Y.; Kuwano, K. Triacylated lipoproteins derived from Mycoplasma pneumoniae activate nuclear factor-κB through toll-like receptors 1 and 2. Immunology 2007, 121, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.C.; Lin, I.H.; Chung, W.J.; Hu, W.S.; Ng, W.V.; Lu, C.Y.; Huang, T.Y.; Shu, H.W.; Hsiao, K.J.; Tsai, S.F.; et al. Proteomics characterization of cytoplasmic and lipid-associated membrane proteins of human pathogen Mycoplasma fermentans M64. PLoS ONE 2012, 7, e35304. [Google Scholar] [CrossRef] [PubMed]
- Medvedeva, E.S.; Baranova, N.B.; Mouzykantov, A.A.; Grigorieva, T.Y.; Davydova, M.N.; Trushin, M.V.; Chernova, O.A.; Chernov, V.M. Adaptation of mycoplasmas to antimicrobial agents: Acholeplasma laidlawii extracellular vesicles mediate the export of ciprofloxacin and a mutant gene related to the antibiotic target. Sci. World, J. 2014, 2014, 150615. [Google Scholar] [CrossRef] [PubMed]
- Krishnakumar, R.; Assad-Garcia, N.; Benders, G.A.; Phan, Q.; Montague, M.G.; Glass, J.I. Targeted chromosomal knockouts in Mycoplasma pneumoniae. App. Env. Microbiol. 2010, 76, 5297–5299. [Google Scholar] [CrossRef] [PubMed]
- Lambert, T. Antibiotics that affect the ribosome. Revue Sci. Tech. OIE 2012, 31, 57. [Google Scholar] [CrossRef]
- Hames, C.; Halbedel, S.; Hoppert, M.; Frey, J.; Stülke, J. Glycerol metabolism is important for cytotoxicity of Mycoplasma pneumoniae. J. Bacteriol. 2009, 191, 747–753. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.; Singh, V.P.; Kashoo, Z.A.; Rana, R.; Cheema, P.S. Serological and molecular characterization of central domain of lipoprotein LppA in Indian isolates of Mycoplasma mycoides subsp. capri and Mycoplasma mycoides subsp. mycoides (LC). Int. J. Livest. Res. 2017, 7, 90–108. [Google Scholar] [CrossRef]
- Zhang, D.; Long, Y.; Li, M.; Gong, J.; Li, X.; Lin, J.; Meng, J.; Gao, K.; Zhao, R.; Jin, T. Development and evaluation of novel recombinant adenovirus-based vaccine candidates for infectious bronchitis virus and Mycoplasma gallisepticum in chickens. Avian Pathol. 2018, 47, 213–222. [Google Scholar] [CrossRef]
- Moura, L.; Dohms, J.; Almeida, J.M.; Ferreira, P.S.; Biffi, C.P.; Backes, R.G. Development and evaluation of a novel subunit vaccine for Mycoplasma gallisepticum. Arq Bras Med Vet Zootec. 2012, 64, 1569–1576. [Google Scholar] [CrossRef]
- Virginio, V.G.; Gonchoroski, T.; Paes, J.A.; Schuck, D.C.; Zaha, A.; Ferreira, H.B. Immune responses elicited by Mycoplasma hyopneumoniae recombinant antigens and DNA constructs with potential for use in vaccination against porcine enzootic pneumonia. Vaccine 2014, 32, 5832–5838. [Google Scholar] [CrossRef]
- Marques Neto, L.M.; Kipnis, A.; Junqueira-Kipnis, A.P. Role of metallic nanoparticles in vaccinology: Implications for infectious disease vaccine development. Front. Immunol. 2017, 8, 239. [Google Scholar] [CrossRef] [PubMed]
- Virginio, V.G.; Bandeira, N.C.; Leal, F.M.; Lancellotti, M.; Zaha, A.; Ferreira, H.B. Assessment of the adjuvant activity of mesoporous silica nanoparticles in recombinant Mycoplasma hyopneumoniae antigen vaccines. Heliyon 2017, 3, e00225. [Google Scholar] [CrossRef] [PubMed]
- Jorge, S.; Dellagostin, O.A. The development of veterinary vaccines: A review of traditional methods and modern biotechnology approaches. Biotech. Res. Innov. 2017, 1, 6–13. [Google Scholar] [CrossRef]
- Shams, H. Recent developments in veterinary vaccinology. Vet. J. 2005, 170, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Duthie, M.S.; Windish, H.P.; Fox, C.B.; Reed, S.G. Use of defined TLR ligands as adjuvants within human vaccines. Immunol. Rev. 2011, 239, 178–196. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.L.; Staats, H.F. Cytokines: The future of intranasal vaccine adjuvants. Clin. Dev. Immunol. 2011, 2011, 289597. [Google Scholar] [CrossRef] [PubMed]
- Temizoz, B.; Kuroda, E.; Ishii, K.J. Vaccine adjuvants as potential cancer immunotherapeutics. Int. Immunol. 2016, 28, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Cheema, P.S. Expression and Immunodiagnostic Evaluation of Membrane Protein P48 of Mycoplasma agalactiae. Ph.D. Thesis, Indian Veterinary Research Institute, Bareilly, India, 2009. [Google Scholar]
- Dhama, K.; Mahendran, M.; Gupta, P.K.; Rai, A. DNA vaccines and their applications in veterinary practice: Current perspectives. Vet. Res. Commun. 2008, 32, 341–356. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.L.; Wang, S.N.; Yang, W.J.; Chen, Y.J.; Lin, H.H.; Shiuan, D. Expression and immunogenicity of Mycoplasma hyopneumoniae heat shock protein antigen P42 by DNA vaccination. Infect. Immun. 2003, 71, 1155–1160. [Google Scholar] [CrossRef]
- Dhama, K.; Wani, M.Y.; Deb, R.; Karthik, K.; Tiwari, R.; Barathidasan, R.; Kumar, A.; Mahima; Verma, A.K.; Singh, S.D. Plant based oral vaccines for human and animal pathogens – a new era of prophylaxis: Current and future perspectives. J. Exp. Biol. Agri. Sci. 2013, 1, 1–12. [Google Scholar]
- Sander, V.A.; Corigliano, M.G.; Clemente, M. Promising plant-derived adjuvants in the development of coccidial vaccines. Front Vet Sci. 2019, 6, 20. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.K.; Badasara, S.K.; Dhama, K.; Malik, Y.P.S. Progress and prospects in vaccine research. In Proceedings of the National Workshop on “Current Trends and Future Research Challenges in Vaccines and Adjuvants”, Organized at ICAR Indian Veterinary Research Institute, Bareilly, India, 19–20 November 2015; pp. 1–19. [Google Scholar]
- Parameswaran, N.; Russell, G.C.; Bartley, K.; Grant, D.M.; Deane, D.; Todd, H.; Dagleish, M.P.; Haig, D.M. The effect of the TLR9 ligand CpG-oligodeoxynucleotide on the protective immune response to alcelaphine herpesvirus-1-mediated malignant catarrhal fever in cattle. Vet Res. 2014, 45, 59. [Google Scholar] [CrossRef] [PubMed]
- Kawai, T.; Akira, S. The role of pattern-recognition receptors in innate immunity: Update on Toll-like receptors. Nat. Immunol. 2010, 11, 373. [Google Scholar] [CrossRef] [PubMed]
| Mycoplasma | Vaccine Type/Candidate | Remarks | Commercial Availability | Dose, Route | Reference |
|---|---|---|---|---|---|
| Mycoplasma capricolum subspecies capripneumoniae (Mccp) | Lung extract or pleural fluid from affected animals | Crude type of vaccination | Commercially not available | Subcutaneously | [46] |
| Mccp strain F38 | Attenuated/passaged broth culture | Culture medium-based vaccination | Commercially not available | 10 mL (109 CFU), intratracheal route | [47] |
| Sonicated antigens of the Mccp strain F38 | Inactivated or attenuated with incomplete Freund’s adjuvant (IFA), emulsified with aluminum hydroxide or phosphate buffered saline (PBS) | Antigen incorporated in IFA provided solid immunity to the challenge | Commercially not available | Subcutaneously | [10] |
| Lyophilized Mccp strain F38 | Lyophilized vaccine | Challenged goats developed complete immunity to experimentally induced-CCPP | Commercially not available | Minimum dose 0.15 mg, subcutaneously | [7] |
| Strain F38 of Mycoplasma in saponin | Inactivated or attenuated Mccp vaccines | Provided immunity for more than 12 months, can be stored at 4 or 22 °C for 14 months | Commercially available. Cost about 100 USD | Dose of 0.15 mg optimum, subcutaneously | [11] |
| Sonicated antigens of the Mccp strain F38 | Inactivated or attenuated with Freund’s incomplete adjuvant (IFA), saponin, aluminium hydroxide gel or PBS | Saponin and IFA were similar in their immune potentiating ability and were superior to aluminum hydroxide | Commercially not available | Subcutaneously | [63] |
| Mccp strain F38 | Formalinized Mycoplasma culture | Optimum age for vaccination beyond 10 weeks of age | Commercially not available | 1 mL per goat | [50] |
| Mccp strain F38 | Inactivated Mccp strain F38-saponin vaccine | 3 mg of saponin inactivates 1 mL of sonicated protein (2 mg/mL). 100% protection against natural CCPP | Commercially available. Cost about 100 USD | 1 mL per goat, subcutaneously | [8] |
| Mccp strain F38 | Polysaccharide vaccines | Humoral immune response | Vaccine candidates. Commercially not available | Vaccination potential not evaluated | [51] |
| Mccp strain F38 | Lyophilized, saponin-killed vaccine, field vaccine | 100% protection against mortality and 95% protection against clinical disease | Commercially available. Cost about 100 USD | Single dose of 0.15 mg, subcutaneously | [52] |
| Mccp strain F38 | Epitope on a surface-exposed polysaccharide antigen | Detected by monoclonal antibody (mAb) WM-25 | Vaccine candidate. Commercially not available | Antiserum raised against this epitope caused growth inhibition and agglutination. Developed immune response in goats | [64] |
| Mccp strain F38 | Crude or membrane protein antigens | Identified by spotting on nitrocellulose using immunobinding | Vaccine candidate. Commercially not available | Standardized 0.5 mg protein/ml and finally 4 out of 60 specific antigens were identified by mAbs. Vaccination potential not evaluated | [53] |
| Mccp strains (G22, G94/83, G108/83, and G280/80 | Specific integral membrane surface protein (p24) | Identified with the help of mAb E8-18 | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [55] |
| Mccp strain 19/2 | Subunit fractions of Mccp | Inhibitory effects as vaccines were noted | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [56] |
| Mccp strain 19/2 | Capsular polysaccharide (CPS) | Prophylactic ability evaluated | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [15,56,57] |
| Mccp strain 19/2 | Immunodominant core proteins (108, 70, 62 kDa) | Basis for recombinant protein for prophylactic vaccine | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [18] |
| Mccp Kenyan isolate (F38) | Saponin-adjuvated vaccines versus Montanide ISA 50-adjuvated vaccine | Montanide ISA 50-adjuvanted vaccines are safe, effective and show compatibility | Commercially available. Cost about 100 USD | 1 mL/animal of saponin and Montanide ISA 50 adjuvated vaccines and 2 mL of MCCP and Bacillus anthracis adjuvanted with saponin. 0.2 mg of Mycoplasma protein per animal and 3 mg/dose of saponin. Subcutaneous injection into right thoracic wall | [12] |
| Mccp F38 strain | Inactivated F38 vaccine, aluminum hydroxide terpene vaccine | Booster 1 month, immunity short lived, kids vaccinated at above 12 months age | Commercially available. Cost about 100 USD | Recommended as vaccination | [58] |
| Kenyan isolate of Mccp | Live vaccines | Absence of any post-vaccination reaction, early appearance and longer persistence of antibodies. Chance of disease outbreaks | Commercially available. Cost about 100 USD | Dose of 105 Mccp candidate live vaccine. Subcutaneously into right thoracic wall | [59] |
| F-38 Kenyan strain of Mccp | Inactivated whole culture vaccines | 61.1% goats seroconverted, higher antibody titer in young and adult goats than older ones | Commercially available. Cost about 100 USD | 1 mL/goat subcutaneously into neck region | [60] |
| Mccp Kenyan isolate | Inactivated whole culture vaccine | Equally safe and immunogenic as other vaccines but easy production, requires less time and is not capital investment intensive | Commercially available. Cost about 50–100 USD | 2 mL subcutaneously | [61] |
| Mccp (local isolate) | Saponin-inactivated vaccine | 14 month-shelf life and 12 month-immunity. Adverse reactions and incompatibility issues of saponin adjuvants, not recommended in pregnant animals | Commercially available. Cost about 100 USD | 1 mL per goat (0.15 mg of freeze-dried-Mccp protein and 3 mg of saponin in a dose of 1 mL) subcutaneously | [2] |
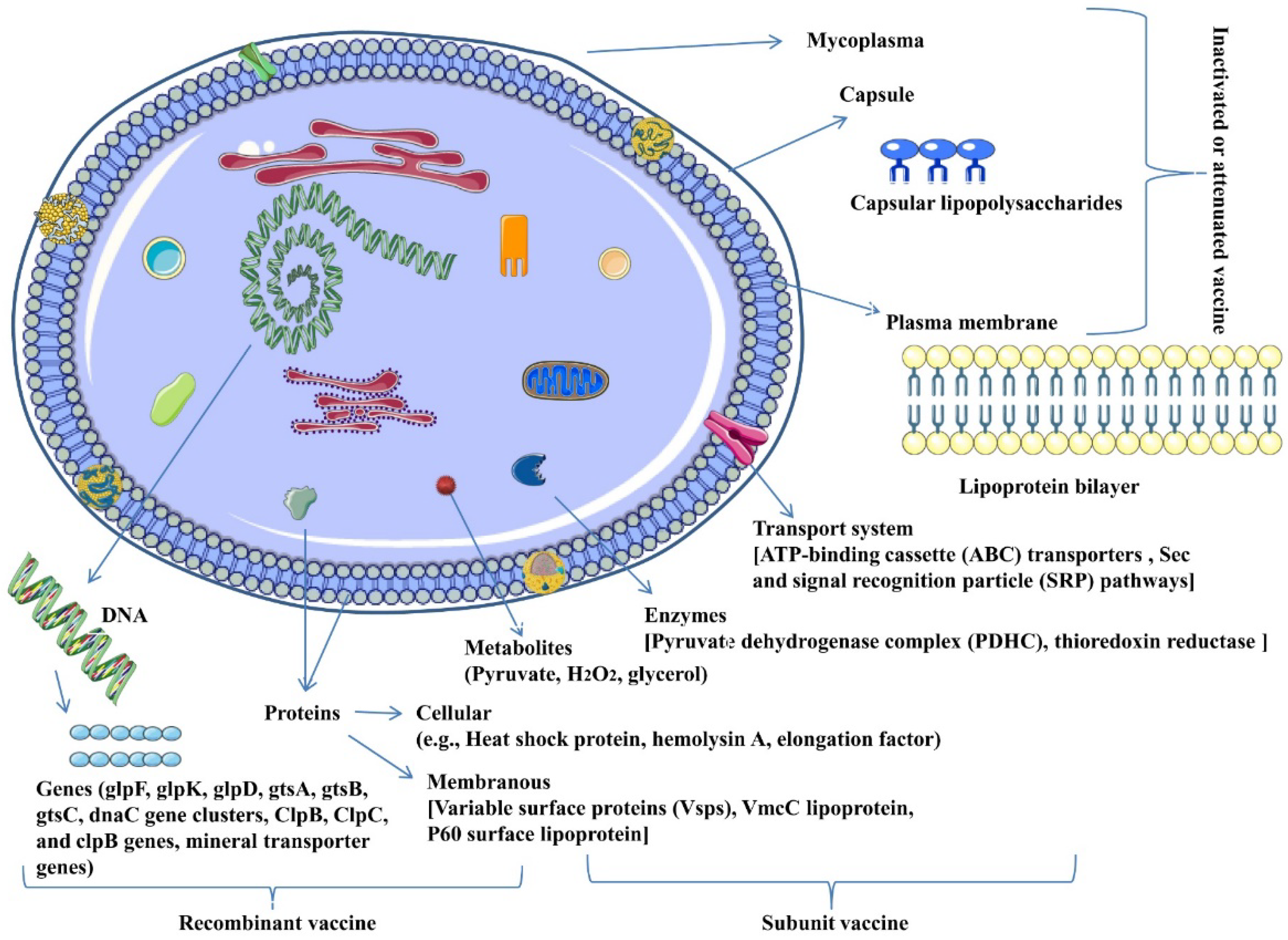
| Mccp (strain M1601, ILRI181, 9231-Abomsa) | Proteins (both membranous and cellular) | Heat shock protein 70 (HSP70), elongation factor G, glutamyl-tRNA amidotransferase subunit A family catalytic domain protein, aldehyde dehydrogenase (NAD) family protein, thioredoxin reductase (NADPH), elongation factor Tu and peptidase M24 family | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [13,16,17] |
| Mccp (strain M1601, 9231-Abomsa) | Proteins, peptides | Variable surface proteins (Vsps), VmcC lipoprotein, P60 surface lipoprotein, hemolysin A, specific peptides | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [13,17,20,21] |
| Mccp (strain M1601, ILRI181, strain 9231-Abomsa) | Genes | 16S rRNA genes, H2 locus and arginine deiminase (ADI) operon, glpF, glpK and glpD gene cluster, and gtsA, gtsB, and gtsC gene cluster, dnaC, adhesion protein gene, capsule synthesis gene clusters, lipoproteins, hemolysin A, ClpB, ClpC, and clpB genes, magnesium transporter genes (XDU01000099, XDU01000796, XDU01000848), potassium transporter TrkA (XDU01000743) and sodium transporter (XDU01000742) genes | Vaccine candidate. Commercially not available | Vaccination potential not evaluated | [20,21,65,66,67,68] |
| Mccp (strain M1601, ILRI181) | Enzymes | Pyruvate dehydrogenase complex (PDHC), transketolase, phosphoenolpyruvate protein phosphotransferase, L-lactate dehydrogenase, cytosol aminopeptidase, L-α-glycerophosphate oxidase (GlpO) | Vaccine candidate. Commercially not available | Vaccination potential not evaluated. | [16,19] |
| Mccp (strain M1601, ILRI181) | Metabolic pathways | Pyruvate metabolism, transporter systems [ATP-binding cassette (ABC) transporters and phosphotransferase], secretion systems [Sec and signal recognition particle (SRP) pathways], glycerol uptake, hydrogen peroxide production | Vaccine candidate. Commercially not available | Vaccination potential not evaluated. | [17,19,20] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yatoo, M.I.; Parray, O.R.; Muheet; Bhat, R.A.; Nazir, Q.U.; Haq, A.U.; Malik, H.U.; Fazili, M.U.R.; Gopalakrishnan, A.; Bashir, S.T.; et al. Novel Candidates for Vaccine Development Against Mycoplasma Capricolum Subspecies Capripneumoniae (Mccp)—Current Knowledge and Future Prospects. Vaccines 2019, 7, 71. https://doi.org/10.3390/vaccines7030071
Yatoo MI, Parray OR, Muheet, Bhat RA, Nazir QU, Haq AU, Malik HU, Fazili MUR, Gopalakrishnan A, Bashir ST, et al. Novel Candidates for Vaccine Development Against Mycoplasma Capricolum Subspecies Capripneumoniae (Mccp)—Current Knowledge and Future Prospects. Vaccines. 2019; 7(3):71. https://doi.org/10.3390/vaccines7030071
Chicago/Turabian StyleYatoo, Mohd Iqbal, Oveas Raffiq Parray, Muheet, Riyaz Ahmed Bhat, Qurat Un Nazir, Abrar Ul Haq, Hamid Ullah Malik, Mujeeb Ur Rehman Fazili, Arumugam Gopalakrishnan, Shah Tauseef Bashir, and et al. 2019. "Novel Candidates for Vaccine Development Against Mycoplasma Capricolum Subspecies Capripneumoniae (Mccp)—Current Knowledge and Future Prospects" Vaccines 7, no. 3: 71. https://doi.org/10.3390/vaccines7030071
APA StyleYatoo, M. I., Parray, O. R., Muheet, Bhat, R. A., Nazir, Q. U., Haq, A. U., Malik, H. U., Fazili, M. U. R., Gopalakrishnan, A., Bashir, S. T., Tiwari, R., Khurana, S. K., Chaicumpa, W., & Dhama, K. (2019). Novel Candidates for Vaccine Development Against Mycoplasma Capricolum Subspecies Capripneumoniae (Mccp)—Current Knowledge and Future Prospects. Vaccines, 7(3), 71. https://doi.org/10.3390/vaccines7030071






