Measles Epidemiology and Coverage of Immunization Against Measles in the Autonomous Province of Vojvodina, Serbia: Local Trends in a Regional Context
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Data Collection and Variables
- Annual measles incidence rate: Number of reported cases per 100,000 population per year in AP Vojvodina.
- Age-specific measles incidence rate: Number of reported cases per 100,000 population within specific age groups in AP Vojvodina.
- MCV I (MMR I) coverage: Annual percentage of the target population (at 12–15 months) receiving the first dose of vaccine against measles.
- MCV II (MMR II) coverage: Annual percentage of the target population (at 12 years in the period 1994–2005; at 6–7 years in the period 2006–2024) receiving the second dose of vaccine against measles.
2.3. Data Analysis
2.4. Ethical Considerations
3. Results
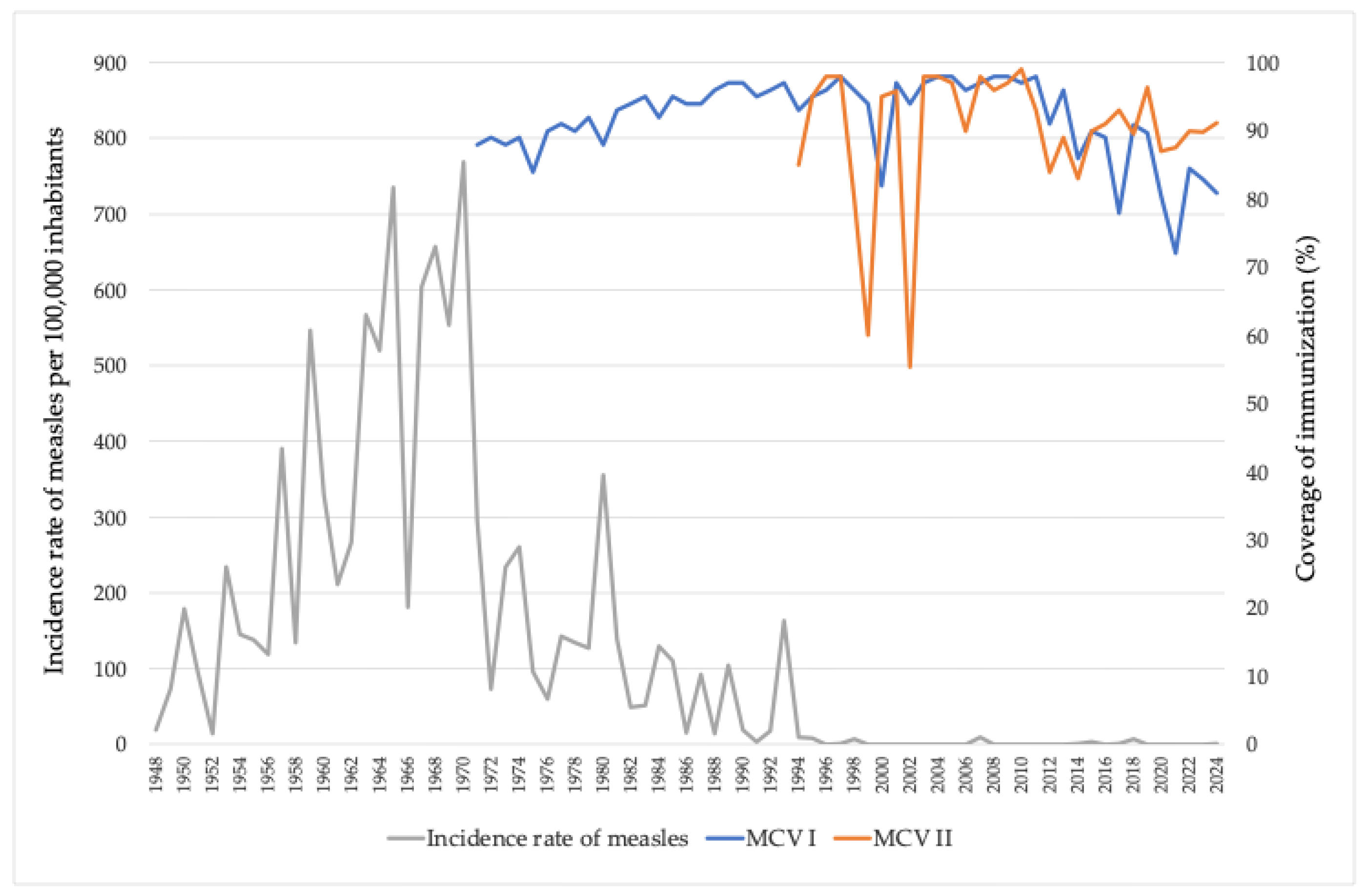
3.1. Trends in Measles Incidence and MCV Coverage in AP Vojvodina, 1948–2024
3.2. MMR Vaccination Coverage and Measles Incidence Across the Districts of AP Vojvodina, 2000–2024
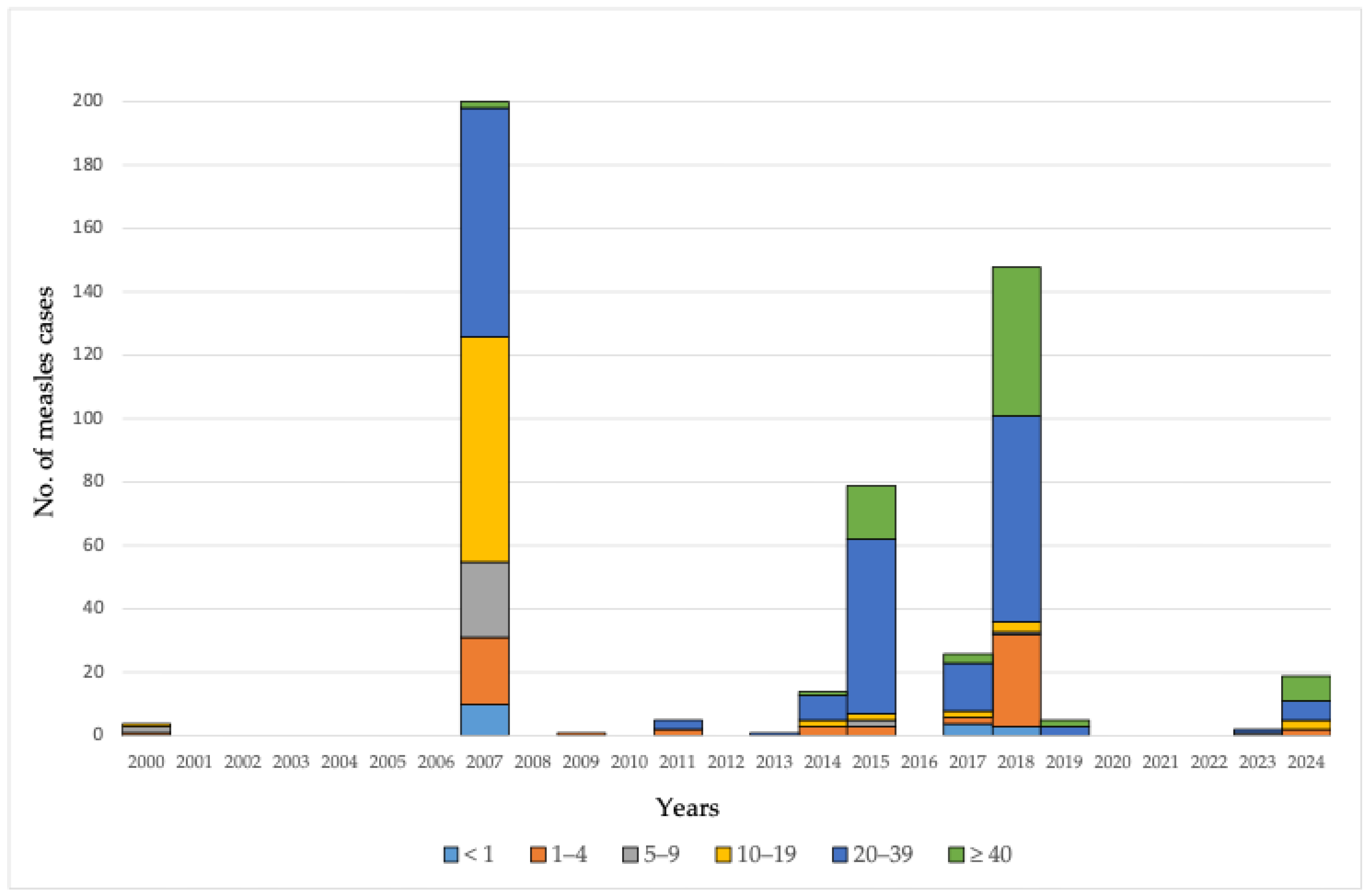
3.3. Measles Cases by Age Groups in AP Vojvodina, 2000–2024

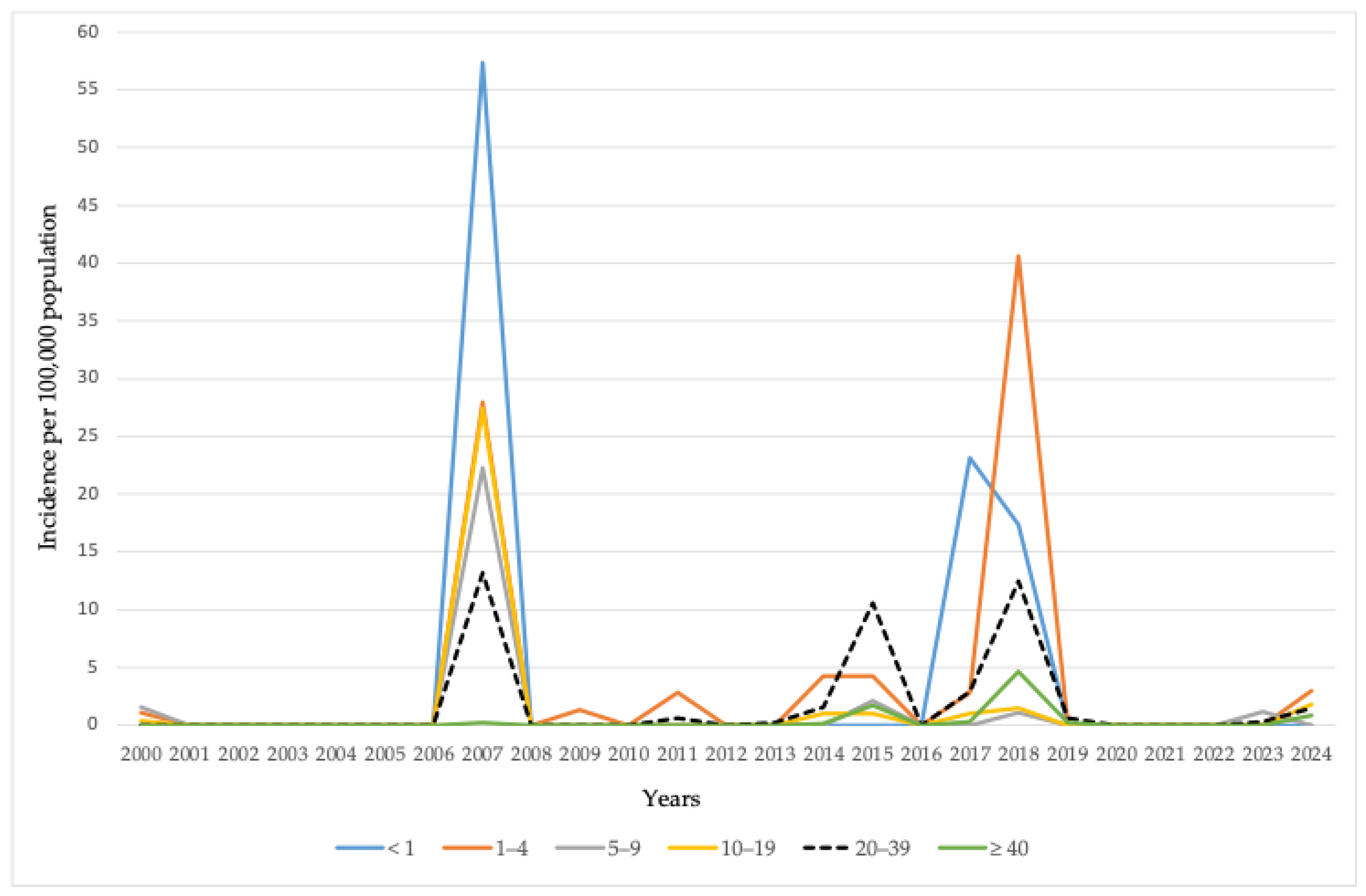
3.4. Incidence Rates of Measles by Age Groups in AP Vojvodina, 2000–2024
3.5. Measles Cases by Age Group and Vaccination Status Against Measles in AP Vojvodina, 2000–2024
4. Discussion
4.1. Regional Measles Epidemiology and Vaccination Coverage
4.2. Measles Notification and Introduction of Immunization
4.3. Measles Outbreaks in Serbia and Neighboring Countries Between 2000 and 2023
4.4. Measles Outbreaks in AP Vojvodina Between 2000 and 2024
4.5. Factors Potentially Associated with the Decline in Measles Immunization Coverage
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Measles and Rubella Surveillance Data. WHO Regional Office for Europe. Immunization Analysis and Insights. Available online: https://www.who.int/teams/immunization-vaccines-and-biologicals/immunization-analysis-and-insights/surveillance/monitoring/provisional-monthly-measles-and-rubella-data (accessed on 1 June 2025).
- Hübschen, J.M.; Bork, S.M.; Brown, K.E.; Mankertz, A.; Santibanez, S.; Ben-Mamou, M.; Mulders, M.N.; Muller, C.P. Challenges of measles and rubella laboratory diagnostic in the era of elimination. Clin. Microbiol. Infect. 2017, 23, 511–515. [Google Scholar] [CrossRef] [PubMed]
- European Centre for Disease Prevention and Control (ECDC). Measles Annual Epidemiological Reports. Available online: https://www.ecdc.europa.eu/sites/default/files/documents/MEAS-AER-2024-Report.pdf (accessed on 1 June 2025).
- World Health Organization. Measles Vaccines: WHO Position Paper, April 2017—Recommendations. Vaccine 2019, 37, 219–222. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Immunization Dashboard. Available online: https://immunizationdata.who.int/ (accessed on 30 May 2025).
- Perry, R.T.; Gacic-Dobo, M.; Dabbagh, A.; Mulders, M.N.; Strebel, P.M.; Okwo-Bele, J.M.; Rota, P.A.; Goodson, J.L. Centers for Disease Control and Prevention (CDC). Progress toward regional measles elimination--worldwide, 2000–2013. MMWR Morb. Mortal. Wkly. Rep. 2014, 63, 1034–1038. [Google Scholar] [PubMed] [PubMed Central]
- Muscat, M.; Ben-Mamou, M.; Reynen-de Kat, C.; Jankovic, D.; Hagan, J.; Singh, S.; Datta, S.S. Progress and Challenges in Measles and Rubella Elimination in the WHO European Region. Vaccines 2024, 12, 696. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Institute of Public Health of Vojvodina. Communicable Diseases in Vojvodina, 2017. Annual Report; Institute of Public Health of Vojvodina: Novi Sad, Serbia, 2018; pp. 26–30. (In Serbian) [Google Scholar]
- World Health Organization. Immunization Coverage. Department for Vaccines and Biologicals, Immunization, Surveillance and Monitoring System. Available online: https://www.who.int/immunization/monitoring_surveillance/routine/coverage/en/ (accessed on 1 June 2025).
- Çomo, N.; Meta, E.; Qato, M.; Kraja, D.; Pipero, P.; Fico, A. Measles, a re-emerging disease in Albania: Epidemiology and clinical presentations. SEEJPH 2022, 17. [Google Scholar] [CrossRef]
- Musa, S.; Salimović-Bešić, I.; Džambić, J.B.; Tihić, N.; Bajramović, A.; Arapčić, S.; Dedeić-Ljubović, A.; Skočibušić, S. Ongoing measles outbreak, the Federation of Bosnia and Herzegovina, December 2023 to February 2024. Euro Surveill. 2024, 29, 2400107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Muscat, M.; Marinova, L.; Mankertz, A.; Gatcheva, N.; Mihneva, Z.; Santibanez, S.; Kunchev, A.; Filipova, R.; Kojouharova, M. The measles outbreak in Bulgaria, 2009–2011: An epidemiological assessment and lessons learnt. Euro Surveill. 2016, 21, 30152. [Google Scholar] [CrossRef] [PubMed]
- Brzovic, M.; Barac-Juretic, K.; Jurcev-Savicevic, A.; Mihojevic, L.; Nonkovic, D.; Rizvan, P.; Vujevic-Petrovic, M.; Tonkic, M.; Kaic, B.; Babic-Erceg, A.; et al. Measles cases in Split-Dalmatia County (a Croatian tourist region), in May-July 2019: Outbreak report and lessons learnt. Eur. J. Public Health 2022, 32, 948–954. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Drenjančević, I.; Samardžić, S.; Stupin, A.; Borocz, K.; Nemeth, P.; Berki, T. Measles Vaccination and Outbreaks in Croatia from 2001 to 2019; A Comparative Study to Other European Countries. Int. J. Environ. Res. Public Health 2022, 19, 4140. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kaić, B.; Tešović, G. Measles outbreak: A warning sign of troubles ahead. Croat. Med. J. 2019, 60, 393–396. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Orosz, L.; Gáspár, G.; Rózsa, Á.; Rákos, N.; Sziveri, S.; Bosnyákovits, T. Epidemiological situation of measles in Romania, Italy, and Hungary: On what threats should we focus nowadays? Acta Microbiol. Immunol. Hung. 2018, 65, 127–134. [Google Scholar] [CrossRef] [PubMed]
- Lengyel, G.; Marossy, A.; Ánosi, N.; Farkas, S.L.; Kele, B.; Nemes-Nikodém, É.; Szentgyörgyi, V.; Kopcsó, I.; Mátyus, M. Screening of more than 2000 Hungarian healthcare workers’ anti-measles antibody level: Results and possible population-level consequences. Epidemiol. Infect. 2018, 147, e7. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mugoša, B.; Ceccarelli, G.; Begić, S.; Vujošević, D.; Zekovic, Z.; Ciccozzi, M.; Vratnica, Z. Measles outbreak, Montenegro January-July 2018: Lessons learned. J. Med. Virol. 2022, 94, 514–520. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kondova, I.T.; Milenkovic, Z.; Marinkovic, S.P.; Bosevska, G.; Kuzmanovska, G.; Kondov, G.; Alabakovska, S.; Muller, C.P.; Hübschen, J.M. Measles outbreak in Macedonia: Epidemiological, clinical and laboratory findings and identification of susceptible cohorts. PLoS ONE 2013, 8, e74754. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- IFRC GO. Over 1285 Cases of Measels and 5 Dead in Measels Outbrake in Republic of North Macedonia. Report Date: 2019-05-06. Available online: https://go.ifrc.org/field-reports/11793 (accessed on 4 April 2025).[Green Version]
- Kriss, J.L.; Stanescu, A.; Pistol, A.; Butu, C.; Goodson, J.L. The World Health Organization Measles Programmatic Risk Assessment Tool-Romania, 2015. Risk Anal. 2017, 37, 1096–1107. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pițigoi, D.; Săndulescu, O.; Crăciun, M.D.; Drăgănescu, A.; Jugulete, G.; Streinu-Cercel, A.; Vișan, A.; Rîciu, C.; Rafila, A.; Aramă, V.; et al. Measles in Romania—Clinical and epidemiological characteristics of hospitalized measles cases during the first three years of the 2016-ongoing epidemic. Virulence 2020, 11, 686–694. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lazar, M.; Pascu, C.; Roșca, M.; Stănescu, A. Ongoing measles outbreaks in Romania, March 2023 to August 2023. Euro Surveill. 2023, 28, 2300423. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nedeljković, J.; Rakić-Adrović, S.; Tasić, G.; Kovačević-Jovanović, V.; Lončarević, G.; Hübschen, J.M.; Muller, C.P. Resurgence of measles in Serbia 2010-2011 highlights the need for supplementary immunization activities. Epidemiol. Infect. 2016, 144, 1121–1128. [Google Scholar] [CrossRef] [PubMed]
- Medić, S.; Petrović, V.; Lončarević, G.; Kanazir, M.; Begović-Lazarević, I.; Rakić-Adrović, S.; Bančević, M.; Muller, C.P.; Hübschen, J.M. Epidemiological, clinical and laboratory characteristics of the measles resurgence in the Republic of Serbia in 2014–2015. PLoS ONE 2019, 14, e0224009. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Institut za Javno Zdravlje Srbije “Dr Milan Jovanović Batut”. Aktuelna Epidemiološka Situacija Malih Boginja (Morbila) u Republici Srbiji. 23.08.2019. (In Serbian). Available online: https://www.batut.org.rs/index.php?content=1629 (accessed on 10 April 2025).
- Burgess, C.; Lisul, B.; Pawaskar, M.; Petigara, T.; Murtagh, J.; Kanazir, M.; Loncarevic, G.; Carias, C. Impact of the COVID-19 Pandemic on Measles Vaccination Coverage and Estimated Catch-up Efforts for Serbia. Pediatr. Infect. Dis. J. 2024, 43, 1011–1017. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- World Health Organization. 50th Anniversary of the Expanded Programme on Immunization (EPI). Available online: https://www.who.int/news-room/events/detail/2024/01/01/default-calendar/50th-anniversary-of-the-expanded-programme-on-immunization-(epi) (accessed on 5 June 2025).
- Seguliev, Z.; Duric, P.; Petrovic, V.; Stefanovic, S.; Cosic, G.; Hrnjakovic, I.C.; Milosevic, V.; Karagiannis, I.; Boxall, N.; Jankovic, D. Current measles outbreak in Serbia: A preliminary report. Euro Surveill. 2007, 12, E070315.2. [Google Scholar] [CrossRef] [PubMed]
- Mankertz, A.; Mihneva, Z.; Gold, H.; Baumgarte, S.; Baillot, A.; Helble, R.; Roggendorf, H.; Bosevska, G.; Nedeljkovic, J.; Makowka, A.; et al. Spread of measles virus D4-Hamburg, Europe, 2008–2011. Emerg. Infect. Dis. 2011, 17, 1396–1401. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ristić, M.; Milošević, V.; Medić, S.; Djekić-Malbaša, J.; Rajčević, S.; Boban, J.; Petrović, V. Sero-epidemiological study in prediction of the risk groups for measles outbreaks in Vojvodina, Serbia. PLoS ONE 2019, 14, e0216219. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Aritonovic-Pribakovic, J.; Katanic, N.; Ilic, A.; Stojanovic-Tasic, M.; Mitic, N.R.; Mirkovic, M.; Radomirovic, D.; Milentijevic, M.; Mirkovic, M.; Katanic, R. The measles epidemic in northern Kosovo and Metohija, Serbia, October 2017–August 2019. J. Infect. Dev. Ctries. 2022, 16, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Dnevnik. Dopunska Vakcinacija Zaustavila Male Boginje. 2018. Available online: https://www.dnevnik.rs/drustvo/dopunska-vakcinacija-zaustavila-male-bogine-05-01-2019 (accessed on 30 April 2025). (In Serbian).
- Blic. Vojvodina Stvorila Epidemiološki Bedem za Male Boginje. 2018. Available online: https://www.blic.rs/vesti/vojvodina/pokrajinski-sekretar-vojvodina-stvorila-epidemioloski-bedem-za-maleboginje/m97sscl (accessed on 30 April 2025). (In Serbian).
- World Health Organization, Regional Office for E. European Immunization Agenda 2030. World Health Organization. Regional Office for Europe: Copenhagen, Denmark. 2021. Available online: https://www.who.int/europe/initiatives/the-european-immunization-agenda-2030 (accessed on 7 April 2025).
- Wilder-Smith, A.B.; Qureshi, K. Resurgence of Measles in Europe: A Systematic Review on Parental Attitudes and Beliefs of Measles Vaccine. J. Epidemiol. Glob. Health 2020, 10, 46–58. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Radovanović, Z. Anti-vaccinationists and their arguments in the Balkan countries that share the same language. Srp. Arh. Za Celok. Lek. 2017, 145, 199–204. [Google Scholar] [CrossRef]
- Čekanac, R. Significance of immunization for public health. Vojnosanit. Pregl. 2015, 72, 395–396. [Google Scholar] [CrossRef]
- Dowdle, W.R. The principles of disease elimination and eradication. Bull. World Health Organ. 1998, 76 (Suppl. S2), 22–25. [Google Scholar] [PubMed] [PubMed Central]
- Haverkate, M.; D’Ancona, F.; Giambi, C.; Johansen, K.; Lopalco, P.L.; Cozza, V.; Appelgren, E. VENICE project gatekeepers and contact points. Mandatory and recommended vaccination in the EU, Iceland and Norway: Results of the VENICE 2010 survey on the ways of implementing national vaccination programmes. Euro Surveill. 2012, 17, 20183. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ristić, M.; Ilić, S.; Rajčević, S.; Štrbac, M.; Medić, S.; Pustahija, T.; Vuković, V.; Koprivica, M.; Dragovac, G.; Petrović, V. Measles Epidemiology and Coverage of Immunization Against Measles in the Autonomous Province of Vojvodina, Serbia: Local Trends in a Regional Context. Vaccines 2025, 13, 711. https://doi.org/10.3390/vaccines13070711
Ristić M, Ilić S, Rajčević S, Štrbac M, Medić S, Pustahija T, Vuković V, Koprivica M, Dragovac G, Petrović V. Measles Epidemiology and Coverage of Immunization Against Measles in the Autonomous Province of Vojvodina, Serbia: Local Trends in a Regional Context. Vaccines. 2025; 13(7):711. https://doi.org/10.3390/vaccines13070711
Chicago/Turabian StyleRistić, Mioljub, Svetlana Ilić, Smiljana Rajčević, Mirjana Štrbac, Snežana Medić, Tatjana Pustahija, Vladimir Vuković, Marko Koprivica, Gorana Dragovac, and Vladimir Petrović. 2025. "Measles Epidemiology and Coverage of Immunization Against Measles in the Autonomous Province of Vojvodina, Serbia: Local Trends in a Regional Context" Vaccines 13, no. 7: 711. https://doi.org/10.3390/vaccines13070711
APA StyleRistić, M., Ilić, S., Rajčević, S., Štrbac, M., Medić, S., Pustahija, T., Vuković, V., Koprivica, M., Dragovac, G., & Petrović, V. (2025). Measles Epidemiology and Coverage of Immunization Against Measles in the Autonomous Province of Vojvodina, Serbia: Local Trends in a Regional Context. Vaccines, 13(7), 711. https://doi.org/10.3390/vaccines13070711






