Trust in Information Sources and Parents’ Knowledge, Attitudes, and Practices (KAP) of Children’s PCV13 Vaccination in the Yangtze River Delta Region, China
Abstract
1. Introduction
2. Materials and Methods
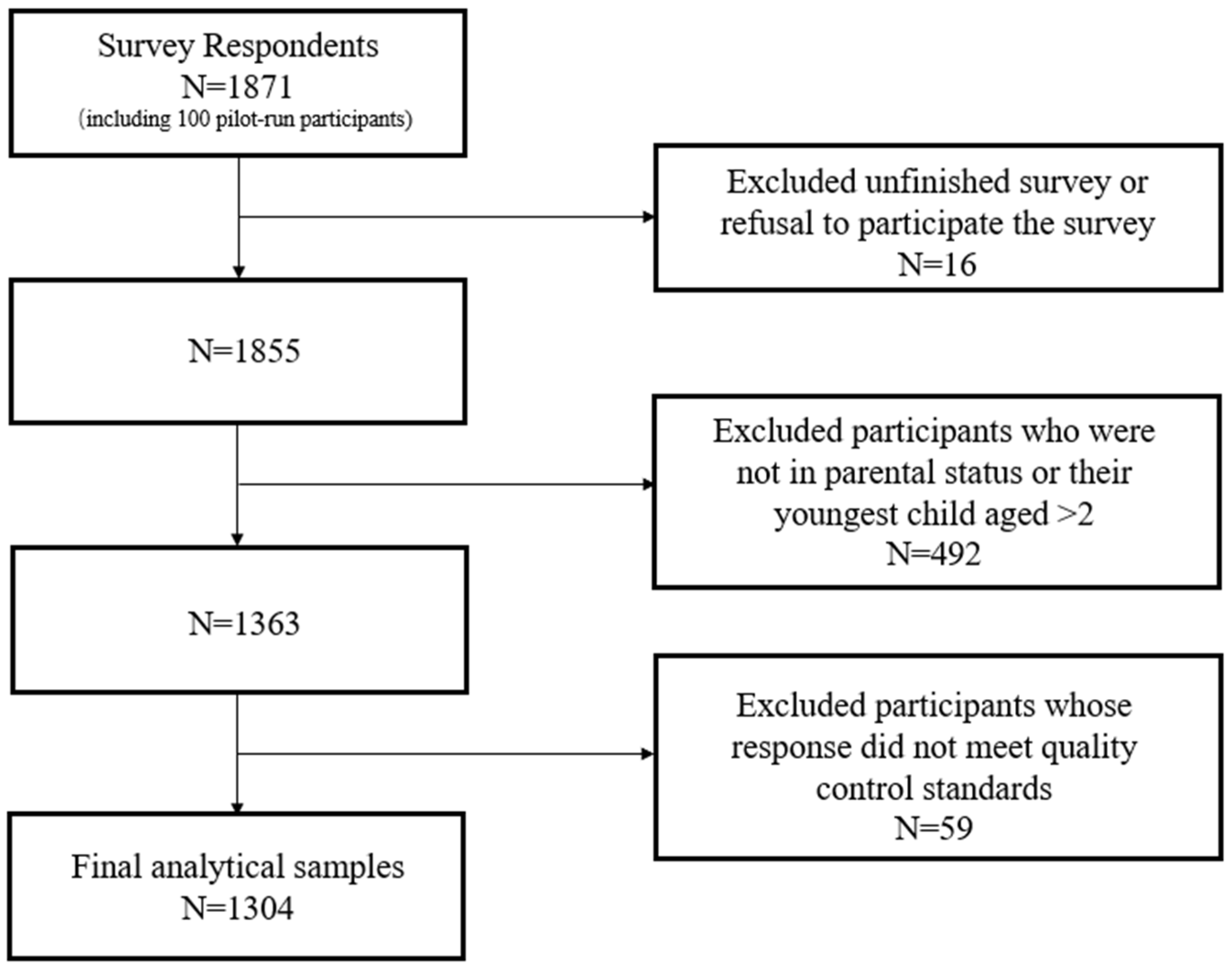
2.1. Study Setting and Sample
2.2. Data Collection
2.3. Measurement
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CDC | Center of Disease Control and Prevention |
| IPD | Invasive pneumococcal disease(s) |
| KAP | Knowledge, attitudes, and practices |
| NIP | National Immunization Program |
| OLS | Ordinary Least Square |
| PCV | Pneumococcal conjugate vaccine |
| UAE | United Arab Emirates |
| YRD | Yangtze River Delta |
References
- O’Brien, K.L.; Wolfson, L.J.; Watt, J.P.; Henkle, E.; Deloria-Knoll, M.; McCall, N.; Lee, E.; Mulholland, K.; Levine, O.S.; Cherian, T. Burden of Disease Caused by Streptococcus Pneumoniae in Children Younger than 5 Years: Global Estimates. Lancet 2009, 374, 893–902. [Google Scholar] [CrossRef]
- Lai, X.; Wahl, B.; Yu, W.; Xu, T.; Zhang, H.; Garcia, C.; Qin, Y.; Guo, Y.; Yin, Z.; Knoll, M.D.; et al. National, Regional, and Provincial Disease Burden Attributed to Streptococcus Pneumoniae and Haemophilus Influenzae Type b in Children in China: Modelled Estimates for 2010–17. Lancet Reg. Health West. Pac. 2022, 22, 100430. [Google Scholar] [CrossRef] [PubMed]
- Immunization, Vaccines and Biologicals (IVB). Table 1: Summary of WHO Position Papers—Recommendations for Routine Immunization 2024. Available online: https://cdn.who.int/media/docs/default-source/immunization/immunization_schedules/table_1_april_2024_english.pdf?sfvrsn=2e112cea_2&download=true (accessed on 8 September 2024).
- Versluys, K.A.; Eurich, D.T.; Marrie, T.J.; Forgie, S.; Tyrrell, G.J. Invasive Pneumococcal Disease and Long-Term Outcomes in Children: A 20-Year Population Cohort Study. Lancet Reg. Health Am. 2022, 14, 100341. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Zhang, Z.; Zhang, X.; Xu, C.; Song, Y.; Li, L.; Ye, J.; Wang, Z.; Liang, H.; Zhang, W.; et al. Coverage of 13-Valent Pneumococcal Conjugate Vaccine Among Children 0–15 Months of Age—9 Provinces, China, 2019–2021. China CDC Wkly. 2023, 5, 379–384. [Google Scholar] [CrossRef]
- Jiang, M.; Chen, S.; Yan, X.; Ying, X.; Tang, S. The Coverage and Challenges of Increasing Uptake of Non-National Immunization Program Vaccines in China: A Scoping Review. Infect. Dis. Poverty 2023, 12, 114. [Google Scholar] [CrossRef]
- Larson, H. Stuck: How Vaccine Rumors—and Why They Don’t Go Away; Oxford University Press: New York, NY, USA, 2020; ISBN 978-0-19-007724-2. [Google Scholar]
- Berlo, D.K.; Lemert, J.B.; Mertz, R.J. Dimensions for Evaluating the Acceptability of Message Sources. Public Opin. Q. 1969, 33, 563. [Google Scholar] [CrossRef]
- Ni, Y.; Xu, Z.; Wang, J. Understanding Vaccine Hesitancy with PCV13 in Children: Results of a Survey in Shanghai, China. PLoS ONE 2023, 18, e0284810. [Google Scholar] [CrossRef]
- Luo, Y.-F.; Chen, L.-C.; Yang, S.-C.; Hong, S. Knowledge, Attitude, and Practice (KAP) toward COVID-19 Pandemic among the Public in Taiwan: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 2784. [Google Scholar] [CrossRef]
- Clayman, M.L.; Manganello, J.A.; Viswanath, K.; Hesse, B.W.; Arora, N.K. Providing Health Messages to Hispanics/Latinos: Understanding the Importance of Language, Trust in Health Information Sources, and Media Use. J. Health Commun. 2010, 15, 252–263. [Google Scholar] [CrossRef]
- Fridman, I.; Lucas, N.; Henke, D.; Zigler, C.K. Association Between Public Knowledge About COVID-19, Trust in Information Sources, and Adherence to Social Distancing: Cross-Sectional Survey. JMIR Public Health Surveill. 2020, 6, e22060. [Google Scholar] [CrossRef]
- Ashkenazi, S.; Livni, G.; Klein, A.; Kremer, N.; Havlin, A.; Berkowitz, O. The Relationship between Parental Source of Information and Knowledge about Measles / Measles Vaccine and Vaccine Hesitancy. Vaccine 2020, 38, 7292–7298. [Google Scholar] [CrossRef]
- de La Cruz-Sánchez, E.; Moreno-Llamas, A.; Mendiola Olivares, J.; García-Mayor, J.; Torres-Cantero, A.; Devine, E.B. Association between Covid-19 Sources of Information, Beliefs, and Vaccination Rates: An EU-Wide Survey. Eur. J. Public Health 2023, 33, 897–904. [Google Scholar] [CrossRef]
- Li, K.; Zhou, F. Influence of Information Sources on Chinese Parents Regarding COVID-19 Vaccination for Children: An Online Survey. Int. J. Environ. Res. Public Health 2022, 19, 7037. [Google Scholar] [CrossRef] [PubMed]
- Osuagwu, U.L.; Mashige, K.P.; Ovenseri-Ogbomo, G.; Envuladu, E.A.; Abu, E.K.; Miner, C.A.; Timothy, C.G.; Ekpenyong, B.N.; Langsi, R.; Amiebenomo, O.M.; et al. The Impact of Information Sources on COVID-19 Vaccine Hesitancy and Resistance in Sub-Saharan Africa. BMC Public Health 2023, 23, 38. [Google Scholar] [CrossRef] [PubMed]
- Dong, Y.; Yang, X.; Zhang, X.; Jiang, J. ‘They Are Conspiring against Us’: How Outgroup Conspiracy Theories Stimulate Environmental Neglect in Intergroup Resource Dilemmas. Br. J. Soc. Psychol. 2024, 63, 1856–1878. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhang, Y. Organizational Appeals and Civic Voluntarism. Asian Surv. 2024, 64, 365–395. [Google Scholar] [CrossRef]
- Su, Z.; Li, Y.; Xie, Y.; Huang, Z.; Cheng, A.; Zhou, X.; Li, J.; Qin, R.; Wei, X.; Liu, Y.; et al. Acute and Long COVID-19 Symptoms and Associated Factors in the Omicron-Dominant Period: A Nationwide Survey via the Online Platform Wenjuanxing in China. BMC Public Health 2024, 24, 2086. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, R.; Liu, J.; Xu, R.; Zhao, L.; Li, E.; Zhang, Y. An Online Survey on Public Awareness of Drug Clinical Trials in Inland Cities of Northern China. Front. Public Health 2024, 12, 1276536. [Google Scholar] [CrossRef]
- Chinadaily.com.cn. Brief Introduction to Yangtze River Delta—Regional. China Daily. Available online: http://www.chinadaily.com.cn/regional/2020-06/01/content_37536491.htm (accessed on 29 October 2023).
- Wang, J.; Wu, Q.; Lu, J.; Ni, Y.; Zhou, F. Low Vaccination Coverage of Pneumococcal Conjugate Vaccines (PCVs) in Shanghai, China: A Database Analysis Based on Birth Cohorts from 2012 to 2020. Vaccine 2021, 39, 6189–6194. [Google Scholar] [CrossRef]
- Hou, Z.; Chang, J.; Yue, D.; Fang, H.; Meng, Q.; Zhang, Y. Determinants of Willingness to Pay for Self-Paid Vaccines in China. Vaccine 2014, 32, 4471–4477. [Google Scholar] [CrossRef]
- Tung, T.-H.; Lin, X.-Q.; Chen, Y.; Wu, H.; Zhang, M.-X.; Zhu, J.-S. Why Do Parents Willingness-to-Pay to Vaccinate Their Children against COVID-19? A Real-World Evidence in Taizhou, China. Hum. Vaccines Immunother. 2022, 18, 1–9. [Google Scholar] [CrossRef]
- Wu, L.; Huang, Z.; Guo, X.; Liu, J.; Sun, X. Measuring Parents’ Acceptance of Non-National Immunization Program Vaccines for Children and Its Influencing Factors during the COVID-19 Pandemic in Shanghai, China. Hum. Vaccines Immunother. 2022, 18, 2069427. [Google Scholar] [CrossRef] [PubMed]
- Institute of Social Science Survey (ISSS). China Family Pannel Studies Questionnaires. 2020. Available online: https://www.isss.pku.edu.cn/cfps/docs/20230912155632775874.pdf (accessed on 8 September 2024).
- Chinese Preventive Medicine Association; Vaccine and Immunology Branch of the Chinese Preventive Medicine Association. [Expert Consensus on Immunoprophylaxis of Pneumococcal Disease (2020 Version)]. Zhonghua Liu Xing Bing Xue Za Zhi 2020, 41, 1945–1979. [Google Scholar] [CrossRef]
- Figueiras, M.J.; Ghorayeb, J.; Coutinho, M.V.C.; Marôco, J.; Thomas, J. Levels of Trust in Information Sources as a Predictor of Protective Health Behaviors During COVID-19 Pandemic: A UAE Cross-Sectional Study. Front. Psychol. 2021, 12, 633550. [Google Scholar] [CrossRef] [PubMed]
- Gao, H.; Zhao, Q.; Li, L.; Bai, X.; Guo, D. The Multi-Dimensional Impact of Different Sources of Information on Influenza Vaccination of College Students in China. J. Am. Coll. Health 2024, 72, 995–1000. [Google Scholar] [CrossRef]
- Goodson, B.; Larson, H. How to Build Trust in Vaccines: Understanding the Drivers of Vaccine Confidence. World Economic Forum. 2021. Available online: https://www.weforum.org/publications/how-to-build-trust-in-vaccines-understanding-the-drivers-of-vaccine-confidence/ (accessed on 29 October 2023).
- Liu, Y.; Li, X. Information Source, Media Credibility, and Epidemic Control in COVID-19 Pandemic. J. Emerg. Manag. Disaster Commun. 2021, 2, 81–99. [Google Scholar] [CrossRef]
- Castelfranchi, C.; Falcone, R. Principles of Trust for MAS: Cognitive Anatomy, Social Importance, and Quantification. In Proceedings of the International Conference on Multi Agent Systems (Cat. No.98EX160), Paris, France, 3–7 July 3 1998; pp. 72–79. [Google Scholar] [CrossRef]
- Freiman, O. Vaccine Hesitancy and the Concept of Trust: An Analysis Based on the Israeli COVID-19 Vaccination Campaign. Minerva 2023, 61, 357–381. [Google Scholar] [CrossRef]
- McLeod, C. Trust. In The Stanford Encyclopedia of Philosophy Archive; Fall 2023 Edition; Stanford Encyclopedia of Philosophy: Stanford, CA, USA, 2006. [Google Scholar]
- Faulkner, P. Collective Testimony and Collective Knowledge. Open Access J. Philos. 2018, 5, 20201214. [Google Scholar] [CrossRef]
- Lin, S.-Y.; Zhang, S.-Y.; Chantler, T.; Sun, F.Y.; Zou, J.-T.; Cheng, J.-J.; Chen, Y.-Q.; Sun, M.; Howard, N. Vaccination Coverage Determinants in Low Uptake Areas of China: A Qualitative Study of Provider Perspectives in Sichuan, Guangdong, and Henan Provinces. Hum. Vaccines Immunother. 2022, 18, 2030623. [Google Scholar] [CrossRef]
- Liu, T.-L.; Hsiao, R.C.; Chen, Y.-M.; Lin, P.-C.; Yen, C.-F. Sources of Information about COVID-19 Vaccines for Children and Its Associations with Parental Motivation to Have Their Children Vaccinated in Taiwan. Vaccines 2023, 11, 1337. [Google Scholar] [CrossRef]
- Du, F.; Chantler, T.; Francis, M.R.; Sun, F.Y.; Zhang, X.; Han, K.; Rodewald, L.; Yu, H.; Tu, S.; Larson, H.; et al. Access to Vaccination Information and Confidence/Hesitancy towards Childhood Vaccination: A Cross-Sectional Survey in China. Vaccines 2021, 9, 201. [Google Scholar] [CrossRef]
- Gehrau, V.; Fujarski, S.; Lorenz, H.; Schieb, C.; Blöbaum, B. The Impact of Health Information Exposure and Source Credibility on COVID-19 Vaccination Intention in Germany. Int. J. Environ. Res. Public Health 2021, 18, 4678. [Google Scholar] [CrossRef]
- Tian, J.; Zheng, B.; Yang, L.; Guan, Y.; Xu, C.; Wang, W. Effectiveness of 13-Valent Pneumococcal Conjugate Vaccine on All-Cause Pneumonia in Children under 5 Years in Shanghai, China: An Observational Study. Vaccine 2023, 41, 5979–5986. [Google Scholar] [CrossRef]
- Rowley, J.; Johnson, F.; Sbaffi, L. Gender as an Influencer of Online Health Information-seeking and Evaluation Behavior. J. Assoc. Inf. Sci. Technol. 2017, 68, 36–47. [Google Scholar] [CrossRef]
- Van Der Heide, I.; Wang, J.; Droomers, M.; Spreeuwenberg, P.; Rademakers, J.; Uiters, E. The Relationship Between Health, Education, and Health Literacy: Results From the Dutch Adult Literacy and Life Skills Survey. J. Health Commun. 2013, 18, 172–184. [Google Scholar] [CrossRef]
- Latkin, C.A.; Dayton, L.; Yi, G.; Konstantopoulos, A.; Boodram, B. Trust in a COVID-19 Vaccine in the U.S.: A Social-Ecological Perspective. Soc. Sci. Med. 2021, 270, 113684. [Google Scholar] [CrossRef]
- Lohmann, S.; Albarracín, D. Trust in the Public Health System as a Source of Information on Vaccination Matters Most When Environments Are Supportive. Vaccine 2022, 40, 4693–4699. [Google Scholar] [CrossRef]
- Maykrantz, S.A.; Gong, T.; Petrolino, A.V.; Nobiling, B.D.; Houghton, J.D. How Trust in Information Sources Influences Preventative Measures Compliance during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5867. [Google Scholar] [CrossRef]
- Tabacchi, G.; Costantino, C.; Cracchiolo, M.; Ferro, A.; Marchese, V.; Napoli, G.; Palmeri, S.; Raia, D.; Restivo, V.; Siddu, A.; et al. Information Sources and Knowledge on Vaccination in a Population from Southern Italy: The ESCULAPIO Project. Hum. Vaccines Immunother. 2017, 13, 339–345. [Google Scholar] [CrossRef]
- Ning, C.; Guo, D.; Wu, J.; Gao, H. Media Exposure and Media Credibility Influencing Public Intentions for Influenza Vaccination. Vaccines 2022, 10, 526. [Google Scholar] [CrossRef]

| Variable | N (%) | |
|---|---|---|
| Age | 18–24 | 79 (6.1%) |
| 25–34 | 1012 (77.6%) | |
| 35–45 | 171 (13.1%) | |
| >45 | 42 (3.2%) | |
| Gender | Female | 749 (57.4%) |
| Male | 555 (42.6%) | |
| Education attainment | Secondary school and below | 56 (4.3%) |
| High school and technical secondary school | 159 (12.2%) | |
| Junior college | 289 (22.2%) | |
| Bachelor’s degree | 719 (55.1%) | |
| Postgraduate and above | 81 (6.2%) | |
| Annual household income (Unit: CNY) | <20,000 | 0 (-) |
| 20,000 to 49,999 | 20 (1.5%) | |
| 50,000 to 99,999 | 230 (17.6%) | |
| 100,000 to 300,000 | 915 (70.2%) | |
| >300,000 | 139 (10.7%) | |
| Number of children | 1 | 922 (70.7%) |
| >1 | 382 (29.3%) |
| Category | Sources | Trust Level (Mean, SD) | Frequency |
|---|---|---|---|
| Medical institutions | CDC | 4.48 (0.71) | 497 |
| Vaccination clinics | 4.16 (0.81) | 712 | |
| Hospitals | 4.04 (0.82) | 625 | |
| Medical media | 3.68 (0.86) | 328 | |
| Official media | Official media | 4.18 (0.81) | 476 |
| Personal network | Family/friends | 3.63 (0.78) | 614 |
| Online community | Maternal Apps | 3.28 (0.91) | 358 |
| Online forum | 2.85 (0.89) | 431 | |
| Social media | 2.73 (0.88) | 198 |
| Trust in Different Information Source Categories | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variables | Medical Institutions | Official Media | Personal Network | Online Community | ||||
| SMD (β) | SE | SMD (β) | SE | SMD (β) | SE | SMD (β) | SE | |
| Constant | 4.03 *** | (0.13) | 3.90 *** | (0.18) | 2.82 *** | (0.16) | 2.98 *** | (0.17) |
| Age | −0.05 | (0.03) | −0.05 | (0.04) | −0.07 * | (0.04) | 0.04 | (0.04) |
| Male | −0.06 | (0.03) | 0.04 | (0.05) | −0.17 *** | (0.04) | −0.16 *** | (0.04) |
| Annual household income | 0.03 | (0.03) | 0.04 | (0.04) | 0.01 | (0.04) | 0.10 * | (0.04) |
| Education | 0.03 | (0.02) | 0.06 * | (0.03) | 0.09 *** | (0.02) | 0.08 ** | (0.02) |
| Number of children | −0.02 | (0.04) | 0.05 | (0.05) | 0.01 | (0.05) | −0.02 | (0.05) |
| R2 | 0.01 | 0.01 | 0.03 | 0.03 | ||||
| Knowledge | Vaccine Hesitancy | Vaccine Uptake | |||||
|---|---|---|---|---|---|---|---|
| SMD (β) | SE | SMD (β) | SE | SMD (β) | SE | ||
| Constant | 1.94 *** | (0.01) | 4.67 *** | (0.35) | 2.58 *** | (0.38) | |
| Predictors | Medical institutions | 0.08 *** | (0.02) | −0.49 *** | (0.07) | 0.24 ** | (0.07) |
| Official media | 0.01 | (0.01) | 0.07 | (0.05) | −0.11 ** | (0.05) | |
| Personal network | −0.01 | (0.01) | −0.03 | (0.05) | 0.02 | (0.05) | |
| Online community | 0.02 | (0.01) | −0.05 | (0.05) | 0.21 *** | (0.06) | |
| Covariates | Age | 0.01 | (0.02) | 0.11 | (0.06) | −0.22 *** | (0.06) |
| Male | −0.08 *** | (0.02) | 0.03 | (0.07) | 0.23 ** | (0.07) | |
| Annual household income | 0.02 | (0.04) | −0.03 | (0.06) | 0.01 | (0.07) | |
| Education | 0.01 | (0.01) | −0.08 * | (0.04) | 0.08 * | (0.04) | |
| Number of children | 0.02 | (0.02) | 0.09 | (0.07) | 0.03 | (0.08) | |
| R2 | 0.05 | 0.08 | 0.05 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pan, Z.; Liang, F.; Tang, S. Trust in Information Sources and Parents’ Knowledge, Attitudes, and Practices (KAP) of Children’s PCV13 Vaccination in the Yangtze River Delta Region, China. Vaccines 2025, 13, 947. https://doi.org/10.3390/vaccines13090947
Pan Z, Liang F, Tang S. Trust in Information Sources and Parents’ Knowledge, Attitudes, and Practices (KAP) of Children’s PCV13 Vaccination in the Yangtze River Delta Region, China. Vaccines. 2025; 13(9):947. https://doi.org/10.3390/vaccines13090947
Chicago/Turabian StylePan, Zhangyang, Fan Liang, and Shenglan Tang. 2025. "Trust in Information Sources and Parents’ Knowledge, Attitudes, and Practices (KAP) of Children’s PCV13 Vaccination in the Yangtze River Delta Region, China" Vaccines 13, no. 9: 947. https://doi.org/10.3390/vaccines13090947
APA StylePan, Z., Liang, F., & Tang, S. (2025). Trust in Information Sources and Parents’ Knowledge, Attitudes, and Practices (KAP) of Children’s PCV13 Vaccination in the Yangtze River Delta Region, China. Vaccines, 13(9), 947. https://doi.org/10.3390/vaccines13090947





