Incidence of Pertussis in Older Children Underestimated in the Whole-Cell Vaccine Era: A Cross-Sectional Seroprevalence Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Research Subjects
2.2. Laboratory Testing
2.3. Statistical Analysis
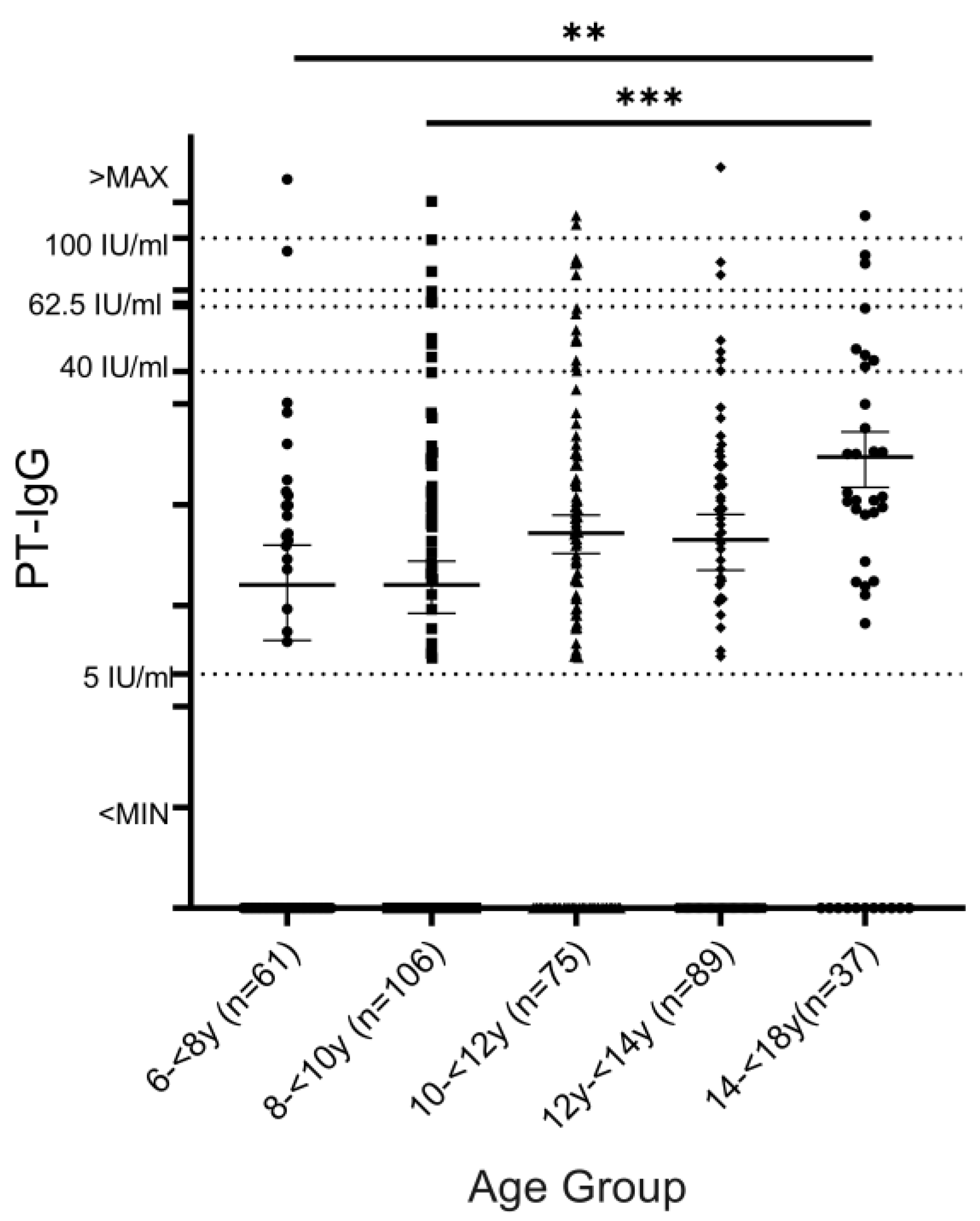
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EPI | Expanded Program on Immunization |
| wP | Whole-cell pertussis |
| DTwP | Diphtheria, tetanus, and whole-cell pertussis |
| DTaP | Diphtheria, tetanus, and acellular pertussis |
| PT | Pertussis toxin |
| TT | Tetanus toxin |
References
- Kilgore, P.E.; Salim, A.M.; Zervos, M.J.; Schmitt, H.J. Pertussis: Microbiology, disease, treatment, and prevention. Clin. Microbiol. Rev. 2016, 29, 449–486. [Google Scholar] [CrossRef] [PubMed]
- Lindstrand, A.; Cherian, T.; Chang-Blanc, D.; Feikin, D.; O’Brien, K.L. The world of immunization: Achievements, challenges, and strategic vision for the next decade. J. Infect. Dis. 2021, 224 (Suppl. S2), S452–S467. [Google Scholar] [CrossRef]
- Guiso, N.; Meade, B.D.; Wirsing von König, C.H. Pertussis vaccines: The first hundred years. Vaccine 2020, 38, 1271–1276. [Google Scholar] [CrossRef] [PubMed]
- Notice on the Adjustment of Immunization Schedules for National Immunization Program’s Diphtheria-Tetanus-Pertussis (DTP) Vaccine and Tetanus-Diphtheria (TD) Vaccine. Available online: https://www.ndcpa.gov.cn/jbkzzx/c100014/common/content/content_1872098276166717440.html (accessed on 26 December 2024).
- Wan, M.; Zhang, G.; Yi, H. Unraveling the resurgence of pertussis: Insights into epidemiology and global health strategies. Pulmonology 2024, 30, 503–505. [Google Scholar] [CrossRef]
- Zhang, D.; Mu, Q.; Dai, L.; Zhu, Q. Evaluation of the Effectiveness of Checking Vaccination Certificates for School Entry and Admission to Childcare Institutions in Guizhou Province from 2003 to 2009. Xian Dai Yu Fang Yi Xue 2013, 40, 864–867. (In Chinese) [Google Scholar]
- Shi, W.; Wang, B.; Meng, Q.; Zhang, X.; Li, Z.; He, F.; Ying, F.; Cong, L.; Yao, K. Seroprevalence of tetanus and pertussis antibodies among health care workers in Wuhu, China. Hum. Vaccines Immunother. 2024, 20, 2318892. [Google Scholar] [CrossRef] [PubMed]
- Hua, C.Z.; He, H.Q.; Shu, Q. Resurgence of pertussis: Reasons and coping strategies. World J. Pediatr. 2024, 20, 639–642. [Google Scholar] [CrossRef]
- Ning, G.J.; Gao, Y.; Wu, D.; Li, J.H.; Li, Y.X.; Shao, Z.J.; Yin, Z.D. Epidemiology of pertussis in China, 2011–2017. Chin. J. Vaccines Immun. 2018, 3, 264–267. [Google Scholar]
- Jiang, F.; Mu, Q.; Zhang, D.; Feng, J.; Zhu, Q. Epidemiological characteristic of pertussis reported cases from 2004 to 2013, Guizhou Province. Xian Dai Yu Fang Yi Xue 2015, 42, 1927–1930+1924. (In Chinese) [Google Scholar]
- Hu, Y.; Guo, M.; Yao, K. Infections in preschool and school-aged children are driving the recent rise in pertussis in China. J. Infect. 2024, 88, 106170. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Zheng, H.; Liu, M.; Han, K.; Shu, J.; Wu, C.; Xu, N.; He, Q.; Luo, H. The seroepidemiology of immunoglobulin G antibodies against pertussis toxin in China: A cross-sectional study. BMC Infect. Dis. 2012, 12, 138. [Google Scholar] [CrossRef] [PubMed]
- Zheng, M.H.; Jiao, Z.Q.; Zhang, L.J.; Yu, S.J.; Tang, G.P.; Yan, X.M.; He, L.H.; Meng, F.L.; Zhao, F.; Zhang, M.J.; et al. Genetic analysis of group A streptococcus isolates recovered during acute glomerulonephritis outbreaks in Guizhou Province of China. J. Clin. Microbiol. 2009, 47, 715–720. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control (ECDC). Laboratory Diagnosis and Molecular Surveillance of Bordetella Pertussis [EB/OL]. 21 December 2022. Available online: https://www.ecdc.europa.eu/en/publications-data/bordetella-pertussis-laboratory-diagnosis-and-molecular-surveillance (accessed on 6 June 2023).
- Meng, Q.; Qian, Q.; Li, L.; Liu, D.; Gao, W.; Yuan, L.; Yao, K. The maternal antibody against diphtheria, tetanus and pertussis showed distinct regional difference in China. BMC Pediatr. 2019, 19, 480. [Google Scholar] [CrossRef] [PubMed]
- Wendelboe, A.M.; Van Rie, A.; Salmaso, S.; Englund, J.A. Duration of immunity against pertussis after natural infection or vaccination. Pediatr. Infect. Dis. J. 2005, 24, S58–S61. [Google Scholar] [CrossRef]
- Lambert, H.J. Epidemiology of a small pertussis outbreak in Kent County, Michigan. Public Health Rep. 1965, 80, 365–369. [Google Scholar] [CrossRef] [PubMed]
- Grimprel, E.; Bégué, P.; Anjak, I.; Njamkepo, E.; François, P.; Guiso, N. Long-term human serum antibody responses after immunization with whole-cell pertussis vaccine in France. Clin. Diagn. Lab. Immunol. 1996, 3, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Torvaldsen, S.; McIntyre, P.B. Effect of the preschool pertussis booster on national notifications of disease in Australia. Pediatr. Infect. Dis. J. 2003, 22, 956–959. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, A.M.; Baptista, P.N.; Ximenes, R.A.; Rodrigues, L.C.; Magalhães, V.; Silva, A.R.S.; Souza, N.F.; Matos, D.G.C.D.; Pessoa, A.K.L. Pertussis may be the cause of prolonged cough in adolescents and adults in the interepidemic period. Braz. J. Infect. Dis. 2015, 19, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Chinese Preventive Medicine Association; Vaccine and Immunology Branch of the Chinese Preventive Medicine Association. Expert consensus on the China Pertussis Initiative. Zhonghua Yu Fang Yi Xue Za Zhi 2021, 55, 709–719. (In Chinese) [Google Scholar]
- Shi, W.; Meng, Q.; Hu, Y.; Feng, G.; Wang, X.; Yao, K. Epidemiology of pertussis among pediatric inpatients in mainland. China J. Infect. 2024, 89, 106327. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Cheng, X.; Wei, S.; Yuan, L.; Chen, C.; Yao, K. Decline of serologic immunity to diphtheria, tetanus and pertussis with age suggested a full life vaccination in mainland China. Hum. Vaccines Immunother. 2021, 17, 1757–1762. [Google Scholar] [CrossRef]
- Chen, Q.; Wang, W.; Shi, X.; Xu, Y.; Zhu, Y.; Wu, Y.; Wang, Z.; Sun, H.; Sun, X. Seroepidemiology of pertussis in the east of China: Estimates of incidence of infection in adolescents and adults pre- and post-COVID-19. Front. Public Health 2022, 10, 1054617. [Google Scholar] [CrossRef]
| No. | Anti-PT IgG | Anti-TT IgG | |||||
|---|---|---|---|---|---|---|---|
| <5 IU/mL | 5–62.5 IU/mL | >62.5 IU/mL | <0.1 IU/mL | 0.1–1 IU/mL | >1 IU/mL | ||
| Total | 368 | 204 (55.4%) | 148 (40.2%) | 16 (4.9%) | 154 (41.8%) | 165 (44.8%) | 49 (13.4%) |
| Age | |||||||
| 6–<8 y | 61 | 41 (67.2%) | 18 (29.5%) | 2 (3.3%) | 15 (24.6%) | 35 (57.4%) | 11 (18.0%) |
| 8–<10 y | 106 | 72 (67.9%) | 30 (28.3%) | 4 (3.8%) | 33 (31.0%) | 54 (50.9%) | 19 (17.9%) |
| 10–<12 y | 75 | 36 (48.0%) | 36 (48.0%) | 3 (4.0%) | 34 (45.3%) | 31 (41.4%) | 10 (13.3%) |
| 12–<14 y | 89 | 45 (50.6%) | 41 (46.1%) | 3 (3.3%) | 48 (53.9%) | 35 (39.4%) | 6 (6.7%) |
| 14–<18 y | 37 | 10 (27.0%) | 23 (62.2%) | 4 (10.8%) | 24 (64.9%) | 10 (27.0%) | 3 (8.1%) |
| School | |||||||
| A | 26 | 16 (61.5%) | 7 (26.9%) | 3 (11.6%) | 8 (30.8%) | 16 (61.5%) | 2 (7.7%) |
| B | 39 | 18 (46.2%) | 20 (51.3%) | 1 (2.5%) | 17 (43.6%) | 20 (51.28%) | 2 (5.1%) |
| C | 40 | 16 (40.0%) | 20 (50.0%) | 4 (10.0%) | 19 (47.5%) | 13 (32.5%) | 8 (20.0%) |
| D | 26 | 4 (15.4%) | 17 (65.4%) | 5 (19.2%) | 10 (38.5%) | 9 (34.6%) | 7 (26.9%) |
| E | 84 | 51 (60.7%) | 32 (38.1%) | 1 (1.2%) | 23 (27.3%) | 48 (57.1%) | 13 (15.6%) |
| F | 43 | 33 (76.7%) | 9 (20.9%) | 1 (2.4%) | 17 (39.5%) | 23 (53.5%) | 3 (7.0%) |
| G | 82 | 43 (52.4%) | 38 (46.3%) | 1 (1.2%) | 47 (57.3%) | 24 (29.3%) | 11 (12.6%) |
| H | 28 | 23 (82.1%) | 5 (17.9%) | 0 (0.0%) | 13 (46.4%) | 12 (42.9%) | 3 (10.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Du, Q.-Q.; Meng, Q.-H.; Shi, W.; Yao, K.-H. Incidence of Pertussis in Older Children Underestimated in the Whole-Cell Vaccine Era: A Cross-Sectional Seroprevalence Study. Vaccines 2025, 13, 200. https://doi.org/10.3390/vaccines13020200
Du Q-Q, Meng Q-H, Shi W, Yao K-H. Incidence of Pertussis in Older Children Underestimated in the Whole-Cell Vaccine Era: A Cross-Sectional Seroprevalence Study. Vaccines. 2025; 13(2):200. https://doi.org/10.3390/vaccines13020200
Chicago/Turabian StyleDu, Qian-Qian, Qing-Hong Meng, Wei Shi, and Kai-Hu Yao. 2025. "Incidence of Pertussis in Older Children Underestimated in the Whole-Cell Vaccine Era: A Cross-Sectional Seroprevalence Study" Vaccines 13, no. 2: 200. https://doi.org/10.3390/vaccines13020200
APA StyleDu, Q.-Q., Meng, Q.-H., Shi, W., & Yao, K.-H. (2025). Incidence of Pertussis in Older Children Underestimated in the Whole-Cell Vaccine Era: A Cross-Sectional Seroprevalence Study. Vaccines, 13(2), 200. https://doi.org/10.3390/vaccines13020200





