A Quantitative Exploration of the Relationship Between Healthcare Accessibility and Mass Media in Nigeria Using the Levesque Framework of Healthcare Access
Abstract
1. Introduction
- AreNigerian mothers/caregivers of children with incomplete immunizations less likely to be exposed to mass media and ICT?
- Do sociodemographic factors influence the relationship between media/ICT exposure and incomplete immunization?
2. Materials and Methods
2.1. Dataset and Population
2.2. Dependent and Independent Variables
2.3. Statistical Analyses
2.4. Geospatial Mapping
3. Results
3.1. Frequency Analysis
3.2. Bivariate Cross-Tabulation Analysis Using Chi-Square Test
3.3. Linear Logistic Regression Model Analysis
4. Discussion
Study Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- United Nations. Pact for the Future: Including the Global Digital Compact and Declaration on Future Generations (Resolution A/RES/79/1) [PDF]. United Nations. 2024. Available online: https://www.un.org/sites/un2.un.org/files/sotf-pact_for_the_future_adopted.pdf (accessed on 7 August 2025).
- World Health Organization; World Bank. Tracking Universal Health Coverage: 2023 Global Monitoring Report. © World Health Organization and the International Bank for Reconstruction and Development/The World Bank. License: CC BY-NC-SA 3.0 IGO. 2023. Available online: http://hdl.handle.net/10986/40348 (accessed on 7 August 2025).
- Ilesanmi, O.S.; Afolabi, A.A.; Adeoya, C.T. Driving the implementation of the National Health Act of Nigeria to improve the health of her population. Pan Afr. Med. J. 2023, 45, 157. [Google Scholar] [CrossRef]
- Levesque, J.-F.; Harris, M.F.; Russell, G. Patient-centred access to health care: Conceptualising access at the interface of health systems and populations. Int. J. Equity Health 2013, 12, 18. [Google Scholar] [CrossRef]
- Cu, A.; Meister, S.; Lefebvre, B.; Ridde, V. Assessing healthcare access using the Levesque’s conceptual framework– a scoping review. Int. J. Equity Health 2021, 20, 116. [Google Scholar] [CrossRef]
- Eboreime, E.; Abimbola, S.; Bozzani, F. Access to Routine Immunization: A Comparative Analysis of Supply-Side Disparities between Northern and Southern Nigeria. PLoS ONE 2015, 10, e0144876. [Google Scholar] [CrossRef]
- Welcome, M. The Nigerian health care system: Need for integrating adequate medical intelligence and surveillance systems. J. Pharm. Bioallied Sci. 2011, 3, 470. [Google Scholar] [CrossRef] [PubMed]
- Adesina, M.A.; Olufadewa, I.I.; Oladele, R.I.; Solagbade, A.; Olaoyo, C. Determinants of childhood immunization among rural mothers in Nigeria. Popul. Med. 2023, 5, 1–7. [Google Scholar] [CrossRef]
- Ataguba, J.E.; Ojo, K.O.; Ichoku, H.E. Explaining socio-economic inequalities in immunization coverage in Nigeria. Health Policy Plan. 2016, 31, 1212–1224. [Google Scholar] [CrossRef]
- Ayodele, A.M.; Fasasi, M.I.; Rejoice Uche, O.; Gideon Ikemdinachi, N.; Henry Ugochukwu, U. Factors associated with full childhood vaccination coverage among young mothers in Northern Nigeria. Pan Afr. Med. J. 2024, 47, 4. [Google Scholar] [CrossRef]
- Olorunsaiye, C.Z.; Degge, H. Variations in the Uptake of Routine Immunization in Nigeria: Examining Determinants of Inequitable Access. Glob. Health Commun. 2016, 2, 19–29. [Google Scholar] [CrossRef]
- Williams, S.V.; Akande, T.; Abbas, K. Systematic review of social determinants of childhood immunisation in low- and middle-income countries and equity impact analysis of childhood vaccination coverage in Nigeria. PLoS ONE 2024, 19, e0297326. [Google Scholar] [CrossRef]
- Olaoye, A.; Onyenankeya, K. A systematic review of health communication strategies in Sub-Saharan Africa-2015–2022. Health Promot. Perspect. 2023, 13, 10–20. [Google Scholar] [CrossRef]
- Ajaero, C.K.; Odimegwu, C.; Ajaero, I.D.; Nwachukwu, C.A. Access to mass media messages, and use of family planning in Nigeria: A spatio-demographic analysis from the 2013 DHS. BMC Public Health 2016, 16, 427. [Google Scholar] [CrossRef] [PubMed]
- Konkor, I.; Sano, Y.; Antabe, R.; Kansanga, M.; Luginaah, I. Exposure to mass media family planning messages among post-delivery women in Nigeria: Testing the structural influence model of health communication. Eur. J. Contracept. Reprod. Health Care 2019, 24, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Chukwu, C.; Onuoha, H.; Okorafor, K.A.K.; Ojomo, O.; Mokuolu, O.A.; Ekholuenetale, M. Geopolitical zones differentials in intermittent preventive treatment in pregnancy (IPTp) and long lasting insecticidal nets (LLIN) utilization in Nigeria. PLoS ONE 2021, 16, e0254475. [Google Scholar] [CrossRef] [PubMed]
- Adedire, E.B.; Ajumobi, O.; Bolu, O.; Nguku, P.; Ajayi, I. Maternal knowledge, attitude, and perception about childhood routine immunization program in Atakumosa-west Local Government Area, Osun State, Southwestern Nigeria. Pan Afr. Med. J. 2021, 40, 8. [Google Scholar]
- Taiwo, L.; Idris, S.; Abubakar, A.; Nguku, P.; Nsubuga, P.; Gidado, S.; Okeke, L.; Emiasegen, S.; Waziri, E. Factors affecting access to information on routine immunization among mothers of under 5 children in Kaduna State Nigeria, 2015. Pan Afr. Med. J. 2017, 27, 186. [Google Scholar] [CrossRef]
- Olaniyan, A.; Isiguzo, C.; Agbomeji, S.; Akinlade-Omeni, O.; Ifie, B.; Hawk, M. Barriers, facilitators, and recommendations for childhood immunisation in Nigeria: Perspectives from caregivers, community leaders, and healthcare workers. Pan Afr. Med. J. 2022, 43, 19. [Google Scholar] [CrossRef]
- National Bureau of Statistics (NBS); United Nations Children’s Fund (UNICEF). Multiple Indicator Cluster Survey 2021, Statistical Snapshot Report. Abuja, Nigeria: National Bureau of Statistics and United Nations Children’s Fund. 2022. Available online: https://www.unicef.org/nigeria/media/6126/file/2021-MICS-Statistical-Snapshots-Report.pdf (accessed on 31 March 2025).
- Jacques, M.; Lorton, F.; Dufourg, M.N.; Bois, C.; Launay, E.; Simeon, T.; Raude, J.; Gras-Le Guen, C.; Levy-Bruhl, D.; Charles, M.A.; et al. Determinants of incomplete vaccination in children at age two in France: Results from the nationwide ELFE birth cohort. Eur. J. Pediatr. 2023, 182, 1019–1028. [Google Scholar] [CrossRef]
- Ogundele, O.A.; Ogunwemimo, H.S.; Fehintola, F.O.; Ogundele, T.; Olorunsola, A.; Bello, O.E.; Asubario, O.Y. Predictors of incomplete childhood vaccination in four West African countries: A population based cross-sectional study. Sci. Rep. 2025, 15, 17119. [Google Scholar] [CrossRef]
- Tsegaw, T.K.; Alemaw, H.B.; Wale, Y.B.; Nigatu, S.G.; Birhan, T.Y.; Taddese, A.A. Incomplete immunization uptake and associated factors among children aged 12–23 months in sub-Saharan African countries; multilevel analysis evidenced from latest demography and health survey data, 2023. Ital. J. Pediatr. 2024, 50, 96. [Google Scholar] [CrossRef]
- Ogundele, O.A.; Ogundele, T.; Fehintola, F.O.; Fagbemi, A.T.; Beloved, O.O.; Osunmakinwa, O.O. Determinants of incomplete vaccination among children 12-23 months in Nigeria: An analysis of a national sample. Tzu Chi Med. J. 2022, 34, 448–455. [Google Scholar] [CrossRef]
- Ahmed, L.Q.; Adebowale, A.S.; Palamuleni, M.E. Bayesian spatial analysis of incomplete vaccination among children aged 12–23 months in Nigeria. Sci. Rep. 2024, 14, 18297. [Google Scholar] [CrossRef] [PubMed]
- Atta, G.; Newton, P.; Shah, T. Insights into Intimate Partner Violence: Exploring Predictive Factors in Ghana Multiple Indicator Cluster Surveys 2018. Societies 2025, 15, 100. [Google Scholar] [CrossRef]
- Clarke, K.C.; McLafferty, S.L.; Tempalski, B.J. On Epidemiology and Geographic Information Systems: A Review and Discussion of Future Directions. Emerg. Infect. Dis. 1996, 2, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Dimitrova, A.; Carrasco-Escobar, G.; Richardson, R.; Benmarhnia, T. Essential childhood immunization in 43 low- and middle-income countries: Analysis of spatial trends and socioeconomic inequalities in vaccine coverage. PLOS Med. 2023, 20, e1004166. [Google Scholar] [CrossRef]
- Maqbool, N.; Newton, P.; Shah, T. Child Labor in Sindh, Pakistan: Patterns and Areas in Need of Intervention. Stats 2024, 7, 1437–1453. [Google Scholar] [CrossRef]
- Hui, C.Y.; Abdulla, A.; Ahmed, Z.; Goel, H.; Monsur Habib, G.M.; Teck Hock, T.; Khandakr, P.; Mahmood, H.; Nautiyal, A.; Nurmansyah, M.; et al. Mapping national information and communication technology (ICT) infrastructure to the requirements of potential digital health interventions in low- and middle-income countries. J. Glob. Health 2022, 12, 04094. [Google Scholar] [CrossRef]
- Oliver-Williams, C.; Brown, E.; Devereux, S.; Fairhead, C.; Holeman, I. Using Mobile Phones to Improve Vaccination Uptake in 21 Low- and Middle-Income Countries: Systematic Review. JMIR Mhealth Uhealth 2017, 5, e148. [Google Scholar] [CrossRef]
- Udenigwe, O.; Yaya, S. Leaving no woman or girl behind? Inclusion and participation in digital maternal health programs in sub-Saharan Africa. Reprod Health 2022, 19, 54. [Google Scholar] [CrossRef]
- Naugle, D.A.; Hornik, R.C. Systematic Review of the Effectiveness of Mass Media Interventions for Child Survival in Low- and Middle-Income Countries. J. Health Commun. 2014, 19 (Suppl. S1), 190–215. [Google Scholar] [CrossRef]
- Till, S.; Mkhize, M.; Farao, J.; Shandu, L.D.; Muthelo, L.; Coleman, T.L.; Mbombi, M.; Bopape, M.; Klingberg, S.; Van Heerden, A.; et al. Digital Health Technologies for Maternal and Child Health in Africa and Other Low- and Middle-Income Countries: Cross-disciplinary Scoping Review with Stakeholder Consultation. J. Med. Internet Res. 2023, 25, e42161. [Google Scholar] [CrossRef]
- Uzoma, I.E. Adewoyin, Y., Ed.; Nigeria. In Health and Medical Geography in Africa; Global Perspectives on Health Geography: Springer, Cham, 2023. [Google Scholar] [CrossRef]
- Asubiaro, T.; Badmus, O.; Ikenyei, U.; Popoola, B.; Igwe, E. Exploring Sub-Saharan Africa’s Communication of COVID-19-Related Health Information on Social Media. Libri 2021, 71, 123–139. [Google Scholar] [CrossRef]
- Rhoda, D.A.; Wagai, J.N.; Beshanski-Pedersen, B.R.; Yusafari, Y.; Sequeira, J.; Hayford, K.; Brown, D.W.; Danovaro-Holliday, M.C.; Braka, F.; Ali, D.; et al. Combining cluster surveys to estimate vaccination coverage: Experiences from Nigeria’s multiple indicator cluster survey/national immunization coverage survey (MICS/NICS), 2016–2017. Vaccine 2020, 38, 6174–6183. [Google Scholar] [CrossRef]
| Variable | Description |
|---|---|
| Sex of Child | Male or female |
| Health Insurance of Child | Whether or not the child has health insurance of any kind |
| Area of Residence | Urban or rural |
| Region | Which of 37 distinct regions a respondent was living |
| Geopolitical Zone | Which of 6 geopolitical zones a respondent was living |
| Mother’s Age | 7 age ranges between 15 and 49 |
| Mother’s Education | Highest level of education attended (but not necessarily completed) |
| Ethnicity of Household Head | Ethnicity of household head |
| Wealth Index Quintile | Household’s income status by quintile |
| Ever Read a Newspaper or Magazine ª | Whether a mother has ever read a newspaper or magazine |
| Ever Listened to Radio ª | Whether a mother has ever listened to the radio |
| Ever Watched Television ª | Whether a mother has ever watched television |
| Ever Used Internet ª | Whether a mother has ever used the internet |
| Own a Mobile Phone ª | Whether or not a mother owns a mobile phone |
| Variables | Frequency | Percent | Variables | Frequency | Percent |
|---|---|---|---|---|---|
| Region | Childhood Immunization Status | ||||
| Abia | 201 | 1.6 | Complete | 3283 | 26.2 |
| Adamawa | 299 | 2.4 | Incomplete | 9250 | 73.8 |
| Akwa Ibom | 259 | 2.1 | Area | ||
| Anambra | 318 | 2.5 | Urban | 4601 | 36.7 |
| Bauchi | 651 | 5.2 | Rural | 7933 | 63.3 |
| Bayelsa | 111 | 0.9 | Mother’s education ª | ||
| Benue | 386 | 3.1 | None | 5093 | 40.6 |
| Borno | 367 | 2.9 | Primary | 1946 | 15.5 |
| Cross River | 192 | 1.5 | Junior secondary | 820 | 6.5 |
| Delta | 257 | 2.0 | Senior secondary | 3402 | 27.1 |
| Ebonyi | 188 | 1.5 | Higher/tertiary | 1270 | 10.1 |
| Edo | 204 | 1.6 | Mother’s Age ª | ||
| Ekiti | 151 | 1.2 | 15–19 | 239 | 1.9 |
| Enugu | 217 | 1.7 | 20–24 | 1682 | 13.4 |
| Gombe | 260 | 2.1 | 25–29 | 2763 | 22.0 |
| Jigawa | 539 | 4.3 | 30–34 | 2442 | 19.5 |
| Kaduna | 562 | 4.5 | 35–39 | 1897 | 15.1 |
| Kano | 927 | 7.4 | 40–44 | 985 | 7.9 |
| Katsina | 761 | 6.1 | 45–49 | 437 | 3.5 |
| Kebbi | 413 | 3.3 | Health insurance ª | ||
| Kogi | 229 | 1.8 | With insurance | 337 | 2.7 |
| Kwara | 198 | 1.6 | Without insurance | 12,167 | 97.1 |
| Lagos | 716 | 5.7 | Wealth index quintile ª | ||
| Nasarawa | 180 | 1.4 | Poorest | 3029 | 24.2 |
| Niger | 395 | 3.2 | Second | 2813 | 22.4 |
| Ogun | 327 | 2.6 | Middle | 2440 | 19.5 |
| Ondo | 206 | 1.6 | Fourth | 2200 | 17.6 |
| Osun | 193 | 1.5 | Richest | 2050 | 16.4 |
| Oyo | 376 | 3.0 | Sex of Child | ||
| Plateau | 300 | 2.4 | Male | 6263 | 50.0 |
| Rivers | 383 | 3.1 | Female | 6270 | 50.0 |
| Sokoto | 434 | 3.5 | Ethnicity of household head | ||
| Taraba | 272 | 2.2 | Hausa | 4135 | 33.0 |
| Yobe | 290 | 2.3 | Igbo | 1496 | 11.9 |
| Zamfara | 401 | 3.2 | Yoruba | 1589 | 12.7 |
| FCT | 144 | 1.1 | Fulani | 1179 | 9.4 |
| Imo | 229 | 1.8 | Kanuri | 318 | 2.5 |
| Geopolitical Zone | Ijaw | 179 | 1.4 | ||
| North Central | 1831 | 14.6 | Ibibio | 252 | 2.0 |
| North East | 2138 | 17.1 | Edo | 164 | 1.3 |
| North West | 4037 | 32.2 | Tiv | 327 | 2.6 |
| South East | 1153 | 9.2 | Other ethnicity | 2893 | 23.1 |
| South South | 1405 | 11.2 | |||
| South West | 1968 | 15.7 |
| Variables | Frequency | Percent |
|---|---|---|
| Television ª | ||
| Have Never Watched TV | 9424 | 75.2 |
| Have Watched TV | 1015 | 8.1 |
| Radio ª | ||
| Have Never Listened to Radio | 5957 | 47.5 |
| Have Listened to Radio | 4488 | 35.8 |
| Newspaper/Magazine ª | ||
| Have Never Read Newspaper/Magazine | 6363 | 50.8 |
| Have Read Newspaper/Magazine | 4075 | 32.5 |
| Internet Use (Ever) ª | ||
| Yes | 1391 | 11.1 |
| No | 8780 | 70.1 |
| Own a Mobile Phone ª | ||
| Yes | 5456 | 43.5 |
| No | 4983 | 39.8 |
| Factors | Immunization Status of Child | Chi-Square p-Value | |
|---|---|---|---|
| Complete | Incomplete | ||
| Individual Factors | |||
| Sex of Child | 0.362 | ||
| Male | 1663 (26.6%) | 4600 (73.4%) | |
| Female | 1620 (25.8%) | 4650 (74.2%) | |
| Health insurance | <0.001 | ||
| With insurance | 131 (38.9%) | 206 (61.1%) | |
| Without insurance | 3149 (25.9%) | 9019 (74.1%) | |
| Household Factors | |||
| Area of Residence | <0.001 | ||
| Urban | 1670 (36.3%) | 2930 (63.7%) | |
| Rural | 1612 (20.3%) | 6320 (79.7%) | |
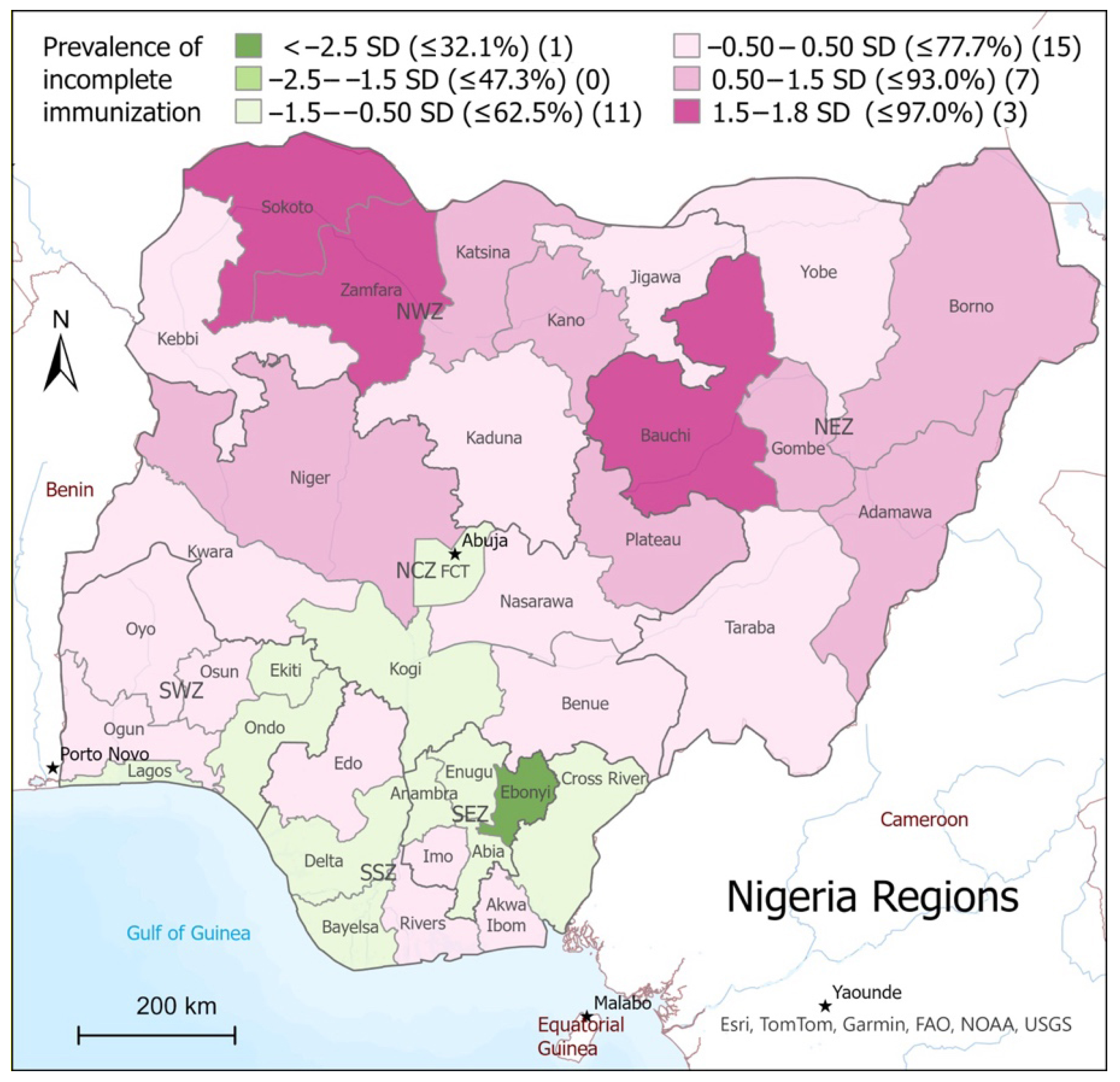
| Region | <0.001 | ||
| Abia | 86 (43.0%) | 114 (57.0%) | |
| Adamawa | 43 (14.4%) | 255 (85.6%) | |
| Akwa Ibom | 82 (31.7%) | 177 (68.3%) | |
| Anambra | 158 (49.7%) | 160 (50.3%) | |
| Bauchi | 35 (5.4%) | 615 (94.6%) | |
| Bayelsa | 47 (42.3%) | 64 (57.7%) | |
| Benue | 109 (28.2%) | 277 (71.8%) | |
| Borno | 32 (8.7%) | 335 (91.3%) | |
| Cross River | 79 (40.9%) | 114 (59.1%) | |
| Delta | 103 (40.1%) | 154 (59.9%) | |
| Ebonyi | 139 (73.9%) | 49 (26.1%) | |
| Edo | 68 (33.3%) | 136 (66.7%) | |
| Ekiti | 59 (39.1%) | 92 (60.9%) | |
| Enugu | 103 (47.5%) | 114 (52.5%) | |
| Gombe | 28 (10.7%) | 233 (89.3%) | |
| Imo | 61 (26.6%) | 168 (73.4%) | |
| Jigawa | 125 (23.2%) | 414 (76.8%) | |
| Kaduna | 141 (25.1%) | 420 (74.9%) | |
| Kano | 79 (8.5%) | 849 (91.5%) | |
| Katsina | 136 (17.9%) | 625 (82.1%) | |
| Kebbi | 147 (35.7%) | 265 (64.3%) | |
| Kogi | 111 (48.5%) | 118 (51.5%) | |
| Kwara | 57 (28.9%) | 140 (71.1%) | |
| Lagos | 358 (50.0%) | 358 (50.0%) | |
| Nasarawa | 43 (23.9%) | 137 (76.1%) | |
| Niger | 47 (11.9%) | 348 (88.1%) | |
| Ogun | 87 (26.6%) | 240 (73.4%) | |
| Ondo | 86 (41.7%) | 120 (58.3%) | |
| Osun | 65 (33.7%) | 128 (66.3%) | |
| Oyo | 119 (31.6%) | 257 (68.4%) | |
| Plateau | 48 (16.0%) | 252 (84.0%) | |
| Rivers | 123 (32.1%) | 260 (67.9%) | |
| Sokoto | 13 (3.0%) | 421 (97.0%) | |
| Taraba | 90 (33.3%) | 181 (66.8%) | |
| Yobe | 96 (33.1%) | 194 (66.9%) | |
| Zamfara | 21 (5.2%) | 380 (94.8%) | |
| FCT | 56 (39.2%) | 87 (60.8%) | |
| Geopolitical Zone | <0.001 | ||
| North Central | 470 (25.7%) | 1361 (74.3%) | |
| North East | 325 (15.2%) | 1813 (84.8%) | |
| North West | 663 (16.4%) | 3374 (83.6%) | |
| South East | 548 (47.5%) | 605 (52.5%) | |
| South South | 501 (35.7%) | 904 (64.3%) | |
| South West | 775 (39.4%) | 1194 (60.6%) | |
| Mother’s Age | |||
| 15–19 | 39 (16.3%) | 201 (83.8%) | <0.001 |
| 20–24 | 301 (17.9%) | 1380 (82.1%) | |
| 25–29 | 577 (20.9%) | 2185 (79.1%) | |
| 30–34 | 709 (29.0%) | 1733 (71.0%) | |
| 35–39 | 511 (26.9%) | 1386 (73.1%) | |
| 40–44 | 227 (23.0%) | 758 (77.0%) | |
| 45–49 | 88 (20.1%) | 349 (79.9%) | |
| Mother’s Education | <0.001 | ||
| None | 759 (14.9%) | 4334 (85.1%) | |
| Primary | 482 (24.8%) | 1464 (75.2%) | |
| Junior secondary | 195 (23.8%) | 626 (76.2%) | |
| Senior secondary | 1290 (37.9%) | 2112 (62.1%) | |
| Higher/tertiary | 557 (43.9%) | 713 (56.1%) | |
| Ethnicity of Household Head | <0.001 | ||
| Hausa | 634 (15.3%) | 3501 (84.7%) | |
| Igbo | 692 (46.3%) | 804 (53.7%) | |
| Yoruba | 633 (39.8%) | 957 (60.2%) | |
| Fulani | 173 (14.7%) | 1005 (85.3%) | |
| Kanuri | 53 (16.7%) | 265 (83.3%) | |
| Tiv | 90 (27.5%) | 237 (72.5%) | |
| Ijaw | 65 (36.1%) | 115 (63.9%) | |
| Ibibio | 90 (35.7%) | 162 (64.3%) | |
| Edo | 65 (39.6%) | 99 (60.4%) | |
| Other ethnicity | 789 (27.3%) | 2104 (72.7%) | |
| Wealth Index Quintile | <0.001 | ||
| Poorest | 475 (15.7%) | 2554 (84.3%) | |
| Second | 539 (19.2%) | 2274 (80.8%) | |
| Middle | 645 (26.4%) | 1795 (73.6%) | |
| Fourth | 704 (32.0%) | 1496 (68.0%) | |
| Richest | 918 (44.8%) | 1132 (55.2%) | |
| Mother’s Media Access Variables | |||
| Ever Read a Newspaper/Magazine | <0.001 | ||
| Yes | 1345 (33.0%) | 2729 (67.0%) | |
| No | 1103 (17.3%) | 5260 (82.7%) | |
| Ever Listened to Radio | <0.001 | ||
| Yes | 1297 (28.9%) | 3191 (71.1%) | |
| No | 1156 (19.4%) | 4801 (80.6%) | |
| Ever Watched Television | <0.001 | ||
| Yes | 454 (44.7%) | 561 (55.3%) | |
| No | 1995 (21.2%) | 7429 (78.8%) | |
| Ever Used Internet | <0.001 | ||
| Yes | 545 (39.2%) | 846 (60.8) | |
| No | 1810 (20.6%) | 6970 (79.4%) | |
| Own a Mobile Phone | <0.001 | ||
| Yes | 1664 (30.5%) | 3792 (69.5%) | |
| No | 789 (15.8%) | 4194 (84.2%) | |
| Factors | B | Sig. | AOR | 95% CI for AOR | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Individual Factors | |||||
| Health insurance | |||||
| With insurance (ref) | |||||
| Without insurance | −0.251 | 0.119 | 0.778 | 0.567 | 1.067 |
| Household Factors | |||||
| Area | |||||
| Urban (ref) | |||||
| Rural | 0.077 | 0.317 | 1.080 | 0.929 | 1.255 |
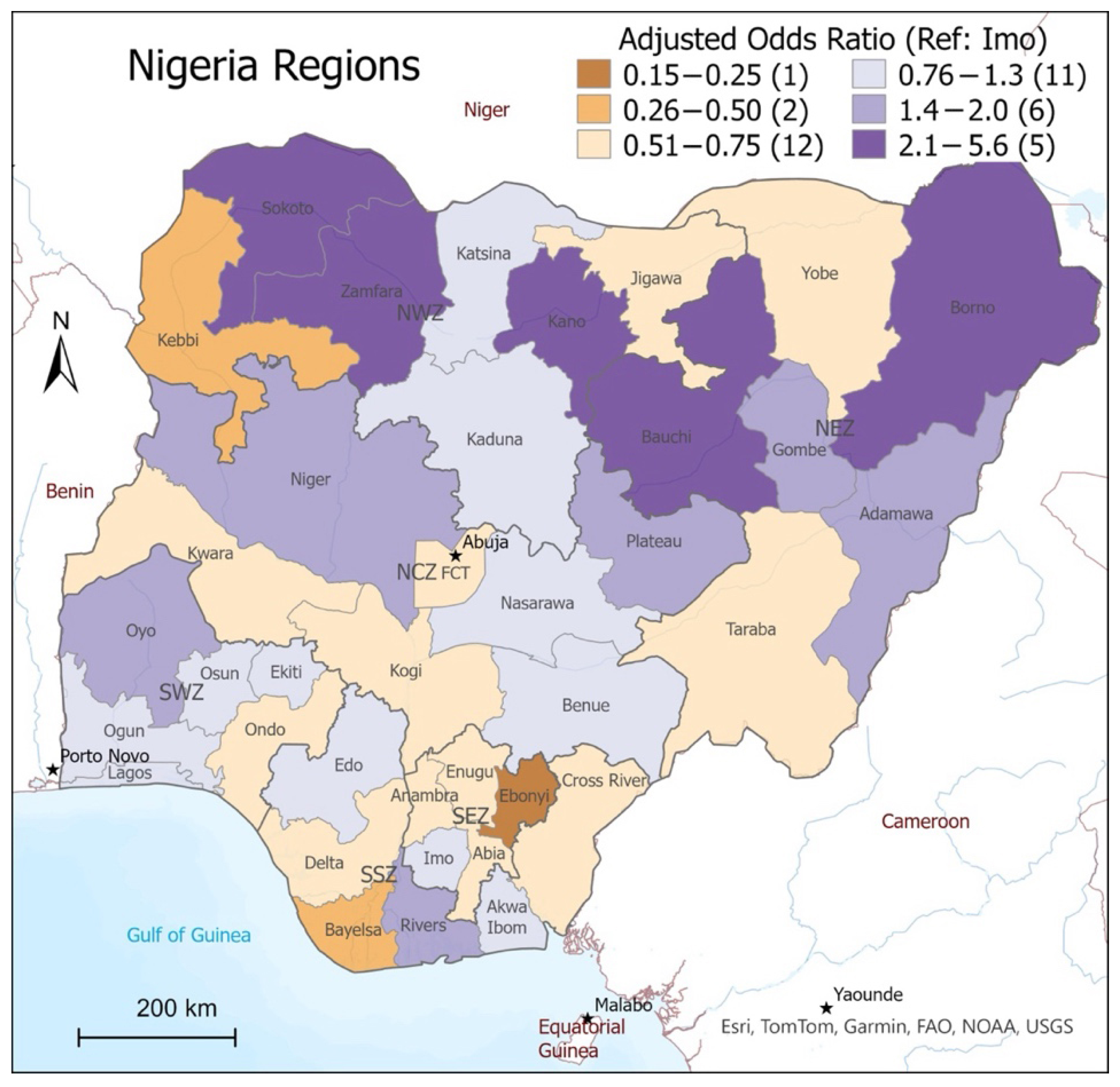
| Region | |||||
| Imo (ref) | <0.001 * | ||||
| Abia | −0.481 | 0.034 * | 0.618 | 0.396 | 0.964 |
| Adamawa | 0.685 | 0.024 * | 1.984 | 1.092 | 3.602 |
| Akwa Ibom | 0.004 | 0.990 | 1.004 | 0.568 | 1.774 |
| Anambra | −0.677 | 0.001 * | 0.508 | 0.339 | 0.762 |
| Bauchi | 1.224 | <0.001 * | 3.400 | 1.906 | 6.063 |
| Bayelsa | −1.263 | <0.001 * | 0.283 | 0.135 | 0.592 |
| Benue | −0.085 | 0.798 | 0.918 | 0.478 | 1.762 |
| Borno | 0.864 | 0.006 * | 2.372 | 1.277 | 4.404 |
| Cross River | −0.651 | 0.017 * | 0.522 | 0.305 | 0.892 |
| Delta | −0.546 | 0.040 * | 0.580 | 0.344 | 0.976 |
| Ebonyi | −1.882 | <0.001 * | 0.152 | 0.092 | 0.251 |
| Edo | −0.137 | 0.646 | 0.872 | 0.485 | 1.567 |
| Ekiti | −0.251 | 0.390 | 0.778 | 0.438 | 1.380 |
| Enugu | −0.393 | 0.097 | 0.675 | 0.425 | 1.074 |
| Gombe | 0.654 | 0.037 * | 1.924 | 1.039 | 3.564 |
| Jigawa | −0.497 | 0.065 | 0.608 | 0.358 | 1.032 |
| Kaduna | 0.180 | 0.498 | 1.198 | 0.710 | 2.019 |
| Kano | 1.060 | <0.001 * | 2.885 | 1.695 | 4.913 |
| Katsina | −0.090 | 0.732 | 0.914 | 0.545 | 1.532 |
| Kebbi | −1.126 | <0.001 * | 0.324 | 0.193 | 0.545 |
| Kogi | −0.550 | 0.050 | 0.577 | 0.329 | 1.012 |
| Kwara | −0.686 | 0.025 * | 0.504 | 0.276 | 0.918 |
| Lagos | −0.154 | 0.51 | 0.857 | 0.543 | 1.355 |
| Nasarawa | 0.200 | 0.530 | 1.222 | 0.654 | 2.282 |
| Niger | 0.692 | 0.013 * | 1.998 | 1.154 | 3.457 |
| Ogun | 0.197 | 0.465 | 1.217 | 0.719 | 2.062 |
| Ondo | −0.575 | 0.039 * | 0.563 | 0.326 | 0.971 |
| Osun | −0.188 | 0.516 | 0.829 | 0.471 | 1.460 |
| Oyo | 0.401 | 0.150 | 1.493 | 0.865 | 2.577 |
| Plateau | 0.635 | 0.032 * | 1.887 | 1.055 | 3.376 |
| Rivers | 0.482 | 0.077 | 1.619 | 0.949 | 2.763 |
| Sokoto | 1.727 | <0.001 * | 5.626 | 2.719 | 11.644 |
| Taraba | −0.496 | 0.074 | 0.609 | 0.353 | 1.050 |
| Yobe | −0.479 | 0.099 | 0.619 | 0.350 | 1.094 |
| Zamfara | 1.105 | <0.001 * | 3.019 | 1.574 | 5.790 |
| FCT | −0.419 | 0.154 | 0.658 | 0.370 | 1.169 |
| Age | |||||
| 15–19 (ref) | <0.001 * | ||||
| 20–24 | 0.100 | 0.622 | 1.105 | 0.743 | 1.642 |
| 25–29 | 0.009 | 0.963 | 1.009 | 0.685 | 1.486 |
| 30–34 | −0.293 | 0.139 | 0.746 | 0.506 | 1.100 |
| 35–39 | −0.046 | 0.817 | 0.955 | 0.644 | 1.416 |
| 40–44 | −0.032 | 0.879 | 0.969 | 0.643 | 1.459 |
| 45–49 | −0.011 | 0.961 | 0.989 | 0.631 | 1.551 |
| Mother’s education | |||||
| None (ref) | <0.001 * | ||||
| Primary | −0.193 | 0.033 * | 0.824 | 0.690 | 0.984 |
| Junior secondary | −0.213 | 0.075 | 0.809 | 0.640 | 1.022 |
| Senior secondary | −0.432 | <0.001 * | 0.649 | 0.540 | 0.780 |
| Higher/tertiary | −0.558 | <0.001 * | 0.573 | 0.447 | 0.734 |
| Ethnicity of household head | |||||
| Tiv (ref) | 0.036 * | ||||
| Hausa | 0.092 | 0.749 | 1.096 | 0.624 | 1.925 |
| Igbo | −0.142 | 0.642 | 0.867 | 0.476 | 1.580 |
| Yoruba | −0.314 | 0.287 | 0.731 | 0.410 | 1.302 |
| Fulani | −0.198 | 0.503 | 0.820 | 0.459 | 1.465 |
| Kanuri | −0.268 | 0.428 | 0.765 | 0.394 | 1.485 |
| Ijaw | 0.282 | 0.467 | 1.326 | 0.620 | 2.837 |
| Ibibio | −0.368 | 0.272 | 0.692 | 0.359 | 1.334 |
| Edo | −0.417 | 0.248 | 0.659 | 0.325 | 1.336 |
| Other ethnicity | −0.165 | 0.544 | 0.848 | 0.498 | 1.445 |
| Wealth index quintile | |||||
| Poorest (ref) | 0.439 | ||||
| Second | −0.088 | 0.303 | 0.915 | 0.774 | 1.083 |
| Middle | −0.121 | 0.218 | 0.886 | 0.731 | 1.074 |
| Fourth | −0.190 | 0.108 | 0.827 | 0.656 | 1.043 |
| Richest | −0.269 | 0.056 | 0.764 | 0.580 | 1.007 |
| Mothers’ Media Access Variables | |||||
| Ever Read a Newspaper/Magazine | |||||
| No | |||||
| Yes | −0.050 | 0.520 | 0.951 | 0.817 | 1.108 |
| Ever Listened to Radio | |||||
| No | |||||
| Yes | 0.031 | 0.631 | 1.031 | 0.909 | 1.170 |
| Ever Watched Television | |||||
| No | |||||
| Yes | −0.452 | <0.001 * | 0.636 | 0.529 | 0.765 |
| Ever Used Internet | |||||
| No | |||||
| Yes | 0.101 | 0.223 | 1.107 | 0.940 | 1.302 |
| Own a Mobile Phone | |||||
| Yes | |||||
| No | 0.144 | 0.034 * | 1.155 | 1.011 | 1.320 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gordon, C.; Paslawski, T.; Bandara, T.; Floer, S.; Shah, T. A Quantitative Exploration of the Relationship Between Healthcare Accessibility and Mass Media in Nigeria Using the Levesque Framework of Healthcare Access. Vaccines 2025, 13, 981. https://doi.org/10.3390/vaccines13090981
Gordon C, Paslawski T, Bandara T, Floer S, Shah T. A Quantitative Exploration of the Relationship Between Healthcare Accessibility and Mass Media in Nigeria Using the Levesque Framework of Healthcare Access. Vaccines. 2025; 13(9):981. https://doi.org/10.3390/vaccines13090981
Chicago/Turabian StyleGordon, Chelsea, Teresa Paslawski, Thilina Bandara, Shannon Floer, and Tayyab Shah. 2025. "A Quantitative Exploration of the Relationship Between Healthcare Accessibility and Mass Media in Nigeria Using the Levesque Framework of Healthcare Access" Vaccines 13, no. 9: 981. https://doi.org/10.3390/vaccines13090981
APA StyleGordon, C., Paslawski, T., Bandara, T., Floer, S., & Shah, T. (2025). A Quantitative Exploration of the Relationship Between Healthcare Accessibility and Mass Media in Nigeria Using the Levesque Framework of Healthcare Access. Vaccines, 13(9), 981. https://doi.org/10.3390/vaccines13090981












