Recent Advances in Bioconjugate Vaccine Development
Abstract
1. Introduction
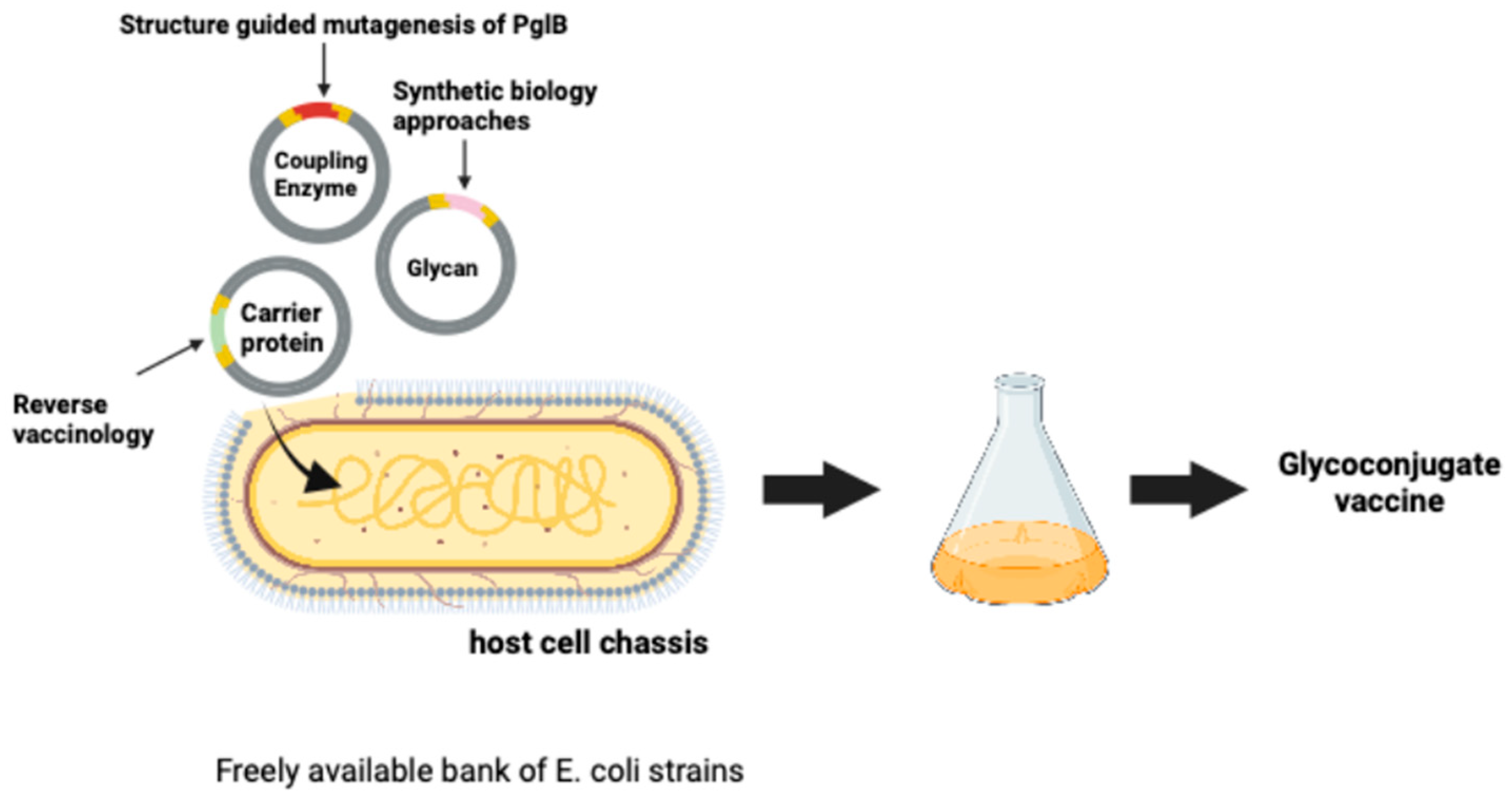
2. Discovery of N-Linked Protein Glycosylation and the Development of PGCT and Bioconjugation
3. Recent Technical Development of Bioconjugation
3.1. Glycan
3.2. The Carrier Protein
3.3. The Oligosaccharyltransferase Enzyme
3.3.1. N-Linked OSTs
3.3.2. O-Linked OSTs
3.4. Microbial Chassis Engineering
4. Selected Exemplars of Bioconjugate Vaccines with Different Glycan Structures
5. Discussion and Future Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Parke, J.C., Jr. Capsular polysaccharide of Haemophilus influenzae type B as a vaccine. Pediatr. Infect. Dis. J. 1987, 6, 79–80. [Google Scholar] [CrossRef] [PubMed]
- Avci, F.Y.; Li, X.; Tsuji, M.; Kasper, D.L. A mechanism for glycoconjugate vaccine activation of the adaptive immune system and its implications for vaccine design. Nat. Med. 2011, 17, 1602–1609. [Google Scholar] [CrossRef]
- Rappuoli, R. Glycoconjugate vaccines: Principles and mechanisms. Sci. Transl. Med. 2018, 10, eaat4615. [Google Scholar] [CrossRef]
- Schneerson, R.; Barrera, O.; Sutton, A.; Robbins, J.B. Preparation, characterization, and immunogenicity of Haemophilus influenzae type b polysaccharide-protein conjugates. J. Exp. Med. 1980, 152, 361–376. [Google Scholar] [CrossRef]
- Daugla, D.M.; Gami, J.P.; Gamougam, K.; Naibei, N.; Mbainadji, L.; Narbé, M.; Toralta, J.; Kodbesse, B.; Ngadoua, C.; Coldiron, M.E.; et al. Effect of a serogroup A meningococcal conjugate vaccine (PsA-TT) on serogroup A meningococcal meningitis and carriage in Chad: A community study. Lancet 2014, 383, 40–47. [Google Scholar] [CrossRef]
- Jackson, L.A.; Gurtman, A.; van Cleeff, M.; Jansen, K.U.; Jayawardene, D.; Devlin, C.; Scott, D.A.; Emini, E.A.; Gruber, W.C.; Schmoele-Thoma, B. Immunogenicity and safety of a 13-valent pneumococcal conjugate vaccine compared to a 23-valent pneumococcal polysaccharide vaccine in pneumococcal vaccine-naive adults. Vaccine 2013, 31, 3577–3584. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Gibani, M.M.; Moore, M.; Juel, H.B.; Jones, E.; Meiring, J.; Harris, V.; Gardner, J.; Nebykova, A.; Kerridge, S.A.; et al. Efficacy and immunogenicity of a Vi-tetanus toxoid conjugate vaccine in the prevention of typhoid fever using a controlled human infection model of Salmonella Typhi: A randomised controlled, phase 2b trial. Lancet 2017, 390, 2472–2480. [Google Scholar] [CrossRef]
- Jefferies, J.M.C.; Macdonald, E.; Faust, S.N.; Clarke, S.C. 13-valent pneumococcal conjugate vaccine (PCV13). Hum. Vaccin. 2011, 7, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Micoli, F.; Del Bino, L.; Alfini, R.; Carboni, F.; Romano, M.R.; Adamo, R. Glycoconjugate vaccines: Current approaches towards faster vaccine design. Expert Rev. Vaccines 2019, 18, 881–895. [Google Scholar] [CrossRef]
- Szymanski, C.M.; Ruijin, Y.; Ewing, C.P.; Trust, T.J.; Guerry, P. Evidence for a system of general protein glycosylation in Campylobacter jejuni. Mol. Microbiol. 1999, 32, 1022–1030. [Google Scholar] [CrossRef]
- Parkhill, J.; Wren, B.W.; Mungall, K.; Ketley, J.M.; Churcher, C.; Basham, D.; Chillingworth, T.; Davies, R.M.; Feltwell, T.; Holroyd, S.; et al. The genome sequence of the food-borne pathogen Campylobacter jejuni reveals hypervariable sequences. Nature 2000, 403, 665–668. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.; Linton, D.; Hitchen, P.G.; Nita-Lazar, M.; Haslam, S.M.; North, S.J.; Panico, M.; Morris, H.R.; Dell, A.; Wren, B.W.; et al. N-linked glycosylation in Campylobacter jejuni and its functional transfer into E. coli. Science 2002, 298, 1790–1793. [Google Scholar] [CrossRef] [PubMed]
- Kowarik, M.; Young, N.M.; Numao, S.; Schulz, B.L.; Hug, I.; Callewaert, N.; Mills, D.C.; Watson, D.C.; Hernandez, M.; Kelly, J.F.; et al. Definition of the bacterial N-glycosylation site consensus sequence. EMBO J. 2006, 25, 1957–1966. [Google Scholar] [CrossRef]
- Feldman, M.F.; Wacker, M.; Hernandez, M.; Hitchen, P.G.; Marolda, C.L.; Kowarik, M.; Morris, H.R.; Dell, A.; Valvano, M.A.; Aebi, M.; et al. Engineering N-linked protein glycosylation with diverse O antigen lipopolysaccharide structures in Escherichia coli. Proc. Natl. Acad. Sci. USA 2005, 102, 3016–3021. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.; Feldman, M.F.; Callewaert, N.; Kowarik, M.; Clarke, B.R.; Pohl, N.L.; Hernandez, M.; Vines, E.D.; Valvano, M.A.; Whitfield, C.; et al. Substrate specificity of bacterial oligosaccharyltransferase suggests a common transfer mechanism for the bacterial and eukaryotic systems. Proc. Natl. Acad. Sci. USA 2006, 103, 7088–7093. [Google Scholar] [CrossRef]
- Langdon, R.H.; Jon, C.; Wren, B.W. N-Linked Glycosylation in Bacteria: An Unexpected Application. Future Microbiol. 2009, 4, 401–412. [Google Scholar] [CrossRef]
- Bentley, S.D.; Aanensen, D.M.; Mavroidi, A.; Saunders, D.; Rabbinowitsch, E.; Collins, M.; Donohoe, K.; Harris, D.; Murphy, L.; Quail, M.A.; et al. Genetic Analysis of the Capsular Biosynthetic Locus from All 90 Pneumococcal Serotypes. PLoS Genet. 2006, 2, e31. [Google Scholar] [CrossRef]
- Wantuch, P.L.; Knoot, C.J.; Robinson, L.S.; Vinogradov, E.; Scott, N.E.; Harding, C.M.; Rosen, D.A. Capsular polysaccharide inhibits vaccine-induced O-antigen antibody binding and function across both classical and hypervirulent K2:O1 strains of Klebsiella pneumoniae. PLoS Pathog. 2023, 19, e1011367. [Google Scholar] [CrossRef]
- Patro, L.P.P.; Sudhakar, K.U.; Rathinavelan, T. K-PAM: A unified platform to distinguish Klebsiella species K- and O-antigen types, model antigen structures and identify hypervirulent strains. Sci. Rep. 2020, 10, 16732. [Google Scholar] [CrossRef]
- Løchen, A.; Croucher, N.J.; Anderson, R.M. Divergent serotype replacement trends and increasing diversity in pneumococcal disease in high income settings reduce the benefit of expanding vaccine valency. Sci. Rep. 2020, 10, 18977. [Google Scholar] [CrossRef]
- Obaro, S.K.; Adegbola, R.A.; Banya, W.A.; Greenwood, B.M. Carriage of pneumococci after pneumococcal vaccination. Lancet 1996, 348, 271–272. [Google Scholar] [CrossRef] [PubMed]
- Weinberger, D.M.; Malley, R.; Lipsitch, M. Serotype replacement in disease after pneumococcal vaccination. Lancet 2011, 378, 1962–1973. [Google Scholar] [CrossRef] [PubMed]
- Reglinski, M.; Ercoli, G.; Plumptre, C.; Kay, E.; Petersen, F.C.; Paton, J.C.; Wren, B.W.; Brown, J.S. A recombinant conjugated pneumococcal vaccine that protects against murine infections with a similar efficacy to Prevnar-13. npj Vaccines 2018, 3, 53. [Google Scholar] [CrossRef]
- Feldman, M.F.; Mayer Bridwell, A.E.; Scott, N.E.; Vinogradov, E.; McKee, S.R.; Chavez, S.M.; Twentyman, J.; Stallings, C.L.; Rosen, D.A.; Harding, C.M. A promising bioconjugate vaccine against hypervirulent Klebsiella pneumoniae. Proc. Natl. Acad. Sci. USA 2019, 116, 18655–18663. [Google Scholar] [CrossRef]
- Cuccui, J.; Thomas, R.M.; Moule, M.G.; D’Elia, R.V.; Laws, T.R.; Mills, D.C.; Williamson, D.; Atkins, T.P.; Prior, J.L.; Wren, B.W. Exploitation of bacterial N-linked glycosylation to develop a novel recombinant glycoconjugate vaccine against Francisella tularensis. Open Biol. 2013, 3, 130002. [Google Scholar] [CrossRef][Green Version]
- Ihssen, J.; Kowarik, M.; Dilettoso, S.; Tanner, C.; Wacker, M.; Thöny-Meyer, L. Production of glycoprotein vaccines in Escherichia coli. Microb. Cell Fact. 2010, 9, 1–13. [Google Scholar] [CrossRef]
- Wang, Y.; Perepelov, A.V.; Senchenkova, S.N.; Lu, G.; Wang, X.; Ma, G.; Yang, Q.; Yuan, J.; Wang, Y.; Xie, L.; et al. Glycoengineering directs de novo biomanufacturing of UPEC O21 O-antigen polysaccharide-based glycoprotein. Int. J. Biol. Macromol. 2023, 253, 126993. [Google Scholar] [CrossRef]
- Williams, A.J.; Warfel, K.F.; Desai, P.; Li, J.; Lee, J.J.; Wong, D.A.; Nguyen, P.M.; Qin, Y.; Sobol, S.E.; Jewett, M.C.; et al. A low-cost recombinant glycoconjugate vaccine confers immunogenicity and protection against enterotoxigenic Escherichia coli infections in mice. Front. Mol. Biosci. 2023, 10, 1085887. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Pan, C.; Wang, K.; Guo, Y.; Sun, Y.G.; Li, X.; Sun, P.; Wu, J.; Wang, H.; Zhu, L. Preparation of a Klebsiella pneumoniae conjugate nanovaccine using glycol-engineered Escherichia coli. Microb. Cell Fact. 2023, 22, 95. [Google Scholar] [CrossRef]
- Li, S.; Huang, J.; Wang, K.; Liu, Y.; Guo, Y.; Li, X.; Wu, J.; Sun, P.; Wang, Y.; Zhu, L.; et al. A bioconjugate vaccine against Brucella abortus produced by engineered Escherichia coli. Front. Bioeng. Biotechnol. 2023, 11, 1121074. [Google Scholar] [CrossRef]
- Wantuch, P.L.; Knoot, C.J.; Robinson, L.S.; Vinogradov, E.; Scott, N.E.; Harding, C.M.; Rosen, D.A. Heptavalent O-Antigen Bioconjugate Vaccine Exhibiting Differential Functional Antibody Responses Against Diverse Klebsiella pneumoniae Isolates. J. Infect. Dis. 2024, 230, 578–589. [Google Scholar] [CrossRef]
- Castro, S.A.; Passmore, I.J.; Ndeh, D.; Shaw, H.A.; Ruda, A.; Burns, K.; Thomson, S.; Nagar, R.; Alagesan, K.; Lucas, K.; et al. A platform for the recombinant production of Group A Streptococcus glycoconjugate vaccines. npj Vaccines 2025, 10, 16. [Google Scholar] [CrossRef] [PubMed]
- Taylor, G.M.; Mordaka, P.M.; Heap, J.T. Start-Stop Assembly: A functionally scarless DNA assembly system optimized for metabolic engineering. Nucleic Acids Res. 2019, 47, e17. [Google Scholar] [CrossRef] [PubMed]
- Passmore, I.J.; Faulds-Pain, A.; Abouelhadid, S.; Harrison, M.A.; Hall, C.L.; Hitchen, P.; Dell, A.; Heap, J.T.; Wren, B.W. A combinatorial DNA assembly approach to biosynthesis of N-linked glycans in E. coli. Glycobiology 2023, 33, 138–149. [Google Scholar] [CrossRef] [PubMed]
- Harrison, M.A.; Atkins, E.; Faulds-Pain, A.; Heap, J.T.; Wren, B.W.; Passmore, I.J. Modular Combinatorial DNA Assembly of Group B Streptococcus Capsular Polysaccharide Biosynthesis Pathways to Expediate the Production of Novel Glycoconjugate Vaccines. Vaccines 2025, 13, 279. [Google Scholar] [CrossRef]
- Valenzuela-Ortega, M.; French, C. Joint universal modular plasmids (JUMP): A flexible vector platform for synthetic biology. Synth. Biol. 2021, 6, ysab003. [Google Scholar] [CrossRef]
- Jones, J.A.; Vernacchio, V.R.; Lachance, D.M.; Lebovich, M.; Fu, L.; Shirke, A.N.; Schultz, V.L.; Cress, B.; Linhardt, R.J.; Koffas, M.A.G. EPathOptimize: A combinatorial approach for transcriptional balancing of metabolic pathways. Sci. Rep. 2015, 5, 11301. [Google Scholar] [CrossRef]
- Gasperini, G.; Raso, M.M.; Schiavo, F.; Aruta, M.G.; Ravenscroft, N.; Bellich, B.; Cescutti, P.; Necchi, F.; Rappuoli, R.; Micoli, F. Rapid generation of Shigella flexneri GMMA displaying natural or new and cross-reactive O-Antigens. npj Vaccines 2022, 7, 1–10. [Google Scholar] [CrossRef]
- Micoli, F.; Adamo, R.; Costantino, P. Protein carriers for glycoconjugate vaccines: History, selection criteria, characterization and new trends. Molecules 2018, 23, 1451. [Google Scholar] [CrossRef]
- Ielmini, M.V.; Feldman, M.F. Desulfovibrio desulfuricans PglB homolog possesses oligosaccharyltransferase activity with relaxed glycan specificity and distinct protein acceptor sequence requirements. Glycobiology 2011, 21, 734–742. [Google Scholar] [CrossRef]
- Ollis, A.A.; Chai, Y.; Natarajan, A.; Perregaux, E.; Jaroentomeechai, T.; Guarino, C.; Smith, J.; Zhang, S.; DeLisa, M.P. Substitute sweeteners: Diverse bacterial oligosaccharyltransferases with unique N-glycosylation site preferences. Sci. Rep. 2015, 5, 15237. [Google Scholar] [CrossRef] [PubMed]
- Castric, P. PilO, a gene required for glycosylation of Pseudomonas aeruginosa 1244 pilin. Microbiology 1995, 141, 1247–1254. [Google Scholar] [CrossRef] [PubMed]
- Faridmoayer, A.; Fentabil, M.A.; Mills, D.C.; Klassen, J.S.; Feldman, M.F. Functional characterization of bacterial oligosaccharyltransferases involved in O-linked protein glycosylation. J. Bacteriol. 2007, 189, 8088–8098. [Google Scholar] [CrossRef]
- Harding, C.M.; Nasr, M.A.; Kinsella, R.L.; Scott, N.E.; Foster, L.J.; Weber, B.S. Fiester, S.E.; Actis, L.A.; Tracy, E.N.; Munson, R.S.; et al. Acinetobacter strains carry two functional oligosaccharyltransferases, one devoted exclusively to type IV pilin, and the other one dedicated to O-glycosylation of multiple proteins. Mol. Microbiol. 2015, 96, 1023–1041. [Google Scholar] [CrossRef] [PubMed]
- Vik, Å.; Aas, F.E.; Anonsen, J.H.; Bilsborough, S.; Schneider, A.; Egge-Jacobsen, W.; Koomey, M. Broad spectrum O-linked protein glycosylation in the human pathogen Neisseria gonorrhoeae. Proc. Natl. Acad. Sci. USA 2009, 106, 4447–4452. [Google Scholar] [CrossRef]
- Qutyan, M.; Henkel, M.; Horzempa, J.; Quinn, M.; Castric, P. Glycosylation of pilin and non-pilin protein constructs by Pseudomonas aeruginosa 1244. J. Bacteriol. 2010, 192, 5972–5981. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.; Sun, P.; Liu, B.; Liang, H.; Peng, Z.; Dong, Y.; Wang, D.; Liu, X.; Wang, B.; Zeng, M.; et al. Biosynthesis of conjugate vaccines using an O-linked glycosylation system. mBio 2016, 7, e00443-16. [Google Scholar] [CrossRef]
- Knoot, C.J.; Robinson, L.S.; Harding, C.M. A minimal sequon sufficient for O-linked glycosylation by the versatile oligosaccharyltransferase PglS. Glycobiology 2021, 31, 1192–1203. [Google Scholar] [CrossRef]
- Fisher, A.C.; Haitjema, C.H.; Guarino, C.; Çelik, E.; Endicott, C.E.; Reading, C.A.; Merritt, J.H.; Ptak, A.C.; Zhang, S.; DeLisa, M.P. Production of secretory and extracellular N-linked glycoproteins in Escherichia coli. Appl. Environ. Microbiol. 2011, 77, 871–881. [Google Scholar] [CrossRef]
- Fierro, C.A.; Sarnecki, M.; Doua, J.; Spiessens, B.; Go, O.; Davies, T.A.; van den Dobbelsteen, G.; Poolman, J.; Abbanat, D.; Haazen, W. Safety, Reactogenicity, Immunogenicity, and Dose Selection of 10-Valent Extraintestinal Pathogenic Escherichia coli Bioconjugate Vaccine (VAC52416) in Adults Aged 60-85 Years in a Randomized, Multicenter, Interventional, First-in-Human, Phase 1/2a Study. Open Forum Infect. Dis. 2023, 10, ofad417. [Google Scholar] [CrossRef]
- Clarkson, K.A.; Talaat, K.R.; Alaimo, C.; Martin, P.; Bourgeois, A.L.; Dreyer, A.; Porter, C.K.; Chakraborty, S.; Brubaker, J.; Elwood, D.; et al. Immune response characterization in a human challenge study with a Shigella flexneri 2a bioconjugate vaccine. eBioMedicine 2021, 66, 103308. [Google Scholar] [CrossRef] [PubMed]
- Duke, J.A.; Paschall, A.V.; Robinson, L.S.; Knoot, C.J.; Vinogradov, E.; Scott, N.E.; Feldman, M.F.; Avci, F.Y.; Harding, C.M. Development and Immunogenicity of a Prototype Multivalent Group B Streptococcus Bioconjugate Vaccine. ACS Infect. Dis. 2021. [CrossRef]
- Sun, P.; Pan, C.; Zeng, M.; Liu, B.; Liang, H.; Wang, D.; Liu, X.; Wang, B.; Lyu, Y.; Wu, J.; et al. Design and production of conjugate vaccines against S. Paratyphi A using an O-linked glycosylation system in vivo. npj Vaccines 2018, 3, 4. [Google Scholar] [CrossRef]
- Micoli, F.; Stefanetti, G.; MacLennan, C.A. Exploring the variables influencing the immune response of traditional and innovative glycoconjugate vaccines. Front. Mol. Biosci. 2023, 10, 1201693. [Google Scholar] [CrossRef] [PubMed]
- Anish, C.; Beurret, M.; Poolman, J. Combined effects of glycan chain length and linkage type on the immunogenicity of glycoconjugate vaccines. npj Vaccines 2021, 6, 150. [Google Scholar] [CrossRef] [PubMed]
- Marshall, L.E.; Nelson, M.; Davies, C.H.; Whelan, A.O.; Jenner, D.C.; Moule, M.G.; Denman, C.; Cuccui, J.; Atkins, T.P.; Wren, B.W.; et al. An O-Antigen glycoconjugate vaccine produced using protein glycan coupling technology is protective in an inhalational rat model of tularemia. J. Immunol. Res. 2018, 2018, 8087916. [Google Scholar] [CrossRef]
- Sun, X.; Stefanetti, G.; Berti, F.; Kasper, D.L. Polysaccharide structure dictates mechanism of adaptive immune response to glycoconjugate vaccines. Proc. Natl. Acad. Sci. USA 2019, 116, 193–198. [Google Scholar] [CrossRef]
- Schutze, M.P.; Leclerc, C.; Jolivet, M.; Audibert, F.; Chedid, L. Carrier-induced epitopic suppression, a major issue for future synthetic vaccines. J. Immunol. 1985, 135, 2319–2322. [Google Scholar] [CrossRef]
- Wang, Y.; Liu, H.; Wang, B.; Gheyret, G.; Qin, J.; Wang, H.; Di, Y.; Wang, Y.; Wang, J.; Tan, H. Recent advances in the biosynthesis of polysaccharide-based antimicrobial glycoconjugate vaccines. Front. Microbiol. 2025, 15, 1457908. [Google Scholar] [CrossRef]
- Rappuoli, R. Reverse vaccinology, a genome-based approach to vaccine development. Vaccine 2001, 19, 2688–2691. [Google Scholar] [CrossRef]
- Correia, B.E.; Bates, J.T.; Loomis, R.J.; Baneyx, G.; Carrico, C.; Jardine, J.G.; Rupert, P.; Correnti, C.; Kalyuzhniy, O.; Vittal, V.; et al. Proof of principle for epitope-focused vaccine design. Nature 2014, 507, 201–206. [Google Scholar] [CrossRef] [PubMed]
- Corti, D.; Sallusto, F.; Lanzavecchia, A. High throughput cellular screens to interrogate the human T and B cell repertoires. Curr. Opin. Immunol. 2011, 23, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Rappuoli, R.; Bottomley, M.J.; D’Oro, U.; Finco, O.; De Gregorio, E. Reverse vaccinology 2.0: Human immunology instructs vaccine antigen design. J. Exp. Med. 2016, 213, 469–481. [Google Scholar] [CrossRef]
- Goodswen, S.J.; Kennedy, P.J.; Ellis, J.T. A guide to current methodology and usage of reverse vaccinology towards in silico vaccine discovery. FEMS Microbiol. Rev. 2023, 47, fuad004. [Google Scholar] [CrossRef] [PubMed]
- Masignani, V.; Pizza, M.; Moxon, E.R. The development of a vaccine against Meningococcus B using reverse vaccinology. Front. Immunol. 2019, 10, 751. [Google Scholar] [CrossRef]
- Moriel, D.G.; Bertoldi, I.; Spagnuolo, A.; Marchi, S.; Rosini, R.; Nesta, B.; Pastorello, I.; Mariani Corea, V.A.; Torricelli, G.; Cartocci, E.; et al. Identification of protective and broadly conserved vaccine antigens from the genome of extraintestinal pathogenic Escherichia coli. Proc. Natl. Acad. Sci. USA 2010, 107, 9072–9077. [Google Scholar] [CrossRef]
- de Alwis, R.; Liang, L. Taghavian, O.; Werner, E.; The, H.C.; Thu, T.N.H.; Duong, V.T.; Davies, D.H.; Felgner, P.L.; Baker, S. The identification of novel immunogenic antigens as potential Shigella vaccine components. Genome Med. 2021, 13, 8. [Google Scholar] [CrossRef]
- Maione, D.; Margarit, I.; Rinaudo, C.D.; Masignani, V.; Mora, M.; Scarselli, M.; Tettelin, H.; Brettoni, C.; Iacobini, E.T.; Rosini, R.; et al. Identification of a Universal Group B Streptococcus Vaccine by Multiple Genome Screen. Science 2005, 309, 148–150. [Google Scholar] [CrossRef]
- Al-Hasani, K.; Boyce, J.; McCarl, V.P.; Bottomley, S.; Wilkie, I.; Adler, B. Identification of novel immunogens in Pasteurella multocida. Microb. Cell Fact. 2007, 6, 3. [Google Scholar] [CrossRef]
- Muruato, L.A.; Tapia, D.; Hatcher, C.L.; Kalita, M.; Brett, P.J.; Gregory, A.E.; Samuel, J.E.; Titball, R.W.; Torres, A.G. Use of reverse vaccinology in the design and construction of nanoglycoconjugate vaccines against Burkholderia pseudomallei. Clin. Vaccine Immunol. 2017, 24, e00206-17. [Google Scholar] [CrossRef]
- Nothaft, H.; Szymanski, C.M. Protein glycosylation in bacteria: Sweeter than ever. Nat. Rev. Microbiol. 2010, 8, 765–778. [Google Scholar] [CrossRef] [PubMed]
- Valderrama-Rincon, J.D.; Fisher, A.C.; Merritt, J.H.; Fan, Y.Y.; Reading, C.A.; Chhiba, K.; Heiss, C.; Azadi, P.; Aebi, M.; DeLisa, M.P. An engineered eukaryotic protein glycosylation pathway in Escherichia coli. Nat. Chem. Biol. 2012, 8, 434–436. [Google Scholar] [CrossRef] [PubMed]
- Cuccui, J.; Wren, B. Hijacking bacterial glycosylation for the production of glycoconjugates, from vaccines to humanised glycoproteins. J. Pharm. Pharmacol. 2015, 67, 338–350. [Google Scholar] [CrossRef]
- Lizak, C.; Gerber, S.; Numao, S.; Aebi, M.; Locher, K.P. X-ray structure of a bacterial oligosaccharyltransferase. Nature 2011, 474, 350–356. [Google Scholar] [CrossRef]
- Zorzoli, A.; Meyer, B.H.; Adair, E.; Torgov, V.I.; Veselovsky, V.V.; Danilov, L.L.; Uhrin, D.; Dorfmueller, H.C. Group A, B, C, and G Streptococcus Lancefield antigen biosynthesis is initiated by a conserved α-D-GlcNAc-β-1,4-L-rhamnosyltransferase. J. Biol. Chem. 2019, 294, 15237–15256. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.M.; Glover, K.J.; Imperiali, B. From Peptide to Protein: Comparative Analysis of the Substrate Specificity of N-Linked Glycosylation in C. jejuni. Biochemistry 2007, 46, 5579–5585. [Google Scholar] [CrossRef] [PubMed]
- Faridmoayer, A.; Fentabil, M.A.; Haurat, M.F.; Yi, W.; Woodward, R.; Wang, P.G.; Feldman, M.F. Extreme substrate promiscuity of the Neisseria oligosaccharyl transferase involved in protein O-glycosylation. J. Biol. Chem. 2008, 283, 34596–34604. [Google Scholar] [CrossRef]
- Schulz, B.L.; Jen, F.E.C.; Power, P.M.; Jones, C.E.; Fox, K.L.; Ku, S.C.; Blanchfield, J.T.; Jennings, M.P. Identification of Bacterial Protein O-Oligosaccharyltransferases and Their Glycoprotein Substrates. PLoS ONE 2013, 8, e62768. [Google Scholar] [CrossRef]
- Power, P.M.; Seib, K.L.; Jennings, M.P. Pilin glycosylation in Neisseria meningitidis occurs by a similar pathway to wzy-dependent O-antigen biosynthesis in Escherichia coli. Biochem. Biophys. Res. Commun. 2006, 347, 904–908. [Google Scholar] [CrossRef]
- Harding, C.M.; Nasr, M.A.; Scott, N.E.; Goyette-Desjardins, G.; Nothaft, H.; Mayer, A.E.; Chavez, S.M.; Huynh, J.P.; Kinsella, R.L.; Szymanski, C.M.; et al. A platform for glycoengineering a polyvalent pneumococcal bioconjugate vaccine using E. coli as a host. Nat. Commun. 2019, 10, 891. [Google Scholar] [CrossRef]
- Comer, J.E.; Marshall, M.A.; Blanch, V.J.; Deal, C.D.; Castric, P. Identification of the Pseudomonas aeruginosa 1244 pilin glycosylation site. Infect. Immun. 2002, 70, 2837–2845. [Google Scholar] [CrossRef] [PubMed]
- Knoot, C.J.; Wantuch, P.L.; Robinson, L.S.; Rosen, D.A.; Scott, N.E.; Harding, C.M. Discovery and characterization of a new class of O-linking oligosaccharyltransferases from the Moraxellaceae family. Glycobiology 2023, 33, 57–74. [Google Scholar] [CrossRef] [PubMed]
- Kämpf, M.M.; Braun, M.; Sirena, D.; Ihssen, J.; Thöny-Meyer, L.; Ren, Q. In vivo production of a novel glycoconjugate vaccine against Shigella flexneri 2a in recombinant Escherichia coli: Identification of stimulating factors for in vivo glycosylation. Microb. Cell Fact. 2015, 14, 12. [Google Scholar] [CrossRef]
- Kay, E.J.; Dooda, M.K.; Bryant, J.C.; Reid, A.J.; Wren, B.W.; Troutman, J.M.; Jorgenson, M.A. Engineering Escherichia coli for increased Und-P availability leads to material improvements in glycan expression technology. Microb. Cell Fact. 2024, 23, 72. [Google Scholar] [CrossRef]
- Pandhal, J.; Ow, S.Y.; Noirel, J.; Wright, P.C. Improving N-glycosylation efficiency in Escherichia coli using shotgun proteomics, metabolic network analysis, and selective reaction monitoring. Biotechnol. Bioeng. 2011, 108, 902–912. [Google Scholar] [CrossRef]
- Pandhal, J.; Ow, S.Y.; Noirel, J.; Wright, P.C. Inverse metabolic engineering to improve Escherichia coli as an N-glycosylation host. Biotechnol. Bioeng. 2013, 110, 2482–2493. [Google Scholar] [CrossRef] [PubMed]
- Strutton, B.; Jaffé, S.R.P.; Pandhal, J.; Wright, P.C. Producing a glycosylating Escherichia coli cell factory: The placement of the bacterial oligosaccharyl transferase pglB onto the genome. Biochem. Biophys. Res. Commun. 2018, 495, 686–692. [Google Scholar] [CrossRef]
- Abouelhadid, S.; Atkins, E.R.; Kay, E.J.; Passmore, I.J.; North, S.J.; Lehri, B.; Hitchen, P.; Bakke, E.; Rahman, M.; Bossé, J.T.; et al. Development of a novel glycoengineering platform for the rapid production of conjugate vaccines. Microb. Cell Fact. 2023, 22, 159. [Google Scholar] [CrossRef]
- Yates, L.E.; Natarajan, A.; Li, M.; Hale, M.E.; Mills, D.C.; DeLisa, M.P. Glyco-recoded Escherichia coli: Recombineering-based genome editing of native polysaccharide biosynthesis gene clusters. Metab. Eng. 2019, 53, 59–68. [Google Scholar] [CrossRef]
- Kay, E.J.; Mauri, M.; Willcocks, S.J.; Scott, T.A.; Cuccui, J.; Wren, B.W. Engineering a suite of E. coli strains for enhanced expression of bacterial polysaccharides and glycoconjugate vaccines. Microb. Cell Fact. 2022, 21, 1–15. [Google Scholar] [CrossRef]
- Ravenscroft, N.; Haeuptle, M.A.; Kowarik, M.; Fernandez, F.S.; Carranza, P.; Brunner, A.; Steffen, M.; Wetter, M.; Keller, S.; Ruch, C.; et al. Purification and characterization of a Shigella conjugate vaccine, produced by glycoengineering Escherichia coli. Glycobiology 2016, 26, 51–62. [Google Scholar] [CrossRef] [PubMed]
- Ravenscroft, N.; Braun, M.; Schneider, J.; Dreyer, A.M.; Wetter, M.; Haeuptle, M.A.; Kemmler, S.; Steffen, M.; Sirena, D.; Herwig, S.; et al. Characterization and immunogenicity of a Shigella flexneri 2a O-antigen bioconjugate vaccine candidate. Glycobiology 2019, 29, 669–681. [Google Scholar] [CrossRef] [PubMed]
- Wacker, M.; Wang, L.; Kowarik, M.; Dowd, M.; Lipowsky, G.; Faridmoayer, A.; Shields, K.; Park, S.; Alaimo, C.; Kelley, K.A.; et al. Prevention of Staphylococcus aureus infections by glycoprotein vaccines synthesized in Escherichia coli. J. Infect. Dis. 2014, 209, 1551–1561. [Google Scholar] [CrossRef] [PubMed]
- Riddle, M.S.; Kaminski, R.W.; Di Paolo, C.; Porter, C.K.; Gutierrez, R.L.; Clarkson, K.A.; Weerts, H.E.; Duplessis, C.; Castellano, A.; Alaimo, C.; et al. Safety and immunogenicity of a candidate bioconjugate vaccine against Shigella flexneri 2a administered to healthy adults: A single-blind, randomized phase I study. Clin. Vaccine Immunol. 2016, 23, 908–917. [Google Scholar] [CrossRef]
- Fierro, C.A.; Sarnecki, M.; Spiessens, B.; Go, O.; Day, T.A.; Davies, T.A.; van den Dobbelsteen, G.; Poolman, J.; Abbanat, D.; Haazen, W. A randomized phase 1/2a trial of ExPEC10V vaccine in adults with a history of UTI. npj Vaccines 2024, 9, 106. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wren, B.W.; Hall, C.L.; Terra, V.S.; Harrison, M.A.; Atkins, E.; Nasher, F.; Passmore, I.J. Recent Advances in Bioconjugate Vaccine Development. Vaccines 2025, 13, 703. https://doi.org/10.3390/vaccines13070703
Wren BW, Hall CL, Terra VS, Harrison MA, Atkins E, Nasher F, Passmore IJ. Recent Advances in Bioconjugate Vaccine Development. Vaccines. 2025; 13(7):703. https://doi.org/10.3390/vaccines13070703
Chicago/Turabian StyleWren, Brendan W., Catherine L. Hall, Vanessa S. Terra, Mark A. Harrison, Elizabeth Atkins, Fauzy Nasher, and Ian J. Passmore. 2025. "Recent Advances in Bioconjugate Vaccine Development" Vaccines 13, no. 7: 703. https://doi.org/10.3390/vaccines13070703
APA StyleWren, B. W., Hall, C. L., Terra, V. S., Harrison, M. A., Atkins, E., Nasher, F., & Passmore, I. J. (2025). Recent Advances in Bioconjugate Vaccine Development. Vaccines, 13(7), 703. https://doi.org/10.3390/vaccines13070703






