Pediatric Rotavirus Hospitalization Rates in the Military Health System Before and During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
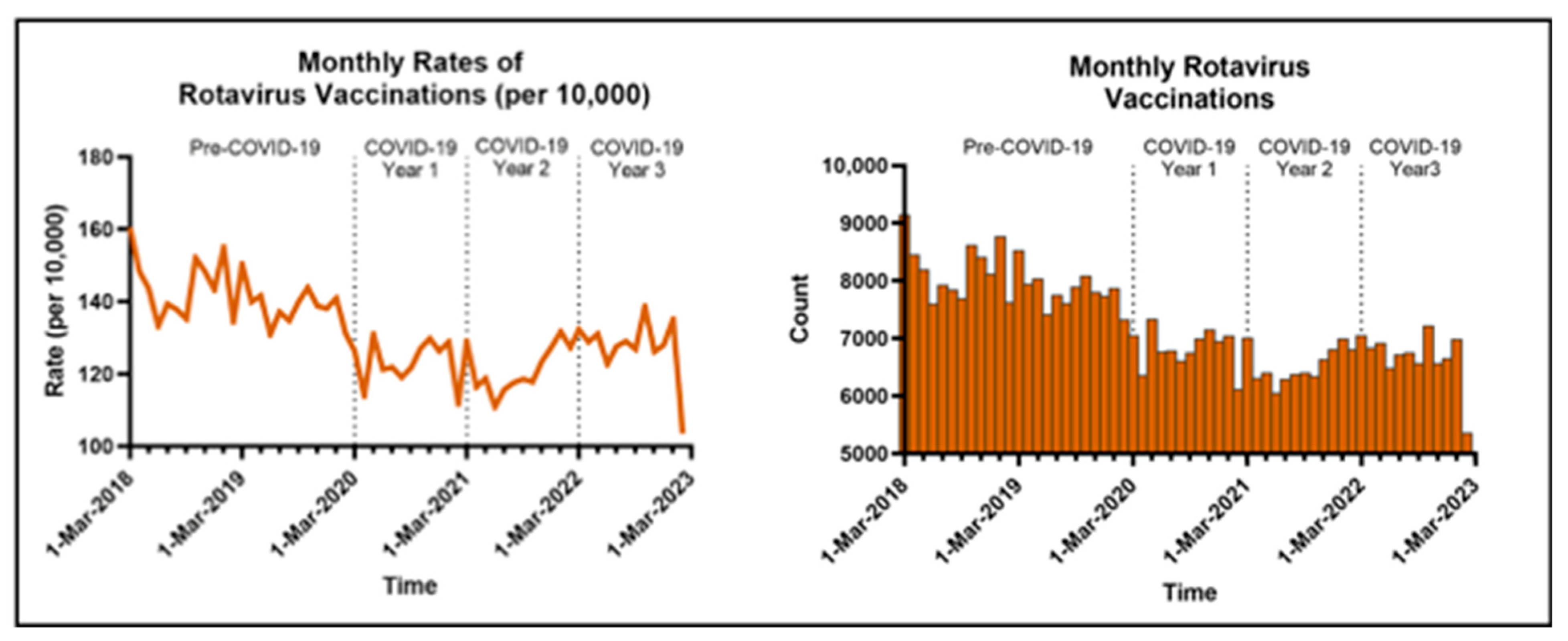
3. Results
Rotavirus Hospitalizations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| MDR | Military Health System Data Repository |
| US | United States |
| NPI | Non-pharmaceutical Intervention |
| AGI | Acute Gastrointestinal Illness |
| MHS | Military Health System |
| ICD-10 | International Classification of Diseases 10th Revision |
| CPT | Current Procedural Terminology |
| RR | Rate Ratio |
| CI | 95% Confidence Intervals |
| DTaP | Diphtheria, Tetanus, and acellular Pertussis |
References
- Tate, J.E.; Burton, A.H.; Boschi-Pinto, C.; Parashar, U.D. Global, Regional, and National Estimates of Rotavirus Mortality in Children <5 Years of Age, 2000–2013. Clin. Infect. Dis. 2016, 62 (Suppl. S2), S96–S105. [Google Scholar] [CrossRef] [PubMed]
- Troeger, C.; Khalil, I.A.; Rao, P.C.; Cao, S.; Blacker, B.F.; Ahmed, T.; Armah, G.; Bines, J.E.; Brewer, T.G.; Colombara, D.V.; et al. Rotavirus Vaccination and the Global Burden of Rotavirus Diarrhea Among Children Younger Than 5 Years. JAMA Pediatr. 2018, 172, 958–965. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.P.; Dahl, R.M.; Parashar, U.D.; Lopman, B.A. Annual changes in rotavirus hospitalization rates before and after rotavirus vaccine implementation in the United States. PLoS ONE 2018, 13, e0191429. [Google Scholar] [CrossRef] [PubMed]
- Pindyck, T.; Tate, J.E.; Parashar, U.D. A decade of experience with rotavirus vaccination in the United States—vaccine uptake, effectiveness, and impact. Expert. Rev. Vaccines 2018, 17, 593–606. [Google Scholar] [CrossRef]
- Burnett, E.; Parashar, U.D.; Winn, A.; Tate, J.E. Trends in Rotavirus Laboratory Detections and Internet Search Volume Before and After Rotavirus Vaccine Introduction and in the Context of the Coronavirus Disease 2019 Pandemic-United States, 2000–2021. J. Infect. Dis. 2022, 226, 967–974. [Google Scholar] [CrossRef]
- Terliesner, N.; Unterwalder, N.; Edelmann, A.; Corman, V.; Knaust, A.; Rosenfeld, L.; Gratopp, A.; Ringe, H.; Martin, L.; von Bernuth, H.; et al. Viral infections in hospitalized children in Germany during the COVID-19 pandemic: Association with non-pharmaceutical interventions. Front. Pediatr. 2022, 10, 935483. [Google Scholar] [CrossRef]
- Kuitunen, I.; Artama, M.; Haapanen, M.; Renko, M. Noro- and rotavirus detections in children during COVID-19 pandemic-A nationwide register study in Finland. Acta Paediatr. 2022, 111, 1978–1980. [Google Scholar] [CrossRef]
- Zhang, J.; Cao, J.; Ye, Q. Nonpharmaceutical interventions against the COVID-19 pandemic significantly decreased the spread of enterovirus in children. J. Med. Virol. 2022, 94, 3581–3588. [Google Scholar] [CrossRef]
- Yunusa, A.; Cabral, C.; Anderson, E. The impact of the COVID-19 pandemic on the uptake of routine maternal and infant vaccines globally: A systematic review. PLOS Glob. Public Health 2022, 2, e0000628. [Google Scholar] [CrossRef]
- Santoli, J.M.; Lindley, M.C.; DeSilva, M.B.; Kharbanda, E.O.; Daley, M.F.; Galloway, L.; Gee, J.; Glover, M.; Herring, B.; Kang, Y.; et al. Effects of the COVID-19 Pandemic on Routine Pediatric Vaccine Ordering and Administration—United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 591–593. [Google Scholar] [CrossRef]
- Sexton, K.; Susi, A.; Lee, E.; Hisle-Gorman, E.; Rajnik, M.; Krishnamurthy, J.; Nylund, C.M. Trends in Well-Child Visits and Routine Vaccination among Children of U.S. Military Members: An Evaluation of the COVID-19 Pandemic Effects. J. Clin. Med. 2022, 11, 6842. [Google Scholar] [CrossRef]
- Cunniff, L.; Alyanak, E.; Fix, A.; Novak, M.; Peterson, M.; Mevis, K.; Eiden, A.L.; Bhatti, A. The impact of the COVID-19 pandemic on vaccination uptake in the United States and strategies to recover and improve vaccination rates: A review. Hum. Vaccin. Immunother. 2023, 19, 2246502. [Google Scholar] [CrossRef] [PubMed]
- Lebrun-Harris, L.A.; Sappenfield, O.R.; Warren, M.D. Missed and Delayed Preventive Health Care Visits Among US Children Due to the COVID-19 Pandemic. Public Health Rep. 2022, 137, 336–343. [Google Scholar] [CrossRef]
- Leonardelli, M.; Mele, F.; Marrone, M.; Germinario, C.A.; Tafuri, S.; Moscara, L.; Bianchi, F.P.; Stefanizzi, P. The Effects of the COVID-19 Pandemic on Vaccination Hesitancy: A Viewpoint. Vaccines 2023, 11, 1191. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.M.; Pitzer, V.E.; Alonso, W.J.; Vera, D.; Lopman, B.; Tate, J.; Viboud, C.; Parashar, U.D. Global seasonality of rotavirus disease. Pediatr. Infect. Dis. J. 2013, 32, e134–e147. [Google Scholar] [CrossRef] [PubMed]
- Maldonado-Barrueco, A.; García-Rodríguez, J.; Yániz-Ramirez, J.; Serrano-Vaquero, I.; Parra-Alonso, J.C.; Vega-Nieto, C.; Ruiz-Carrascoso, G. Impact of the SARS-CoV-2 Pandemic on the Prevalence and Incidence of Gastrointestinal Viruses in Children up to Five Years Old: A Retrospective Cohort Study. Microbiol. Spectr. 2022, 10, e0266921. [Google Scholar] [CrossRef]
- Liu, P.; Xu, M.; Lu, L.; Ma, A.; Cao, L.; Su, L.; Dong, N.; Jia, R.; Zhu, X.; Xu, J. The changing pattern of common respiratory and enteric viruses among outpatient children in Shanghai, China: Two years of the COVID-19 pandemic. J. Med. Virol. 2022, 94, 4696–4703. [Google Scholar] [CrossRef]
- Lee, E.; Solomon, Z.; Susi, A.; Chokshi, B.; Hisle-Gorman, E.; Nylund, C. Utilizing the US Military’s Electronic Health Records System to Determine COVID-19 Period Effects on Pediatric Acute Gastroenteritis Service Utilization. In Proceedings of the Academy Health Annual Research Meeting, Seattle, WA, USA, 24–27 June 2023; Available online: https://academyhealth.confex.com/academyhealth/2023arm/meetingapp.cgi/Paper/60160 (accessed on 22 April 2025).
- Brueggemann, A.B.; Jansen van Rensburg, M.J.; Shaw, D.; McCarthy, N.D.; Jolley, K.A.; Maiden, M.C.J.; van der Linden, M.P.G.; Amin-Chowdhury, Z.; Bennett, D.E.; Borrow, R.; et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: A prospective analysis of surveillance data. Lancet Digit. Health 2021, 3, e360–e370. [Google Scholar] [CrossRef]
- Rybak, A.; Levy, C.; Angoulvant, F.; Auvrignon, A.; Gembara, P.; Danis, K.; Vaux, S.; Levy-Bruhl, D.; van der Werf, S.; Béchet, S.; et al. Association of Nonpharmaceutical Interventions During the COVID-19 Pandemic With Invasive Pneumococcal Disease, Pneumococcal Carriage, and Respiratory Viral Infections Among Children in France. JAMA Netw. Open 2022, 5, e2218959. [Google Scholar] [CrossRef]
- Bertran, M.; Amin-Chowdhury, Z.; Sheppard, C.L.; Eletu, S.; Zamarreño, D.V.; Ramsay, M.E.; Litt, D.; Fry, N.K.; Ladhani, S.N. Increased Incidence of Invasive Pneumococcal Disease among Children after COVID-19 Pandemic, England. Emerg. Infect. Dis. 2022, 28, 1669–1672. [Google Scholar] [CrossRef]
- Perniciaro, S.; van der Linden, M.; Weinberger, D.M. Reemergence of Invasive Pneumococcal Disease in Germany During the Spring and Summer of 2021. Clin. Infect. Dis. 2022, 75, 1149–1153. [Google Scholar] [CrossRef] [PubMed]
- Deghmane, A.E.; Taha, M.K. Changes in Invasive Neisseria meningitidis and Haemophilus influenzae Infections in France during the COVID-19 Pandemic. Microorganisms 2022, 10, 907. [Google Scholar] [CrossRef]
- Steens, A.; Stanoeva, K.R.; Knol, M.J.; Mariman, R.; de Melker, H.E.; van Sorge, N.M. Increase in invasive disease caused by Haemophilus influenzae b, the Netherlands, 2020 to 2021. Eurosurveillance 2021, 26, 2100956. [Google Scholar] [CrossRef]
- Hallowell, B.D.; Chavers, T.; Parashar, U.; Tate, J.E. Global Estimates of Rotavirus Hospitalizations Among Children Below 5 Years in 2019 and Current and Projected Impacts of Rotavirus Vaccination. J. Pediatric. Infect. Dis. Soc. 2022, 11, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Eberly, M.D.; Gorman, G.H.; Eide, M.B.; Olsen, C.H.; Rajnik, M. The effect of rotavirus immunization on rotavirus gastroenteritis hospitalization rates in military dependents. Vaccine 2011, 29, 650–659. [Google Scholar] [CrossRef]
- Ai, C.E.; Steele, M.; Lopman, B. Disease burden and seasonal impact of improving rotavirus vaccine coverage in the United States: A modeling study. PLoS ONE 2020, 15, e0228942. [Google Scholar] [CrossRef] [PubMed]
- Hill, H.A.; Elam-Evans, L.D.; Yankey, D.; Singleton, J.A.; Kang, Y. Vaccination Coverage Among Children Aged 19-35 Months—United States, 2016. MMWR Morb. Mortal. Wkly. Rep. 2017, 66, 1171–1177. [Google Scholar] [CrossRef]
- Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Infect. Dis. 2018, 18, 1211–1228. [CrossRef]
- Baker, J.M.; Dahl, R.M.; Cubilo, J.; Parashar, U.D.; Lopman, B.A. Effects of the rotavirus vaccine program across age groups in the United States: Analysis of national claims data, 2001–2016. BMC Infect. Dis. 2019, 19, 186. [Google Scholar] [CrossRef]
- Kraay, A.N.M.; Chaney, D.M.; Deshpande, A.; Pitzer, V.E.; Lopman, B.A. Predicting indirect effects of rotavirus vaccination programs on rotavirus mortality among children in 112 countries. NPJ Vaccines 2023, 8, 32. [Google Scholar] [CrossRef]
- Ali, A.S.; Yohannes, M.W.; Tesfahun, T. Hygiene Behavior and COVID-19 Pandemic: Opportunities of COVID-19-Imposed Changes in Hygiene Behavior. Inquiry 2023, 60, 469580231218421. [Google Scholar] [CrossRef] [PubMed]


| Unique Cases of Rotavirus (n = 186) * | Full Study Population (n = 1,268,604) ** | ||
|---|---|---|---|
| Age (months old) | 0–5 months | 42 (22.6%) | 604,871 (47.7%) |
| 6–11 months | 31 (16.7%) | 80,395 (6.3%) | |
| 12–23 months | 42 (22.6%) | 152,975 (12.1%) | |
| 24–35 months | 39 (21.0%) | 148,146 (11.7%) | |
| 36–47 months | 18 (9.7%) | 143,572 (11.3%) | |
| 48–59 months | 14 (7.5%) | 138,645 (10.9%) | |
| Sex | Male | 100 (53.8%) | 648,834 (51.2%) |
| Female | 86 (46.2%) | 619,770 (48.9%) | |
| Sponsor Rank | Junior Enlisted | 44 (23.7%) | 369,208 (29.1%) |
| Other | 142 (76.3%) | 899,396 (70.9%) | |
| Region | North | 35 (18.8%) | 392,933 (31.0%) |
| South | 60 (32.3%) | 376,091 (29.7%) | |
| West | 75 (40.3%) | 409,512 (32.3%) | |
| Outside the US | 16 (8.6%) | 90,068 (7.10%) |
| Rotavirus Hospitalizations | |||
|---|---|---|---|
| Unadjusted RR (95% CI) | Adjusted RR (95% CI) | ||
| Age (reference = 48–59 months) | 0–5 months | 6.27 (3.42, 11.47) | 6.12 (3.33, 11.23) |
| 6–11 months | 4.51 (2.40, 8.49) | 4.43 (2.35, 8.34) | |
| 12–23 months | 3.20 (1.76, 5.85) | 3.17 (1.73, 5.79) | |
| 24–35 months | 2.82 (1.53, 5.19) | 2.79 (1.52, 5.14) | |
| 36–47 months | 1.36 (0.68, 2.72) | 1.35 (0.68, 2.70) | |
| Rank (reference = Junior Enlisted) | Senior Military | 0.82 (0.59, 1.14) | 0.97 (0.69, 1.36) |
| Sex (reference = Male) | Female | 0.90 (0.67, 1.19) | 0.90 (0.67, 1.19) |
| Region (reference = South) | North | 0.57 (0.37, 0.86) | 0.56 (0.37, 0.86) |
| Outside the US | 1.19 (0.69, 2.07) | 1.15 (0.66, 1.99) | |
| West | 1.23 (0.88, 1.72) | 1.19 (0.85, 1.67) | |
| Time Period (reference = Pre-COVID-19) | COVID-19 Year 1 | 0.18 (0.09, 0.35) | 0.18 (0.10, 0.34) |
| COVID-19 Year 2 | 0.41 (0.26, 0.65) | 0.41 (0.26, 0.65) | |
| COVID-19 Year 3 | 0.84 (0.59, 1.19) | 0.84 (0.59, 1.19) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Penfold, M.D.; Prabhakar, S.; Susi, A.; Rajnik, M.; Nylund, C.M.; Eberly, M.D. Pediatric Rotavirus Hospitalization Rates in the Military Health System Before and During the COVID-19 Pandemic. Vaccines 2025, 13, 492. https://doi.org/10.3390/vaccines13050492
Penfold MD, Prabhakar S, Susi A, Rajnik M, Nylund CM, Eberly MD. Pediatric Rotavirus Hospitalization Rates in the Military Health System Before and During the COVID-19 Pandemic. Vaccines. 2025; 13(5):492. https://doi.org/10.3390/vaccines13050492
Chicago/Turabian StylePenfold, Matthew D., Sarah Prabhakar, Apryl Susi, Michael Rajnik, Cade M. Nylund, and Matthew D. Eberly. 2025. "Pediatric Rotavirus Hospitalization Rates in the Military Health System Before and During the COVID-19 Pandemic" Vaccines 13, no. 5: 492. https://doi.org/10.3390/vaccines13050492
APA StylePenfold, M. D., Prabhakar, S., Susi, A., Rajnik, M., Nylund, C. M., & Eberly, M. D. (2025). Pediatric Rotavirus Hospitalization Rates in the Military Health System Before and During the COVID-19 Pandemic. Vaccines, 13(5), 492. https://doi.org/10.3390/vaccines13050492






