1. Introduction
The first year of the SARS-CoV-2 pandemic was a particular threat for patients with Crohn’s disease and ulcerative colitis, because most of them require long-term immune-suppressive therapy. Before the availability of COVID-19 vaccines, patients with inflammatory bowel diseases (IBD) and their families were very concerned about these therapies increasing their risk of acquiring infection and experiencing severe disease with increased mortality [
1]. Data from large national and international registries and observational cohort studies provided convincing evidence that IBD patients are not more prone to acquiring SARS-CoV-2 infection compared to the general population [
2,
3]. However, these analyses did not consider that due to a higher self-estimated risk from COVID-19, patients under immunosuppression may take more precautions and preventive measures against infection, e.g., by avoiding crowding, social contacts, and the use of public transport [
1]. Registry data identified IBD-specific risk factors that predispose patients to a severe disease course, as evidenced by the need for hospitalization, admission to an intensive care unit, and mortality. Only the use of systemic corticosteroids and a poorly controlled active bowel inflammation had been reported to increase the risk for complicated disease [
4,
5]. These findings resulted in the refinement of management recommendations and a pandemic-related update of the guidelines [
3,
6,
7].
The availability of mRNA COVID-19 vaccines brought hope for a rapid and successful containment of the pandemic. However, concerns were raised about IBD-specific side effects, such as vaccination-related induction of disease flare and impaired effectiveness of the vaccines under mono- or combination therapy with different drugs that possibly affect the B-cell and T-cell-mediated immune response to vaccination. Assessing the effectiveness of COVID-19 vaccines in patients under immunosuppressive drugs is complex due to the influence of various factors. These include patient characteristics such as age, gender, genetic predisposition, comorbidities, and lifestyle choices and the specific type of COVID-19 vaccine administered. The interaction of different factors further complicates the analysis of single effects, even when confounders are considered. The RisCoin Study, a prospective longitudinal monocentric observational cohort study conducted at the LMU University Hospital, Munich, Germany, addressed this complexity [
8]. In this manuscript, we focused on adult patients with IBD treated with various drugs, with particular interest in the biologics anti-TNF antibodies, vedolizumab, and ustekinumab. TNF is a key cytokine involved in the activation and differentiation of immune cells, playing an essential role in T-cell-dependent antibody production—such as the activation of circulating T follicular helper cells—and in the formation of germinal centers, where B cells mature, diversify, and develop into antibody-producing memory B cells and long-lived plasma cells. In contrast, ustekinumab specifically targets the p40 subunit shared by IL-12 and IL-23, thereby blocking their signaling but not interfering with the overall function of T or B cells involved in vaccine responses. Similarly, vedolizumab acts by inhibiting the trafficking of T cells to the gut and does not impact the immune response to systemically administered vaccines.
We investigated humoral immune responses to mRNA vaccination in IBD patients after basic and booster immunization and compared them to those in health care workers (HCW) without and those with underlying diseases. Furthermore, we assessed epidemiological and environmental factors potentially affecting the observed immune responses.
2. Materials and Methods
2.1. RisCoin Study
Detailed information on the RisCoin study has been previously published [
8]. In brief, all participants were enrolled at the LMU University Hospital Munich between 7 October and 16 December 2021, during a COVID-19 booster vaccination campaign organized by the hospital. Inclusion criteria for the participation were as follows: (i) completed basic SARS-CoV-2 immunization (at least two vaccinations) with the last vaccine ≥4 weeks prior to enrollment; (ii) age ≥18 years; and (iii) signed informed consent. At enrollment, participants donated blood samples for assessment of SARS-CoV-2-specific antibody concentrations and antibody-mediated live-virus neutralization. Participants completed an extensive questionnaire covering demographics, their living and occupational situation, details on adverse effects of COVID-19 vaccinations, previous influenza immunizations, pre-existing health conditions and allergies, regular intake of medication, vitamins, and supplements, dietary habits, and lifestyle factors including tobacco and alcohol consumption [
8].
To evaluate mental stress, we utilized the validated German short version of the standardized Perceived Stress Questionnaire (PSQ) [
9,
10]. This questionnaire provides an overall stress score as well as scores across four domains: (i) worries/fears about the future and feelings of despair and frustration, (ii) tension encompassing restlessness, fatigue, and lack of relaxing, (iii) joy highlighting positive aspects such as feeling challenged, motivated, and secure, and (iv) demands measuring time constraints, pressure, and feeling overwhelmed.
Throughout the entire study period, participants were asked to complete short questionnaires weekly or event-related via a study app. These short questionnaires inquired about information regarding common clinical symptoms of COVID-19, COVID-19 test results, and the occurrence of any SARS-CoV-2 breakthrough infection confirmed by a PCR test. Further, participants could report details regarding their COVID-19 booster vaccination(s) including adverse effects and related countermeasures such as intake of antipyretics [
8,
11].
Follow-up visits took place from 13 December 2021 to 15 March 2022 and, subsequently, from 19 September 2022 to 6 October 2022 [
8]. Participants were invited to additional SARS-CoV-2 antibody testing if they (i) received a booster vaccine after enrollment and ≥4 weeks prior to the follow-up visit or (ii) after they reported a PCR-confirmed breakthrough infection, a suspected infection with typical clinical symptoms, a positive rapid antigen test, or experiencing a close contact with a SARS-CoV-2 PCR-positive person.
2.2. Serological Vaccine Immune Response
The humoral immune response to SARS-CoV-2 was determined by measuring anti-spike and anti-nucleocapsid antibodies via the Elecsys Anti-SARS-CoV-2 N (Roche, Basel, Switzerland, cat.: 09203095190) and Elecsys Anti-SARS-CoV-2 S (Roche, Basel, Switzerland, cat.: 09289267190), respectively, which were performed in accordance with the manufacturer’s recommendations [
11]. Anti-SARS-CoV-2 spike antibody levels were quantified as binding antibody units per milliliter (BAU/mL).
To assess antibody-mediated live-virus neutralization, a highly predictive biomarker of immune protection from symptomatic SARS-CoV-2 infection and severe COVID-19 [
12,
13], a live-virus neutralization assay was employed as described with a clinical isolate of SARS-CoV-2 variant Omicron B.1.1.529 BA.1 (GISAID EPI ISL: 7808190) [
12,
14]. Neutralization titers were calculated as the half-maximal effective dilution of each serum to neutralize viral infection. The upper threshold for the detection of neutralizing activity in the participants’ sera was set to ≥1:10 serum dilution.
2.3. Data Extraction
For this analysis, we extracted data from participants with IBD who were receiving regular care in one of the IBD-Clinics at the LMU University Hospital Munich and from participating HCW. Only data that were complete regarding age, gender, type or date of all previous COVID-19 vaccinations, and key covariates at enrollment (baseline) and at the first follow-up (FU) were extracted (
Supplementary File S1). We excluded participants who had already received their third COVID-19 vaccination (booster) at enrollment, those with a PCR-confirmed SARS-CoV-2 infection prior to or within 2 weeks of recruitment, and those with reactive anti-SARS-CoV-2 nucleocapsid antibodies indicating a subacute or resolved COVID-19. Additionally, we excluded participants who had received non-mRNA vaccines (
Supplementary File S1).
2.3.1. IBD Cohort
We included adult patients with Crohn’s disease or ulcerative colitis. These individuals completed an additional questionnaire on their current IBD-specific medication, which we categorized into three different groups: (i) anti-TNF antibodies (infliximab, adalimumab or golimumab), (ii) no anti-TNF, but vedolizumab or ustekinumab, and (iii) other IBD-specific medications than those in groups i and ii. For group ii, we first investigated the immune response to basic COVID-19 vaccination, stratified by treatment with either vedolizumab or ustekinumab. Since no significant difference or even a trend was found with respect to the vaccination immune response, we combined patients treated with vedolizumab or ustekinumab in one group (group ii).
2.3.2. HCW Cohorts as Comparator
The HCW cohort served as a control group for the IBD cohort, as they may experience similar environmental exposures as patients but are generally healthier. Based on comorbidities reported in the initial questionnaire and current use of any medication, we divided the HCW cohort into three subgroups: HCW-healthy, HCW-plus, and HCW with current immunosuppressive therapy [
8]. The rationale for stratification of the HCW cohort was also provided in the details in
Supplementary File S2. HCW-healthy reported no current or regular intake of any medication (excluding vitamins and supplements) as well as the absence of the following diseases: chronic cardiovascular, pulmonary, renal, gastro-intestinal, liver, neurological, hematological, rheumatological or (auto)immune disease, diabetes mellitus, dyslipidemia or other metabolic disorders, thyroid or other endocrinological disease, and current or previous malignancy. HCW with overweight or obesity, those reporting food or contact allergies, and those with allergic rhino conjunctivitis without current drug therapy were considered healthy. In contrast, HCW-plus was defined as HCW reporting any of the above-mentioned co-morbidities or regular intake of medication excluding immunosuppressive drugs. HCW currently treated with immunosuppressive drugs were not included as controls due to the limited number of participants and the heterogeneity regarding immunosuppressive treatment in this subgroup (
Supplementary Files S1 and S2).
2.4. Statistical Analysis
2.4.1. Stratification Matching
At the exploration step, our data revealed that age, but not gender, and time since the second COVID-19 vaccination were significantly associated with the humoral immune response as quantified by anti-spike IgG (BAU/mL) and neutralization antibody titers (NT) (
Supplementary File S2). To mitigate the confounding effect of age and the time interval since the latest vaccination on the immune response, we applied stratification matching. Herein, randomly selected participants from HCW-healthy and HCW-plus within each age category (18–30, 31–40, 41–50, 51–60, >60 years) and time interval (>6 months or ≤6 months) since the date of sample collection to the second vaccination were matched with individuals from the IBD cohort. We strived to achieve the highest possible matching ratio. Details of the stratification matching for the IBD cohort are provided in
Supplementary File S2.
2.4.2. Descriptive Statistics
Descriptive statistics were presented using median and interquartile range (IQR) from the 25th to the 75th percentile for continuous variables, while frequency (n) and percentage (%) were used for categorical variables. To determine the significant difference in the proportion of respective factors between the IBD cohort and its matched HCW cohorts, the Mann–Whitney U-test was employed for continuous variables, and Pearson’s Chi-square test was used for categorical variables.
When comparing quantitative anti-spike Ig in IBD cohort and its matched HCW cohorts or in different strata among IBD patients, we conducted the Kruskal–Wallis test and afterwards applied the Dwass, Steel, and Critchlow-Fligner method to assess pairwise two-sided multiple comparisons analysis of quantitative anti-spike levels between different strata while controlling for the overall error level.
2.4.3. Multivariable Analysis
To investigate factors associated with quantitative anti-spike Ig among IBD patients, we performed a multivariable Generalized Linear Model (GLM) applying log-nature transformation of anti-spike Ig adjusted for gamma distribution due to the positive-skewed non-normal distribution of anti-spike Ig. All factors associated with a higher quantitative anti-spike Ig (p-value ≤ 0.25) were included in the multivariable GLM. After applying backward elimination and adjusting for age (years), gender, IBD type, and time interval from second vaccination to enrollment, the final multivariable GLM was achieved with no missing co-variates. Results are given as coefficients with their 95% confidence interval (CI) and p-value determining the significance of their respective coefficients obtained from the Wald chi-square test.
Neutralization activities of participants were categorized as non-neutralizing if their neutralization titers (NT) were above the threshold (≥1:10 serum dilution) and as neutralizing if their NT was <1:10 serum dilution. Pearson’s chi-square test was performed to determine the significant difference in the proportion of non-neutralizing NT and neutralizing NT across different strata among IBD patients as well as comparing the IBD cohort with its matched cohorts. In the case of multiple comparisons, Holm–Bonferroni correction for p-value was applied.
To identify the factors associated with non-neutralizing NT among patients with IBD, we performed a multivariable logistic regression. All variables that showed a higher likelihood of non-neutralizing NT (p-value ≤ 0.25) were included in the analysis. The final model was determined after backward elimination and adjusted for gender, age (in years), type of IBD, co-existing underlying diseases, and the time difference (in months) between the second vaccination and enrollment. The odds ratios (OR) and 95% confidence intervals (CI) with their corresponding p-values from the Wald chi-square test are reported.
All statistical tests were conducted with a two-sided significance level of 5%. Statistical analyses were performed using SAS Enterprise Guide 8.1 (Statistical Analysis Software, SAS Institute Inc., Cary, NC, USA) and Prism 10.2.1 (GraphPad Software, Boston, MA, USA).
3. Results
3.1. Characteristics of the Study Population
Out of 4115 participants with serology results in the RisCoin study [
8], inclusion criteria for the immune response analysis and stratification matching were met for 110 of 180 enrolled patients with IBD, for 1512 HCW-healthy, as well as 1262 HCW-plus with underlying diseases and no current immunosuppressive therapy (
Supplementary Files S1 and S2). The 110 IBD patients were matched by age groups and time since the second COVID-19 vaccination to HCW-healthy (n = 306) and HCW-plus (n = 292). Comparison of the cohorts before and after matching is shown in
Supplementary File S2. Almost all IBD patients received advanced therapies, most of them biologics: anti-TNF antibodies (n = 53), ustekinumab, or/and vedolizumab (n = 44). The third subgroup of individuals without biologics treatment consisted of 13 patients treated with kinase inhibitors (tofacitinib, n = 2), with immunomodulators (azathioprine or tacrolimus, n = 5), with prednisolone (less than 20 mg/d, n = 2), and with mesalazine only (n = 4). Given the small number of patients without biologics, these patients were combined into one subgroup and analyzed separately.
The baseline characteristics of the IBD cohort compared to matched HCW-healthy and HCW-plus are shown in
Table 1. There were more females in the HCW-healthy (66%) and HCW-plus (82%) groups compared to the IBD cohort (45%). The median BMI of patients with IBD was higher than that of HCW-healthy individuals, with significant differences in the distribution of BMI categories between the two groups. The frequency and intensity of clinical symptoms after the second COVID-19 vaccination were significantly lower in patients with IBD than in both HCW subgroups. More IBD patients than HCW had received influenza vaccination during the previous winter season (2020/2021). We found significant differences between the IBD and the two HCW-groups regarding regular intake of food supplements, e.g., vitamin D, multivitamins, minerals, trace elements, and fish oil. The percentage of active smokers was significantly higher in IBD patients (20%) than in HCW-healthy (12%) but comparable to HCW-plus participants (17%) (
Table 1).
Further comparison of the matched subgroups regarding different lifestyle factors is given in
Supplementary File S3. IBD patients reported any or regular alcohol consumption less often compared to matched HCW-healthy and HCW-plus participants. With respect to dietary habits, IBD patients reported more frequent consumption of meat compared to the two HCW subgroups, but they consumed fewer portions of vegetables and fruits per day. Twenty percent of IBD patients reported avoiding special foods due to food allergy or intolerance compared to only 4% of HCW-healthy and 8% of HCW-plus participants, both
p < 0.001. Compared to HCW-healthy, significantly fewer patients with IBD reported traveling abroad in the 12 months prior to enrollment. No differences were observed between the groups regarding the frequency of moderate to heavy physical activity per week.
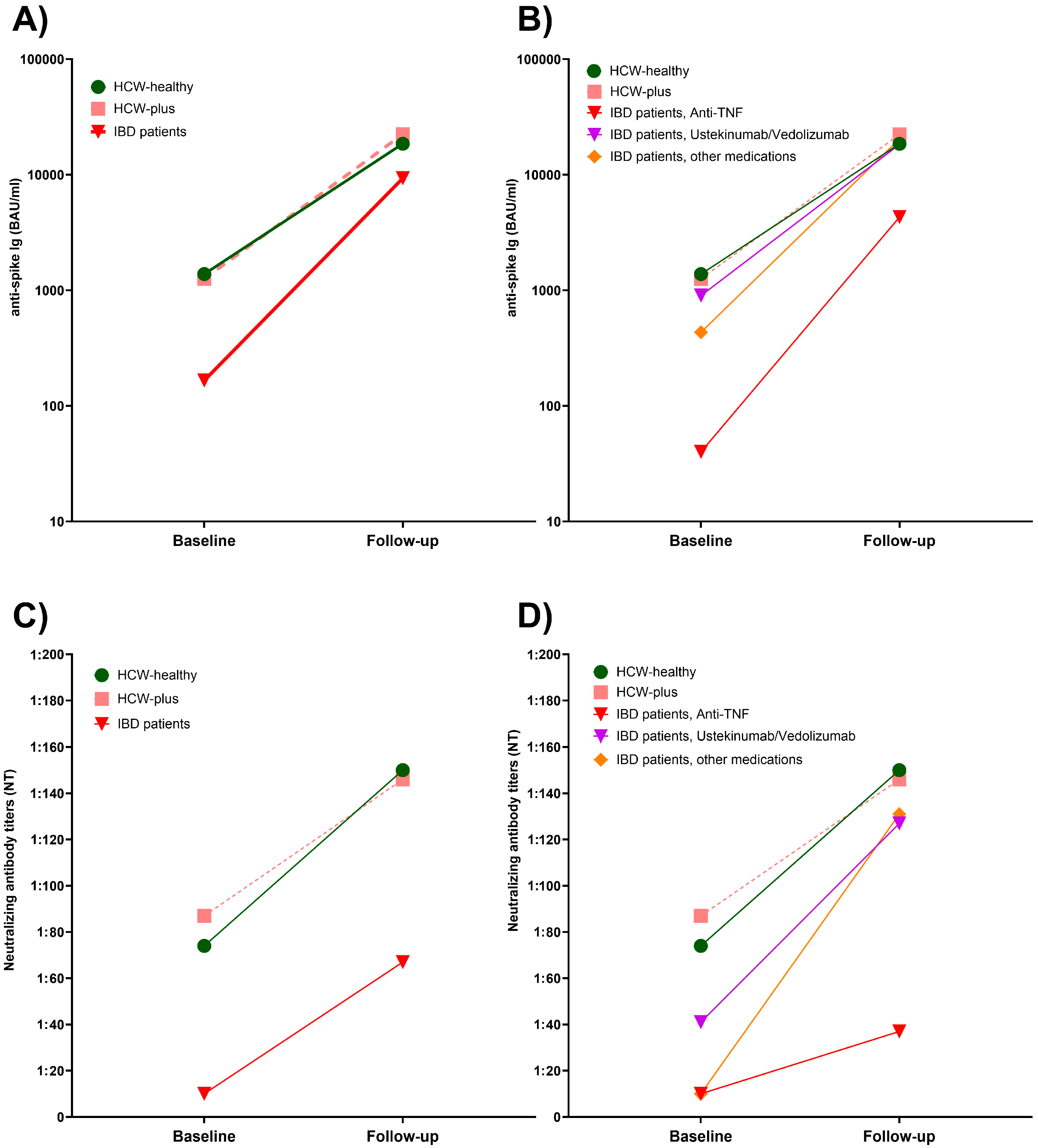
3.2. Comparison of Anti-Spike Ig Titers After Basic Immunization
The quantitative titers of anti-spike Ig antibodies after two COVID-19 mRNA vaccinations in IBD patients showed a larger range with a significantly lower median value compared to the matched HCW-healthy (166 vs. 1384 BAU/mL,
p < 0.001) and HCW-plus subgroup (166 vs. 1258 BAU/mL,
p < 0.001), with no significant difference between the two HCW subgroups regarding anti-spike Ig titers (
Figure 1A). When IBD patients were stratified by medication, only IBD patients treated with anti-TNF antibodies had significantly lower anti-spike Ig titers compared to both HCW groups (both
p < 0.001) and also compared to IBD patients treated with ustekinumab/vedolizumab (
p < 0.001) as well as IBD patients with other medications (
p < 0.001) (
Figure 1B). IBD patients treated with ustekinumab or vedolizumab had anti-spike Ig titers that were comparable to the two HCW subgroups. Patients of the third IBD subgroup (i.e., other medications) had slightly lower antibody titers compared to HCW healthy (
p = 0.018) and HCW-plus (
p = 0.016) (
Figure 1B).
3.3. Factors Associated with Anti-Spike Ig Titers After Basic Immunization in Patients with IBD
We used multivariable generalized linear modeling to identify factors associated with anti-spike-Ig titers after basic immunization in adult IBD patients. Compared to treatment with ustekinumab or vedolizumab, treatment with anti-TNF antibodies was confirmed as the most significant factor associated with lower anti-spike antibody concentrations (OR 0.04; 95% CI: 0.03–0.06,
p < 0.001) (
Table 2). Other factors associated with lower anti-spike Ig level included female versus male gender (
p = 0.004), having chronic pulmonary disease (
p = 0.001), and active smoking behavior (
p = 0.010). The subtype of IBD and the time since the second vaccination showed no significant impact on Ig titers (
Table 2).
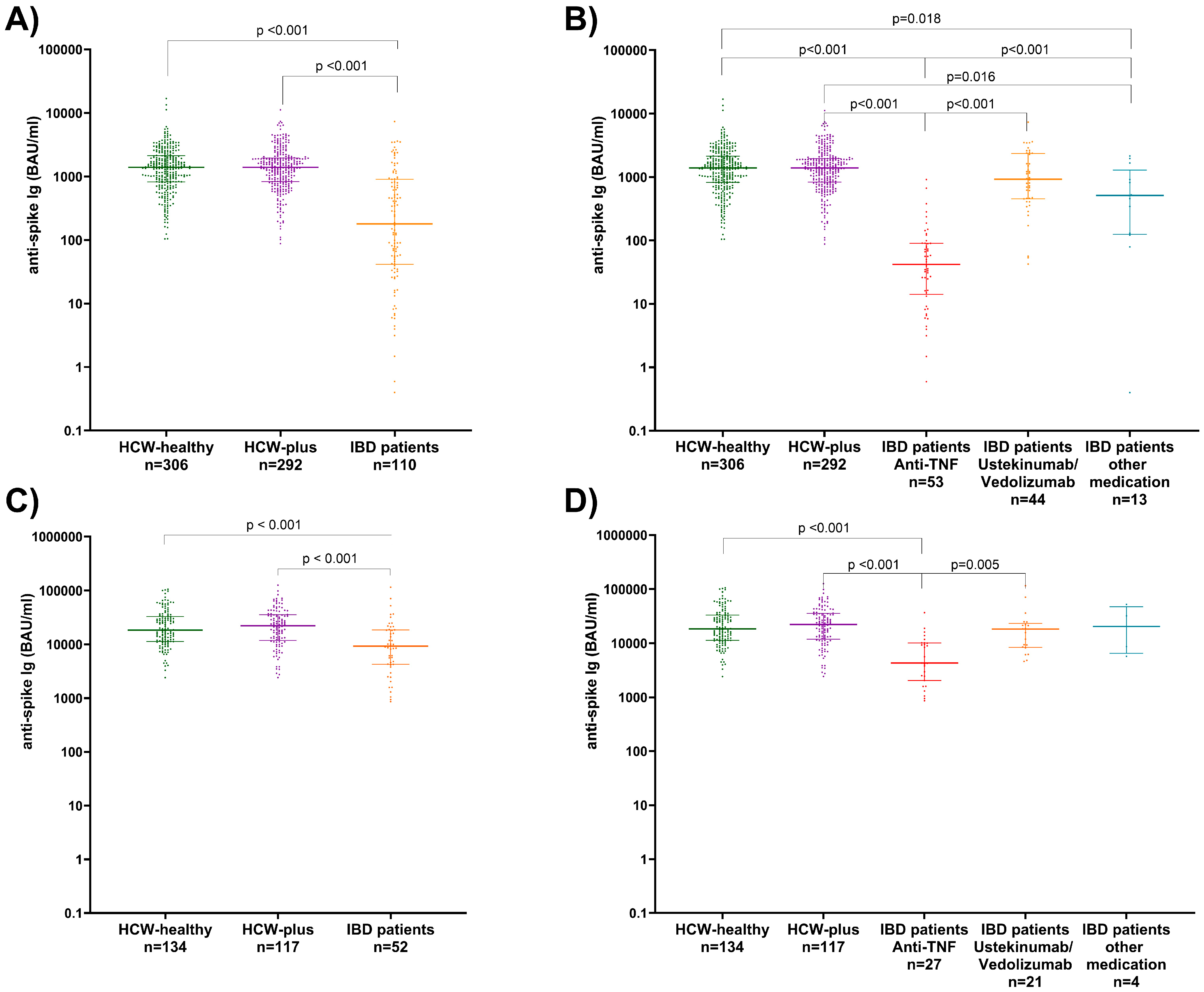
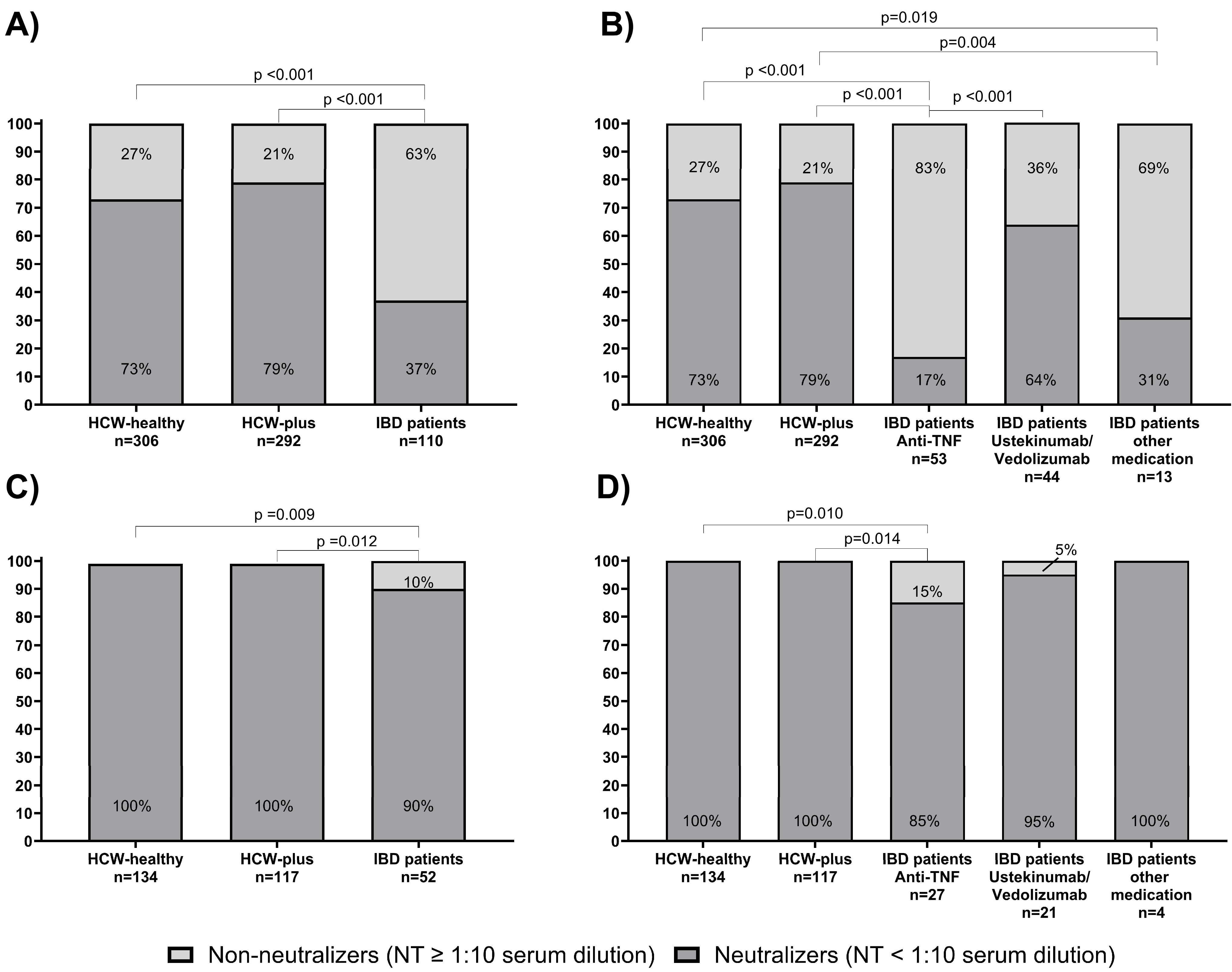
3.4. Comparison of Virus Neutralization Activities After Basic Immunization
The rates of participants with no neutralization activity against SARS-CoV-2 Omicron BA.1 and of confirmed neutralizers after the second vaccination in the three matched groups are depicted in
Figure 2A. Only 37% of IBD patients showed Omicron BA.1-specific neutralization activity compared to 73% of HCW-healthy and 79% of HCW-plus (both
p < 0.001). After stratification of the IBD cohort into subgroups according to their medication, the lowest proportion of patients having neutralization activity against the virus was the anti-TNF group (17%). Patients with ustekinumab or vedolizumab therapy, in comparison, had 64% neutralizers, and patients with other IBD drugs had 31% (
Figure 2B).
3.5. Factors Associated with Insufficient Neutralizing Activities Against SARS-CoV-2 Omicron BA.1 After Basic Immunization in Patients with IBD
When we compared non-neutralizers among the IBD patients with those that showed neutralizing activity against Omicron BA.1, we found no significant relation to gender, age group, BMI, type of IBD, additional morbidity, symptoms after the first or second vaccination, or most assessed lifestyle factors (
Table 3 and
Supplementary File S4). The only significant results in the univariate analysis were the type of IBD medication and smoking behavior.
In the multivariable logistic regression analysis (
Figure 3), these two factors were confirmed to be significantly associated with having non-neutralizing activity against the virus. Patients treated with anti-TNF antibodies had a 16 times higher risk for being non-neutralizers than patients with IBD receiving ustekinumab or vedolizumab treatment (
p < 0.001). Active smokers had a four to five times higher risk than non-smokers or previous smokers (
p = 0.043) (
Figure 3). Age, gender, IBD type, and having another co-morbidity had no impact on the measured NT.
3.6. Follow-Up After the Third Vaccination (Booster)
Blood sampling at least 4 weeks after the third COVID-19 vaccination was performed in 1784 participants (1694 HCW and 90 patients with IBD). After applying the same exclusion criteria as for the initial case-control analysis, 52 patients with IBD remained eligible for analysis. These were matched to 134 HCW-healthy and 117 HCW-plus.
3.7. Comparison of Anti-Spike Ig Concentrations After Booster Vaccination
After the third vaccination, a significant difference in median anti-spike Ig titers remained between patients with IBD (9328 BAU/mL), HCW-healthy (18,553 BAU/mL), and HCW-plus (22,350 BAU/mL), both
p < 0.001 (
Figure 1C). When stratified by medication, only anti-TNF-treated IBD patients had significantly lower anti-spike titers compared to the other subgroups (
Figure 1D).
Figure 4A depicts the median titers of the three matched groups at baseline and after the booster vaccination. As shown here, there was no significant difference in the median anti-SARS-CoV-2 spike levels in HCW-healthy compared to HCW-plus. Although patients with IBD showed a strong increase in antibody concentrations after the booster vaccination, their median titers did not reach levels that were comparable to those of the HCW groups.
Figure 4B demonstrates that an impaired antibody response to booster vaccination was only observed in the subgroup of patients with IBD receiving anti-TNF antibody therapy. After booster vaccination, IBD patients treated with vedolizumab or ustekinumab or other IBD medications reached anti-spike titers that were similar to those in the matched HCW groups.
3.8. Factors Associated with Anti-Spike IgG Titers After the Third Vaccination
Multivariable regression analysis (GLM) confirmed that anti-TNF antibody therapy was a significant risk factor for low anti-spike titers compared to ustekinumab/vedolizumab therapy (
p < 0.001) (
Table 2). In contrast to the analysis after basic immunization, the type of IBD was significantly related to anti-spike titers after adjusting for other possible confounders, with patients with ulcerative colitis having higher titers than those with Crohn’s disease (
p = 0.007).
3.9. Comparison of SARS-CoV-2 Omicron BA.1 Neutralizing Activities After the Third Vaccination
After booster vaccination, all HCW and 90% of IBD patients (85% with anti-TNF therapies, 95% with ustekinumab/vedolizumab, and 100% with other IBD medications) showed neutralizing activity against Omicron BA.1 (
Figure 2C,D). Significant differences in the proportion of individuals with neutralizing activity were found only between patients with IBD receiving anti-TNF therapies and the two HCW groups (
p = 0.010 and
p = 0.014, respectively).
The comparison of neutralization titers at baseline and after booster vaccination in the three matched groups is given in
Figure 4C. Although titers were significantly increased, the median titers after the third vaccinations in IBD patients remained lower than those in the two HCW groups after baseline immunization.
Figure 4D depicts the marked differences according to the IBD medications used. Patients treated with anti-TNF antibodies reached comparably low titers after booster vaccination.
3.10. Perceived Stress Questionnaire Score (PSQ-Score)
The results for the mean total PSQ-Score and for the four specific subdomains in the three matched groups at enrollment are shown in the
Supplementary File S5A–C. The mean total PSQ-Scores in HCW-healthy was 33, which is equal to the mean values found in 334 healthy adults of similar age in a previous publication from Germany [
10]. The mean total score in HCW-plus was significantly higher compared to the HCW-healthy group (43 vs. 33,
p < 0.001) (
Supplementary File S5A). The percentage of HCW-plus individuals with values above 33, indicating increased level of stress, was higher than in HCW-healthy (63% vs. 48%,
p < 0.001) (
Supplementary File S5B). IBD patients showed for the total score and the domains “tension,” “worries,” and “demands” similar values to HCW-healthy individuals but lower scores compared to HCW-plus individuals (
p < 0.018). Values in the domain “joy” were significantly lower in IBD patients compared to HCW-healthy (
p < 0.015) and comparable to those in the HCW-plus group (
Supplementary File S5C).
Figure 4.
Booster effect after the third vaccination on anti-spike levels (A,B) and neutralization titers (NT) (C,D) among adult IBD patients in total (A,C) and after stratification by type of IBD-medication (B,D) as well as in healthy HCW (HCW-healthy) and HCW with underlying diseases (HCW-plus).
Figure 4.
Booster effect after the third vaccination on anti-spike levels (A,B) and neutralization titers (NT) (C,D) among adult IBD patients in total (A,C) and after stratification by type of IBD-medication (B,D) as well as in healthy HCW (HCW-healthy) and HCW with underlying diseases (HCW-plus).
4. Discussion
This study explored the risk factors associated with impaired humoral immune responses to COVID-19 mRNA vaccines in SARS-CoV-2 infection-naïve IBD patients, utilizing data from the RisCoin study [
8]. Beyond medical conditions and medication, we examined the influence of a wide range of demographic and lifestyle factors [
8]. The large number of HCW included in the original study (see
Supplementary File S1) enabled us to create two well-matched control groups (matched in a 1:3 ratio): one consisting of healthy HCW and the other comprising HCW with underlying medical conditions. This approach effectively mitigated the confounding effects of age and temporal distance to the latest vaccination on humoral immune responses [
15].
Our findings reveal that IBD patients under immunosuppressive medication with anti-TNF antibodies exhibit significantly lower median anti-spike concentrations after basic immunization compared to both HCW control groups and to IBD patients treated with ustekinumab/vedolizumab. The differential effect of these therapies on vaccine-induced humoral immunity is consistent with previous publications [
16,
17,
18]. Neutralizing antibody titers, a key correlate of protection, were similarly affected with only 17% of IBD patients on anti-TNF therapies achieving neutralizing activities against SARS-CoV-2 Omicron BA.1 above threshold after basic immunization, compared to over 70% in both HCW groups and 65% in patients on ustekinumab/vedolizumab therapies. Multivariable regression analysis confirmed that anti-TNF therapy was the strongest negative predictor of anti-spike levels and neutralization titers, which is in line with recent literature [
16,
19].
The booster vaccination significantly improved antibody responses across all groups, but IBD patients on anti-TNF therapy continued to show significantly lower median anti-spike antibody levels and neutralization activities compared to HCW, with still 15% of them being non-neutralizers. Notably, under anti-TNF-therapies, the median NT after booster remained lower than titers in HCW after basic immunization (
Figure 4D). Our results are in accordance with existing data on the efficacy of booster vaccination in patients with impaired humoral responses due to anti-TNF therapies [
16,
18,
20,
21]. Taken together, these data combined with the previously observed accelerated decline of antibody titers under anti-TNF therapies [
17] sustain an individualized vaccination schedule with (repeated) booster vaccination to improve and extend immune responses in IBD patients receiving anti-TNF therapies. In contrast, patients receiving ustekinumab or vedolizumab achieved antibody levels comparable to HCWs, suggesting that mRNA vaccine booster doses may effectively overcome some of the immunosuppressive effects associated with these treatments. Due to the small number of IBD patients treated with other drugs in our cohort, e.g., tofacitinib and immunomodulators, our study does not allow for any conclusions regarding their association with the humoral immune response.
The marked impairment of SARS-CoV-2 neutralization activities among anti-TNF-treated IBD patients is a critical finding, as these could potentially lead to dismal protection from symptomatic SARS-CoV-2 infection and severe COVID-19 [
12,
13]. Reduced neutralization capacities may contribute to reduced viral clearance and longer-term infections, which may favor virus adaptation to the host adaptation and the evolution of novel virus variants [
22]. Repeated booster vaccination with variant adapted vaccines could be beneficial for patients treated with anti-TNF, and mucosal vaccination strategies should emerge [
16,
21].
Besides medication, our study evaluated the impact on humoral vaccine response of a wide variety of demographic factors, dietary habits, regular intake of vitamins and supplements, lifestyle factors including tobacco and alcohol consumption, and co-morbidities. Among the investigated factors, female gender, chronic pulmonary disease, and active smoking status were independently associated with lower anti-spike antibody concentrations after basic immunization, while smoking status was associated with showing no neutralization activity. After booster vaccination, all these factors lost their significant impact, but the phenotype of Crohn’s disease was associated with lower antibody titers compared to ulcerative colitis. Although in line with another publication [
19], this finding should be interpreted with caution, given the small number of participants at follow-up.
Besides the known male bias for COVID-19 severity and mortality [
23], sex differences have also been described for immunogenicity, with females having higher antibody titers than males after conventional [
24] and mRNA vaccinations [
25]. In our IBD cohort, female gender was associated with lower spike antibody titers after basic immunization, which may have resulted in a selection bias.
Having a chronic pulmonary disease and active smoking behavior were independent risk factors for lower anti-spike antibody titers after basic immunization in patients with IBD. Current smoking was associated with a four to five times higher risk for being a non-neutralizer after basic immunization. Twenty percent of our IBD patients were current smokers, despite the known negative effects of smoking on the course of IBD [
26]. This percentage was higher compared to the 8–9% reported in an IBD cohort from UK [
19]. The observation of an impaired humoral immune response to mRNA vaccination in active smokers is in line with data in patients with IBD and various other disease entities and healthy control populations [
20,
27,
28], confirmed by meta-analyses [
29]. An individualized vaccine schedule should also consider active smoking in patients with IBD. These individuals are also prone to a more severe disease course, increased rates of hospitalization and surgery, and the need for more aggressive immunosuppressive therapies [
30].
Our study design allowed us to perform a comprehensive dietary, lifestyle, and perceived stress analysis in patients with IBD compared to HCW during the COVID-19 pandemic. As expected, we found significant differences between groups regarding regular intake of vitamin D supplements, reflecting recommendations given in our IBD clinic. A higher proportion of patients with IBD reported avoidance of special foods and consuming fewer portions of vegetables and fruits per day, which, although not advisable, is an expected finding [
31]. Complete avoidance of alcohol was more often reported in IBD patients compared to controls, although data about its harmful effect in IBD are less solid than for smoking. The higher median BMI observed in the IBD cohort is most likely multifactorial (e.g., systemic inflammation, steroid use, or reduced physical activity) [
32], but like smoking, this calls for more attention and counseling in clinical care. The reported avoidance of traveling aboard among IBD patients may be related to a more precautious life style due to a higher self-estimated risk during the pandemic [
1].
Our patients with IBD performed well in the PSQ, obtaining comparable values with healthy HCW for the domains “tension,” “worries,” and “demands” and lower scores compared to HCW with associated medical conditions (HCW-plus). This may partly be attributed to our regular newsletter updates on scientific findings and recommendations for patients with IBD during the pandemic [
1]. The self-perceived stress level was lower compared to that of 144 IBD patients enrolled in the validation study of the German short version of PSQ [
10]. However, that study was performed 20 years ago, before the availability of most current IBD drugs with a more favorable benefit-to-harm ratio.
The reduced frequency and intensity of clinical symptoms after the second COVID-19 vaccination in IBD patients compared to HCW groups indicate the blunted immune response in this population, potentially due to immunosuppressive therapies [
33]. The good tolerability of the vaccine and the fact that IBD patients already had higher rates of influenza vaccination predict a good acceptance of COVID-19 vaccination in the IBD population. Indeed, current observations confirm an overall positive attitude toward COVID-19 vaccination in IBD patients, which is an encouraging finding [
34].
Our study has several strengths. The use of well-matched control groups and stratification based on age and vaccination timing reduced potential confounding effects. Only participants who received a homologous mRNA vaccine regimen for primary immunization and booster doses were included. Additionally, individuals with known prior SARS-CoV-2 infection or positive nucleocapsid antibodies were excluded. This eliminated the effects of heterologous vaccination or hybrid immunity, both of which have been shown to impact vaccine response [
35,
36,
37]. Limitations include female dominance in the HCW cohort, which did not allow a 3:1 matching with the IBD patients, and a high loss rate of approximately 50% of our cohort until the follow-up. This was in part due to exclusions of participants who had COVID-19 between the baseline and the follow-up time points.
5. Conclusions
In conclusion, our analysis, conducted in a homogenous and well-matched cohort study, adds to the existing research by confirming the impaired humoral responses to COVID-19 mRNA vaccination in patients with IBD receiving anti-TNF-alpha immunosuppressive therapies. Furthermore, it identifies smoking as an independent risk factor for impaired vaccine immunogenicity in this group. Vaccines based on mRNA technology have been applied for the first time on a large scale against COVID-19. Due to their various advantages compared to conventional vaccines [
38], we expect them to be used in the future against several other infections. Therefore, our findings may not be restricted to mRNA vaccines against SARS-CoV-2. Our findings sustain the implementation of individualized vaccine schedules in patients with different immunosuppressive therapies and encourage consideration of the smoking status. These findings also highlight the need for targeted interventions, such as smoking cessation programs and nutritional counseling, to optimize not only health but also vaccine responses in patients with IBD.
Supplementary Materials
The following supporting information can be downloaded at
https://www.mdpi.com/article/10.3390/vaccines13070673/s1: Supplementary File S1: Flowchart for analysis of the IBD group of the RisCoin Study; Supplementary File S2: Stratification matching for IBD cohort; Supplementary File S3: Dietary habits and lifestyle factors among IBD patients, healthy HCW (HCW-healthy), and HCW with underlying diseases (HCW-plus); Supplementary File S4: Antibody neutralization titers (NT) after the second COVID-19 vaccination in adult patients with IBD categorized non-neutralizing (NT ≥ 1:10 serum dilution) or neutralizing (NT < 1:10 serum dilution) according to different dietary habits and lifestyle factors; Supplementary File S5: PSQ—Score in healthy HCW (HCW-healthy), HCW with underlying diseases (HCW-plus), and adult patients with IBD (A). Frequency of lower (≤33) or higher (>33) stress (B) and PSQ score based on the different determined domains (C).
Author Contributions
Conceptualization, A.C., V.H., O.T.K., K.A., H.P.T. and S.K.; data curation, T.G.L.T. and S.K.; formal analysis, K.C. and T.G.L.T.; funding acquisition, A.C., V.H., O.T.K., K.A., H.P.T. and S.K.; investigation, K.C., L.K., P.R.W., A.Z., S.B., M.S., G.L., T.S., A.C., O.T.K., K.A., H.P.T. and S.K.; methodology, T.G.L.T., O.T.K., H.P.T. and S.K.; project administration, K.A. and S.K.; resources, O.T.K., K.A., H.P.T. and S.K.; software, T.G.L.T. and S.K.; supervision, H.P.T. and S.K.; validation, K.C., L.K., T.G.L.T., A.Z., H.P.T. and S.K.; visualization, K.C. and T.G.L.T.; writing—original draft, K.C. and L.K.; writing—review and editing, K.C., L.K., T.G.L.T., P.R.W., A.Z., S.B., M.S., G.L., T.S., A.C., V.H., O.T.K., K.A., H.P.T. and S.K. All authors have read and agreed to the published version of the manuscript.
Funding
The RisCoin study was funded by research grants from the German Federal Ministry of Health (Bundesministerium für Gesundheit, BMG) (K.A., S.K.: ZMI1-2521COR933-BMG), the Corona Research Program 21/22 of the Bavarian Ministry of Science and Art (Bayerisches Staatsministerium für Wissenschaft und Kunst), and intramural and extramural funding of participating research groups (A.C. has been co-funded by the Ministry of Economic and Climate Action #50WB2222, S.K. has been funded for the KoCo19-CED Study by the Bayerisches Staatsministerium für Wissenschaft und Kunst). The researchers are independent of the funders. The study funders had no role in the study design, data analysis, interpretation of data, or writing of this manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (or Ethics Committee) of the LMU Munich, study protocol on 21 September 2021 (Project Number: 21-0839), amendments on 22 February 2022, and 4 May 2022.
Informed Consent Statement
Written informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Datasets can be made available in an irreversibly anonymized format upon reasonable request to the principal investigators.
Acknowledgments
The authors thank all healthcare workers and patients participating in the RisCoin study for their cooperation. We thank the teams of the Emergency Department, LMU University Hospital, LMU Munich (M. Klein), and of the Institute for Infectious Diseases and Tropical Medicine, LMU University Hospital, LMU Munich (M. Hoelscher, C. Janke, C. Reinkemeyer, I. Noreña) for their support in recruiting participants and their collaboration. We thank the leaders of the Work Package 8 of the COVIM project (L. E. Sanders, Berlin and F. Klein, Cologne) for allowing us to use parts of the questionnaire developed for their study to characterize the participants for later comparison. We are grateful to the board members and colleagues in the administration and medical departments of the University hospital, particularly M. Lerch and S. Horster, for providing RisCoin study facilities to recruit hospital employees. We acknowledge the contribution of students, physicians, and scientific staff who helped in the study logistics and recruitment and follow-up of participants (Biener I., Boeing B., Brammer M., Brüseke J., Camci H., Choukér M.-T., Choukér M., D’Amico F., Deutinger M., De Zen F., Faro T., Geist M., Haesner-Stricker C., Han B., Hao Y., Heynckes S., Hölz H., Huppert K., Jurk A., Kaufmann A., Kamm L., Kavrakova I., Knabe R., Klucker E., Kriesel F., Litwin A., Matzel S., Öztan G.N., Rech J., Rosenberger S., Ruf J., Said-Fabry A., Shabani R., Socas K., Späth P., Tsvetkova R., Tuschen M., Wohrle T., and Tu L.) and medical students. We appreciate Castor EDC for providing us with the electronic data capture system free of charge in their framework of joining the global fight against SARS-CoV-2. We gratefully acknowledge the kind support of our IT experts, Wichert S. and Endres S., and the CentraXX project team of KAIROS GmbH in establishing the CentraXX Study App at our LMU University Hospital, LMU Munich. Members of RisCoin Study Group: O. Keppler, A. Osterman, I. Badell Garcia, M. Huber, P. R. Wratil, A. Gryaznova, T. Jebrini, P. Kohl, S. De Jonge, K. Neumeier, S. Koletzko, B. Koletzko, S. Kim-Helmuth, Y. Hao, J. Horak, S. Koletzko, K. Csollarova, T.G. Le Thi, T. Schwerd, H.P. Török, L. Koletzko, S. Breiteneicher, A. Choukér, M. Tuschen, K. Biere, T. Wöhrle, S. Matzel, M. Hörl, M. Moser, V. Hornung, J. Rech, C. Ludwig, L. Hansbauer, A. Zhelyazkova, M. Klein, S. Völk, S. Kim-Helmuth, B. Puzek, and G. Kastenmüller.
Conflicts of Interest
L.K. reports consultant fees from Janssen-Cilag and Takeda and lecture honoraria from Falk Foundation outside the submitted work. TS received lecture honoraria from Nutricia and MSD, travel support from AbbVie and Ferring, and consulting fees from AstraZeneca outside the submitted work. H.P.T. reports consultant fees from AbbVie, Calypso Biotech, Immunic Janssen-Cilag, and Pharmacosmos and lecture honoraria from AbbVie, Biogen, BMS, Falk Foundation, Galapagos, Janssen-Cilag Pfizer, Pharmacosmos, and Takeda Pharma outside the submitted work. SK reports personal fees from AbbVie, AstraZeneca, Danone, Janssen, Mead Johnson, Nestle Nutrition, Pfizer, Sanofi, Takeda, and Tillotts outside the submitted work. All authors declare no conflicts of interest to this published work. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Abbreviations
The following abbreviations are used in this manuscript:
| CI | confidence interval |
| FU | follow-up |
| GLM | Generalized Linear Model |
| HCW | healthcare workers |
| HCW-healthy | healthcare workers without comorbidities |
| HCW-plus | healthcare workers with medical conditions |
| IBD | inflammatory bowel disease |
| IQR | interquartile range |
| NT | neutralization antibody titers |
| PSQ | Perceived Stress Questionnaire |
References
- Koletzko, L.; Klucker, E.; Le Thi, T.G.; Breiteneicher, S.; Rubio-Acero, R.; Neuhaus, L.; Stark, R.G.; Standl, M.; Wieser, A.; Török, H. Following pediatric and adult IBD patients through the COVID-19 pandemic: Changes in psychosocial burden and perception of infection risk and harm over time. J. Clin. Med. 2021, 10, 4124. [Google Scholar] [CrossRef] [PubMed]
- Amiot, A.; Rahier, J.-F.; Baert, F.; Nahon, S.; Hart, A.; Viazis, N.; Biancone, L.; Domenech, E.; Reenears, C.; Peyrin-Biroulet, L. The impact of COVID-19 on patients with IBD in a prospective European cohort study. J. Crohn’s Colitis 2023, 17, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, C.; Stallmach, A.; Sturm, A.; Bachmann, O.; Helwig, U.; Koletzko, S.; Lynen, P.; Schnoy, E.; Dignass, A.; Kucharzik, T. Update: Addendum to S3-Guidelines Crohn disease and ulcerative colitis: Management of Patients with Inflammatory Bowel Disease with regard to COVID-19 (version 2.0). Z. Gastroenterol. 2024, 62, 517–534. [Google Scholar] [PubMed]
- Long, M.D.; Parlett, L.; Lewis, J.D.; Haynes, K.; Adimadhyam, S.; Hou, L.; Wolfe, A.; Toh, S.; Burris, J.; Dorand, J.; et al. Corticosteroids but not Anti-TNF Are Associated With Increased COVID-19 Complications in Patients With Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2024, 30, 1345–1352. [Google Scholar] [CrossRef]
- Brenner, E.J.; Ungaro, R.C.; Gearry, R.B.; Kaplan, G.G.; Kissous-Hunt, M.; Lewis, J.D.; Ng, S.C.; Rahier, J.-F.; Reinisch, W.; Ruemmele, F.M. Corticosteroids, but not TNF antagonists, are associated with adverse COVID-19 outcomes in patients with inflammatory bowel diseases: Results from an international registry. Gastroenterology 2020, 159, 481–491.e483. [Google Scholar] [CrossRef]
- Rubin, D.T.; Abreu, M.T.; Rai, V.; Siegel, C.A.; Ahuja, V.; Allez, M.; Ananthakrishnan, A.N.; Bernstein, C.N.; Braun, J.G.; Chowers, Y. Management of patients with Crohn’s disease and ulcerative colitis during the coronavirus disease-2019 pandemic: Results of an international meeting. Gastroenterology 2020, 159, 6–13.e16. [Google Scholar] [CrossRef]
- Kennedy, N.A.; Jones, G.-R.; Lamb, C.A.; Appleby, R.; Arnott, I.; Beattie, R.M.; Bloom, S.; Brooks, A.J.; Cooney, R.; Dart, R.J. British Society of Gastroenterology guidance for management of inflammatory bowel disease during the COVID-19 pandemic. Gut 2020, 69, 984–990. [Google Scholar] [CrossRef]
- Koletzko, S.; Le Thi, T.G.; Zhelyazkova, A.; Osterman, A.; Wichert, S.P.; Breiteneicher, S.; Koletzko, L.; Schwerd, T.; Völk, S.; Jebrini, T.; et al. A prospective longitudinal cohort study on risk factors for COVID-19 vaccination failure (RisCoin): Methods, procedures and characterization of the cohort. Clin. Exp. Med. 2023, 23, 4901–4917. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Levenstein, S.; Klapp, B.F. Validierung des “Perceived Stress Questionnaire“ (PSQ) an einer deutschen Stichprobe. Diagnostica 2001, 47, 142–152. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Walter, O.B.; Kocalevent, R.D.; Weber, C.; Klapp, B.F. The Perceived Stress Questionnaire (PSQ) reconsidered: Validation and reference values from different clinical and healthy adult samples. Psychosom. Med. 2005, 67, 78–88. [Google Scholar] [CrossRef]
- Wratil, P.R.; Le Thi, T.G.; Osterman, A.; Badell, I.; Huber, M.; Zhelyazkova, A.; Wichert, S.P.; Litwin, A.; Hörmansdorfer, S.; Strobl, F.; et al. Dietary habits, traveling and the living situation potentially influence the susceptibility to SARS-CoV-2 infection: Results from healthcare workers participating in the RisCoin Study. Infection 2024, 52, 1425–1437. [Google Scholar] [CrossRef] [PubMed]
- Keppler-Hafkemeyer, A.; Greil, C.; Wratil, P.R.; Shoumariyeh, K.; Stern, M.; Hafkemeyer, A.; Ashok, D.; Hollaus, A.; Lupoli, G.; Priller, A. Potent high-avidity neutralizing antibodies and T cell responses after COVID-19 vaccination in individuals with B cell lymphoma and multiple myeloma. Nat. Cancer 2023, 4, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Wratil, P.R.; Stern, M.; Priller, A.; Willmann, A.; Almanzar, G.; Vogel, E.; Feuerherd, M.; Cheng, C.-C.; Yazici, S.; Christa, C. Three exposures to the spike protein of SARS-CoV-2 by either infection or vaccination elicit superior neutralizing immunity to all variants of concern. Nat. Med. 2022, 28, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Muenchhoff, M.; Mairhofer, H.; Nitschko, H.; Grzimek-Koschewa, N.; Hoffmann, D.; Berger, A.; Rabenau, H.; Widera, M.; Ackermann, N.; Konrad, R.; et al. Multicentre comparison of quantitative PCR-based assays to detect SARS-CoV-2, Germany, March 2020. Euro Surveill. 2020, 25, 2001057. [Google Scholar] [CrossRef]
- Tober-Lau, P.; Schwarz, T.; Vanshylla, K.; Hillus, D.; Gruell, H.; Suttorp, N.; Landgraf, I.; Kappert, K.; Seybold, J.; Drosten, C. Long-term immunogenicity of BNT162b2 vaccination in older people and younger health-care workers. Lancet Respir. Med. 2021, 9, e104–e105. [Google Scholar] [CrossRef]
- Alexander, J.L.; Kennedy, N.A.; Ibraheim, H.; Anandabaskaran, S.; Saifuddin, A.; Castro Seoane, R.; Liu, Z.; Nice, R.; Bewshea, C.; D’Mello, A.; et al. COVID-19 vaccine-induced antibody responses in immunosuppressed patients with inflammatory bowel disease (VIP): A multicentre, prospective, case-control study. Lancet Gastroenterol. Hepatol. 2022, 7, 342–352. [Google Scholar] [CrossRef]
- Lin, S.; Kennedy, N.A.; Saifuddin, A.; Sandoval, D.M.; Reynolds, C.J.; Seoane, R.C.; Kottoor, S.H.; Pieper, F.P.; Lin, K.M.; Butler, D.K.; et al. Antibody decay, T cell immunity and breakthrough infections following two SARS-CoV-2 vaccine doses in inflammatory bowel disease patients treated with infliximab and vedolizumab. Nat. Commun. 2022, 13, 1379. [Google Scholar] [CrossRef]
- Liu, Z.; Le, K.; Zhou, X.; Alexander, J.L.; Lin, S.; Bewshea, C.; Chanchlani, N.; Nice, R.; McDonald, T.J.; Lamb, C.A.; et al. Neutralising antibody potency against SARS-CoV-2 wild-type and omicron BA.1 and BA.4/5 variants in patients with inflammatory bowel disease treated with infliximab and vedolizumab after three doses of COVID-19 vaccine (CLARITY IBD): An analysis of a prospective multicentre cohort study. Lancet Gastroenterol. Hepatol. 2023, 8, 145–156. [Google Scholar] [CrossRef]
- Liu, Z.; Alexander, J.L.; Le, K.; Zhou, X.; Ibraheim, H.; Anandabaskaran, S.; Saifuddin, A.; Lin, K.W.; McFarlane, L.R.; Constable, L.; et al. Neutralising antibody responses against SARS-CoV-2 Omicron BA.4/5 and wild-type virus in patients with inflammatory bowel disease following three doses of COVID-19 vaccine (VIP): A prospective, multicentre, cohort study. EClinicalMedicine 2023, 64, 102249. [Google Scholar] [CrossRef]
- Geldof, J.; Truyens, M.; Sabino, J.; Ferrante, M.; Lambert, J.; Lapeere, H.; Hillary, T.; Van Laethem, A.; de Vlam, K.; Verschueren, P. Did We Overreact? Insights on COVID-19 Disease and Vaccination in a Large Cohort of Immune-Mediated Inflammatory Disease Patients during Sequential Phases of the Pandemic (The BELCOMID Study). Vaccines 2024, 12, 1157. [Google Scholar] [CrossRef]
- Woelfel, S.; Dütschler, J.; Junker, D.; König, M.; Leinenkugel, G.; Graf, N.; Krieger, C.; Truniger, S.; Franke, A.; Koller, S. Systemic and mucosal immunogenicity of monovalent XBB. 1.5-adapted COVID-19 mRNA vaccines in patients with inflammatory bowel disease. Vaccines 2024, 12, 774. [Google Scholar] [CrossRef] [PubMed]
- Markov, P.V.; Ghafari, M.; Beer, M.; Lythgoe, K.; Simmonds, P.; Stilianakis, N.I.; Katzourakis, A. The evolution of SARS-CoV-2. Nat. Rev. Microbiol. 2023, 21, 361–379. [Google Scholar] [CrossRef] [PubMed]
- Takahashi, T.; Ellingson, M.K.; Wong, P.; Israelow, B.; Lucas, C.; Klein, J.; Silva, J.; Mao, T.; Oh, J.E.; Tokuyama, M. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature 2020, 588, 315–320. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Jedlicka, A.; Pekosz, A. The Xs and Y of immune responses to viral vaccines. Lancet Infect. Dis. 2010, 10, 338–349. [Google Scholar] [CrossRef]
- Bachmann, M.; Gültekin, N.; Stanga, Z.; Fehr, J.S.; Ülgür, I.I.; Schlagenhauf, P. Disparities in response to mRNA SARS-CoV-2 vaccines according to sex and age: A systematic review. N. Microbes N. Infect. 2024, 63, 101551. [Google Scholar] [CrossRef]
- Noble, A.J.; Nowak, J.K.; Adams, A.T.; Uhlig, H.H.; Satsangi, J. Defining Interactions Between the Genome, Epigenome, and the Environment in Inflammatory Bowel Disease: Progress and Prospects. Gastroenterology 2023, 165, 44–60.e42. [Google Scholar] [CrossRef]
- Şen, S.; Arslan, G.; Tütüncü, M.; Demir, S.; Dinç, Ö.; Gündüz, T.; Uzunköprü, C.; Gümüş, H.; Tütüncü, M.; Akçin, R.; et al. The Effect of Smoking on Inactivated and mRNA Vaccine Responses Applied to Prevent COVİD-19 in Multiple Sclerosis. Noro Psikiyatr. Ars. 2023, 60, 252–256. [Google Scholar] [CrossRef]
- Mori, Y.; Tanaka, M.; Kozai, H.; Hotta, K.; Aoyama, Y.; Shigeno, Y.; Aoike, M.; Kawamura, H.; Tsurudome, M.; Ito, M. Antibody response of smokers to the COVID-19 vaccination: Evaluation based on cigarette dependence. Drug Discov. Ther. 2022, 16, 78–84. [Google Scholar] [CrossRef]
- Valeriani, F.; Protano, C.; Pozzoli, A.; Vitale, K.; Liguori, F.; Liguori, G.; Gallè, F. Does Tobacco Smoking Affect Vaccine-Induced Immune Response? A Systematic Review and Meta-Analysis. Vaccines 2024, 12, 1260. [Google Scholar] [CrossRef]
- Caron, B.; Honap, S.; Peyrin-Biroulet, L. Epidemiology of inflammatory bowel disease across the ages in the era of advanced therapies. J. Crohn’s Colitis 2024, 18, ii3–ii15. [Google Scholar] [CrossRef]
- Kaliora, A.C. Nutrition in inflammatory bowel diseases; Is there a role? Best. Pract. Res. Clin. Gastroenterol. 2023, 62–63, 101827. [Google Scholar] [CrossRef] [PubMed]
- Hyun, H.K.; Cheon, J.H. Metabolic Disorders and Inflammatory Bowel Diseases. Gut Liver 2025, 19, 307–317. [Google Scholar] [CrossRef] [PubMed]
- Simon, D.; Tascilar, K.; Kleyer, A.; Fagni, F.; Krönke, G.; Meder, C.; Dietrich, P.; Orlemann, T.; Kliem, T.; Mößner, J.; et al. Impact of Cytokine Inhibitor Therapy on the Prevalence, Seroconversion Rate, and Longevity of the Humoral Immune Response Against SARS-CoV-2 in an Unvaccinated Cohort. Arthritis Rheumatol. 2022, 74, 783–790. [Google Scholar] [CrossRef] [PubMed]
- Mastrangeli, G.; Vernia, F.; Necozione, S.; Muselli, M.; Frassino, S.; Cesaro, N.; Latella, G.; Fabiani, L. Vaccine Acceptance in Patients with Inflammatory Bowel Disease: Lessons Learned from the COVID-19 Pandemic. Vaccines 2024, 12, 551. [Google Scholar] [CrossRef]
- Mrak, D.; Sieghart, D.; Simader, E.; Tobudic, S.; Radner, H.; Mandl, P.; Göschl, L.; Koblischke, M.; Hommer, N.; Wagner, A. Heterologous vector versus homologous mRNA COVID-19 booster vaccination in non-seroconverted immunosuppressed patients: A randomized controlled trial. Nat. Commun. 2022, 13, 5362. [Google Scholar] [CrossRef]
- Alexander, J.L.; Liu, Z.; Sandoval, D.M.; Reynolds, C.; Ibraheim, H.; Anandabaskaran, S.; Saifuddin, A.; Seoane, R.C.; Anand, N.; Nice, R. COVID-19 vaccine-induced antibody and T-cell responses in immunosuppressed patients with inflammatory bowel disease after the third vaccine dose (VIP): A multicentre, prospective, case-control study. Lancet Gastroenterol. Hepatol. 2022, 7, 1005–1015. [Google Scholar] [CrossRef]
- Goldberg, Y.; Mandel, M.; Bar-On, Y.M.; Bodenheimer, O.; Freedman, L.S.; Ash, N.; Alroy-Preis, S.; Huppert, A.; Milo, R. Protection and waning of natural and hybrid immunity to SARS-CoV-2. N. Engl. J. Med. 2022, 386, 2201–2212. [Google Scholar] [CrossRef]
- Pardi, N.; Hogan, M.J.; Weissman, D. Recent advances in mRNA vaccine technology. Curr. Opin. Immunol. 2020, 65, 14–20. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).